Abstract
Objective
The purpose of this study was to comprehensively evaluate the lipid profiles in patients with juvenile idiopathic arthritis (JIA).
Methods
The literature and relevant reviews were searched for published clinical studies on the relationship between JIA and blood lipid levels. The Newcastle–Ottawa scale (NOS) was applied to evaluate the risk and methodological value of the included case‒control and cohort studies. Standardized mean differences (SMDs) and 95% confidence intervals were derived for all variables with adequate unprocessed data. This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.
Results
In total, 16 studies were incorporated through screening. The analysis findings revealed that the levels of very low-density lipoprotein cholesterol [SMD=-0.411, 95% CI (-0.774~-0.048), P = 0.026], high-density lipoprotein cholesterol [SMD=-0.528, 95% CI (-0.976~-0.079), P = 0.021], and apolipoprotein A1 [SMD=-1.050, 95% CI (-1.452~-0.647), P = 0.000] in JIA patients were statistically lower than those observed in healthy controls. The level of low-density lipoprotein cholesterol [SMD = 0.202, 95% CI (0.003 ~ 0.400), P = 0.046] was significantly higher in JIA patients than in healthy controls. In JIA patients, body mass index [SMD=-0.189, 95% CI (-0.690 ~ 0.311), P = 0.459], high-density lipoprotein [SMD =-1.235, 95% CI (-2.845 ~ 0.374), P = 0.133), low-density lipoprotein [SMD = 0.616, 95% CI (-0.813 ~ 2.046), P = 0.398), triglycerides (SMD = 0.278, 95% CI (-0.182 ~ 0.738), P = 0.236], total cholesterol [SMD=-0.073, 95% CI (-0.438 ~ 0.293), P = 0.696] and apolipoprotein B levels [SMD = 0.226, 95% CI (-0.133 ~ 0.585), P = 0.217] were not significantly different from those in healthy controls.
Conclusions
The outcomes of this meta-analysis suggest that dyslipidemia is common in JIA patients compared to healthy controls. Patients with JIA have a significantly increased risk of atherosclerosis and cardiovascular disease later in life.
Similar content being viewed by others
Introduction
Juvenile idiopathic arthritis (JIA) is a long-term rheumatic disorder that is mainly characterized by joint damage, which can be accompanied by multiple systemic systems [1]. The onset of the disease occurs before the age of 16 years, and the main feature of the disease is chronic synovitis [2]. Patients in advanced stages of the disease may experience complications such as impairment of the functions of the eyes, liver, spleen, and other organs and serious long-term health disorders, including physical disabilities [3]. The incidence of JIA ranges from 0.007 to 0.401%, affecting more females than males [4].
Much research evidence shows that long-term chronic inflammation affects lipid metabolism [5, 6]. The mechanism of dyslipidemia in JIA may be related to the chronic inflammatory process during the active phase of joint disease, the excessive release of some proinflammatory cytokines, and anti-rheumatic drug therapy [7]. Many studies [8,9,10] have demonstrated the presence of dyslipidemia in JIA patients during both acute and prolonged phases, yet findings across various investigations remain inconsistent. This study aims to measure and assess the existing research on lipid profiles in patients with JIA. The basic characteristics of dyslipidemia in JIA patients may preliminarily explore the mechanism of lipid metabolism disorder.
Methods
This analysis was carried out in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) regulations [11]. The protocol has been registered in PROSPERO (CRD42023445239).
Inclusion and exclusion criteria
The criteria for inclusion were as follows: (1) cohort studies, case‒control studies, or cross-sectional studies evaluating the relationship between serum lipid levels and JIA. The diagnosis of JIA was made according to the consensus conference of the International League of Associations for Rheumatology (ILAR) in 2001 or the American College of Rheumatology (ACR) in 1986. The control group was composed of healthy children. (2) Quantitative measurements of blood lipids and the total number of cases were provided in the article. (3) Studies were published in either Chinese or English.
The exclusion criteria were as follows: (1) duplicate studies; (2) research papers or conference abstracts that could not be procured online; and (3) reviews and case series.
