Abstract
Background
Stroke represents the second most prevalent contributor to global mortality. The Chinese Visceral Adiposity Index (CVAI) serves as an established metric for assessing visceral adiposity in the Chinese population, exhibiting prognostic capabilities. This investigation aimed to explore the association of CVAI and new-onset stroke among middle-aged and older Chinese populations.
Methods
The study employed data from the 2011 and 2018 China Health and Retirement Longitudinal Study (CHARLS) to assess the association of CVAI and the incidence of new-onset stroke. Utilizing a directed acyclic graph (DAG), 10 potential confounders were identified. Moreover, to explore the association between CVAI and new-onset stroke, three multifactor logistic regression models were constructed, accounting for the identified confounders and mitigating their influence on the findings.
Results
The study comprised 7070 participants, among whom 417 (5.9%) experienced new-onset strokes. After controlling for confounding variables, regression analysis suggested that the new-onset stroke’s highest risk was linked to the fourth quartile (Q4) of the CVAI, with an odds ratio (OR) of 2.33 and a 95% confidence interval (CI) of 1.67–3.28. The decision tree analysis demonstrated a heightened probability of new-onset stroke among hypertensive individuals with a CVAI equal to or greater than 83, coupled with a C-reactive protein level no less than 1.1 mg/l. Age seemed to have a moderating influence on the CVAI and new-onset stroke association, exhibiting a more prominent interaction effect in participants under 60 years.
Conclusions
In middle-aged and older Chinese populations, a linear relationship was discerned between CVAI and the probability of new-onset stroke. CVAI provides a predictive framework for stroke incidence in this demographic, laying the groundwork for more sophisticated risk prediction models that improve the precision and specificity of stroke risk evaluations.
Similar content being viewed by others
Background
Stroke is one of the most prevalent cerebrovascular disease, encompassing both ischemic and hemorrhagic types. Stroke, arising from organic brain injuries, is defined by its abrupt onset and the quick emergence of either localized or diffuse brain function impairments. Globally, stroke ranks as the second most common cause of mortality and a principal factor in morbidity [1]. The United States and Japan report estimated annual incidences of approximately 795,000 and 191,000 new-onset and recurrent strokes, respectively [2]. In China, approximately two million new-onset stroke cases occur annually, exhibiting an 8.7% growth rate [3]. Although age-standardized mortality and Disability-Adjusted Life Year (DALY) rates for stroke have declined, the global burden of disease (GBD) estimates reveal an increase in overall incidence and crude stroke burden rates between 1990 and 2019 [4]. Consequently, stroke presents a significant public health challenge and imposes a considerable financial strain on individuals and society. Prior studies have identified hypertension, diabetes, atrial fibrillation, dyslipidemia, visceral obesity, smoking, and advanced age as factors associated with an elevated risk of new-onset stroke [5,6,7,8]. Proactive management and mitigation of these risk factors can substantially reduce stroke incidence.
Visceral obesity represents a global health issue, with World Health Organization data indicating that over 40% of adults worldwide are overweight, while 13% are classified as obese [9, 10]. China is home to an estimated 89.6 million obese individuals [11], constituting the largest obese population globally. Standard indices employed to evaluate adipose tissue encompass hip girth, adipose tissue proportion, and the waist-height ratio [12]. However, these indices independently fail to provide a comprehensive assessment of visceral adipose distribution. Xia et al. [13] developed the Chinese visceral adiposity index (CVAI) based on the visceral adiposity index (VAI) and incorporated body mass index (BMI), age, high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), and Waist circumference (WC) to better reflect visceral fat characteristics in the Chinese population. Existing research [14] suggests that CVAI functions as a potent and credible measure of visceral adipose tissue dysregulation.
In recent years, the prognostic utility of CVAI has gained increasing interest in numerous studies. Xie et al. [15] proposed that CVAI might function as a substantial prognosticator of cardiometabolic risk in adults experiencing growth hormone deficiency, facilitating the recognition of potential cardiovascular ailments and vascular occurrences. Han et al. [16] documented a positive correlation between CVAI and the susceptibility to type 2 diabetes mellitus, while Chen et al. [17] posited that CVAI might assist in diagnosing non-alcoholic fatty liver disease. However, limited research has examined the direct relationship between CVAI and new-onset stroke. Although previous investigations [18, 19] have explored the association between VAI and stroke incidence, VAI calculations were based on equations established for Caucasian populations. CVAI, due to considerable differences in body fat distribution across ethnic groups [20], is better suited for Chinese populations. CVAI is posited to influence the onset of cerebrovascular diseases, like stroke, potentially through mechanisms such as dyslipidemia and insulin resistance. Given that inflammation and thrombosis are key players in stroke pathogenesis, we hypothesize that higher CVAI may affect the incidence of new strokes. Consequently, as a China-specific metabolic marker, CVAI holds significance in predicting new-onset stroke.
