Abstract
Purpose
Retinol-binding protein 4 (RBP4) has been considered to be related to metabolic related diseases, such as hyperuricemia, obesity, and diabetes mellitus. However, whether nonalcoholic fatty liver disease (NAFLD) is related to RBP4 is unclear. Previous studies on the relationship between NAFLD and RBP4 levels have yielded inconsistent results. Hence, this meta-analysis was aimed to clarify whether circulating RBP4 levels are in relation to the risk of NAFLD.
Methods
A meta-analysis was performed by applying observational studies to evaluate circulating RBP4 levels and NAFLD. Eligible studies published up to September 23, 2022, were searched in Embase, PubMed, and Cochrane databases.
Results
In this study, 17 cross-sectional studies involving 8423 participants were included. Results from a random effects model showed that circulating RBP4 levels were higher in NAFLD patients than non-NAFLD (standardized mean difference (SMD) 0.28; 95% confidence intervals (CI): 0.11–0.46, I2: 89.8%). This association was confirmed in the Yellow race. However, no significant association was noted in the Caucasian race. After excluding the morbidly obese Population from the weight loss study (n = 2), the results of the comparison remained largely unchanged (SMD 0.28; 95% CI: 0.10–0.47, I2: 90.8%). Remarkable publication bias was not found. Although considerable heterogeneity was observed among the studies, no potential sources of heterogeneity were found in the subgroup analysis. Diagnostic methods for NAFLD were determined to be a potential source of statistical heterogeneity in meta-regression.
Conclusion
The findings provide evidence that NAFLD patients exhibit higher levels of circulating RBP4 compared with controls, but high heterogeneity was observed. Thus, a high RBP4 level is probably a potential risk factor for NAFLD. To confirm the causal link between NAFLD and RBP4 level of causality, further prospective cohort studies are needed.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a major public health issue impacting about one quarter of the global population [1] and its prevalence is predicted to grow to 56% in the next decade [2]. NAFLD, including simple steatosis (SS) and non-alcoholic steatohepatitis (NASH) that can develop into cirrhosis and hepatocellular carcinoma (HCC) [3, 4], is closely related to metabolic syndrome. Existing research suggests that NAFLD may not only progress to intrahepatic diseases, such as hepatocellular carcinoma, but is also closely related to extrahepatic diseases, such as cardiovascular disease, obesity, diabetes, and hyperuricemia [5]. Hence, treating NAFLD is imperative.
Retinol binding protein 4 (RBP4) is a 21 kDa protein belonging to the Lipocalin family and is the only known particular transporter protein for vitamin A, which regulates the circulating levels of retinol [6]. RBP4 is primarily synthesized and released from the adipose and the liver [7], and it is an adipokine that plays a vital role in growth, vision and metabolic diseases [8]. Free RBP4 has a low molecular weight and is generally bound to transthyretin in a 1:1 ratio in the circulation to keep it from filtration by the glomerulus of the kidney [9].
Till date, the etiology and pathogenesis of NAFLD has not been fully elucidated. Numerous studies have indicated that it involves an intricate interaction among obesity, environmental factors, microbiota changes, and susceptibility gene variants [10,11,12,13,14,15]. These interactions lead to disturbed lipid homeostasis and excessive accumulation of lipidic substances, such as triglycerides, in hepatocytes [16]. Of these, insulin resistance (IR) is the core mechanism. Serum RBP4 has been reported to be elevated in animal models of IR. In some human studies, a positive correlation has been observed among obese adults between RBP4 levels and fasting glucose and homoeostasis model assessment of insulin resistance (HOMA-IR) [17, 18]. Therefore, NAFLD and RBP4 levels may be correlated. However, there has been inconsistencies regarding the relationship between the two. A previous meta-analysis [19] dating back to 2017 suggests that the two are not correlated, but numerous studies have been published after that. In this research, new studies were included to ensure an updated meta-analysis and systematic review.
Methods
This meta-analysis is registered on prospero (ID: CRD42022362281).