Literature searches
Before designing the search strategy, the opinions of literature search experts were sought. From database establishment to July 15, 2023, under English and Chinese language restrictions, the MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature, and Web of Science databases were systematically searched. The MEDLINE search strategy (Table 1) was modified to facilitate its application in other databases. Further relevant research was identified by manually searching the bibliographies of excluded review articles.
Data extraction
To ensure the quality of this meta-analysis, strict treatment control was carried out in the research design, literature retrieval and screening, data extraction, and data entry processes. The papers were retrieved, and then the content and data that met the criteria were sorted. The extraction of variables and inputting of data were independently conducted by two research members (J.-H.D., W.-J.Z.) back to back to ensure the quality of data entry. Conflicting literature or data that were difficult to determine were resolved by consultation or with the assistance of a third researcher (C.-F.L).
Risk of bias (quality) assessment
The Newcastle–Ottawa scale (NOS) was applied to evaluate the risk and methodological value of the included case‒control and cohort studies [12]. The scale evaluates three research areas (selection criteria, comparability, and results) on a nine-point scoring system to indicate the level of quality achieved. To assess risk in the included cross-sectional surveys, the assessment standards were suggested by the Agency for Healthcare Research and Quality (AHRQ). Responses were evaluated as “Yes” (1 point), “No” (0 points), or “unclear” (0 points) [13]. A deviation risk table was created, and the research quality was summarized.
Data synthesis and statistical analysis
The statistical software Stata (version 14.2) was utilized for synthesizing data and statistical interpretation [14]. To assist in the synthesis process, data were compressed through a dual approach. First, although all relevant data in the research reports were extracted, the comprehensive report only contains the most exhaustive evidence for the lipid profiles in each paper. Second, a single-point value was estimated for each variable in every study, and the confidence interval was 95%. The indicators in this meta-analysis were the mean and standard deviation of TC, TG, HDL and LDL levels, which were continuous variables. The detection methods in each study were different or did not provide the detection methods, so the standardized mean difference (SMD) was used for data analysis. If zero events were reported for one group in a comparison, a value of 0.5 was added to both groups for each study. All tests were 2-tailed, and P < 0.05 was considered statistically significant. Where possible, before meta-analysis, the ordered classification data were transformed into a single estimation through the implementation of the generalized trend least-squares method, as facilitated by the Stata glst module [15]. A random-effects model was used to pool the data, and statistical heterogeneity between summary data was evaluated utilizing Cochran’s Q-test and Higgin’s I2 value [16]. When P > 0.1 and I2 < 50%, there was no statistical heterogeneity among the studies, and the fixed effect model method was used to calculate the SMD value. Conversely, when P ≤ 0.1 or I2 ≥ 50%, the presence of statistical heterogeneity necessitates the employment of a random effect model for calculating the SMD value. Begg’s test and Egger’s test were used to test publication bias. Sensitivity analysis was performed by recombining and analyzing individual studies one by one.
Results
Study characteristics
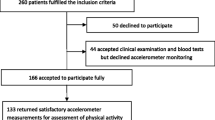
The literature search obtained 1894 unique database records. Most of the studies (1739) were eliminated during the initial screening process based on their titles and summaries. Out of the 155 full-text studies that were scrutinized, only 16 studies [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] satisfied the predetermined inclusion criteria (Fig. 1; Table 2). Table 2 details the 2 case‒control studies, 7 cohort studies, and 7 cross-sectional studies incorporated in this meta-analysis. In total, this study encompassed 1502 participants, comprising 639 individuals diagnosed with JIA and 863 healthy controls. Most of the JIA patients included in the study were female, accounting for an average of 64.31%.
Risk of bias
The incorporated papers exhibited varying degrees of quality, with scores ranging from five to eight. The scores were frequently downgraded due to the absence of independent verification of case status and insufficient follow-up measures (Tables 3, 4 and 5).