Drawing upon the publicly available China Health and Retirement Longitudinal Study (CHARLS) database [21], this investigation delved into the association between CVAI and new-onset stroke among middle-aged and older Chinese individuals, in addition to assessing the predictive utility of CVAI for stroke incidence.
Methodological approaches and materials
Investigated cohort
Data for this cohort investigation were procured from CHARLS (http://charls.pku.edu.cn/). The study utilized baseline information gathered in 2011 and follow-up data from 2018. CHARLS, an open-access resource, is a continuous, nationally representative cohort study encompassing participants aged 45 years and above from over 400 villages and communities within 25 provinces, districts, and cities. The database compiles a plethora of information, including personal, familial, financial, health, employment, and neighborhood data. The primary objective is to amass high-quality microdata that typifies middle-aged and older Chinese households, thereby assessing the nation’s aging population. The dataset from CHARLS categorizes individuals aged 45 years and beyond as middle-aged and elderly, a classification that aligns with the United Nations’ definition of older adults as being 60 years and above [22,23,24,25], in line with previous studies [26]. This investigation strictly adhered to relevant CHARLS guidelines and recommendations.
Prior to the survey, participants willingly signed informed consent forms. Of the 17,707 respondents in the 2011 baseline survey, each provided fasting blood samples, underwent baseline physical examinations, and completed questionnaires. Subsequently, 10,683 participants were excluded based on the following criteria: age under 45 years (n = 423), lipid-lowering drug usage history (n = 904), incomplete CVAI data (n = 7520), unavailable stroke information in the 2011 wave (n = 23), unavailable stroke information in the 2018 wave (n = 1708), and stroke presence at baseline (n = 105) (Fig. 1).
Measurement
Assessment of the CVAI
The CVAI amalgamates anthropometric and functional parameters, providing insight into visceral adipose tissue distribution. CVAI computation employed the subsequent formula [16]:
Evaluation of new-onset strokes
Incidence of new-onset stroke was evaluated by inquiring respondents, “Have you ever been diagnosed with a stroke by a doctor?” and “When did you first discover the condition?” If an affirmative response was provided during the follow-up, and the participant had not reported a stroke in the baseline survey but did so during the follow-up, they were deemed to have experienced a new-onset stroke [27].
Assessment of potential confounders
Covariates considered in the directed acyclic graph (DAG) encompassed age, sex, marital status, education, location, smoking, drinking, low-density lipoprotein cholesterol (LDL-C), BMI, WC, diabetes, hypertension, HDL-C, TG, and C-reactive protein (CRP). These covariates were classified into socio-demographic characteristics, health-related behaviors, and anthropometric measurements. Socio-demographic attributes were classified into five categories: age, sex, educational attainment (primary school or below, middle school, and high school or above), residential location (urban and rural), and marital status (married and unpartnered). Health-related behaviors encompassed four classifications: smoking status (non-smoker, former smoker, and current smoker), as well as alcohol consumption habits (none, less than once a month, and more than once a month). Anthropometric measurements, such as TG, BMI, HDL-C, CRP, LDL-C, and WC, were obtained using standardized techniques [21, 28]. Waist circumference was measured utilizing a specific protocol with the following steps: First, we utilized a non-elastic tape measure as our equipment. Participants were instructed to stand upright, their feet positioned shoulder-width apart, and arms relaxed, perpendicular to the body. The waist circumference was gauged using the tape measure without clothing, at the level of the navel. While the participant was breathing calmly, the investigator fastened the measuring tape snugly around the body without compressing the skin and read the measurement to two decimal places at the end of the participant’s exhalation. This process was repeated thrice, and the average of these three measurements was recorded as the final result. All measurement instruments were appropriately calibrated to guarantee an error margin of less than 0.5 cm in waist circumference measurements. Comprehensive methodologies are accessible on the CHARLS website (http://charls.pku.edu.cn/).
In this study, a DAG [29, 30] was employed to select a minimally sufficient set of confounding variables (Fig. 2). DAG execution was facilitated by dagitty.net [31]. Given that age, WC, BMI, TG, and HDL-C were already incorporated in the CVAI equation, they were not adjusted for in the regression model. Through the DAG, relevant adjustment factors and eliminated confounding variables were identified, thereby minimizing bias in the final model’s estimated association between CVAI and new-onset stroke. Adjusted variables encompassed sex, marital status, education, location, smoking, drinking, diabetes, hypertension, LDL-C, and CRP levels.
