Abstract
Background
Ischemic strokes are primarily caused by intracranial and extracranial atherosclerotic stenosis. Nontraditional lipid parameters broaden traditional lipid profiles, better reflect the metabolism and interaction between different lipid components, and optimize the predictive ability of lipid profiles for atherosclerotic diseases. This research was carried out to investigate the predictive value of nontraditional lipid parameters for intracranial or extracranial atherosclerotic stenosis.
Methods
The investigation collected data from inpatients who underwent cervical vascular ultrasonography, carotid CTA, cerebral artery CTA or MRA, and brain MRI or CT from December 2014 to December 2021. The nontraditional lipid parameters were calculated by collecting traditional lipid parameters. To evaluate the predictive power of nontraditional lipid parameters, logistic regression and receiver operating characteristic curve (ROC) analyses were performed.
Results
Based on the inclusion and exclusion criteria, 545 patients were included. According to the imaging results, inpatients were divided into two groups, including no intracranial or extracranial atherosclerotic stenosis (n = 250) and intracranial or extracranial atherosclerotic stenosis (AS, n = 295). Among them, AS was further divided into three subgroups: intracranial atherosclerotic stenosis (ICAS), extracranial atherosclerotic stenosis (ECAS) and combined intracranial and extracranial atherosclerotic stenosis (IECAS). Logistic regression analysis showed that nontraditional lipid parameters, including the atherogenic index of plasma (AIP), TG/HDL-C, remnant cholesterol (RC), nonhigh-density lipoprotein cholesterol (non-HDL-C), lipoprotein combine index (LCI), atherogenic coefficient (AC), Castelli’s index-I (CRI-I) and Castelli’s index-II (CRI-II), were significantly correlated with intracranial or extracranial atherosclerotic stenosis (P < 0.05). Compared with other nontraditional lipid parameters, regardless of adjusting for potential confounding factors, AIP had a greater OR value in ICAS (OR = 4.226, 95% CI: 1.681–10.625), ECAS (OR = 2.993, 95% CI: 1.119–8.003) and IECAS (OR = 4.502, 95% CI: 1.613–12.561). ROC curve analysis revealed that nontraditional lipid parameters had good predictive power for intracranial or extracranial atherosclerotic stenosis.
Conclusions
This Chinese hospital-based study demonstrates that nontraditional lipid parameters (AIP, LCI, RC, CRI-II, AC, CRI-I and non-HDL-C) are effective predictors of intracranial and extracranial atherosclerotic stenosis, of which AIP may be a significant risk factor for predicting atherosclerotic arterial stenosis in the intracranial or extracranial regions.
Similar content being viewed by others
Introduction
Stroke is the second leading cause of death and the third leading cause of death and disability combined worldwide, with ischemic strokes representing over half of all stroke types [1]. Ischemic strokes are primarily caused by intracranial and extracranial atherosclerotic stenosis [2,3,4]. It is paramount that extracranial and intracranial atherosclerotic stenosis be identified as early as possible to prevent ischemic strokes. Atherosclerotic disease risk can be predicted by traditional serum lipid parameters, which are widely used because of their easy collection process and low cost. Previous studies have demonstrated that traditional lipid parameters such as low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C) were considered to be correlated with cardiovascular disease or ischemic strokes [2, 5,6,7,8,9,10,11]. Among them, LDL-C, HDL-C, and TC were found to be linked to intracranial or extracranial carotid arterial stenosis [12,13,14].
Unlike traditional individual lipid parameters, nontraditional lipid parameters, such as the atherogenic index of plasma (AIP), TG/HDL-C, remnant cholesterol (RC), nonhigh-density lipoprotein cholesterol (non-HDL-C), lipoprotein combine index (LCI), atherogenic coefficient (AC), Castelli’s index-I (CRI-I) and Castelli’s index-II (CRI-II), are calculated from two or more traditional lipid parameters. Nontraditional lipid parameters provide insight into the balance between atherogenic lipoproteins and antiatherogenic lipoproteins, and several studies have shown that nontraditional lipid parameters such as AIP, non-HDL-C, LCI, RC, TG/HDL-C, AC, CRI-I and CRI-II were closely related to cardiovascular and cerebrovascular diseases, which might be even superior to traditional lipid parameters [6, 15,16,17,18,19].
The AIP is the base 10 logarithm of circulating TG/HDL-C, which is a plasma atherosclerosis marker proposed by Dobiás̆ová in 2001 [20]. The AIP value can be a straightforward means to indirectly reflect the level of sdLDL-C. SdLDL-C was defined as LDL-C particles with a diameter of less than 25.5 nm and a density of more than 1.034 g/mL [21], which was strongly atherogenic [22]. SdLDL-C has been listed as a potential biomarker of cardiovascular disease [23]. Studies have found that AIP is a novel marker of cardiovascular disease [24, 25] and may be superior to traditional lipid parameters [26,27,28]. Nevertheless, only a few studies have been conducted regarding the association between AIP and intracranial or extracranial atherosclerotic stenosis; the predictive value remains unclear for intracranial atherosclerotic stenosis [29, 30].