Body mass index (BMI)
A total of 11 studies [17,18,19, 22,23,24,25, 27, 29, 30, 32] surveyed the association between BMI and JIA. The heterogeneity result (P = 0.000, I2 = 92.9%) showed that there was a significant level of heterogeneity in the research literature, and the random effects model was employed for combined statistics. The results indicated a pooled SMD of -0.189, a 95% CI of -0.690 ~ 0.311, and a Z score of 0.74 (P = 0.459), suggesting no significant differences in BMI between JIA patients and healthy controls. To further analyze the sources of heterogeneity, sensitivity analysis was used to eliminate the studies one by one, and it was found that the analysis results were relatively robust. Subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design, and none of the results changed (Fig. 2; Table 6).
High-density lipoprotein (HDL)
A total of 6 studies [17, 20, 21, 26, 28, 29] surveyed the association between HDL and JIA. The heterogeneity result (P = 0.000, I2 = 98.0%) showed that there was a significant level of heterogeneity in the research literature, and the random effect model was employed for combined statistics. The results indicated a pooled SMD of -1.235, a 95% CI of -2.845 ~ 0.374, and a Z score of 1.50 (P = 0.133), suggesting no significant differences in HDL cholesterol between JIA patients and healthy controls. To further analyze the sources of heterogeneity, sensitivity analysis was used to eliminate the studies one by one, and it was found that the analysis results were relatively robust. Subgroup analyses were performed according to the study design, and none of the results changed (Fig. 3; Table 6).
Low-density lipoprotein (LDL) cholesterol
A total of 5 studies [17, 20, 21, 26, 28] surveyed the association between LDL cholesterol and JIA. The heterogeneity result (P = 0.000, I2 = 97.5%) shows that there was a significant level of heterogeneity in the research literature, and the random effect model was utilized for combined analysis. The results indicated a pooled SMD of 0.616, a 95% CI of -0.813 ~ 2.046, and a Z score of 0.84 (P = 0.398), suggesting no significant differences in LDL cholesterol levels between JIA patients and healthy controls. To further analyze the sources of heterogeneity, sensitivity analysis was used to eliminate the studies one by one, and it was found that the analysis results were relatively robust. Subgroup analyses were performed according to the study design, and none of the results changed (Fig. 4; Table 6).
Very low-density lipoprotein (VLDL) cholesterol
A total of 4 studies [17, 20, 21, 28] surveyed the association between VLDL cholesterol and JIA. The heterogeneity result (P = 0.043, I2 = 63.3%) showed that there was some homogeneity in the research literature, and the random effect model was implemented for combined statistics. The results indicated a pooled SMD of -0.411, a 95% CI of -0.774~-0.048, and a Z score of 2.22 (P = 0.026), suggesting that the VLDL cholesterol level of JIA patients was statistically less than that of healthy controls (Fig. 5; Table 6). To further analyze the sources of heterogeneity, sensitivity analysis was used to eliminate the studies one by one, and it was found that the analysis results were relatively robust. All four study designs were of the same type, so no subgroup analysis was conducted.
Triglyceride (TG)
A total of 11 studies [18,19,20,21,22, 26, 28,29,30,31,32] surveyed the association between TGs and JIA. The heterogeneity result (P = 0.000, I2 = 87.8%) showed that there was some homogeneity in the research literature, and the random effect model was employed for combined statistics. The results indicated a pooled SMD of 0.278, a 95% CI of -0.182 ~ 0.738, and a Z score of 1.18 (P = 0.236), suggesting no significant differences in TG levels between JIA patients and healthy controls. To further explore the potential sources of heterogeneity, subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design. Subgroup analyses were performed according to the study design. The results found significant differences in the case‒control study and no differences in the other types (Fig. 6; Table 6).
Total cholesterol (TC)
A total of 9 studies [17, 19, 20, 22, 26, 28, 30,31,32] surveyed the association between TC and JIA. The heterogeneity result (P = 0.000, I2 = 76.1%) showed that there was some homogeneity in the research literature, and the random effect model was utilized for combined statistics. The results indicated a pooled SMD of -0.073, a 95% CI of -0.438 ~ 0.293, and a Z score of 0.39 (P = 0.696), suggesting no significant differences in TC levels between JIA patients and healthy controls. To further explore the potential sources of heterogeneity, subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design. The results found significant differences in the case‒control study and no differences in the other types (Fig. 7; Table 6).