Statistical analysis
For non-normally distributed data, medians and quartiles (Q1–Q3) were computed, while categorical variables were expressed as proportions. Baseline characteristics and CVAI were stratified according to the presence or absence of new-onset stroke. Data comparisons were conducted using the t-test, Mann–Whitney U, and Chi-square test, as appropriate. In order to evaluate the odds ratio (OR) and 95% confidence interval (CI) of new-onset stroke in relation to CVAI as continuous (per interquartile range [IQR] increment) or categorical (quartiles) variables, three logistic regression models were implemented: Model 1 depicted crude associations between CVAI and new-onset stroke; Model 2 incorporated further adjustments for sex, educational attainment, residential location, and marital status; Model 3 encompassed adjustments from Model 2, alongside health behavior and disease history factors, such as smoking status, alcohol consumption habits, LDL-C, CRP, and hypertension and diabetes histories.
A restricted cubic splines (RCS) analysis incorporating three knots at the 10th, 50th, and 90th percentiles of CVAI was undertaken to investigate potential linear associations and illustrate dose–response relationships between CVAI and new-onset stroke. Interaction analyses were carried out independently to evaluate moderating influences among socio-demographic characteristics and health-related behaviors in the connection between CVAI and new-onset stroke. Models integrated multiplicative interaction terms, and likelihood-ratio tests were conducted to appraise the interaction. Furthermore, a decision tree was utilized to examine the predictive merit of CVAI.
All statistical evaluations were performed utilizing R 4.1. The ‘ANOVA’ function within the rms R package enabled RCS analysis. The decision tree construction employed the ‘rpart’ package. A two-tailed P-value less than 0.05 denoted statistical significance in the analysis.
Results
Baseline attributes
Table 1 presents participant characteristics. The study encompassed a total of 7,070 individuals (median age: 58 years; 3,158 males: 45%; 3,912 females: 55%), among which 417 (5.9%) experienced new-onset strokes, while the rest remained healthy. The baseline median (IQR) CVAI for participants was 93.9 (64.1–124.4). Notably, CVAI was substantially elevated in individuals with new-onset stroke compared to healthy counterparts. Distinct characteristics were observed among participants with new-onset stroke; they exhibited a higher likelihood of being older, residing unaccompanied, being former smokers, having hypertension and diabetes, while exhibiting higher BMI, WC, TG, CRP, and LDL-C levels, and displaying lower HDL-C levels (P < 0.05).
Dose–response association of CVAI and new-onset stroke
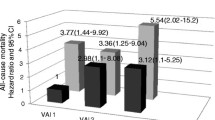
Table 2 delineates the correlation between the incidence of novel stroke events and CVAI quartiles. The analysis revealed a significant escalation in stroke risk concomitant with elevated CVAI quartiles after accounting for confounding factors such as sex, marital status, LDL-C, smoking habits, CRP, hypertension history, geographical location, alcohol consumption, educational background, and diabetes prevalence (P for trend < 0.001, OR: 2.33, 95% CI: 1.67–3.28). Moreover, Q4 exhibited the most pronounced susceptibility to novel stroke occurrences in comparison to Q1. CVAI demonstrated a marked association with the emergence of new stroke cases. Upon assessment as a continuous variable, evidence suggested a 57% surge in stroke risk for each IQR increment in CVAI (OR: 1.57, 95% CI: 1.34–1.84). Figure 3 portrays the linear dose-response relationship between CVAI and novel stroke risk (P overall < 0.001, P nonlinear = 0.562). The investigation determined a progressive augmentation in stroke risk, concomitant with a consistent elevation in CVAI. The CVAI threshold of 94.1 emerged as a determinant of novel stroke events.
Association of CVAI and the risk of new-onset stroke utilizing the adjusted cubic spline model. The model accounts for confounding factors, including sex, educational background, geographical location, marital status, smoking habits, alcohol consumption, LDL-C, and CRP, as well as histories of hypertension and diabetes. The graphical representation demonstrates a linear association of CVAI and the hazard of new-onset stroke. CVAI, Chinese Visceral Adiposity Index; LDL-C, low-density lipoprotein cholesterol; CRP, C-reactive protein
Decision tree analysis of CVAI for new-onset stroke
To appraise the prognostic utility of CVAI, we conducted a decision tree analysis incorporating demographic and clinicopathological features of new-onset stroke occurrences (Fig. 4). The resultant model demonstrated an accuracy of 84%. The analysis revealed a heightened stroke risk in hypertensive individuals presenting with CVAI ≥ 83 and CRP ≥ 1.1 mg/l.
Stratified analysis
The aforementioned DAG facilitated the identification of pertinent adjustment factors, thereby eradicating confounding variables, which in turn mitigated bias in estimating the association between CVAI and the new-onset stroke in the final model. The considered covariates for adjustment included demographic and behavioral factors such as sex [32], marital status [33], educational attainment [34, 35], geographic location [36], smoking habits [37], and alcohol consumption [38], along with diseases history like presence of diabetes [39], hypertension [40], LDL-C [41, 42], and CRP levels [43].