Search strategy
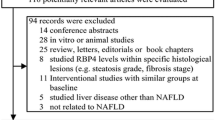
Two independent reviewers (Rui Hu and Xiaoyue Yang) applied the subject terms “non-alcoholic fatty liver disease” and “retinol binding protein 4” and their corresponding free words in the Embase, PubMed, and Cochrane database for studies published before September 23, 2022. Without setting any language restrictions, all potentially eligible studies were included. In addition, the review articles and reference lists in the relevant original studies were examined to search for other potentially eligible researches. Based on the search strategy, all literature collected was independently assessed by two authors (Rui Hu and Xiaoyue Yang). They were both blinded to each other’s records and sought out potentially eligible studies. Any issues raised were addressed through discussion with the fourth author, Guangyao Song. A flow chart depicting the literature selection methodology is given in Fig. 1.
Inclusion and exclusion criteria
Inclusion criteria: (1) observational researches involving humans; (2) age ≥ 18 years; (3) studies involving measurement of the circulating RBP4 levels in NAFLD and non-NAFLD patients.
Exclusion criteria: Past studies wherein the participants had liver injury due to infectious factors (such as hepatitis B or hepatitis C virus), total parenteral nutrition, alcohol use, drug use, or genetic causes. After excluding these articles, those with insufficient data or those studies that did not include non-NAFLD population were excluded.
Data extraction
Two researchers (Rui Hu and Xiaoyue Yang) used a specially designed form extracted the independently the necessary data. Any discrepancies were resolved by discussion or by involving a fourth reviewer (Guangyao Song) whenever deemed necessary. The extracted data included the publication year, first author’s name, the design of study, participants’ characteristics (age, the number of females, race, and body mass index [BMI]), NAFLD diagnosis methods, and the technique of measuring RBP4. To sought the missing details, the appropriate person was contacted.
Quality assessment
Two researchers (Rui Hu and Xiaoyue Yang) assessed the extracted researches. The modified Newcastle–Ottawa Quality Assessment Scale (NOS) [20] was applied to evaluate the study quality. Low quality studies were defined as less than 3 points, moderate quality studies as 4–6 and high-quality studies as 7–9.
Statistical analyses
Stata14.0 software was applied to conduct all statistical analyses. The standardized mean difference (SMD) was applied to evaluate the study outcomes. In addition, the mean ± standard deviation (SD) was expressed as the normally distributed data. Considering the potential for significant heterogeneity between the enrolled studies, this meta-analysis opted for a more conservative random-effects model. Two-tailed P-value was extracted in this meta-analysis.
Using Q and I2 statistics, the heterogeneity was evaluated. For Q statistics and I2 statistics, P < 0.10 and I2 < 50% was considered as statistical significance. An I2 values of 25% was poor heterogeneity, 50 and 75% represented medium and high heterogeneities, respectively [21].
Through subgroup analyses, the influence of the potential factors on the correlation was assessed, which included ethnicity, the method of diagnosing NAFLD, and the method of measuring the RBP4 levels. In addition, possible sources of heterogeneity were analyzed using meta-regression.
The stability of the outcomes was evaluated for sensitivity analyses by removing individual studies. In addition, Egger’s, Begg’s tests, and funnel plot were applied to assess the publication bias.
Results
Literature search
The initial literature search resulted in the identification of 597 articles. After removing 87 duplicates and 467 irrelevant articles, 43 articles remained. After full text screening, 28 articles were excluded because of disagreement with the eligibility criteria listed in Fig. 1. Finally, 17 studies were pooled, all of which were cross-sectional studies.
Research characteristics
The features of the studies included in this article were shown in Table 1. In brief, 8432 subjects, including 3989 patients with NAFLD and 4443 healthy controls were involved in these 17 studies. Of these, nine studies had a predominantly Caucasian race and eight studies had a predominantly Yellow race. In all studies, 15 studies used enzyme-linked immunosorbent assay to determine RBP4 levels and 2 studies used immunoturbidimetric assay to determine RBP4 levels. Of the 17 studies, 11 studies employed the abdominal ultrasound technique to determine NAFLD, 5 used liver biopsy, and 1 study combined the two methods. Serum RBP4 levels, number of (female) subjects, age, and BMI levels were reported.