High-density lipoprotein cholesterol (HDL-C)
A total of 7 studies [18, 19, 22, 29,30,31,32] surveyed the association between HDL-C and JIA. The heterogeneity result (P = 0.000, I2 = 78.1%) showed that there was some homogeneity in the research literature, and the random effect model was implemented for combined statistics. The results indicated a pooled SMD of -0.528, a 95% CI of -0.976~-0.079, and a Z score of 2.31 (P = 0.021), suggesting that the HDL-C level of JIA patients was statistically lower than that of healthy controls. To further explore the potential sources of heterogeneity, subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design. The results found significant differences in the cohort studies and no differences in the other types (Fig. 8; Table 6).
LDL-C
A total of 7 studies [18, 19, 22, 29,30,31,32] surveyed the association between LDL-C and JIA. The heterogeneity result (P = 0.138, I2 = 38.1%) showed that there was little homogeneity in the research literature, and the fixed effect model was utilized for combined statistics. The results indicated a pooled SMD of 0.202, a 95% CI of 0.003 ~ 0.400, and a Z score of 1.99 (P = 0.046), suggesting that the LDL-C level of JIA patients was statistically higher than that of healthy controls. To further explore the potential sources of heterogeneity, subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design. The results found significant differences in the case‒control study and no differences in the other types (Fig. 9; Table 6).
Apolipoprotein (Apo)-A1
A total of 3 studies [22, 28, 29] surveyed the association between Apo-A1 and JIA. The heterogeneity result (P = 0.950, I2 = 0.0%) showed that there was little homogeneity in the research literature, and the fixed effect model was employed for combined statistics. The results indicated a pooled SMD of -1.050, a 95% CI of -1.452~-0.647, and a Z score of 5.11 (P = 0.000), suggesting that the Apo-A1 level of JIA patients was statistically inferior to that of healthy controls. To further explore the potential sources of heterogeneity, subgroup analysis was conducted on potential regulatory variables. Subgroup analyses were performed according to the study design, and none of the results changed (Fig. 10; Table 6).
Apo-B
A total of 3 studies [22, 28, 30] surveyed the association between Apo-B and JIA. The heterogeneity result (P = 0.361, I2 = 1.9%) showed that there was little homogeneity in the research literature, and the fixed effect model was employed for combined statistics. The results indicated a pooled SMD of 0.226, a 95% CI of -0.133 ~ 0.585, and a Z score of 1.23 (P = 0.217), suggesting no significant differences in Apo-B between JIA patients and healthy controls. Subgroup analyses were performed according to the study design, and none of the results changed (Fig. 11; Table 6).
Sensitivity analysis and publication bias test
Sensitivity analysis did not identify any studies that caused heterogeneity in this study, and the results of this study are stable and reliable (Fig. 12). Begg’s and Egger’s bias tests and funnel plots showed no obvious asymmetry, indicating that there was little publication bias in the selected studies (Figs. 13 and 14).
Discussion
The differences in serum lipid levels between the JIA and control groups were compared in this meta-analysis. In this meta-analysis of 16 trials involving 1502 participants, the results showed that the VLDL, HDL-C, and Apo-A1 levels in the JIA group were lower than those observed in the control group, and the LDL-C level in the JIA group was higher than that in the control group. There were no significant differences in BMI, HDL, LDL, TG, TC, and Apo-B between the JIA group and the control group.
