Abstract
Background
Controlling cholesterol levels is one of the primary goals of preventing atherosclerotic plaque progression in patients undergoing coronary artery bypass graft (CABG) surgery. This study aimed to investigate the impact of serum cholesterol profile at multiple time points following isolated CABG surgery on long-term patient outcomes.
Method
This retrospective cohort study was conducted on the admission and follow-up data of isolated CABG patients from the Tehran Heart Center registry between 2009 and 2016. The association of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and their ratio as an atherogenic index with major adverse cardiac and cerebrovascular events (MACCE) and all-cause mortality were evaluated using time-varying survival analysis methods.
Result
A total of 18657 patients were included in this analysis. After adjusting for known confounding factors, no significant difference in all-cause mortality and MACCE was observed at different LDL levels. The incidence of acute coronary syndrome (ACS) in patients with LDL > 100 mg/dl and LDL < 50 mg/dl was significantly higher than in the control group (P-value = 0.004 and 0.04, respectively). The incidence of cerebrovascular accidents (CVA) at LDL > 100 mg/dl was also significantly higher compared to the control group (P -value = 0.033). Lower HDL levels were significantly associated with a higher MACCE (P -value < 0.001), all-cause mortality (P -value < 0.001), ACS (P -value = 0.00), and CVA (P -value = 0.014). The atherogenic index was also directly related to MACCE and all its components (all P-values < 0.001).
Conclusion
LDL/HDL ratio is suggested as a better marker for secondary prevention goals compared to LDL alone in patients undergoing CABG surgery.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Dyslipidemia, particularly elevated low-density lipoprotein cholesterol (LDL), is one of the major risk factors leading to the formation and progression of atherosclerotic plaques that lead to coronary artery disease (CAD) [1]. LDL particles can pass through the endothelium of the vascular wall, oxidize, and subsequently cause inflammation and damage to the vascular wall and surrounding smooth muscle cells [2]. These processes can finally lead to atherosclerosis and the subsequent events resulting from vascular stenosis and occlusion. Therefore, controlling the serum level of LDL is one of the primary goals in preventing atherosclerosis progression and its complications [3, 4].
Coronary artery bypass graft (CABG) surgery is a common treatment strategy for coronary artery disease. Over 800,000 CABG surgeries are performed annually in the world [5]. Several indices, including cholesterol profile, can exacerbate coronary artery atherosclerosis and lead to major adverse cardiac and cerebrovascular events (MACCE) after the surgery [5,6,7]. Secondary prevention of CAD following surgery and control of established risk factors, such as serum cholesterol profile, are required to obtain favorable outcomes. Given the dynamic nature of cholesterol profiles based on adherence to lipid-lowering medicines, conducting a time-varying analysis is critical in evaluating the impact of these risk variables on CABG patients' long-term results. This is especially critical because patient adherence to lipid-lowering medicines has significantly impacted patient outcomes [8, 9].
Previous studies have reported the benefits of high-intensity statin therapy after CABG surgery in reducing the incidence of MACCE [10,11,12]. The European Society of Cardiology (ESC) and the American Heart Association/American College of Cardiology (AHA/ACC) practice guidelines recommend serum LDL reduction as a protective measure against long-term MACCE [13, 14]. Nonetheless, the current literature includes sparse evidence comparing different levels of serum cholesterol components at multiple time points after isolated CABG surgery on the incidence of MACCE. On the other hand, several studies have suggested atherogenic indices, such as LDL/HDL ratio, as a risk predictor of cardiovascular disorders [15,16,17,18]. However, the prediction value of these indices for CABG outcomes has not yet been reported. Previous studies have mainly focused on comparing the effect of lipid-lowering agents and their doses on the outcomes of CABG surgery without assessing the impact of the atherogenic index over the follow-up time [19].
This study aimed to assess the impact of postoperative serum LDL and HDL levels at multiple time points on long-term patient outcomes of CABG surgery. Furthermore, the ratio of these factors was investigated as an atherogenic index at various time points after the procedure, considering the dynamic nature of their influence using a time-varying analysis.