Remnant cholesterol refers to the cholesterol content in a subset of triglyceride-rich lipoproteins known as remnants, viz. chylomicron remnants, VLDL, and IDL during nonfasting conditions, and VLDL and IDL during fasting conditions [31]. LCI was also a new nontraditional lipid parameter that was calculated as the ratio of TC∗TG∗LDL-C to HDL-C. Previous investigations on LCI and RC have mainly focused on the field of cardiovascular disease [32, 33], and studies of RC and LCI with extracranial and intracranial atherosclerotic stenosis are very rare.
The relationships between various nontraditional lipid parameters and intracranial or extracranial atherosclerotic arterial stenosis are still unclear. Logistic regression and ROC curves were utilized to analyze the relationships between various nontraditional lipid parameters and intracranial or extracranial atherosclerotic stenosis. A total of 545 inpatients were involved in this research. For more accurate assessment of atherosclerotic stenosis in the intracranial or extracranial regions, multiple imaging examinations were performed.
Methods
Study population
This is observational clinical research conducted at a single center with a total of 545 inpatients involved (Additional file 1: Fig. S1). Patients were divided into two groups, including no intracranial or extracranial artery stenosis (the control group, n = 250) and intracranial or extracranial atherosclerotic stenosis (the study group, n = 295). The study group consisted of three subgroups: intracranial atherosclerotic stenosis (ICAS, n = 108), combined intracranial and extracranial artery stenosis (IECAS, n = 113), and extracranial artery stenosis (ECAS, n = 74). Furthermore, the extracranial atherosclerotic stenosis group consisted of extracranial carotid atherosclerotic stenosis (ECCAS, n = 45), extracranial vertebral atherosclerotic stenosis (n = 40), and combined extracranial carotid and vertebral atherosclerotic stenosis (n = 25). Data for the study were provided by the Medical Research Big Data Platform of the Affiliated Hospital of Qingdao University, with full approval from the Ethics Committee.
Definition
All included patients underwent carotid artery imaging (carotid CTA and cervical vascular ultrasonography), cerebral artery imaging (cerebral artery CTA or MRA), and brain CT or MRI.
Intracranial and extracranial atherosclerotic stenosis could be defined as follows:
-
(1).
Intracranial atherosclerotic stenosis: significant atherosclerotic stenosis of cerebral arteries in the proximal anterior, middle, or posterior areas; the internal carotid, vertebral, or basilar arteries in the intracranial region exhibited obvious atherosclerotic stenosis.
-
(2).
Extracranial atherosclerotic stenosis: common carotid artery, extracranial region of internal carotid artery, or extracranial segment of vertebral artery had obvious stenosis
-
(3).
Combined intracranial and extracranial atherosclerotic stenosis: significant stenosis was present in both the intracranial and extracranial arteries in tandem or parallel lesions;
-
(4).
No intracranial or extracranial arterial stenosis: no obvious stenosis of either intracranial or extracranial arteries;
-
(5).
Significant artery stenosis of intracranial or extracranial regions could be defined as ≥50% stenosis of arteries in the intracranial or extracranial regions [34, 35] or an internal carotid artery flow velocity ≥ 125 cm/s [36].
For patients with different imaging results between cerebral artery CTA and MRA, CTA was given priority due to the limitations of MRA imaging. All imaging findings were assessed by three experienced doctors who were blinded to this study.
Data
Following admission, blood samples from the peripheral veins were collected early in the morning for biochemical testing after 8 hours of fasting. In addition, clinical baseline data of inpatients were collected, such as age, sex, body mass index (BMI), history of hypertension, smoking, ischemic stroke, diabetes mellitus and coronary heart disease.
An automatic biochemical analyzer was utilized to measure LDL-C, TC, TG, and fasting blood glucose (FBG) levels. The following formulas were used to calculate nontraditional lipid parameters:
-
(1)
AIP = lg (TG/HDL − C) [20];
-
(2)
non − HDL − C = TC − HDL − C [16];
-
(3)
AC = non − HDL − C/HDL − C [30];
-
(4)
CRI − I = TC/HDL − C [30];
-
(5)
CRI − II = LDL − C/HDL − C [30];
-
(6)
LCI = TC ∗ TG ∗ LDL − C/HDL − C [32];
-
(7)
RC = TC − HDL − C − LDL − C [37].
Statistical analyses
Normally distributed continuous variables are presented as the mean ± standard deviation, which was compared between two groups by using an independent samples t test. In cases where continuous variables were not normally distributed, the variables are shown as medians and interquartile ranges (IQRs), and the Mann–Whitney U test was applied for comparison. Categorical variables are presented as frequencies (percentages). Analyses of categorical variables were conducted using chi-square tests. To assess the relationship between the nontraditional lipid parameters and intracranial or extracranial atherosclerotic stenosis, logistic regression analyses were utilized. Furthermore, three regression models were constructed: Model 1 (without adjusting for any covariates), Model 2 (adjusted for age and sex) and Model 3 (Model 2 plus BMI, FBG, history of coronary heart disease, hypertension, smoking, ischemic stroke, and diabetes mellitus); in the models, the nontraditional lipid parameters were separated into four quartiles to assess the relationship between quartiles and intracranial or extracranial artery stenosis with the lowest quartile as a reference. ROC curves were applied to calculate the area under the curve (AUC) of nontraditional lipid parameters for each group. All data analysis was performed using IBM SPSS Statistics 26.0. P < 0.05 was considered statistically significant.