Figure 5 displays the outcomes of the stratified analysis. Participants were segregated into distinct subgroups based on specific characteristics to ascertain potential variations in the interaction effect of CVAI on new-onset stroke incidence across diverse subpopulations. The findings indicated that age could serve as a moderating factor in the relationship between CVAI and new stroke events (P for interaction < 0.05). Notably, among individuals below 60 years of age, each IQR increment in CVAI corresponded to a 72% elevated stroke risk (OR: 1.72, 95% CI: 1.37–2.15). Conversely, participants exceeding 60 years of age exhibited a 42% elevated risk (OR: 1.42, 95% CI: 1.12–1.78).
Stratified analysis assessing the interaction effect of CVAI on new-onset stroke incidence across varied subgroups. The forest plot reveals that age may exert moderating influences on the correlation between CVAI and new-onset stroke occurrences (P for interaction < 0.05). CVAI, Chinese Visceral Adiposity Index
Incremental prognostic value of CVAI
Table 3 demonstrates that incorporating CVAI into the fundamental model significantly enhanced the C-statistic for novel stroke incidence prediction. This integration led to substantial improvements in both continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI), increasing by 0.260 and 0.005, respectively (P < 0.001).
Discussion
This prospective cohort study investigated the association of CVAI and new-onset stroke in middle-aged and older Chinese individuals. Upon adjustment for pertinent confounders, an IQR elevation in CVAI was associated with a 57% augmented risk of incident stroke (OR: 1.57, 95% CI: 1.34–1.83). The dose–response analysis showed a linear association of CVAI and the hazard of new-onset stroke.
This research reveals that CVAI can predict the hazard of new-onset stroke among middle-aged and older Chinese adults. In comparison to other indices (TyG-WC, TyG, LAP, TyG-BMI, and VAI) (P < 0.001), CVAI had the largest area under the receiver operating characteristic curve (0.674) and may be the most accurate predictor of new-onset stroke, consistent with the findings of Yang et al. [44]. However, their study population was predominantly rural Chinese, whereas this study population was drawn from a nationally representative cohort comprising 450 villages in 150 districts across 28 provinces. A recent study reported that the incidence of new-onset stroke and related risk factors vary between rural and urban locations in developing countries [45]. A decision tree analysis was also conducted to explore the predictive value of CVAI. A stratified analysis was conducted to determine the interaction effect of CVAI on new-onset stroke in various subgroups.
Smoking is one of the major risk factors for stroke. As shown in Table 1, the ‘sick quitter’ effect [46] might explain the findings, namely, the higher proportion of ex-smokers and lower proportion of current smokers in the stroke patient cohort. The phenomenon known as the ‘sick quitter’ effect [47] suggests that the emergence of health-threatening symptoms in a smoker, prior to the onset of a stroke, can prompt cessation of smoking. Although these participants have ceased smoking, their previous history put them at a higher risk of stroke, thereby the higher proportion of ex-smokers compared to current smokers.
In the adjusted cubic spline model, CVAI was linearly linked to the risk of new-onset stroke (P overall < 0.001, P nonlinear = 0.562). Visceral obesity is a significant risk factor for new-onset strokes. These findings are consistent with previous studies demonstrating that visceral obesity leads to deep white matter lesions through increased pro-inflammatory cytokines [48]. Higher waist-to-hip ratio (WHR) and BMI result in an elevated deep-to-periventricular white matter hyperintensities ratio through elevated interleukin-6, which can increase the likelihood of stroke occurrence. This dose–response curve also revealed that the hazard of new-onset stroke gradually increased with a constant increase in CVAI, highlighting the importance of maintaining CVAI at a suitable level.
Visceral adipose tissue is essential for energy and nutritional metabolism. A recent Mendelian randomization study [49] provided potential evidence for a causal role of visceral adipose tissue in new-onset stroke. However, it also releases inflammatory cytokines and chemokine mediators that contribute to the formation of carotid plaques and elevate the likelihood of new-onset stroke [50]. According to a study by Bi et al. [51], CVAI demonstrated a positive association with the propensity for carotid plaque development. As components of the CVAI formula, a previous large-scale prospective study discovered that WC was positively linked with the risk of subarachnoid and cerebral hemorrhages. In contrast, BMI exhibited an inverse correlation with the likelihood of ischemic cerebrovascular events and intracranial hemorrhage [52]. The results underscore the significance of accounting for visceral adipose tissue when assessing the risk of incident stroke, emphasizing the intricate interplay among BMI, WC, and diverse stroke classifications.
