Abstract
Background
Maternal lipid levels during pregnancy are critical for fetal development. Recent studies revealed that high-density lipoprotein cholesterol (HDL-c) levels during pregnancy were negatively correlated with birthweight. High-density lipoprotein 2 cholesterol (HDL2-c) is one of the major subclasses of HDL-c, and its relationship with birthweight is unclear. Association of HDL2-c concentration in the first trimester and risk of large for gestational age (LGA) was explored.
Methods
This study recruited pregnant women who registered in Fuxing Hospital from October 2018 to January 2020, had regular obstetric examinations during pregnancy, and delivered between June 2019 and September 2020. Finally, 549 participants were recruited for the study. Maternal demographic characteristics and venous blood were collected at the 6th-14th gestational week, and serum total cholesterol (TC), triglyceride (TG), HDL-c, HDL2-c, high-density lipoprotein 3 cholesterol (HDL3-c), and low-density lipoprotein cholesterol (LDL-c) concentrations were detected. Neonatal characteristics were collected at delivery. A logistic regression model was used to explore the relationship between the first trimester HDL2-c concentration and LGA incidence. A nomogram was developed, and the performance was evaluated with a concordance index.
Results
Seventy-five mothers delivered LGA infants, and the LGA incidence was 13.66%. LGA mothers had significantly lower serum HDL-c and HDL2-c concentrations than appropriate for gestational age (AGA) mothers. A logistic regression model showed that HDL2-c concentration was negatively correlated with LGA risk (odds ratio (OR) = 0.237, 95% confidence intervals (CI): 0.099–0.567, P = 0.001) when adjusted for age, prepregnancy body mass index (BMI), and parity. A nomogram was generated using all these risk factors. The area under the curve (AUC) was 0.663 (95% CI: 0.593–0.732).
Conclusions
Maternal HDL2-c concentration in the first trimester was negatively correlated with the risk of LGA.
Similar content being viewed by others
Background
High-density lipoprotein cholesterol (HDL-c) refers to cholesterol and cholesterol esters carried by HDL particles, and recently researchers found that maternal HDL-c concentrations were negatively correlated with birthweight. Misra et al. [1] found that birthweight was negatively correlated with HDL-c concentrations after the 10th week of gestation. A study by our team revealed a negative relationship between birthweight and HDL-c levels at 24th and 36th weeks of gestation [2]. A meta-analysis showed that HDL-c concentrations were reversely correlated with birthweight throughout pregnancy, especially in the third trimester [3]. In summary, maternal HDL-c levels throughout gestation were negatively associated with birthweight.
HDL particles are heterogeneous and consist of multiple subcomponents of different sizes and densities. Based on the difference in density, HDL can be divided into HDL2 and HDL3 by ultracentrifugation. HDL2 has a larger size, smaller density, and weaker antioxidant capacity than HDL3. Whether high-density lipoprotein 2 cholesterol (HDL2-c) or high-density lipoprotein 3 cholesterol (HDL3-c) plays a significant role in fetal growth and birthweight is unclear. However, some evidence suggests that HDL2-c concentration may be a critical factor. A longitudinal study showed that the lengths and head circumferences of newborns correlated negatively with the proportion of HDL2a subclasses in mothers’ plasma before delivery [4]. Another study found that compared with mothers of full-term infants, mothers of preterm infants had higher large HDL concentrations among black women [5]. Similar associations have not been reported for maternal HDL3-c levels.
Large for gestational age (LGA) refers to those newborns whose birthweight are higher than the 90th percentile of the mean birthweight or 2 standard deviations above the mean birthweight of neonates with the same gestational age. Recently, the incidence of LGA has been increasing in China, reaching 8.2%-17.7% in different regions [6]. LGA causes adverse pregnancy outcomes, such as obstructed labor [7] and neonatal asphyxia [8], as well as metabolic diseases in childhood and adulthood [9]. Recent studies found that higher HDL-c concentration was associated with a lower risk of LGA/macrosomia. Research on Chinese individuals found that increased HDL-c concentrations in the mid-pregnancy were correlated with a lower risk for macrosomia [10]. A correlation was noted between decreased HDL-c concentrations and an increased risk of LGA/macrosomia based on meta-analysis [3]. However, whether HDL2-c concentration correlates with LGA incidence has not yet been determined. In addition, early pregnancy is a critical period for fetal development, and it is of great importance to pay attention to maternal lipid levels in the early pregnancy and explore its relationship with fetal development to avoid adverse pregnancy outcomes. The study explored the correlation between HDL2-c concentration in the first trimester and birthweight using the incidence of LGA as the primary outcome measure.