Results
Univariate analysis
Comparison of study and control groups
As shown in Table 1, data for clinical baseline characteristics and lipid parameters of subjects are summarized. Compared to the control group, the study group had significant differences in history of hypertension, ischemic stroke, smoking and diabetes mellitus (P < 0.05). HDL-C was also found to be lower in the study group (P < 0.05). Age, FBG and other lipid parameters were found to be markedly increased in the study group (P < 0.05).
Subgroup analysis
In comparison to the control group, significant differences were found in sex, history of hypertension and BMI in the ICAS group. On the other hand, age, history of smoking, hypertension, diabetes mellitus and ischemic stroke had significant differences in the IECAS (P < 0.05). Traditional lipid parameters (LDL-C, TC and TG) and nontraditional lipid parameters (including non-HDL-C, AIP, AC, RC, CRI-I and CRI-II) and FBG were found to be significantly increased in ICAS and IECAS; in contrast, HDL-C levels were lower in ICAS and IECAS (P < 0.05). Marked differences were shown in age and the history of smoking between the ECAS and the control group, and LDL-C, TC, TG, AIP, AC, LCI, CRI-I, CRI-II, non-HDL-C and RC were markedly increased in ECAS (P < 0.05). In accordance with the subgroup analysis of the extracranial artery stenosis group (ECCAS), significant differences could be seen in age and the history of smoking in ECCAS compared to the control group. Levels of LDL-C and TC were markedly increased in ECCAS (P < 0.05), and non-HDL-C, LCI, AC, CRI-I and CRI-II values were markedly greater in ECCAS (P < 0.05) (Table 1 and Additional file 2: Table S1).
Logistic regression analyses
Three logistic regression models were constructed, and the results are shown in Additional file 3: Table S2 - Additional file 6: Table S5. Regardless of the adjustment of confounding factors, an independent relationship was observed between nontraditional lipid parameters and atherosclerotic arterial stenosis in the intracranial or extracranial regions, and AIP had the largest OR value compared with other lipid parameters.
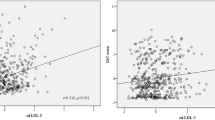
In model 3, the ICAS group indicated the following: LDL-C (OR = 2.665, 95% CI: 1.913–3.712), TC (1.808, 1.411–2.317), TG (1.242, 1.010–1.528), and nontraditional lipid parameters, including AIP (4.226, 1.681–10.625), non-HDL-C (2.026, 1.549–2.649), AC (1.702, 1.318–2.196), CRI-I (1.702, 1.318–2.196), CRI-II (2.581, 1.819–3.660), and LCI (1.014, 1.002–1.025), were significantly correlated with intracranial atherosclerotic stenosis (all P < 0.05), and AIP had the highest OR value. Analysis of the ECAS group showed that LDL-C (OR = 2.187, 95% CI: 1.542–3.100), TC (1.536, 1.176–2.006) and nontraditional lipid parameters, including AIP (2.993, 1.119–8.003), non-HDL-C (1.690, 1.267–2.253), AC (1.509, 1.155–1.972), CRI-I (1.509, 1.155–1.972), and CRI-II (2.274, 1.565–3.303), were all significantly associated with extracranial atherosclerotic stenosis (all P < 0.05). With the lowest quartile as a reference, the 2nd, 3rd and 4th quartiles of LCI were highly correlated with extracranial artery stenosis (P < 0.05), and the 2nd and 3rd quartiles of RC were statistically significantly correlated with extracranial artery stenosis (P < 0.05) (Figs. 1 and 2).
Forest plot of logistic regression analysis of intracranial atherosclerotic stenosis in Model 3. Data were adjusted for age, sex, BMI, FBG, history of ischemic stroke, coronary heart disease, smoking, hypertension, and diabetes mellitus. ICAS intracranial atherosclerotic stenosis, BMI body mass index, FBG fasting blood glucose, LDL-C low-density lipoprotein cholesterol, TC total cholesterol, TG triglyceride, HDL-C high-density lipoprotein cholesterol, AIP atherogenic index of plasma, non-HDL-C nonhigh-density lipoprotein cholesterol, AC atherogenic coefficient, CRI-I Castelli’s index-I, CRI-II Castelli’s index-II, LCI lipoprotein combine index, RC remnant cholesterol
Forest plot of logistic regression analysis of extracranial atherosclerotic stenosis in Model 3. Data were adjusted for age, sex, BMI, FBG, history of ischemic stroke, coronary heart disease, smoking, hypertension, and diabetes mellitus. ECAS extracranial atherosclerotic stenosis, BMI body mass index, FBG fasting blood glucose, LDL-C low-density lipoprotein cholesterol, TC total cholesterol, TG triglyceride, HDL-C high-density lipoprotein cholesterol, AIP atherogenic index of plasma, non-HDL-C nonhigh-density lipoprotein cholesterol, AC atherogenic coefficient, CRI-I Castelli’s index-I, CRI-II Castelli’s index-II, LCI lipoprotein combine index, RC remnant cholesterol
ROC curve analysis
ROC curves revealed that AIP, non-HDL-C, LCI, AC, RC, CRI-I and CRI-II had greater AUC values in IECAS, ICAS and ECAS, while the AUC values of non-HDL-C, AC, CRI-I, CRI-II and LCI were greater in ECCAS (Table 2).