Methods
Study design
This was a large-scale retrospective cohort study on patients undergoing isolated CABG surgery at Tehran Heart Center from March 2009 to March 2016. Data on these patients were retrieved from the Adult Cardiac Surgery Database [20, 21]. The proposal for this study was reviewed and approved by the research board and committee of ethics at Tehran Heart Center (IR.TUMS.MEDICINE.REC.1398.841).
Study setting
Tehran Heart Center is a high-volume tertiary referral hospital affiliated with the Tehran University of Medical Sciences, operating since 2002.
Participants
The study inclusion criteria consisted of all adult patients undergoing isolated CABG surgery between 2009–2016. Patients with simultaneous valvular or congenital heart defect surgery, missing data, or no follow-up data were excluded from the study. Informed consent was obtained from all patients at admission to allow the use of their clinical data for research purposes.
CABG surgeries were performed at Tehran Heart Center by a team of expert cardiovascular surgeons. Following CABG surgery, all patients are evaluated at the surgery follow-up clinic 4–6 and 12 months after surgery and annually thereafter. Patients' symptoms, changes in the risk factors, laboratory tests, and medications were reviewed at each visit. The laboratory tests included measurement of fasting blood glucose, urea, creatinine, lipid profile, complete blood cell count, and liver function tests. Any occurrence of MACCE, defined by non-fatal acute coronary syndrome (ACS), non-fatal revascularization, and non-fatal cerebrovascular accident (CVA), was also recorded. A general practitioner conducted follow-up visits in person, and a trained nurse attained the patient's symptoms, MACCE, and test results. If a patient could not attend their follow-up appointment, a trained nurse would complete the form over the phone. Additionally, the mortality rates of the patients were investigated by phone calls, and a mortality form was completed for every deceased patient to identify the cause of death, i.e., cardiac or non-cardiac.
According to the previous studies [22,23,24,25], Eligible patients were categorized into four groups according to the LDL levels at each visit: 1- LDL < 50 mg/dl, 2- LDL = 50–70 mg/dl, 3- LDL = 70–100 mg/dl, 4- LDL > 100 mg/dl. Based on the latest guidelines, LDL = 50–70 mg/dl was considered the reference group and other LDL levels were compared to this group. All baseline and follow-up variables were subsequently compared between the LDL groups to assess their predictive value for MACCE and all-cause mortality. Subsequently, the effect of HDL levels and atherogenic index (LDL/HDL ratio) on MACEE and its components was further evaluated.
Statistical analysis
The normally distributed continuous variables were described as mean with standard deviation (SD) and were compared between the LDL level groups using one-way analysis of variance (ANOVA). The skew-distributed variables were expressed as median with 25th and 75th percentiles and were compared between groups applying the Kruskal–Wallis test. Categorical variables were described as frequency with percentages, and their distribution among LDL level groups was compared using a chi-square test. The unadjusted and adjusted effects of LDL and LDL/HDL ratio as a time-varying covariate on all-cause mortality and MACCE were evaluated using an extended COX regression model. The results were reported through hazard ratios (HR) and 95% confidence intervals (CIs). The proportional hazards (PH) assumption was assessed using the chi-square test of the correlation coefficient of scaled Schoenfeld residuals and time. The confounder variables for the adjusted model were selected according to the literature. The effects of LDL levels and LDL to HDL ratio on each MACCE component, including ACS and CVA, were assessed in a competing risk setting, considering death as a competing event. The effects were reported via sub-distribution hazard ratio (sHR) and 95% CI. Statistical analyses were conducted using Stata Statistical Software, release 15.2 (College Station, TX: Stata Corp.).