In the present investigation, the decision tree analysis forecasted that hypertensive individuals exhibiting CVAI values ≥ 83, coupled with CRP concentrations ≥ 1.1 mg/l, possess an elevated probability of experiencing a new-onset stroke. This conclusion is consistent with recent findings in the literature. Hypertension constitutes a considerable risk determinant for the emergence of new-onset stroke, as reported by Bangalore et al. [53]. Hypertension also increases the burden of cardiovascular and cerebrovascular diseases [54] and can lead to severe complications, with new-onset stroke being the most common. The decision tree analysis demonstrated a heightened probability of new-onset stroke among hypertensive individuals with a CVAI equal to or greater than 83, coupled with a CRP level no less than ≥ 1.1 mg/l. This result align with those of prior research [55, 56], reaffirming the significant prognostic value of CRP across a spectrum of diseases. As a crucial marker of inflammation in the body, CRP demonstrates a distinct association with both the incidence and prognosis of stroke [57], thus substantiating its role in the prediction and management of this disease; Consequently, individuals falling within the predicted range should engage in ongoing preventive management to control blood pressure, such as self-measurement, and adopt proactive preventive measures to reduce the likelihood of new-onset stroke.
Furthermore, a stratified analysis was executed to explore the association of CVAI and new-onset stroke across different subgroups. The stratified analysis suggested that age could potentially modulate the relationship between CVAI and new-onset stroke (P for interaction < 0.1). Notably, a more pronounced interaction effect of CVAI on new-onset stroke emergence was observed in individuals below 60 years of age. This observation might be attributable to the prevalent incidence of ectopic fat deposits in older participants (> 60 years), which is exacerbated by factors such as positive energy balance, obesity, diabetes, and the reallocation of adipose tissue from subcutaneous to visceral regions [58, 59]. This suggests that the effect of CVAI on new-onset stroke is diminished in patients over 60 years of age, highlighting the significance of age in CVAI equations. Compared to a previous study that examined the association between stroke incidence and VAI, CVAI adds the age indicator to its equation to provide a more comprehensive analysis of visceral adiposity in the Chinese population [19, 20]. According to the latest projections by Yao et al. [60], the burden of stroke in the Chinese population over 65 years will significantly increase by 2050, with a projected increase of 104.7% in incidence, 218.5% in prevalence, and 100% in mortality. With the growing aging population and the apparent increase in the burden of new-onset stroke, adequate attention should be given to healthcare and secondary prevention of new-onset stroke in older adults. In order to effectively reduce the incidence of stroke among individuals over the age of 60, it is crucial to adopt multifaceted measures. These measures encompass lifestyle modifications, regular health surveillance, management of concurrent medical conditions, and potentially, societal health initiatives that address wider determinants of health influencing stroke risk. It is essential to manage factors beyond CVAI to effectively mitigate the rise in stroke incidence attributable to an aging population.
Comparative analysis with prior investigations and contributions to the extant knowledge base
This research stands in contrast to prior investigations by focusing on the associations between the CVAI and new-onset stroke occurrence in middle-aged and older Chinese adults. While previous studies have examined adiposity indices in relation to stroke risk, the present investigation uniquely emphasizes the relevance of CVAI as a culturally specific and demographically sensitive predictor.
Furthermore, this research paves the way for future inquiries into the utility of CVAI in predicting stroke and other health outcomes in distinct populations. Ultimately, the findings presented here serve to enhance the precision and specificity of stroke risk assessments, taking into account the unique cultural and demographic characteristics of the Chinese population.
Strengths and limitations
The primary strength of this study lies in its use of the CHARLS database, which provided access to a large sample cohort obtained through multi-stage probability sampling from multiple regions. Additionally, a DAG was implemented to select the minimum sufficient set of confounding variables and identify relevant adjustment factors to reduce bias in the approximated relationship of CVAI and new-onset stroke in the final model. Moreover, the current study provides innovative findings to the extant body of knowledge regarding the correlations between the CVAI and the incidence of novel strokes in middle-aged and elderly Chinese individuals, utilizing an observational research approach. These advancements encompass: a) delineating a linear association between CVAI and the likelihood of new-onset stroke occurrence, b) underscoring the potential utility of CVAI as a prognostic instrument for stroke incidence, and c) laying the groundwork for the creation of sophisticated risk prediction frameworks, consequently augmenting the precision and specificity of stroke risk evaluations in this demographic.
However, some limitations should be considered. First, this study was unable to distinguish between types of stroke, such as hemorrhagic or ischemic stroke. Further research is necessary to investigate the association between CVAI and specific stroke types. Second, some of the information utilized in this study, such as information on new-onset strokes, was obtained through standardized questionnaires, which may be subject to information or memory bias [61]. Third, observational analyses may be subject to potential bias and confounding factors. Thus, the causal association between CVAI and new-onset stroke cannot be determined from this study alone. Further genetic investigations, such as a Mendelian randomization design, are necessary to establish the causal relationship. Lastly, several unmeasured potential confounders, such as individual occupation, family status, and socioeconomic status, may have influenced the relationship between CVAI and new-onset stroke through other interacting factors. Furthermore, in the CHARLS database, stroke patients lacked imaging information at the time of onset, and there were a considerable number of participants with missing CVAI data. Finally, this study utilized baseline data from 2011, disregarding alterations in the Chinese Visceral Adiposity Index (CVAI) between 2011 and 2018 due to the unavailability of necessary parameters to compute the 2018 CVAI in the CHARLS database.