Methods
Study design
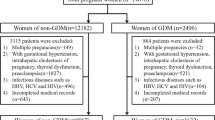
This study recruited pregnant women who registered at Fuxing Hospital from October 2018 to January 2020, had regular obstetric examinations during pregnancy, and delivered between June 2019 and September 2020 as the research population. The criteria for inclusion and exclusion are as follows. The following inclusion criteria were employed: 1) 20–40 years of age; 2) singleton pregnancy; 3) natural fertilization; and 4) first blood collection was performed before the 14th gestational week. The following exclusion criteria were employed: 1) women with infectious disease or other severe disease; 2) fetal malformation or birth defects; and 3) Apgar score < 7 at the 5th min.
Finally, 549 participants were recruited for the study.
Data collection
A questionnaire survey was conducted to obtain maternal demographic characteristics at their first hospital visit. Data collected included age, height, prepregnancy weight, gravidity, parity, disease history, education background and occupation. Neonatal data at delivery, including newborn sex, birthweight, birth length, gestational weeks, gestational weight gain (GWG), mode of delivery and perinatal outcome, were collected in this study.
Measurement of maternal blood lipids
Fasting blood samples of pregnant women were collected for measurement of total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-c), and HDL-c serum concentrations at the 6th-14th weeks. The HDL3-c concentration was measured using a single precipitation method [11]. In brief, 0.06 ml of precipitation reagent, which consisted of heparin (8.25 mg/ml), MnCl2 (98.7 mg/ml), and dextran sulfate (12 mg/ml), was added to 0.3 ml of serum. The mixture was settled at room temperature for 30 min, and centrifuged at 10,000 rpm at 4 °C for 10 min. An aliquot of the supernatant was taken for HDL3-c measurement. To correct for reagent dilution, the HDL3-c value was multiplied by 1.2. Value of HDL2-c concentration was calculated by subtracting HDL3-c from HDL-c.
Statistical analysis
Data were analyzed by SPSS 26.0 and R software. The independent sample t test and chi-square test were used to analyze the differences between the appropriate for gestational age (AGA) and LGA groups. Kendall’s tau_b correlation was used to analyze the associations between LGA incidence and maternal concentrations of HDL-c, HDL2-c, and HDL3-c as well as the ratio of HDL2-c/HDL3-c. The logistic regression model was adjusted based on maternal age, prepregnancy body mass index (BMI), gestational weight gain and parity. A P value < 0.05 was defined as significantly different. A nomogram for LGA risk was created based on the logistic regression model. The nomogram performance was evaluated by a concordance index.
Results
Maternal and neonatal characteristics
In total, 75 mothers delivered LGA infants among all 549 pregnant women, and the LGA incidence was 13.66%. The average age, prepregnancy BMI and GWG of the pregnant women were 31.4 ± 3.7 years old, 21.84 ± 2.95 kg/m2 and 13.25 ± 4.97 kg in the LGA and AGA groups, and no significant difference was detected. The average birth weight, head circumference and birth length of LGA group were significantly higher than those of AGA group, as expected. In terms of parity, neonatal sex, as well as mode of delivery, no significant difference was detected. All the results were shown in Table 1.
Association of HDL2-c concentration in the first trimester and LGA incidence
Compared to AGA mothers, LGA mothers had significantly lower serum HDL-c (1.384 ± 0.345 mmol/L vs. 1.553 ± 0.454 mmol/L) and HDL2-c concentrations (1.031 ± 0.296 mmol/L vs. 1.193 ± 0.423 mmol/L) (Fig. 1a) as well as a lower ratio of HDL2-c/HDL3-c (3.984 ± 1.710 vs. 4.484 ± 1.863) in the first trimester (Fig. 1b).