Discussion
Through the above study, these findings demonstrated that (1) the AIP may represent an independent risk factor for intracranial or extracranial atherosclerotic stenosis; (2) the LCI and RC were closely related to intracranial or extracranial atherosclerotic stenosis; and (3) the AC, CRI-I and CRI-II were highly correlated with intracranial or extracranial artery stenosis, whereas the AC, CRI-I and CRI-II were more effective at predicting ICAS or IECAS.
This study found that regardless of the subgroup, AIP was significantly related to intracranial and extracranial artery stenosis. AIP is a novel nontraditional lipid parameter with values ranging from negative to positive, and values of 0 are closely associated with LDL particles with a diameter of 25.5 nm; that size corresponds to the cutoff value of particle size between the two phenotypes of LDL particles A and B [20]. Since sdLDL-C is predominant in phenotype B [38], AIP can be used as an indicator of the LDL phenotype and indirectly reflect sdLDL-C levels. The low affinity of sdLDL-C to its receptor leads to a longer blood circulation time, which increases the possibility of its atherosclerotic modification in plasma; this longer circulation time, coupled with its small particle size, makes it easier to invade the arterial wall, thus participating in atherogenesis [22, 39,40,41,42]. Compared with LDL-C levels, sdLDL-C levels might serve as a better indicator of coronary heart disease [39, 43]. At the same time, sdLDL-C was also closely associated with ischemic stroke, carotid atherosclerosis and carotid stenosis [22, 44,45,46,47,48]. Unfortunately, sdLDL-C is limited in clinical practice as a result of the high detection cost and complicated procedures, but AIP can only be used as a simple method to reflect the level of sdLDL-C, and many studies have confirmed that AIP can predict the occurrence of cardiovascular disease events [49,50,51]. Nevertheless, a very small number of studies have investigated the relationships between AIP and intracranial or extracranial atherosclerosis [29, 30].
Analyses conducted on ICAS showed that AIP might represent an independent predictor of intracranial artery stenosis in this study. Interestingly, a previous study found that there was an association between AIP and the prevalence of asymptomatic intracranial artery stenosis, but the statistical significance disappeared when potential confounders were fully adjusted [30]. Although this finding seems to be slightly different from the previous study, perhaps it can be explained by the following reasons: (1) the two investigations are based on different study populations; (2) the prevalence of ICAS was higher in this study; (3) this study included all asymptomatic and symptomatic patients with arterial stenosis, and coronary heart disease as a covariate that might have influenced the study results was adjusted; and (4) transcranial Doppler ultrasonography (TCD) was applied to evaluate intracranial artery stenosis in the former and was excessively dependent on the operator, so the accuracy and reliability of its examination might be limited. By using CTA or MRA and cervical vascular ultrasonography, intracranial or extracranial artery stenosis was fully evaluated in this study. In addition, this study indicated that AIP was independently correlated with extracranial carotid atherosclerotic stenosis. Recently, case–controlled research carried out at a single center using a sample of patients who suffered from ischemic stroke found that with quartile 1 as the reference, the 3rd and 4th quartiles of AIP were independently correlated with symptomatic carotid artery stenosis [29]. With the lowest quartile as a reference in this study, the 3rd quartile of AIP was closely associated with extracranial carotid atherosclerotic stenosis regardless of adjustment for potential confounding variables. In contrast to the former study, the research included all symptomatic and asymptomatic patients excluded from lipid-lowering therapy and adjusted for confounding variables in Models 2 and 3, particularly adjusting for multiple potential confounding variables in Model 3. Thus, this research concluded that AIP may be an independent predictor of extracranial carotid atherosclerotic stenosis.
Both LCI and RC were closely associated with intracranial and extracranial atherosclerotic stenosis. A case–control study showed that compared with patients without coronary artery disease, patients who underwent bypass grafting for cardiovascular disease had higher levels of LCI, and an ROC curve analysis showed that its specificity was the highest [33]. Si et al. found that increased retinol-binding protein-4 (RBP-4) and LCI values were independent risk factors for acute coronary syndrome (ACS), and the combination of the two tests might be a potential diagnostic indicator for ACS [32]. It is worth noting that the analysis of LCI demonstrated that even though the OR value of LCI in logistic regression analysis of each group was small, close to the cutoff value of 1, LCI had a large OR in this study during logistic regression analysis of LCI quartiles, and ROC curve analysis showed good predictive values. Therefore, the LCI may be used as an independent predictor of intracranial or extracranial atherosclerotic arterial stenosis. The estimated value of RC can be simply calculated by subtracting LDL-C and HDL-C from TC [37]. Previous studies have reported that even after reducing LDL-C to recommended levels, a larger residual cardiovascular disease risk remained, which might be partly due to increased residual cholesterol levels [31, 37], and the causal relationship between RC and coronary heart disease has been established in multiple studies [31, 52, 53]. A Korean case–control study demonstrated that high levels of remnant lipoprotein cholesterol (RLP-C) were correlated with ischemic stroke, particularly atherosclerotic stroke of the large arteries [54]. Subsequently, a prospective multicenter study in Korea revealed that reduced RLP-C was correlated with preventing the angiographic progression of symptomatic ICAS [55]. Yang et al. found that RC/HDL-C was significantly associated with intracranial atherosclerotic stenosis [56]. Therefore, according to the above studies, this investigation hypothesized that RC was significantly associated with ICAS. Fortunately, especially in the extracranial carotid stenosis subgroup, the results confirmed the speculation that RC also showed a significant difference in the quartile analysis of each group, indicating that RC may be a risk factor independently associated with atherosclerotic stenosis, whether intracranial or extracranial.