Conclusions
This study found a linear relationship of CVAI and the risk of new-onset stroke within the middle-aged and senior Chinese demographic, with CVAI supplying a predictive scope for stroke initiation. Moreover, the interaction effect of CVAI on new-onset stroke events was more pronounced in participants under 60 years of age relative to those surpassing 60 years. Consequently, hypertensive individuals in the middle-aged and older categories presenting with elevated CVAI should emphasize the prevention of new-onset stroke.
The clinical relevance of this study lies in its potential to guide healthcare professionals in identifying middle-aged and older Chinese adults at a higher risk of new-onset stroke due to increased CVAI. By understanding this association, clinicians can develop more targeted prevention and intervention strategies, focusing on reducing visceral adiposity to mitigate stroke risk in this population. From a future perspective, these findings can serve as a foundation for the development of more refined risk prediction models, incorporating the CVAI alongside other established risk factors. By enhancing the accuracy and specificity of stroke risk assessments, such models could help optimize resource allocation and tailor preventive measures to those most in need, ultimately improving patient care and reducing the burden of stroke in this population.
Availability of data and materials
The dataset supporting the conclusions of this article are available in the CHARLS database repository, [at http://charls.pku.edu.cn]. To download the data, approval from the CHARLS team is required.
Abbreviations
- CVAI:
-
Chinese Visceral Adiposity Index
- CHARLS:
-
China Health and Retirement Longitudinal Study
- Q4:
-
Quartile group
- DALY:
-
Disability-Adjusted Life Year
- GBD:
-
Global burden of disease
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- BMI:
-
Body mass index
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- VAI:
-
Visceral adiposity index
- DAG:
-
Directed acyclic graph
- CRP:
-
C-reactive protein
- LDL-C:
-
Low-density lipoprotein cholesterol
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- RCS:
-
Restricted cubic spline
- IQR:
-
Interquartile range
- NRI:
-
Net reclassification improvement
- IDI:
-
Integrated discrimination improvement
References
Jolugbo P, Ariëns RAS. Thrombus composition and efficacy of thrombolysis and thrombectomy in acute ischemic stroke. Stroke. 2021;52:1131–42.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56-528.
Zhang T, Zhao J, Li X, Bai Y, Wang B, Qu Y, et al. Chinese Stroke Association guidelines for clinical management of cereb rovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. 2020;5:250–9.
Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6:e897-906.
Lopez-Garcia E, Rodriguez-Artalejo F, Rexrode KM, Logroscino G, Hu FB, van Dam RM. Coffee consumption and risk of stroke in women. Circulation. 2009;119:1116–23.
Diener H-C, Hankey GJ. Primary and secondary prevention of ischemic stroke and cerebral hemorrhage. J Am Coll Cardiol. 2020;75:1804–18.
Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201:1380–8.
Mujaj B, Bos D, Muka T, van der Lugt A, Ikram MA, Vernooij MW, et al. Antithrombotic treatment is associated with intraplaque haemorrhage in the atherosclerotic carotid artery: a cross-sectional analysis of The Rotterdam Study. Eur Heart J. 2018;39:3369–76.
Sommer I, Teufer B, Szelag M, Nussbaumer-Streit B, Titscher V, Klerings I, et al. The performance of anthropometric tools to determine obesity: a systematic review and meta-analysis. Sci Rep. 2020;10(1):1–2.
Secor JD, Fligor SC, Tsikis ST, Yu LJ, Puder M. Free fatty acid receptors as mediators and therapeutic targets in liver disease. Front Physiol. 2021;12:656441.
Ye P, Xi Y, Huang Z, Xu P. Linking obesity with colorectal cancer: epidemiology and mechanistic insights. Cancers (Basel). 2020;12:1408.
Rana S, Bhatti AA. Predicting anthropometric and metabolic traits with a genetic risk sco re for obesity in a sample of Pakistanis. Sci Rep. 2021;11:8320.
Xia M-F, Chen Y, Lin H-D, Ma H, Li X-M, Aleteng Q, et al. A indicator of visceral adipose dysfunction to evaluate metabolic heal th in adult Chinese. Sci Rep. 2016;6:38214.
Zhao L, Zhu C, Chen Y, Chen C, Cheng J, Xia F, et al. LH/FSH ratio is associated with visceral adipose dysfunction in Chinese women older than 55. Front Endocrinol. 2018;9:419.
Xie X, Li Q, Zhang L, Ren W. Lipid accumulation product, visceral adiposity index, and Chinese visceral adiposity index as markers of cardiometabolic risk in adult growth hormone deficiency patients: a cross-sectional study. Endocr Pract. 2018;24:33–9.