Quality evaluation
A modified NOS scale was used to assess the quality of the included studies. As presented in Table 1, of all studies, 15 were evaluated to be of moderate quality, 1 of high quality, and 1 of low quality.
Statistical results
A random effects meta-analysis was conducted on the 17 studies included in this article. The results showed that serum RBP4 levels was higher in NAFLD patients than non-NAFLD (SMD 0.28; 95% CI: 0.11–0.46, I2: 89.8%, P = 0.001) (Fig. 2).
Subgroup analysis
To examine whether differences in ethnicities (Caucasian, Yellow race) could be the source of the high subgroup analysis was conducted according to the different ethnicities included in the study. As shown in Fig. 3, Yellow ethnic patients with NAFLD presented notably higher circulating RBP4 levels than non-NAFLD (SMD0.49; 95% CI: 0.34–0.65; P = 0.001). However, circulating RBP4 levels in Caucasian NAFLD patients were not statistically different from those of healthy controls (SMD0.01; 95% CI. -0.40–0.43; P = 0.949). Nevertheless, there remained a high level of heterogeneity in the comparison between Yellow (I2 = 84.9%; P = 0.000) and Caucasian (I2 = 89.7%; P = 0.000) populations.
Next, based on the diagnostic method of NAFLD, subgroup analysis was performed. In the subgroup with abdominal ultrasound as the diagnostic method, NAFLD patients had remarkably higher circulating RBP4 levels than those non-NAFLD (SMD 0.48; 95% CI. 0.34–0.65; P = 0.000). However, in the subgroup with liver biopsy as a diagnostic method, patients with NAFLD had no statistically significant difference in circulating RBP4 levels compared to non-NAFLD (SMD -0.38; 95% CI: − 1.02–0.25; P = 0.235). These results suggest that the circulating RBP4 was higher in patients with abdominal ultrasound as a diagnostic method than in controls. (Fig. 4).
Sensitivity analysis and meta-regression
One study was found to exert a remarkable effect on the deviations in RBP4 levels between patients with NAFLD and without in sensitivity analysis (Fig. 5). Hence, this article was removed, and a new meta-analysis of the remaining 16 studies was conducted. The results indicated that NAFLD patients had higher circulating RBP4 levels than non-NAFLD (SMD 0.25; 95% CI: 0.06–0.45, I2: 88.8%, P = 0.011) (Fig. 6). Furthermore, after excluding the weight loss study (n = 2), only a small change was noted in the comparison between NAFLD patients and without NAFLD (SMD 0.42; 95% CI: 0.38–0.47; P = 0.000) (Fig. 7).
In the meta-regression analysis (Table 2), the diagnostic method of NAFLD may be a potential source of high heterogeneity (univariate meta-regression: P = 0.002; multivariate meta-regression: P = 0.024).
Publication bias
Given the subjective nature of funnel plots, we performed an analysis of publication bias using the Egger test and confirmed the absence of publication bias (P = 0.217) (Figs. 8, 9, 10).
Discussion
In this meta-analysis, higher levels of circulating RBP4 were found in NAFLD patients compared to non-NAFLD, although heterogeneity between the combined studies was significant. The findings of a previous meta-analysis (SMD = 0.08, 95% CI: − 0.21 to 0.38, P > 0.05) disagree with the results of this one [19]. However, the broader population and the higher number of participants in the present study might have improved the consistency of the results. Several studies have investigated the relationship between RBP4 levels and NAFLD but have reported varying results. In 3389 individuals with and without NAFLD, a positive connection between circulating RBP4 levels and NAFLD development was observed after 3.09 years of follow-up [Odds ratio (95% CI) for the development of NAFLD (three-digit: 2.01, (1.33, 3.04)] [35]. In contrast, another research showed that circulating RBP4 levels had no relation with the development of NAFLD, as confirmed with liver biopsy [26]. Thus, the results are conflicting, which could be attributed to the differences in diagnostic methods (e.g. abdominal ultrasound and liver biopsy), age, sex composition and sample size. Furthermore, studies that reported serum RBP4 to be an independent risk factor for NAFLD were all conducted in Yellow racial populations, whereas those in Western countries mostly reached opposite conclusions, which may be related to ethnic variability. Therefore, the relationship between RBP4 levels and NAFLD and its severity must be elucidated in larger clinical studies.