Maternal serum HDL-c, HDL2-c, and HDL3-c concentrations and HDL2-c/HDL3-c ratios in the first trimester in the AGA and LGA groups. a Maternal serum HDL-c, HDL2-c, and HDL3-c concentrations in the first trimester in the AGA and LGA groups. b The ratio of HDL2-c/HDL3-c in the AGA and LGA groups. AGA, appropriate for gestational age. LGA, large for gestational age. *P < 0.05, **P < 0.01
HDL-c, HDL2-c and HDL3-c concentrations and the ratio of HDL2-c/HDL3-c were grouped into quartiles. Compared to the group with the lowest level of HDL-c (HDL-c < 1.2275 mmol/L), the LGA incidence in the two groups with the highest HDL-c levels (1.4501 ≤ HDL-c ≤ 1.7399 mmol/L and HDL-c ≥ 1.7400 mmol/L) were significantly lower (P < 0.01, P < 0.01) (Fig. 2a). Compared to the group with the lowest level of HDL2-c (HDL2-c < 0.9015 mmol/L), the LGA incidence in the two groups with the highest HDL2-c levels (1.1040 ≤ HDL2-c ≤ 1.3464 mmol/L and HDL-c ≥ 1.3465 mmol/L) was significantly lower (P < 0.05, P < 0.01) (Fig. 2b). Compared to the group with the lowest level of the ratio of HDL2-c/HDL3-c (ratio of HDL2-c/HDL3-c < 2.6475), the LGA incidence in the group with the ratio of HDL2-c/HDL3-c (3.5800 ≤ HDL2-c/HDL3-c ≤ 4.4499) was significantly lower (P < 0.05) (Fig. 2d).
The incidence of LGA based on different maternal HDL-c, HDL2-c, and HDL3-c concentrations and HDL2-c/HDL3-c ratios in the first trimester. a The incidence of LGA based on different maternal HDL-c concentrations in the first trimester. b The incidence of LGA based on different maternal HDL2-c concentrations in the first trimester. c The incidence of LGA based on different maternal HDL3-c concentrations in the first trimester. d The incidence of LGA based on different maternal ratios of HDL2-c/HDL3-c in the first trimester. LGA, large for gestational age. AGA, appropriate for gestational age. *P value < 0.05, **P value < 0.01
Kendall’s tau_b correlations were used to explore the association between the incidence of LGA and HDL-c, HDL2-c, and HDL3-c concentrations as well as the ratio of HDL2-c/HDL3-c. Concentrations of HDL-c, HDL2-c and HDL3-c and the ratio of HDL2-c/HDL3-c were grouped into quartiles. Table 2 shows that the HDL-c and HDL2-c concentrations and the ratio of HDL2-c/HDL3-c were negatively associated with LGA incidence (P < 0.01, P < 0.01, P < 0.05), yet no correlation was found between HDL3-c concentration and the LGA incidence.
A Logistic regression was performed to explore the association between maternal HDL2-c concentration in the first trimester and the risk of LGA. The model was adjusted by maternal age, pre-BMI, GWG, and parity. HDL2-c concentration (OR = 0.237, P = 0.001) was a protective factor for LGA. A 1 mmol/L increase in HDL2-c concentration was associated with a 23.7% decrease in the incidence of LGA (95% CI 0.099–0.567). GWG (OR = 1.059, P = 0.034) was positively associated with the risk of LGA (Table 3). Then, a nomogram was created using all these factors (Fig. 3). The area under the curve (AUC) was 0.663 (95% CI 0.593–0.732) (Fig. 4).
Nomogram for the risk of LGA. To estimate the probability of LGA, the values of a pregnant woman value were marked at each axis. A straight line was drawn perpendicular to the point axis, and the points for all variables were summed. Next, the sum was noted on the total point axis, and a straight line was drawn perpendicular to the probability axis. LGA, large for gestational age. GWG, gestational weight gain. BMI, body mass index
Discussion
HDL is the predominant lipoprotein in follicular fluid (FF). FF provides cholesterol for steroid production [12], and regulates intrafollicular cholesterol homeostasis [13]. HDL improves oocyte quality and early embryonic development, which may be related to the antioxidant defense capacity of ApoAI and PON1 [14, 15]. However, recent studies have shown that maternal HDL-c levels throughout the gestation were inversely correlated with newborns’ birth weight. Misra et al. [1] found that birthweight was negatively correlated with HDL-c concentrations after the 10th week of gestation. Each 1 mg/dl increase in maternal HDL-c concentration was correlated with a 6.4 g reduction in birthweight in mothers with normal weight and a 13 g reduction in birthweight in those who were overweight or obese. According to a previous study by our team, birthweight was negatively correlated with maternal HDL-c concentrations in the middle and late pregnancies. Small for gestational age (SGA) mothers had higher HDL-c concentrations at 16–20 gestational weeks compared to AGA mothers [16], whereas LGA mothers had lower HDL-c concentrations in the third gestation [17]. Research on the Chinese pregnant women showed that low HDL-c levels were correlated with higher risk of macrosomia as well as lower incidence of SGA [10]. In this study, LGA mothers had significantly lower serum HDL-c concentrations than AGA mothers, and maternal HDL-c concentration was negatively associated with the risk of LGA. These findings were consistent with previous studies.