Results
Participants
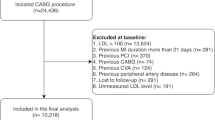
A total of 21380 CABG surgeries were performed at Tehran Heart Center during the study period. After excluding patients according to the inclusion/exclusion criteria, 18941 patients who underwent isolated CABG surgery were eligible for the study. Follow-up data regarding 18657 of these patients were retrieved. The follow-up record for 284 patients (1.4%) could not be achieved (due to migrations, unwillingness for follow-up visits, or lack of a contact number). The median follow-up duration was 4.5 years, with 80754 patient-years of follow-up. A final number of 18657 patients were included in the study with an average age of 67.1 ± 9.7 years old. There were 13689 (73.4%) male patients in the study population.
Descriptive data
In a total of 82421 follow-up visits, postoperative LCL and HDL levels were measured and reported (an average of 4.4 measurements for every patient). According to the baseline LDL levels, patients were divided into four groups (LDL < 50, 50 < LDL < 70, 70 < LDL < 100, and LDL > 100). Figure 1A and B demonstrate the distribution of serum LDL groups at the time of surgery and follow-up visits, respectively.
Table 1 describes the patient characteristics for the total population and 4 LDL-level groups. Among the most common comorbidities, 39.9% of the patients were diagnosed with diabetes mellitus, 54.7% had hypertension, and 2.2% had chronic kidney disease. There was an 18.1% and 11% rate for cigarette and opium addiction at the time of surgery, respectively.
In order to identify cofounder factors, 16 variables were selected based on the differences observed between variables in four LDL groups. The variables identified as confounder factors were age, sex, body mass index, ejection fraction (EF), blood pressure, diabetes, smoking, opium, kidney failure, chronic obstructive pulmonary disease (COPD), CVA, serum HDL level, number of grafts, Intensive care unit (ICU) stay, myocardial infarction in the last seven days, and off-pump CABG surgery.
Outcome data
The primary outcome variables of all-cause mortality, MACCE, CVA, and ACS in the follow-up period are compared between the four LDL level groups in Table 2 before the adjustments for confounder variables. The incidence of all-cause mortality in the 70 ≤ LDL < 100 mg/dl (P -value = 0.025) and LDL ≥ 100 mg/dl (P -value < 0.001) groups and MACCE in the LDL ≥ 100 mg/dl group (P -value < 0.001), was significantly less than the reference group 50 < LDL ≤ 70 mg/dl (Table 2).
Table 3 compares the primary outcome variables between four LDL groups after adjustment for 16 confounder variables. The relationship between four LDL groups and primary outcome variables (all-cause mortality and MACCE) before and after adjustment for confounding factors is illustrated in Figs. 2 and 3.
According to this adjusted model, all-cause mortality and MACCE incidence in any LDL group were not significantly different from the reference group (Table 3). However, the incidence of ACS in patients with LDL levels greater than 100 mg/dl and less than 50 mg/dl during follow-up was significantly higher than in the reference group (P-value = 0.004 and P-value = 0.04, respectively) after adjustment for known confounding factors. Furthermore, CVA was significantly higher in cases with LDL levels greater than 100 mg/dl compared to the reference group (P-value = 0.033, Table 3).
Moreover, a lower HDL level was significantly associated with a higher incidence of MACCE (P-value < 0.001), all-cause mortality (P-value < 0.001), ACS (P-value = 0.004), and CVA (P-value = 0.017). Regression analysis revealed that with every 1 mg/dl increase in serum HDL level, the incidence of all-cause mortality decreases by 7.1% and MACCE by 4.1%.
Finally, a higher LDL/HDL ratio was significantly associated with increased incidence of MACCE, all-cause mortality, ACS, and CVA (all P-values < 0.001). The regression analysis results suggested that with every 0.5 unit increase in this ratio, all-cause mortality increased by 5%, MACCE by 5.7%, ACS by 6%, and CVA by 9.5%. By selecting the median for the LDL/HDL ratio (2.25) as a cut-off point, the patients with a higher than median LDL/HDL value had a significantly higher HR for MACCE rate (26%), the all-cause mortality rate (23%), ACS (26%), and CVA (37%). Long-term survival analysis comparison between 2 groups according to LDL/HDL ratio is demonstrated in Figs. 4 and 5 indicating a significantly higher long-term mortality and MACCE in patients with an LDL/HDL ratio of higher than 2.25. The Proportional Hazards (PH) assumption was not violated in any of the final models for different patient groups according to LDL levels or LDL/HDL ratio.