In recent years, many studies have reported that compared with healthy children, children with JIA have blood fat metabolism disorders [33]. Current studies suggest that the inflammatory state and overexpression of proinflammatory cytokines caused by immune disorders in children with JIA at the active stage may lead to lipid metabolism disorders [34]. Chronic systemic inflammation in JIA patients can also induce changes in the structure and level of lipoproteins. Studies on dyslipidemia in children with JIA have shown different results. IIowite et al. [35] first described the changes in blood lipids in children with JIA, characterized by decreased HDL-C levels and increased TG and VLDL levels. In contrast, Gonvalves et al. [21], in a study of 51 children with JIA, found lower HDL-C levels and lower TG and VLDL levels in children with JIA than in healthy controls. Bohr et al. [36] reported that children with JIA had no obvious dyslipidemia, and TC, LDL-C, and HDL-C levels were within the normal range. However, Marangoni et al. [37] showed that plasma triglyceride, TC, and LDL-C levels were elevated and HDL-C levels were decreased in children with multiarticular JIA. This difference may be related to the JIA subtype and disease activity and to JIA treatment drugs. Glucocorticoids can increase the levels of all lipid components, while TNF-α antagonists and methotrexate may improve lipid metabolism [38].
VLDL is one of the plasma lipoproteins. VLDL may be related to physical activity and disease activity in JIA [39]. Some studies have shown that Apo-A1 is negatively related to JIA disease activity [40]. Apo-A1 can inhibit the activation of monocytes and macrophages and release interleukin-1, TNF-α, and other inflammatory factors [41]. In the process of inflammation in JIA, the level of SAA is significantly increased and replaces Apo-A1, resulting in a decrease in Apo-A1 [42].
Study strengths and limitations
The literature included in this study was all case‒control studies or cohort studies published in the last 30 years, and the NOS evaluation criteria were applied to score each study. The criteria for the diagnosis and exposure of JIA were clear in the included literature, so the bias caused by disease diagnosis errors and the determination and measurement errors of exposure factors was low. The funnel plot also suggested low publication bias.
This study, nonetheless, is not without its constraints. First, bibliographic bias occurs in the process of literature collection. The language scope of the included studies was restricted to Chinese and English; thus, valuable research published in various linguistic versions could not be retrieved or evaluated. Second, all the papers included have been previously published, and unpublished research results and documentary evidence from other nontraditional sources were lacking. The literature with “positive” results may overstate the strength of the association for some risk factors. An analysis of the causes showed that publication bias may be related to the failure to retrieve unpublished literature with negative results, database bias, etc. Due to publication bias, the results may exaggerate the association strength of a risk factor and deviate from the authenticity of JIA. Therefore, this conclusion is clinically relevant for reference. Finally, the included case‒control and cross-sectional studies were observational, and the strength of evidence was low. The quality assessment of the incorporated studies based on NOS and AHRQ evaluation criteria showed that the character of each study was different, and the assessment of some literature was low.
Conclusions
This review highlights studies of serum lipids in JIA. The outcomes of this meta-analysis suggest that dyslipidemia is common in JIA patients compared to healthy controls. The inflammatory status in JIA patients during the active phase of the disease or previous medication use may lead to lipid metabolism disorders. Patients with JIA have a significantly increased risk of atherosclerosis and cardiovascular disease later in life. Therefore, in clinical work, early intervention in lowering blood lipids can be performed on JIA patients with hyperlipidemia, thereby improving the prognosis and quality of life of patients. In future studies, it is still necessary to further analyze whether there is an interaction between different lipid indexes and to conduct a larger sample size population cohort study to explore the pathophysiological mechanism of lipid disorders in JIA.
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article.
Change history
08 September 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12944-023-01913-0
References
Angeles-Han ST, Ringold S, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the screening, monitoring, and treatment of Juvenile Idiopathic Arthritis-Associated Uveitis. Arthritis Care Res. 2019;71(6):703–16. https://doi.org/10.1002/acr.23871.
Mahmud SA, Binstadt BA. Autoantibodies in the pathogenesis, diagnosis, and prognosis of Juvenile Idiopathic Arthritis. Front Immunol. 2019;9:3168. https://doi.org/10.3389/fimmu.2018.03168.
Giancane G, Alongi A, Ravelli A. Update on the pathogenesis and treatment of juvenile idiopathic arthritis. Curr Opin Rheumatol. 2017;29(5):523–9. https://doi.org/10.1097/BOR.0000000000000417.