Lipid ratios, including AC, CRI-I and CRI-II, were shown to be closely correlated with intracranial or extracranial atherosclerotic arterial stenosis in this investigation. Interestingly, based on our findings, CRI-I and AC have the same OR values, confidence intervals and P values. In essence, both CRI-I and AC have the same statistical significance, as the calculation formulas of the two can be converted into each other. Thus, the author recommends that only one of the two is applied in scientific research or clinical practice. It is noteworthy that CRI-II had a larger OR value than CRI-I or AC in each group, suggesting that CRI-II was more strongly associated with intracranial and extracranial atherosclerotic stenosis. This may be because Castelli’s index-II better reflects the balance between LDL-C, which is the major atherogenic lipoprotein, and HDL-C, which is the antiatherogenic lipoprotein. As has been reported previously, CRI-II, AC or CRI-I have been shown to be closely correlated with ischemic stroke [57], carotid intima-media thickness [58,59,60,61], carotid plaque [61,62,63] and intracranial atherosclerotic stenosis [30, 56]. Yang and colleagues reported that CRI-II, AC and CRI-I were closely correlated with ICAS but not with ECAS after adjusting for confounders [56]. In a subsequent community-based study of asymptomatic intracranial artery stenosis, a significant association was also reported between CRI-II AC and CRI-I and an increased prevalence of asymptomatic intracranial artery stenosis [30]. However, this investigation demonstrated that CRI-II, AC and CRI-I had a strong relationship with intracranial or extracranial atherosclerotic stenosis, whether or not adjusted for confounders. This finding seems to contradict the conclusion of Yang and colleagues, and the following reasons may explain why: (1) there is a higher prevalence of extracranial artery stenosis in this study, and the investigation excluded patients taking lipid-lowering treatment, which may well influence the findings; (2) this study included subjects with total occlusion of the intracranial and extracranial arteries, considering subjects with complete intracranial and extracranial arterial occlusion who may have more severe dyslipidemia. This investigation revealed that CRI-II, AC and CRI-I were independent predictors of intracranial or extracranial atherosclerotic stenosis. At the same time, it seemed that CRI-II, AC and CRI-I were more valuable for predicting ICAS or IECAS.
There are several novelties in this study. First, LCI and RC were rarely studied in intracranial and extracranial atherosclerotic stenosis, and the research found that LCI and RC were significantly correlated with intracranial and extracranial atherosclerotic stenosis through both univariate and multivariate analyses. Second, it was also examined whether nontraditional lipid parameters (AIP, LCI, RC, CRI-II, AC, CRI-I and non-HDL-C) could predict IECAS, and the findings showed that nontraditional lipid parameters were closely related to IECAS. Therefore, this research draws broader conclusions that nontraditional lipid parameters (AIP, LCI, RC, CRI-II, AC, CRI-I, and non-HDL-C) are independent risk factors for atherosclerotic stenosis in the intracranial or extracranial regions. Furthermore, since previous studies have not established the predictive value of AIP for intracranial and extracranial atherosclerotic arterial stenosis, the research demonstrated that AIP was an independent predictor of atherosclerotic arterial stenosis in the intracranial or extracranial regions.
Study strengths and limitations
Strengths
(1) This study collected detailed imaging data and integrated several imaging results, so it evaluated intracranial and external arterial stenosis more accurately. (2) Compared with vascular ultrasonography, nontraditional lipid parameters are less operator-dependent and easy to collect; thus, they can also be utilized as a screening method for atherosclerotic arterial stenosis in the intracranial or extracranial regions. (3) Subjects taking lipid-lowering drugs were excluded from this study, and the logistic regression model was adjusted to include history of coronary heart disease and other confounding factors to minimize the interference of these confounding factors on the study results.
Limitations
(1) This is a case–control investigation conducted by a single center based on hospital patients, and the causal relationship is limited. However, it is based on hospital patients for whom we have complete and accurate imaging examinations of intracranial and extracranial arteries, which can fully evaluate intracranial and extracranial artery stenosis. (2) Our study is based on the Chinese population, and it has been reported that AIP is related to race, region, diet and lifestyle, so caution should be taken in extending our study conclusions.