Moreover, After the adjustments for known confounding factors, older age, male gender, lower EF, hypertension, renal failure, COPD, CVA, lower HDL, longer ICU hospitalization, and off-pump surgery were independently associated with a significantly higher MACCE and mortality rate after CABG (all P-values < 0.001, Table 4).
Discussion
This study evaluated the effect of cholesterol profile at multiple follow-up time points on long-term outcomes of isolated CABG patients in a sizeable registry-based cohort study utilizing a time-varying analysis. The incidence of ACS was significantly higher in patients with LDL levels of more than 100 mg/dl and less than 50 mg/dl, although all-cause mortality and MACCE were not associated with different LDL levels. In contrast, HDL levels were significantly associated with postoperative MACCE and its components. Furthermore, a strong association was detected between the atherogenic index and all cardiovascular outcomes (MACCE, ACS, CVA, and all-cause mortality) following CABG surgery.
The current study results align with the findings of the CASCADE study, which suggests that reaching LDL levels of less than 100 mg/dl with statin therapy is independently associated with greater patency of coronary arteries following CABG. This study also reported that lower LDL (< 70 mg/dl) levels had no further improvement in the patency of coronary arteries [11].
A paradoxical increase in the incidence of post-CABG ACS in the LDL < 50 mg/dl group was also detected. Several recent studies have also detected a similar paradoxical cardiovascular outcome in patients with low LDL levels [26,27,28,29]. In a study by Nakahashi et al., all-cause mortality rates were paradoxically higher for patients with ACS when their LDL levels were below 100 mg/dl [26]. One possible reason could be the lower dose of post-discharge statin treatment received by patients with LDL < 100 mg/dl compared to patients with LDL levels above 100 mg/dl. Statins are essential in protecting the coronary endothelium due to their anti-inflammatory effects and stabilization of atherosclerotic plaques [30]. Furthermore, Wang et al., in a study on 41,229 CAD patients, reported that malnutrition might be the cause of poor cardiovascular outcomes in patients with a low LDL level [28]. Additional studies are required to fully understand the impact of low LDL levels and statin treatments on the outcomes of CAD patients.
Another important finding of this study is the association of HDL levels with long-term CABG outcomes. Previous studies have also reported this inverse relationship between serum HDL and cardiovascular events in CAD patients [31]. In a survey by Domanski et al. on 1,248 CABG patients, the survival rate was significantly higher in patients with HDL > 35 mg/dl compared to patients with HDL < 35mg/dl. Similarly, patients with a higher HDL reported significantly lower post-CABG revascularization and myocardial infarction [6]. Several studies have indicated that although increasing serum HDL levels through non-pharmacological measures (diet, exercise, and smoking cessation) is associated with better cardiovascular outcomes [32,33,34], increasing HDL levels through medication was not effective in reducing cardiovascular events [31, 35, 36].
Lastly, LDL/ HDL ratio was investigated as an atherogenic index to simultaneously assess the effects of HDL and LDL levels on patient outcomes, revealing a significant association. Recent studies also propose this index as a valuable predictor for cardiovascular risk assessments [37,38,39,40]. In a study on the Framingham data, Nam et al. reported HDL/Total cholesterol and HDL/LDL as better predictors for cardiovascular outcomes compared to total cholesterol or LDL alone [41]. In an assessment of the Finnish Kuopio Ischemic heart disease (IHD) prospective cohort study, the LDL/HDL ratio was an independent risk factor for sudden cardiac death in IHD patients [42]. Also, Sheng et al. suggested a non-high-density/HDL ratio as a better predictor of diabetes risk compared to cholesterol components [43]. Considering emerging suggestions on utilizing atherogenic index as a cardiovascular predictive factor, LDL/HDL ratio can be a practical outcome predictor for CABG patients.