The mechanism by which RBP4 causes NAFLD progression remains unclear. Liu [39] found via animal experiments that the overexpression of RBP4 could aggravate liver mitochondrial dysfunction and promote steatosis in mice by impairing the oxidative capacity of the liver mitochondria, thereby suggesting that RBP4 is a possible target for liver fat accumulation. Moreover, IR may be one of the critical mechanisms by which NAFLD is associated with RBP4. As an important mechanism of NAFLD occurrence, IR could result in the impairment of the ability of adipocytes to store fat, leading to the release of free fatty acids into the bloodstream, which promotes hepatic lipid deposition and exacerbating the development of NAFLD [40]. However, the relationship between RBP4 and IR is controversial, and the first strong link between RBP4 and IR was demonstrated by Yang [7]. The researcher discovered that circulating RBP4 levels were correlated with the degree of IR in patients, including obese patients, impaired glucose tolerance patients, and type 2 diabetics as well in normal participants with a family history of these diseases. A subsequent study showed that in obese and type 2 diabetic patients, circulating RBP4 level was positively related to metabolic syndrome and IR [41]. Additionally, recent studies have indicated that circulating RBP4 levels were related to IR in people with hyperuricemia [42]. Other studies [27, 43] have arrived at the opposite conclusion, but in these studies, HOMA-IR was used to assess IR rather than the orthoglucose clamp assay, which is the golden standard for assessment. Furthermore, RBP4 is also strongly related to inflammation, and the progression of inflammation in the liver is a factor that influences the advancement of NAFLD because it exacerbates the transformation of simple steatosis into steatohepatitis [16].
In this meta-analysis, high heterogeneity between studies was found when performing subgroup analyses. Moreover, meta-regression suggested that the diagnostic method of NAFLD may be a potential source of heterogeneity. After subgroup analysis based on the diagnostic method of NAFLD, the heterogeneity reduced slightly. Nonetheless, there were no remarkable differences in NOS scores, patient age, sex, measurement method, or diagnostic methods for NAFLD before and after the exclusion of outliers; hence, these results are robust. During the measurement of RBP4 level, only some studies grouped the values according to the severity of NAFLD, Zhou [19] did not find differences in RBP4 levels among the three groups based on a two-by-two comparison of SS, NASH, and control groups. Furthermore, there have been no new studies have since then to compare the RBP4 levels between the three groups. Therefore, the severity of NAFLD could possibly affect the final results.
Genetic variants in the I148Met allele of PNPLA3 and the 167Lys allele of TM6SF2 have been shown to be strongly linked to the increase in hepatic fat deposition and the development of cirrhosis and hepatocellular carcinoma [44]. Additionally, some studies [45, 46] have shown a correlation between serum RBP4 levels and renal insufficiency and that NAFLD is associated with reduced glomerular filtration rate and/or microalbuminuria [47]. Only a few of the included studies specified the glomerular filtration rate and urinary microalbumin values; some studies included these with renal insufficiency as an exclusion criterion, but some studies were not rigorously controlled. Furthermore, one study [34] showed that circulating RBP4 levels were lower in premenopausal NAFLD women than in postmenopausal NAFLD women. This finding implies that serum RBP4 levels could be affected by the menopausal status and that estrogen deficiency may adjust the circulating RBP4 levels downward.
Strengths and limitations
The current meta-analysis including 17 clinical researches has a larger sample size than previous meta-analyses and includes literature from a wider region, including Asia, Europe, and Africa [33,34,35, 37, 38].