Concannon A, Reed P, Ostring G, Incidence. Clinical manifestations, and severity of Juvenile Idiopathic Arthritis among Maori and Pacific Island Children. Arthritis Care Res (Hoboken). 2019;71(9):1270–5. https://doi.org/10.1002/acr.23757.
Ringold S, Angeles-Han ST, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Care Res (Hoboken). 2019;71(6):717–34. https://doi.org/10.1002/acr.23870.
Poznyak A, Grechko AV, Poggio P, Myasoedova VA, Alfieri V, Orekhov AN. The diabetes Mellitus-Atherosclerosis connection: the role of lipid and glucose metabolism and chronic inflammation. Int J Mol Sci. 2020;21(5):1835. https://doi.org/10.3390/ijms21051835.
De Sanctis S, Marcovecchio ML, Gaspari S, Del Torto M, Mohn A, Chiarelli F, et al. Etanercept improves lipid profile and oxidative stress measures in patients with juvenile idiopathic arthritis. J Rheumatol. 2013;40(6):943–8. https://doi.org/10.3899/jrheum.121281.
Schulert GS, Yasin S, Carey B, Chalk C, Do T, Schapiro AH, et al. Systemic Juvenile Idiopathic Arthritis-Associated Lung Disease: characterization and risk factors. Arthritis Rheumatol. 2019;71(11):1943–54. https://doi.org/10.1002/art.41073.
Arsenaki E, Georgakopoulos P, Mitropoulou P, Koutli E, Thomas K, Charakida M, et al. Cardiovascular Disease in Juvenile Idiopathic Arthritis. Curr Vasc Pharmacol. 2020;18(6):580–91. https://doi.org/10.2174/1570161118666200408121307.
Rodrigues WDR, Sarni ROS, Fonseca FLA, Araújo A, Len CA, Terreri MT. Biomarkers of lipid metabolism in patients with juvenile idiopathic arthritis: relationship with disease subtype and inflammatory activity. Pediatr Rheumatol Online J. 2021;19(1):66. https://doi.org/10.1186/s12969-021-00538-w.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Norris JM, Simpson BS, Ball R, Freeman A, Kirkham A, Parry MA, et al. A modified Newcastle–Ottawa Scale for Assessment of Study Quality in genetic Urological Research. Eur Urol. 2021;79(3):325–6. https://doi.org/10.1016/j.eururo.2020.12.017.
Soffin EM, Gibbons MM, Ko CY, Kates SL, Wick E, Cannesson M, et al. Evidence review conducted for the Agency for Healthcare Research and Quality Safety Program for improving Surgical Care and Recovery: Focus on Anesthesiology for total knee arthroplasty. Anesth Analg. 2019;128(3):441–53. https://doi.org/10.1213/ANE.0000000000003564.
Daly C, Soobiah C. Software to Conduct a Meta-Analysis and Network Meta-Analysis. Methods Mol Biol. 2022;2345:223–44. https://doi.org/10.1007/978-1-0716-1566-9_14.
Vogelgesang F, Schlattmann P, Dewey M. The evaluation of bivariate mixed models in Meta-analyses of Diagnostic Accuracy Studies with SAS, Stata and R. Methods Inf Med. 2018;57(3):111–9. https://doi.org/10.1002/jrsm.1157.
Wessel JA, Danhof NA, van Eekelen R, Diamond MP, Legro RS, Peeraer K, et al. Ovarian stimulation strategies for intrauterine insemination in couples with unexplained infertility: a systematic review and individual participant data meta-analysis. Hum Reprod Update. 2022;28(5):733–46. https://doi.org/10.1097/AOG.0000000000003105.
Hussain KS, Gulati R, Satheesh S, Negi VS. Early-onset subclinical cardiovascular damage assessed by noninvasive methods in children with juvenile idiopathic arthritis: analytical cross-sectional study. Rheumatol Int. 2021;41(2):423–9. https://doi.org/10.1007/s00296-020-04689-z.