(3) Previous studies reported that AIP was related to serum uric acid. Unfortunately, we did not collect serum uric acid data from patients, so we did not analyze it.
Conclusion
This investigation demonstrated that AIP, LCI, RC, CRI-II, AC, CRI-I and non-HDL-C were markedly correlated with intracranial and extracranial atherosclerotic stenosis. The AIP may be a better independent predictor of atherosclerotic arterial stenosis in the intracranial or extracranial regions. Nontraditional lipid parameters may be used as an alternative method to imaging examination in the early screening of intracranial and extracranial atherosclerotic stenosis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the first author on reasonable request.
Abbreviations
- AIP:
-
Atherogenic index of plasma
- AC:
-
Atherogenic coefficient
- CRI-I:
-
Castelli’s index-I
- CRI-II:
-
Castelli’s index-II
- Non-HDL-C:
-
Nonhigh-density lipoprotein cholesterol
- LCI:
-
Lipoprotein combine index
- RC:
-
Remnant cholesterol
- AUC:
-
Area under the curve
- LDL-C:
-
Low-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- sdLDL-C:
-
Small dense low-density lipoprotein cholesterol
- AS:
-
Intracranial or extracranial atherosclerotic stenosis
- CTA:
-
Computed tomography angiography
- CT:
-
Computed Tomography
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- ICAS:
-
Intracranial atherosclerotic stenosis
- ECAS:
-
Extracranial atherosclerotic stenosis
- IECAS:
-
Combined intracranial and extracranial atherosclerotic stenosis
- ECCAS:
-
Extracranial carotid atherosclerotic stenosis
- BMI:
-
Body mass index
- FBG:
-
Fasting blood glucose
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- 95% CI:
-
95% confidence interval
References
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820.
Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet (London, England). 2014;383(9921):984–98.
Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2013;12(11):1106–14.
Sun J, Yuan C, Hatsukami TS. Stroke prevention with Extracranial carotid artery disease. Curr Cardiol Rep. 2021;23(11):161.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;139(25):e1082–e143.
Boekholdt SM, Arsenault BJ, Mora S, Pedersen TR, LaRosa JC, Nestel PJ, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. Jama. 2012;307(12):1302–9.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European atherosclerosis society consensus panel. Eur Heart J. 2017;38(32):2459–72.
Holmes MV, Millwood IY, Kartsonaki C, Hill MR, Bennett DA, Boxall R, et al. Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J Am Coll Cardiol. 2018;71(6):620–32.
Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology. 2007;68(8):556–62.
Yuan S, Tang B, Zheng J, Larsson SC. Circulating lipoprotein lipids, Apolipoproteins and ischemic stroke. Ann Neurol. 2020;88(6):1229–36.
Welsh C, Celis-Morales CA, Brown R, Mackay DF, Lewsey J, Mark PB, et al. Comparison of conventional lipoprotein tests and Apolipoproteins in the prediction of cardiovascular disease. Circulation. 2019;140(7):542–52.
Ritz K, Denswil NP, Stam OC, van Lieshout JJ, Daemen MJ. Cause and mechanisms of intracranial atherosclerosis. Circulation. 2014;130(16):1407–14.
Shen Y, Wang J, Wu J, Qu W, Wang C, Gao X, et al. Elevated plasma total cholesterol level is associated with the risk of asymptomatic intracranial arterial stenosis. PLoS One. 2014;9(7):e101232.
Garvey L, Makaroun MS, Muluk VS, Webster MW, Muluk SC. Etiologic factors in progression of carotid stenosis: a 10-year study in 905 patients. J Vasc Surg. 2000;31(1 Pt 1):31–8.
Björnsson E, Thorleifsson G, Helgadóttir A, Guðnason T, Guðbjartsson T, Andersen K, et al. Association of Genetically Predicted Lipid Levels with the extent of coronary atherosclerosis in Icelandic adults. JAMA Cardiol. 2020;5(1):13–20.
Wu J, Chen S, Liu L, Gao X, Zhou Y, Wang C, et al. Non-high-density lipoprotein cholesterol vs low-density lipoprotein cholesterol as a risk factor for ischemic stroke: a result from the Kailuan study. Neurol Res. 2013;35(5):505–11.
Zhu L, Lu Z, Zhu L, Ouyang X, Yang Y, He W, et al. Lipoprotein ratios are better than conventional lipid parameters in predicting coronary heart disease in Chinese Han people. Kardiol Pol. 2015;73(10):931–8.
Millán J, Pintó X, Muñoz A, Zúñiga M, Rubiés-Prat J, Pallardo LF, et al. Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag. 2009;5:757–65.
Kang K, Lee K, Chung SH. The triglyceride:high-density lipoprotein-cholesterol ratio and steno-occlusive disease in the intracranial arteries. J Thromb Thrombolysis. 2011;32(1):103–9.
Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34(7):583–8.
Kanonidou C. Small dense low-density lipoprotein: analytical review. Clinica chimica acta Int J Clin Chem. 2021;520:172–8.
Shoji T, Hatsuda S, Tsuchikura S, Shinohara K, Kimoto E, Koyama H, et al. Small dense low-density lipoprotein cholesterol concentration and carotid atherosclerosis. Atherosclerosis. 2009;202(2):582–8.
Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143–421.
Niroumand S, Khajedaluee M, Khadem-Rezaiyan M, Abrishami M, Juya M, Khodaee G, et al. Atherogenic index of plasma (AIP): a marker of cardiovascular disease. Med J Islam Repub Iran. 2015;29:240.
Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN. Atherogenic index of plasma: novel predictive biomarker for cardiovascular illnesses. Arch Med Res. 2019;50(5):285–94.
Huang H, Yu X, Li L, Shi G, Li F, Xiao J, et al. Atherogenic index of plasma is related to coronary atherosclerotic disease in elderly individuals: a cross-sectional study. Lipids Health Dis. 2021;20(1):68.
Guo Q, Zhou S, Feng X, Yang J, Qiao J, Zhao Y, et al. The sensibility of the new blood lipid indicator--atherogenic index of plasma (AIP) in menopausal women with coronary artery disease. Lipids Health Dis. 2020;19(1):27.
Cai G, Liu W, Lv S, Wang X, Guo Y, Yan Z, et al. Gender-specific associations between atherogenic index of plasma and the presence and severity of acute coronary syndrome in very young adults: a hospital-based observational study. Lipids Health Dis. 2019;18(1):99.
Garg R, Knox N, Prasad S, Zinzuwadia S, Rech MA. The Atherogenic index of plasma is independently associated with symptomatic carotid artery stenosis. J Stroke Cerebrovasc Dis. 2020;29(12):105351.
Guo J, Wang A, Wang Y, Liu X, Zhang X, Wu S, et al. Non-traditional lipid parameters as potential predictors of asymptomatic intracranial arterial stenosis. Front Neurol. 2021;12:679415.
Varbo A, Benn M, Nordestgaard BG. Remnant cholesterol as a cause of ischemic heart disease: evidence, definition, measurement, atherogenicity, high risk patients, and present and future treatment. Pharmacol Ther. 2014;141(3):358–67.
Si Y, Liu J, Han C, Wang R, Liu T, Sun L. The correlation of retinol-binding protein-4 and lipoprotein combine index with the prevalence and diagnosis of acute coronary syndrome. Heart Vessel. 2020;35(11):1494–501.
Çelik E, Çora AR, Karadem KB. The effect of untraditional lipid parameters in the development of coronary artery disease: Atherogenic index of plasma, Atherogenic coefficient and lipoprotein combined index. J Saudi Heart Assoc. 2021;33(3):244–50.
Barnett HJM, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, Ferguson GG, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325(7):445–53.
Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000;21(4):643–6.
Naylor AR, Ricco JB, de Borst GJ, Debus S, de Haro J, Halliday A, et al. Editor's choice - Management of Atherosclerotic Carotid and Vertebral Artery Disease: 2017 clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2018;55(1):3–81.
Sandesara PB, Virani SS, Fazio S, Shapiro MD. The forgotten lipids: triglycerides, remnant cholesterol, and atherosclerotic cardiovascular disease risk. Endocr Rev. 2019;40(2):537–57.
Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82(2):495–506.
Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, et al. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the atherosclerosis risk in communities (ARIC) study. Arterioscler Thromb Vasc Biol. 2014;34(5):1069–77.
Packard C, Caslake M, Shepherd J. The role of small, dense low density lipoprotein (LDL): a new look. Int J Cardiol. 2000;74(Suppl 1):S17–22.
Griffin BA. Lipoprotein atherogenicity: an overview of current mechanisms. Proc Nutr Soc. 1999;58(1):163–9.
Ivanova EA, Myasoedova VA, Melnichenko AA, Grechko AV, Orekhov AN. Small dense low-density lipoprotein as biomarker for atherosclerotic diseases. Oxidative Med Cell Longev. 2017;2017:1273042.
Tsai MY, Steffen BT, Guan W, McClelland RL, Warnick R, McConnell J, et al. New automated assay of small dense low-density lipoprotein cholesterol identifies risk of coronary heart disease: the multi-ethnic study of atherosclerosis. Arterioscler Thromb Vasc Biol. 2014;34(1):196–201.
Shen H, Xu L, Lu J, Hao T, Ma C, Yang H, et al. Correlation between small dense low-density lipoprotein cholesterol and carotid artery intima-media thickness in a healthy Chinese population. Lipids Health Dis. 2015;14:137.
Manabe Y, Morihara R, Matsuzono K, Nakano Y, Takahashi Y, Narai H, et al. Estimation of the presence of small dense lipoprotein cholesterol in acute ischemic stroke. Neurol Int. 2015;7(1):5973.
Landray MJ, Sagar G, Muskin J, Murray S, Holder RL, Lip GY. Association of atherogenic low-density lipoprotein subfractions with carotid atherosclerosis. QJM Monthly J Assoc Phys. 1998;91(5):345–51.
Hulthe J, Bokemark L, Wikstrand J, Fagerberg B. The metabolic syndrome, LDL particle size, and atherosclerosis: the atherosclerosis and insulin resistance (AIR) study. Arterioscler Thromb Vasc Biol. 2000;20(9):2140–7.