Nonetheless, more studies are required to reach an exact LDL/HDL ratio threshold as a post-CABG patient management goal. According to the current study, extended COX regression could not determine a specific off-cut point for the atherogenic index that best predicts a patient's cardiovascular outcomes. Therefore, the median of this ratio, which measured 2.25, can be regarded as a secondary objective after attaining LDL levels below 100 mg/dl.
The large sample size, long-term patient follow-ups, multiple cholesterol profile assessments at different time points, and time-varying analysis can distinguish the present study from the current evidence in the literature. The majority of previous studies, including the ACTIVE trial, examined the effect of different therapeutic doses of statins on anatomical outcomes (e.g., coronary artery occlusion in coronary computed tomography angiography) [10]. However, the assessed study endpoint was MACCE, its components, and all-cause mortality. The report of these outcomes can be more practical in predicting long-term surgical results as postoperative artery occlusion depends on multiple variables, such as surgical techniques.
Strengths and limitations
The large patient population and cholesterol profile assessments at multiple time points were the key strengths of this study. Nevertheless, the main limitation of the present study was the absence of statin treatment dose in the results. Changes in the statin dose based on patients' LDL levels during follow-up could distort the study's results. It was not possible to incorporate additional atherogenic indices like APO-A, APO-B, and LP(a) into the study since these measurements were not part of the routine assessment for the CABG patients. Lastly, despite attempts to identify all variables influencing the cardiovascular outcomes of patients following CABG surgery for adjusting confounding factors, other factors could be impacting the study results.
Conclusion
According to the study findings, LDL level assessment as secondary prevention is insufficient to guide the treatment of CABG patients. Physicians should consider LDL/HDL ratio to better predict patients' cardiovascular risk. A recommended HDL/LDL ratio of < 2.25 and LDL < 100 mg/dl is advised as a secondary prevention goal for patients after isolated CABG surgery and can significantly improve long-term patient outcomes.
Availability of data and materials
The datasets regarding the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ACS:
-
Acute Coronary Syndrome
- CABG:
-
Coronary Artery Bypass Graft
- CAD:
-
Coronary artery disease
- CI:
-
Confidence Interval
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic Obstructive Pulmonary Disease
- CVA:
-
Cerebrovascular Accident
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes Mellitus
- EF:
-
Ejection Fraction
- ESC:
-
European Society of Cardiology
- HDL:
-
High-density Cholesterol
- HTN:
-
Hypertension
- HR:
-
Hazard Ratio
- ICU:
-
Intensive Care Unit
- LDL:
-
Low-density Cholesterol
- MACE:
-
Major Adverse Cardiovascular Events
- MI:
-
Myocardial Infarction
- PCI:
-
Percutaneous Intervention
- SBP:
-
Systolic blood pressure
References
Yurtseven E, et al. An Update on the Role of PCSK9 in Atherosclerosis. J Atheroscler Thromb. 2020;27(9):909–18.
Ding Z, et al. PCSK9 and inflammation: role of shear stress, pro-inflammatory cytokines, and LOX-1. Cardiovasc Res. 2020;116(5):908–15.
Fernández-Friera L, et al. Normal LDL-cholesterol levels are associated with subclinical atherosclerosis in the absence of risk factors. J Am Coll Cardiol. 2017;70(24):2979–91.
Nordestgaard BG, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34(45):3478–90.
Nalysnyk L, et al. Adverse events in coronary artery bypass graft (CABG) trials: a systematic review and analysis. Heart. 2003;89(7):767–72.
Domanski MJ, et al. Prognostic factors for atherosclerosis progression in saphenous vein grafts: the postcoronary artery bypass graft (Post-CABG) trial. Post-CABG Trial Investigators. J Am Coll Cardiol. 2000;36(6):1877–83.