Jednacz E, Rutkowska-Sak L. Assessment of the body composition and parameters of the cardiovascular risk in juvenile idiopathic arthritis. Biomed Res Int. 2015;2015:619023. https://doi.org/10.1155/2015/619023.
Breda L, Di Marzio D, Giannini C, Gaspari S, Nozzi M, Scarinci A, et al. Relationship between inflammatory markers, oxidant-antioxidant status and intima-media thickness in prepubertal children with juvenile idiopathic arthritis. Clin Res Cardiol. 2013;102(1):63–71. https://doi.org/10.1007/s00392-012-0496-3.
Pugliese C, van der Vinne RT, Campos LM, Guardieiro PR, Saviolli C, Bonfá E, et al. Juvenile idiopathic arthritis activity and function ability: deleterious effects in periodontal disease? Clin Rheumatol. 2016;35(1):81–91. https://doi.org/10.1007/s10067-015-3125-5.
Gonçalves M, D’Almeida V, Guerra-Shinohara EM, Galdieri LC, Len CA, Hilário MO. Homocysteine and lipid profile in children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2007;5:2. https://doi.org/10.1186/1546-0096-5-2.
Tselepis AD, Elisaf M, Besis S, Karabina SA, Chapman MJ, Siamopoulou A. Association of the inflammatory state in active juvenile rheumatoid arthritis with hypo-high-density lipoproteinemia and reduced lipoprotein-associated platelet-activating factor acetylhydrolase activity. Arthritis Rheum. 1999;42(2):373–83. https://doi.org/10.1002/1529-0131(199902)42:2<373::AID-ANR21>3.0.CO;2-3.
Bos GJ, Lelieveld OT, Armbrust W, Sauer PJ, Geertzen JH, Dijkstra PU. Physical activity in children with juvenile idiopathic arthritis compared to controls. Pediatr Rheumatol Online J. 2016;14(1):42. https://doi.org/10.1186/s12969-016-0102-8.
Więch P, Sałacińska I, Bazaliński D, Dąbrowski M. Body composition and phase angle as an indicator of nutritional status in children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2018;16(1):82. https://doi.org/10.1186/s12969-018-0297-y.
Risum K, Edvardsen E, Selvaag AM, Dagfinrud H, Sanner H. Measurement properties and performance of an eight-minute submaximal treadmill test in patients with juvenile idiopathic arthritis: a controlled study. Pediatr Rheumatol Online J. 2019;17(1):14. https://doi.org/10.1186/s12969-019-0316-7.
Turoňová L, Kubejová K, Vorčáková K, Ďurdík P, Péčová T, Martinásková K. Endothelial dysfunction in children with Juvenile Psoriatic Arthritis. Acta Medica (Hradec Kralove). 2018;61(3):79–85. https://doi.org/10.14712/18059694.2018.122.
de Sousa Studart SA, Leite AC, Marinho AL, Pinto AC, Rabelo Júnior CN, de Melo Nunes R, et al. Vitamin D levels in juvenile idiopathic arthritis from an equatorial region. Rheumatol Int. 2015;35(10):1717–23. https://doi.org/10.1007/s00296-015-3287-0.
Bakkaloglu A, Kirel B, Ozen S, Saatçi U, Topaloğlu, Beşbaş N. Plasma lipids and lipoproteins in juvenile chronic arthritis. Clin Rheumatol. 1996;15(4):341–5. https://doi.org/10.1007/BF02230355.
Mani P, Uno K, Duong M, Wolski K, Spalding S, Husni ME, et al. HDL function and subclinical atherosclerosis in juvenile idiopathic arthritis. Cardiovasc Diagn Ther. 2016;6(1):34–43. https://doi.org/10.3978/j.issn.2223-3652.2015.12.14.
Aranda-Valera IC, Arias de la Rosa I, Roldán-Molina R, Ábalos-Aguilera MDC, Torres-Granados C, Patiño-Trives A, et al. Subclinical cardiovascular risk signs in adults with juvenile idiopathic arthritis in sustained remission. Pediatr Rheumatol Online J. 2020;18(1):59. https://doi.org/10.1186/s12969-020-00448-3.