Shen H, Zhou J, Shen G, Yang H, Lu Z, Wang H. Correlation between serum levels of small, dense low-density lipoprotein cholesterol and carotid stenosis in cerebral infarction patients >65 years of age. Ann Vasc Surg. 2014;28(2):375–80.
Dobiásová M, Frohlich J, Sedová M, Cheung MC, Brown BG. Cholesterol esterification and atherogenic index of plasma correlate with lipoprotein size and findings on coronary angiography. J Lipid Res. 2011;52(3):566–71.
Wang L, Chen F, Xiaoqi C, Yujun C, Zijie L. Atherogenic index of plasma is an independent risk factor for coronary artery disease and a higher SYNTAX score. Angiology. 2021;72(2):181–6.
Sadeghi M, Heshmat-Ghahdarijani K, Talaei M, Safaei A, Sarrafzadegan N, Roohafza H. The predictive value of atherogenic index of plasma in the prediction of cardiovascular events; a fifteen-year cohort study. Adv Med Sci. 2021;66(2):418–23.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61(4):427–36.
Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76(23):2712–24.
Kim JY, Park JH, Jeong SW, Schellingerhout D, Park JE, Lee DK, et al. High levels of remnant lipoprotein cholesterol is a risk factor for large artery atherosclerotic stroke. J Clin Neurol (Seoul, Korea). 2011;7(4):203–9.
Kim DE, Kim JY, Jeong SW, Cho YJ, Park JM, Lee JH, et al. Association between changes in lipid profiles and progression of symptomatic intracranial atherosclerotic stenosis: a prospective multicenter study. Stroke. 2012;43(7):1824–30.
Yang WS, Li R, Shen YQ, Wang XC, Liu QJ, Wang HY, et al. Importance of lipid ratios for predicting intracranial atherosclerotic stenosis. Lipids Health Dis. 2020;19(1):160.
Pikula A, Beiser AS, Wang J, Himali JJ, Kelly-Hayes M, Kase CS, et al. Lipid and lipoprotein measurements and the risk of ischemic vascular events: Framingham study. Neurology. 2015;84(5):472–9.
Qin G, Tu J, Zhang C, Tang X, Luo L, Wu J, et al. The value of the apoB/apoAΙ ratio and the non-HDL-C/HDL-C ratio in predicting carotid atherosclerosis among Chinese individuals with metabolic syndrome: a cross-sectional study. Lipids Health Dis. 2015;14:24.
Zhang Z, Liu Y, Zhang Y, Qin P, Zhao P, Wang C, et al. The association between low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio cholesterol ratio and thickened carotid intima-media thickness: A case-control study. Vascular. 2022;30(5):943–51.
Qin P, Shi J, Cao L, Li X, Lou Y, Wang C, et al. Low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio and carotid intima-media thickness: a cohort study in China. Lipids. 2021;56(1):59–68.
Iannuzzi A, Giallauria F, Gentile M, Rubba P, Covetti G, Bresciani A, et al. Association between non-HDL-C/HDL-C ratio and carotid intima-media thickness in post-menopausal women. J Clin Med. 2021;11(1):78.
Wang W, Huo Y, Zhao D, Liu J, Liang LR, Sun JY, et al. Prediction value of blood lipid levels on newly identified carotid plaque in middle-aged and elderly Chinese population. Zhonghua xin xue guan bing za zhi. 2010;38(12):1118–22.
Liu Y, Zhu Y, Jia W, Sun D, Zhao L, Zhang C, et al. Association between lipid profiles and presence of carotid plaque. Sci Rep. 2019;9(1):18011.
Acknowledgments
Not applicable.
Funding
This study was supported by the Natural Science Foundation of China (82270518) and the Natural Science Foundation of Shandong Province (ZR2022MH031).
Author information
Authors and Affiliations
Contributions
Shun Yu conceived the study. Shun Yu and Yongxin Li designed the study. Shun Yu analyzed the data and drafted the manuscript. Yongxin Li assisted with the research and polished the manuscript. Junwei Yan, Xiaozhi Sun and Huanhuan Liu evaluated the imaging results. Meixia Fan and Lihong Yan collected the data. Mingjin Guo reviewed and approved the paper. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The research was approved by the Ethics Committee of the Affiliated Hospital of Qingdao University. Since the study data were provided by the Scientific Research Big Data Platform from our medical center, written informed consent was not obtained from the participants.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Flow chart of study.
Additional file 2: Table S1.
Clinical baseline characteristics and lipid parameters of four study groups.
Additional file 3: Table S2.
Logistic regression analysis of intracranial atherosclerotic stenosis.
Additional file 4: Table S3.
Logistic regression analysis of extracranial atherosclerotic stenosis.
Additional file 5: Table S4.
Logistic regression analysis of combined intracranial and extracranial atherosclerotic stenosis.
Additional file 6: Table S5.
Logistic regression analysis of extracranial carotid atherosclerotic stenosis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, S., Yan, L., Yan, J. et al. The predictive value of nontraditional lipid parameters for intracranial and extracranial atherosclerotic stenosis: a hospital-based observational study in China. Lipids Health Dis 22, 16 (2023). https://doi.org/10.1186/s12944-022-01761-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01761-4