Ayati A, et al. Surgical coronary revascularization in patients with COVID-19; complications and outcomes: a retrospective cohort study. Health Sci Rep. 2022;5(5):e751.
Colantonio LD, et al. adherence to statin therapy among US adults between 2007 and 2014. J Am Heart Assoc. 2019;8(1):e010376.
Rodriguez F, et al. association of statin adherence with mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol. 2019;4(3):206–13.
Kulik A, et al. Intensive versus moderate atorvastatin therapy and one-year graft patency after CABG: Rationale and design of the ACTIVE (Aggressive Cholesterol Therapy to Inhibit Vein Graft Events) randomized controlled trial (NCT01528709). Contemp Clin Trials. 2017;59:98–104.
Kulik A, et al. Statin therapy and saphenous vein graft disease after coronary bypass surgery: analysis from the CASCADE randomized trial. Ann Thorac Surg. 2011;92(4):1284–90 (discussion 1290-1).
Shah SJ, et al. Intensive lipid-lowering with atorvastatin for secondary prevention in patients after coronary artery bypass surgery. J Am Coll Cardiol. 2008;51(20):1938–43.
Grundy SM, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–143.
Mach F, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205.
Qin P, et al. Low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio and carotid intima-media thickness: a cohort study in China. Lipids. 2021;56(1):59–68.
Nimkuntod P, Tongdee P. Plasma low-density lipoprotein cholesterol/high-density lipoprotein cholesterol concentration ratio and early marker of carotid artery atherosclerosis. J Med Assoc Thai. 2015;98(Suppl 4):S58–63.
Matsumoto I, et al. Impact of low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio on long-term outcome in patients undergoing percutaneous coronary intervention. Circ J. 2011;75(4):905–10.
Yokokawa H, et al. Serum low-density lipoprotein to high-density lipoprotein ratio as a predictor of future acute myocardial infarction among men in a 2.7-year cohort study of a Japanese northern rural population. J Atheroscler Thrombosis. 2010;18(2):89–98.
Alkhalil M. Effects of intensive lipid-lowering therapy on mortality after coronary bypass surgery: a meta-analysis of 7 randomised trials. Atherosclerosis. 2020;293:75–8.
Abbasi K, et al. Knowledge management in cardiac surgery: the second tehran heart center adult cardiac surgery database report. J Tehran Univ Heart Center. 2012;7(3):111.
Karimi A, et al. First database report on cardiothoracic surgery in Tehran Heart Center. Iran J Public Health. 2008;37(2):1–8.
Ma C, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93(5):e445–57.
Faselis C, et al. Is very low LDL-C harmful? Curr Pharm Des. 2018;24(31):3658–64.
Hsia J, et al. Cardiovascular event reduction and adverse events among subjects attaining low-density lipoprotein cholesterol< 50 mg/dl with rosuvastatin: the JUPITER trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin). J Am Coll Cardiol. 2011;57(16):1666–75.
Rallidis LS, Tsamoulis D, Leventis I, Kalogeras P, Delakis I, Samiotis E, et al. Extremely high-risk patients with acute coronary syndrome: how "extreme" should be the lipid-lowering therapy if the LDL-C target <40 mg/dL is considered? Kardiol Pol. 2023. https://doi.org/10.33963/KP.a2023.0147.
Nakahashi T, et al. Paradoxical impact of decreased low-density lipoprotein cholesterol level at baseline on the long-term prognosis in patients with acute coronary syndrome. Heart Vessels. 2018;33(7):695–705.
Reddy VS, et al. relationship between serum low-density lipoprotein cholesterol and in-hospital mortality following acute myocardial infarction (the lipid paradox). Am J Cardiol. 2015;115(5):557–62.
Wang B, et al. malnutrition affects cholesterol paradox in coronary artery disease: a 41,229 Chinese cohort study. Lipids Health Dis. 2021;20(1):1–8.
Al-Mallah MH, et al. Low admission LDL-cholesterol is associated with increased 3-year all-cause mortality in patients with non ST segment elevation myocardial infarction. Cardiol J. 2009;16(3):227–33.