However, some limitations are present. First, all the included studies were cross-sectional studies, and the causal relationship between RBP4 levels and NAFLD could not be established. Second, although the indicators of circulating RBP4 levels were converted to the same units, the values varied from one study to the other. For patients with NAFLD, the highest RBP4 level was 94.6 μg/mL [36], whereas the lowest was only 0.69 μg/mL [30]. This variation may be related to the differences in the assay methods and experimental kits. Third, the results showed some heterogeneity, which could be ascribed to diet, varying proportions of the diabetic population, etc. In addition, all studies were subject to bias, and although some studies had controlled for factors such as age and sex, many unexpected factors may still exist. Studies have shown that the diagnostic methods for NAFLD may be a source of heterogeneity, but the application of liver biopsy as a diagnostic method for NAFLD has been less well studied, which inevitably has certain deviations. Fourth, although RBP4 belongs to the lipid family and is closely related to IR, HOMA-IR has not been covered in most articles [24, 36,37,38]. Thus, it is impossible to perform reasonable subgroup analysis and meta-regression based on HOMA-IR. Finally, according to the subgroup analysis, the circulating RBP4 levels in the Yellow racial NAFLD population were different from those in the normal population of the same race. However, this discrepancy was not observed in the White race, which might be because of the inclusion of articles mainly from the Yellow race. Therefore, whether the results would be applicable to other ethnicities is uncertain. More data on other ethnicities are, hence, needed to draw comprehensive conclusions.
Conclusions
Patients with NAFLD exhibited higher levels of RBP4 than healthy controls. Hence, RBP4 may be an emerging noninvasive biomarker for NAFLD. In addition, RBP4-targeting agents can be considered for the treatment of this disease.
Availability of data and materials
Within the article and its supplementary files.
References
Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, et al. Global epidemiology of nonalcoholic fatty liver disease:meta-analytic assessment of prevalence, incidence, and outcomes. J Gastroenterol Hepatol. 2016;31:936–44.
Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18:223–38.
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–21.
White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012;10:1342–1359 e1342.
Targher G, Tilg H, Byrne CD. Non-alcoholic fatty liver disease: a multisystem disease requiring a multidisciplinary and holistic approach. Lancet Gastroenterol Hepatol. 2021;6:578–88.
O'Byrne SM, Blaner WS. Retinol and retinyl esters: biochemistry and physiology. J Lipid Res. 2013;54:1731–43.
Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature. 2005;436:356–62.
Fasshauer M, Bluher M. Adipokines in health and disease. Trends Pharmacol Sci. 2015;36:461–70.
Folli C, Viglione S, Busconi M, Berni R. Biochemical basis for retinol deficiency induced by the I41N and G75D mutations in human plasma retinol-binding protein. Biochem Biophys Res Commun. 2005;336:1017–22.
Kawaguchi T, Sumida Y, Umemura A, Matsuo K, Takahashi M, Takamura T, et al. Genetic polymorphisms of the human PNPLA3 gene are strongly associated with severity of non-alcoholic fatty liver disease in Japanese. PLoS One. 2012;7:e38322.
Li Z, Ye CY, Wang L, Li JM, Yang L. Association of Genetic and Environmental Factors with non-alcoholic fatty liver disease in a Chinese Han population. Int J Environ Res Public Health. 2020;17:null.
Loomba R, Seguritan V, Li W, Long T, Klitgord N, Bhatt A, et al. Gut microbiome-based metagenomic signature for non-invasive detection of advanced fibrosis in human nonalcoholic fatty liver disease. Cell Metab. 2017;25:1054–1062.e1055.
Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World j gastroentero. 2014;20:9330–7.
Peng XE, Wu YL, Lin SW, Lu QQ, Hu ZJ, Lin X. Genetic variants in PNPLA3 and risk of non-alcoholic fatty liver disease in a Han Chinese population. PLoS One. 2012;7:e50256.