Han M, Qin P, Li Q, Qie R, Liu L, Zhao Y, et al. Chinese visceral adiposity index: a reliable indicator of visceral fat function associated with risk of type 2 diabetes. Diabetes Metab Res Rev. 2021;37:e3370.
Chen X, Shi F, Xiao J, Huang F, Cheng F, Wang L, et al. Associations between abdominal obesity indices and nonalcoholic fatty liver disease: Chinese visceral adiposity index. Front Endocrinol (Lausanne). 2022;13:831960.
Cui C, He C, Sun Q, Xu Z, Li Q, Yue S, et al. Association between visceral adiposity index and incident stroke: data from the China Health and Retirement Longitudinal Study. Nutr Metab Cardiovasc Dis. 2022;32:1202–9.
Chen Q, Zhang Z, Luo N, Qi Y. Elevated visceral adiposity index is associated with increased stroke prevalence and earlier age at first stroke onset: based on a national cross-sectional study. Front Endocrinol. 2023;13:1086936.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33:920–2.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–8.
Alzahrani ZA, Alghamdi KA, Almaqati AS. Clinical characteristics and outcome of COVID-19 in patients with rheumatic diseases. Rheumatol Int. 2021;41:1097–103.
Attafuah PYA, Amertil N, Sarfo JO, Deegbe DA, Nyonator D, Amponsah-Boama C, et al. ‘I decided to attend to him because it’s my duty’: student Nurses perception and attitude towards care of older adults. BMC Med Educ. 2022;22:23.
Aoki K, Nakamura H, Suzuki H, Matsuo K, Kataoka K, Shimamura T, et al. Prognostic relevance of genetic alterations in diffuse lower-grade gliomas. Neuro Oncol. 2018;20:66–77.
Ye P, Er Y, Wang H, Fang L, Li B, Ivers R, et al. Burden of falls among people aged 60 years and older in mainland China, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6:e907–18.
Deng Y, Gao Q, Yang T, Wu B, Liu Y, Liu R. Indoor solid fuel use and incident arthritis among middle-aged and older adults in rural China: a nationwide population-based cohort study. Sci Total Environ. 2021;772:145395.
Yuan X, Liu T, Wu L, Zou Z-Y, Li C. Validity of self-reported diabetes among middle-aged and older Chinese adults: the China Health and Retirement Longitudinal Study. BMJ Open. 2015;5:e006633.
Chen X, Crimmins E, Hu PP, Kim JK, Meng Q, Strauss J, et al. Venous blood-based biomarkers in the China health and retirement longitudinal study: rationale, design, and results from the 2015 wave. Am J Epidemiol. 2019;188:1871–7.
Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10:37–48.
Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70.
Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745.
Gibson CL. Cerebral ischemic stroke: is gender important? J Cereb Blood Flow Metab. 2013;33:1355–61.
Andersen KK, Olsen TS. Stroke case-fatality and marital status. Acta Neurol Scand. 2018;138:377–83.
Xiuyun W, Qian W, Minjun X, Weidong L, Lizhen L. Education and stroke: evidence from epidemiology and Mendelian randomization study. Sci Rep. 2020;10:21208.
Che B, Shen S, Zhu Z, Wang A, Xu T, Peng Y, et al. Education level and long-term mortality, recurrent stroke, and cardiovascular events in patients with ischemic stroke. J Am Heart Assoc. 2020;9:e016671.
Bejot Y, Benatru I, Rouaud O, Fromont A, Besancenot JP, Moreau T, et al. Epidemiology of stroke in Europe: geographic and environmental differences. J Neurol Sci. 2007;262:85–8.
Larsson SC, Burgess S, Michaëlsson K. Smoking and stroke: a mendelian randomization study. Ann Neurol. 2019;86:468–71.
Larsson SC, Wallin A, Wolk A, Markus HS. Differing association of alcohol consumption with different stroke types: a systematic review and meta-analysis. BMC Med. 2016;14:178.
Lau L-H, Lew J, Borschmann K, Thijs V, Ekinci EI. Prevalence of diabetes and its effects on stroke outcomes: a meta-analysis and literature review. J Diabetes Investig. 2019;10:780–92.
Buonacera A, Stancanelli B, Malatino L. Stroke and hypertension: an appraisal from pathophysiology to clinical practice. Curr Vasc Pharmacol. 2019;17:72–84.
Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316:1289–97.
Xu J, Hao X, Zhan R, Jiang X, Jin A, Xue J, et al. Effect of Lipoprotein(a) on stroke recurrence attenuates at low LDL-C (low-density lipoprotein) and inflammation levels. Stroke. 2022;53:2504–11.
Zhou Y, Han W, Gong D, Man C, Fan Y. Hs-CRP in stroke: a meta-analysis. Clin Chim Acta. 2016;453:21–7.
Zhao Y, Zhang J, Chen C, Qin P, Zhang M, Shi X, et al. Comparison of six surrogate insulin resistance indexes for predicting the risk of incident stroke: the Rural Chinese Cohort Study. Diabetes Metab Res. 2022;38. Available from: https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3567. Cited 2022 Dec 23.