Golia E, et al. Inflammation and cardiovascular disease: from pathogenesis to therapeutic target. Curr Atheroscler Rep. 2014;16(9):435.
Iatan I, Choi HY, Genest J. High-Density Lipoprotein and Cardiovascular Disease—Where do We Stand? Endocrinol Metab Clin. 2022;51(3):557–72.
Puri R, et al. The beneficial effects of raising high-density lipoprotein cholesterol depends upon achieved levels of low-density lipoprotein cholesterol during statin therapy: implications for coronary atheroma progression and cardiovascular events. Eur J Prev Cardiol. 2016;23(5):474–85.
Santos-Gallego C.G, Badimón J.J. High-density lipoprotein and cardiovascular risk reduction: Promises and realities. 2012. p. 305–8.
Adorni MP, et al. High density lipoprotein cholesterol efflux capacity and atherosclerosis in cardiovascular disease: pathophysiological aspects and pharmacological perspectives. Cells. 2021;10(3):574.
Kaur N, et al. Effect of HDL-raising drugs on cardiovascular outcomes: a systematic review and meta-regression. PLoS One. 2014;9(4): e94585.
Riaz H, et al. Effects of high-density lipoprotein targeting treatments on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2019;26(5):533–43.
Sun T, et al. Predictive value of LDL/HDL ratio in coronary atherosclerotic heart disease. BMC Cardiovasc Disord. 2022;22(1):1–11.
Zhong Z, et al. Assessment of the LDL-C/HDL-C ratio as a predictor of one year clinical outcomes in patients with acute coronary syndromes after percutaneous coronary intervention and drug-eluting stent implantation. Lipids Health Dis. 2019;18(1):1–8.
Uzokov J, Alyavi B, Payziev D. Influence of diet with low glycemic index on triglycerides, glycated hemoglobin and LDL-C/HDL-C ratio in patients with coronary artery disease. Atherosclerosis. 2020;315: e253.
Manubolu VS, et al. Coronary computed tomography angiography evaluation of plaque morphology and its relationship to HDL and total cholesterol to HDL ratio. J Clin Lipidol. 2022;16(5):715–24.
Nam BH, Kannel WB, D’Agostino RB. Search for an optimal atherogenic lipid risk profile: from the Framingham Study. Am J Cardiol. 2006;97(3):372–5.
Kunutsor SK, et al. Is high serum LDL/HDL cholesterol ratio an emerging risk factor for sudden cardiac death? Findings from the KIHD study. J Atheroscler Thromb. 2017;24(6):600–8.
Sheng G, et al. Utility of non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio in evaluating incident diabetes risk. Diabetes Metab Syndr Obes. 2022;15:1677.
Acknowledgements
The authors sincerely appreciate the nursing team and administrative staff of Tehran Heart Center, who assisted us substantially in conducting this study.
Funding
This study was supported by the Tehran Heart Center.
Author information
Authors and Affiliations
Contributions
Conceptualization: FM, JB, AZ, Methodology: AJ, AS, AA, Validation: AJ, FM, Data analysis and interpretation: AJ, AA, Investigation: AA, AS, FM, Resources: FM, Data Curation: KA, MP, SS, Writing—Original Draft: AA, KA, Writing—Review & Editing: AA, AS, FM, Visualization: AJ, AA, Supervision: FM, KH, Project administration: FM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out following relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s). The study protocol has been approved by the board of research and the committee of medical ethics at Tehran University of Medical Sciences (code of ethics: IR.TUMS.MEDICINE.REC.1398.841).
Consent for publication
Not applicable.
Competing interests
All authors declare that there were no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ayati, A., Akbari, K., Shafiee, A. et al. Time-varying effect of postoperative cholesterol profile on long-term outcomes of isolated coronary artery bypass graft surgery. Lipids Health Dis 22, 163 (2023). https://doi.org/10.1186/s12944-023-01927-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-023-01927-8