Tsai MC, Liu YY, Lin CC, Wang CC, Wu YJ, Yong CC, Chen KD, Chuah SK, Yao CC, HuangPY, et al. Gut Microbiota Dysbiosis in Patients with Biopsy-Proven Nonalcoholic Fatty Liver Disease: A Cross-Sectional Study in Taiwan. Nutrients. 2020;12(3):820.
Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65:1038–48.
Bremer AA, Devaraj S, Afify A, Jialal I. Adipose tissue dysregulation in patients with metabolic syndrome. J Clin Endocrinol Metab. 2011;96:E1782–8.
Wang X, Huang Y, Gao J, Sun H, Jayachandran M, Qu S. Changes of serum retinol-binding protein 4 associated with improved insulin resistance after laparoscopic sleeve gastrectomy in Chinese obese patients. Diabetol Metab Syndr. 2020;12:7.
Zhou Z, Chen H, Ju H, Sun M. Circulating retinol binding protein 4 levels in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Lipids Health Dis. 2017;16(1):180.
van Dijk GM, Maneva M, Colpani V, Dhana K, Muka T, Jaspers L, et al. The association between vasomotor symptoms and metabolic health in peri- and postmenopausal women: a systematic review. Maturitas. 2015;80:140–7.
Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–6.
Seo JA, Kim NH, Park SY, et al. Serum retinol-binding protein 4 levels are elevated in non-alcoholic fatty liver disease. Clin Endocrinol. 2008;68(4):555–60.
Wu H, Jia W, Bao Y, et al. Serum retinol binding protein 4 and nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2008;79(2):185–90.
Kashyap SR, Diab DL, Baker AR, Yerian L, Bajaj H, Gray-McGuire C, et al. Triglyceride levels and not adipokine concentrations are closely related to severity of nonalcoholic fatty liver disease in an obesity surgery cohort. Obesity (Silver Spring). 2009;17:1696–701.
Koh JH, Shin YG, Nam SM, Lee MY, Chung CH, Shin JY. Serum adipocyte fatty acid-binding protein levels are associated with nonalcoholic fatty liver disease in type 2 diabetic patients. Diabetes Care. 2009;32(1):147–52.
Milner KL, van der Poorten D, Xu A, Bugianesi E, Kench JG, Lam KS, et al. Adipocyte fatty acid binding protein levels relate to inflammation and fibrosis in nonalcoholic fatty liver disease. Hepatology. 2009;49:1926–34.
Schina M, Koskinas J, Tiniakos D, Hadziyannis E, Savvas S, Karamanos B, et al. Circulating and liver tissue levels of retinol-binding protein-4 in non-alcoholic fatty liver disease. Hepatol Res. 2009;39:972–8.
Cengiz C, Ardicoglu Y, Bulut S, Boyacioglu S. Serum retinol-binding protein 4 in patients with nonalcoholic fatty liver disease: does it have a significant impact on pathogenesis? Eur J Gastroenterol Hepatol. 2010;22(7):813–9.
Auguet T, Terra X, Porras JA, et al. Plasma visfatin levels and gene expression in morbidly obese women with associated fatty liver disease. Clin Biochem. 2013;46(3):202–8.
Polyzos SA, Kountouras J, Anastasilakis AD, Geladari EV, Mantzoros CS. Irisin in patients with nonalcoholic fatty liver disease. Metabolism. 2014;63:207–17.
Suh JB, Kim SM, Cho GJ, Choi KM. Serum AFBP levels are elevated in patients with nonalcoholic fatty liver disease. Scand J Gastroenterol. 2014;49(8):979–85.
Chen X, Shen T, Li Q, et al. Retinol binding Protein-4 levels and non-alcoholic fatty liver disease: a community-based cross-sectional study. Sci Rep. 2017;7:45100.
Cai H, Lu S, Chen Y, Das Mbbs Mrcog S, Niu Z, Zhuo G, et al. Serum retinol binding protein 4 and galectin-3 binding protein as novel markers for postmenopausal nonalcoholic fatty liver disease. Clin Biochem. 2018;56:95–101.