Howard G, Kleindorfer DO, Cushman M, Long DL, Jasne A, Judd SE, et al. Contributors to the excess stroke mortality in rural areas in the United States. Stroke. 2017;48:1773–8.
Rimm E. Commentary: alcohol and coronary heart disease—laying the foundation for future work. Int J Epidemiol. 2001;30:738–9.
Park J, Yoon JH, Ki HK, Han K, Kim H. Lifestyle changes and risk of tuberculosis in patients with type 2 diabetes mellitus: a nationwide cohort study. Front Endocrinol (Lausanne). 2022;13:1009493.
Lampe L, Zhang R, Beyer F, Huhn S, Kharabian Masouleh S, Preusser S, et al. Visceral obesity relates to deep white matter hyperintensities via inflammation. Ann Neurol. 2019;85:194–203.
Xu R, Hu X, Wang T, Yang Y, Jiang N, Luo J, et al. Visceral adiposity and risk of stroke: a Mendelian randomization study. Front Neurol. 2022;13:804851.
Williams MD, Nadler JL. Inflammatory mechanisms of diabetic complications. Curr Diab Rep. 2007;7:242–8.
Bi H, Zhang Y, Qin P, Wang C, Peng X, Chen H, et al. Association of Chinese visceral adiposity index and its dynamic change with risk of carotid plaque in a large cohort in China. J Am Heart Assoc. 2022;11:e022633.
Pillay P, Lewington S, Taylor H, Lacey B, Carter J. Adiposity, body fat distribution, and risk of major stroke types among adults in the United Kingdom. JAMA Netw Open. 2022;5:e2246613.
Bangalore S, Schwamm L, Smith EE, Hellkamp AS, Suter RE, Xian Y, et al. Blood pressure and in-hospital outcomes in patients presenting with ischaemic stroke. Eur Heart J. 2017;38:2827–35.
Jamaladin H, van de Belt TH, Luijpers LC, de Graaff FR, Bredie SJ, Roeleveld N, et al. Mobile apps for blood pressure monitoring: systematic search in app stores and content analysis. JMIR Mhealth Uhealth. 2018;6:e187.
Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2006;113:e873-923.
Lunetta C, Lizio A, Maestri E, Sansone VA, Mora G, Miller RG, et al. Serum C-reactive protein as a prognostic biomarker in amyotrophic lateral sclerosis. JAMA Neurol. 2017;74:660–7.
Hakoupian M, Ferino E, Jickling GC, Amini H, Stamova B, Ander BP, et al. Bacterial lipopolysaccharide is associated with stroke. Sci Rep. 2021;11:6570.
Zamboni M, Rossi AP, Fantin F, Zamboni G, Chirumbolo S, Zoico E, et al. Adipose tissue, diet and aging. Mech Ageing Dev. 2014;136–137:129–37.
Kuk JL, Saunders TJ, Davidson LE, Ross R. Age-related changes in total and regional fat distribution. Ageing Res Rev. 2009;8:339–48.
Yao M, Ren Y, Jia Y, Xu J, Wang Y, Zou K, et al. Projected burden of stroke in China through 2050. Chin Med J (Engl). 2022. https://doi.org/10.1097/CM9.0000000000002060.
Tang W, Huang W, Lu H, Cao B, Wu D, Ong J, et al. What happens after HIV self-testing? Results from a longitudinal cohort of Chinese men who have sex with men. BMC Infect Dis. 2019;19:807.
Acknowledgements
We would like to express gratitude to the CHARLS team for providing the data necessary for this study. Additionally, we thank the participants of CHARLS for their valuable contribution to the survey.
Funding
This study was supported by the General Project of the Torch Program of the Fourth Affiliated Hospital of Harbin Medical University (HYDSYHJ201902) and the Special Support Project of the Fourth Affiliated Hospital of Harbin Medical University (HYDSYTB202232).
Author information
Authors and Affiliations
Contributions
HZ analyzed and interpreted the patient data, was a major contributor in writing the manuscript. QZ drew figures. JY drew tables. FD participated in writing part of the manuscript. SZ polished the article. YG download the data from the database. JG was responsible for the calculation of statistics. HF finished the study design. FZ drew tables. XG participated in writing part of the manuscript. XW directed the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The CHARLS was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and all procedures were performed following the guidelines outlined in the Declaration of Helsinki. Furthermore, the Human Research Ethics Committee of Newcastle University granted ethical approval for the utilization of CHARLS data in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, H., Zhan, Q., Dong, F. et al. Associations of Chinese visceral adiposity index and new-onset stroke in middle-aged and older Chinese adults: an observational study. Lipids Health Dis 22, 74 (2023). https://doi.org/10.1186/s12944-023-01843-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-023-01843-x