Sun DM, Ding Y, Zhnag Y, Xia K. Serum lipid profile in children with different subtypes of juvenile idiopathic arthritis. Chin J Contemp Pediatr. 2019;21(6):547–51. https://doi.org/10.7499/j.issn.1008-8830.2019.06.009.
Shen CC, Yao TC, Yeh KW, Huang JL. Association of disease activity and anti-rheumatic treatment in juvenile idiopathic arthritis with serum lipid profiles: a prospective study. Semin Arthritis Rheum. 2013;42(6):590–6. https://doi.org/10.1016/j.semarthrit.2012.10.002.
Rochette E, Bourdier P, Pereira B, Echaubard S, Borderon C, Caron N, et al. Impaired muscular Fat Metabolism in Juvenile Idiopathic Arthritis in Inactive Disease. Front Physiol. 2019;10:528. https://doi.org/10.3389/fphys.2019.00528.
Skare TL, Silva MB, Negreiros P. Lipid profile in adult patients with idiopathic juvenile arthritis. Rev Bras Reumatol. 2013;53(4):371–4. https://doi.org/10.1590/S0482-50042013000400011.
Ilowite NT, Samuel P, Beseler L, Jacobson MS. Dyslipoproteinemia in juvenile rheumatoid arthritis. J Pediatr. 1989;114(5):823–6. https://doi.org/10.1016/s0022-3476(89)80148-9.
Bohr AH, Pedersen FK, Nielsen CH, Müller KG. Lipoprotein cholesterol fractions are related to markers of inflammation in children and adolescents with juvenile idiopathic arthritis: a cross sectional study. Pediatr Rheumatol Online J. 2016;14(1):61. https://doi.org/10.1186/s12969-016-0120-6.
Marangoni RG, Hayata AL, Borba EF, Azevedo PM, Bonfá E, Schainberg CG. Decreased high-density lipoprotein cholesterol levels in polyarticular juvenile idiopathic arthritis. Clin (Sao Paulo). 2011;66(9):1549–52. https://doi.org/10.1590/s1807-59322011000900007.
Rochette E, Bourdier P, Pereira B, Doré E, Birat A, Ratel S, et al. TNF blockade contributes to restore lipid oxidation during exercise in children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2019;17(1):47. https://doi.org/10.1186/s12969-019-0354-1.
Robinson GA, Peng J, Pineda-Torra I, Ciurtin C, Jury EC. Metabolomics defines complex patterns of dyslipidemia in Juvenile-SLE patients Associated with inflammation and potential Cardiovascular Disease Risk. Metabolites. 2021;12(1):3. https://doi.org/10.3390/metabo12010003.
Robinson GA, Waddington KE, Coelewij L, Peng J, Naja M, Wincup C, et al. Increased apolipoprotein-B:A1 ratio predicts cardiometabolic risk in patients with juvenile onset SLE. EBioMedicine. 2021;65:103243. https://doi.org/10.1016/j.ebiom.2021.103243.
Lipińska J, Lipińska S, Stańczyk J, Sarniak A, Przymińska vel Prymont A, Kasielski M, et al. Reactive oxygen species and serum antioxidant defense in juvenile idiopathic arthritis. Clin Rheumatol. 2015;34(3):451–6. https://doi.org/10.1007/s10067-014-2571-9.
van der Vorst EPC. High-density lipoproteins and apolipoprotein A1. Subcell Biochem. 2020;94:399–420. https://doi.org/10.1007/978-3-030-41769-7_16.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Wen-Jia Zhao and Jiang-Hong Deng were involved in the literature search, manuscript writing, and referencing. Cai-Feng Li was involved in conceptualization and editing. Both authors read and agreed on the final draft submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors have no relevant financial or nonfinancial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, WJ., Deng, JH. & Li, CF. Lipid profiles in patients with juvenile idiopathic arthritis: a systematic literature review and meta-analysis. Lipids Health Dis 22, 136 (2023). https://doi.org/10.1186/s12944-023-01885-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-023-01885-1