El-Ashmawy HM, Ahmed AM. Serum fetuin-B level is an independent marker for nonalcoholic fatty liver disease in patients with type 2 diabetes. Eur J Gastroenterol Hepatol. 2019;31:859–64.
Wang X, Chen X, Zhang H, Pang J, Lin J, Xu X, et al. Circulating retinol-binding protein 4 is associated with the development and regression of non-alcoholic fatty liver disease. Diabetes Metab. 2020;46:119–28.
İkizek M, Kasapoğlu B, Türkay C. Investigation of adiponectin, leptin, retinol binding protein-4 and resistin levels in non-diabetic and non-obese patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol Res. 2020;9:3275–82.
Hassan HAAH, Dawood DS, Hussein RJ. Relationship between g3bp and r4bp with some biochemical parameters in iraqi patients with nonalcoholic fatty liver disease. Medico-Legal Update. 2021;21:299–307.
Zhang ZH, Ke JF, Lu JX, Liu Y, Wang AP, Li LX. Serum retinol-binding protein levels are associated with nonalcoholic fatty liver disease in Chinese patients with type 2 diabetes mellitus: a real-world study. Diabetes Metab J. 2022;46:129–39.
Liu Y, Mu D, Chen H, Li D, Song J, Zhong Y, et al. Retinol-binding protein 4 induces hepatic mitochondrial dysfunction and promotes hepatic steatosis. J Clin Endocrinol Metab. 2016;101:4338–48.
Asrih M, Jornayvaz FR. Metabolic syndrome and nonalcoholic fatty liver disease: is insulin resistance the link? Mol Cell Endocrinol. 2015;418(Pt 1):55–65.
Graham TE, Yang Q, Blüher M, Hammarstedt A, Ciaraldi TP, Henry RR, et al. Retinol-binding protein 4 and insulin resistance in lean, obese, and diabetic subjects. New Engl J Med. 2006;354:2552–63.
Liu C, Zhou XR, Ye MY, Xu XQ, Zhang YW, Liu H, et al. RBP4 is associated with insulin resistance in hyperuricemia-induced rats and patients with hyperuricemia. Front Endocrinol (Lausanne). 2021;12:653819.
Chavez AO, Coletta DK, Kamath S, Cromack DT, Monroy A, Folli F, et al. Retinol-binding protein 4 is associated with impaired glucose tolerance but not with whole body or hepatic insulin resistance in Mexican Americans. Am J Physiol Endocrinol Metab. 2009;296:E758–64.
Liu DJ, Peloso GM, Yu H, Butterworth AS, Wang X, Mahajan A, et al. Exome-wide association study of plasma lipids in >300,000 individuals. Nat Genet. 2017;49:1758–66.
Park H, Green MH, Shaffer ML. Association between serum retinol-binding protein 4 concentrations and clinical indices in subjects with type 2 diabetes: a meta-analysis. J Hum Nutr Diet. 2012;25:300–10.
Zhang L, Cheng YL, Xue S, Xu ZG. The role of circulating RBP4 in the type 2 diabetes patients with kidney diseases: a systematic review and Meta-analysis. Dis Markers. 2020;2020:8830471.
Mantovani A, Petracca G, Beatrice G, Csermely A, Lonardo A, Schattenberg JM, et al. Non-alcoholic fatty liver disease and risk of incident chronic kidney disease: an updated meta-analysis. Gut. 2022;71:156–62.
Funding
No funding in this article.
Author information
Authors and Affiliations
Contributions
The first author Rui Hu and the second author Xiaoyue Yang wrote the main manuscript text and the third author Xiaoyu He prepared figures and tables. Any issues raised were resolved through discussion with the fourth author Guangyao Song. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
None.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, R., Yang, X., He, X. et al. The relationship between NAFLD and retinol-binding protein 4 - an updated systematic review and meta-analysis. Lipids Health Dis 22, 8 (2023). https://doi.org/10.1186/s12944-022-01771-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01771-2