Based on the difference in density, HDL can be divided into HDL2 and HDL3 by ultracentrifugation. Density of HDL2 was 1.063–1.125 g/ml and density of HDL3 was of 1.125–1.210 g/ml. HDL2 has a larger size and weaker antioxidant capacity than HDL3 [18]. Although whether HDL2 or HDL3 plays a critical role in fetal growth and birthweight is unclear, some evidence suggests that HDL2-c concentration may be a critical factor. During pregnancy, the HDL2b proportion increased greatly, representing the most predominant subfraction in late pregnancy, which may be associated with estrogen [19]. A study found that the mothers of preterm infants had higher large HDL concentrations than those of full-term infants in black women [5]. Another study also revealed that mothers of macrosomia had significantly lower HDL2-c concentrations than mothers with AGA infants in the first and third trimesters, regardless of prepregnancy BMI [20]. A longitudinal study showed that the lengths and head circumferences of newborns correlated negatively with the proportion of the HDL2a subclass in mothers’ plasma before delivery [4].
In the present study, HDL2-c concentrations of LGA mothers were significantly lower than those of AGA mothers, but HDL3-c concentrations didn’t differ between two groups. In addition, a negative correlation between HDL2-c concentration and the risk of LGA was found in this study. The logistic regression model showed that when adjusted by maternal age, prepregnancy BMI, and parity, HDL2-c concentration was negatively correlated with the risk of LGA (OR = 0.237, 95% CI: 0.099–0.567, p = 0.001). Each 1 mmol/L increase in HDL2-c concentration decreased the risk of LGA by 23.7%. The study also created a nomogram for the risk of LGA using the factors included in the logistic regression model: age, prepregnancy BMI, parity, GWG and HDL2-c concentration in the first trimester. A concordance index was used to evaluate nomogram performance and the AUC was 0.693, indicating a certain discriminative ability. The nomogram suggested that high GWG and low HDL2-c concentrations were the major risk factors for LGA.
The decrease in total antioxidant capacity of HDL particles may be the mechanism involved in the association between HDL2-c levels and the proportion of HDL2-c and fetal development. HDL antioxidant function is mainly realized by ApoA-I, PON1, PAF-AH and other components. Studies have found that ApoA-I is more enriched in small and dense HDL3-c compared to HDL2a and HDL2b [21], and PON1 is mainly present in the HDL3 subclass [22]. In addition, PAF-AH enzymatic activity is also preferentially localized in HDL3. The antioxidant activity of HDL subclasses decreases with density : HDL3c > HDL3b > HDL3a > HDL2b > HDL2a [23]. Decreased HDL3-c concentrations were strongly correlated with an higher risk of cardiovascular diseases (for example, coronary heart disease) and death, whereas HDL2 lacked such associations [24]. The proportion of HDL2b increases significantly during pregnancy and becomes the predominant HDL subcomponent in the third trimester [19]. During pregnancy, the levels of serum lipids increase, and oxidative stress in the body increases. HDL particles with normal physiological functions can reduce the level of oxidative stress through antioxidant effects. With high HDL2-c levels, the total antioxidant capacity of HDL particles decreases, resulting in the inability to effectively suppress oxidative stress levels. A systematic review showed that the serum antioxidant capacity of pregnant women who delivered fetal growth restriction neonates was attenuated and that oxidative stress was enhanced [25]. When HDL2-c levels and its proportion increase, the total antioxidant capacity of HDL particles decreases, which is not conducive to fetal growth and development. From another perspective, it also reduces the risk of LGA.
In recent years, the incidence of LGA in infants has been increasing in China, reaching 8.2%-17.7% in different regions. The incidence of LGA in our study was 13.66%. Women who delivered LGA infants are more likely to have pregnancy complications, including cephalopelvic disproportion and postpartum hemorrhage. Regarding birth outcomes, LGA infants were more likely to get shoulder dystocia, neonatal injury, birth asphyxia and neonatal death. LGA was confirmed to be associated with maternal hyperglycemia, hypertriglyceridemia, obesity, excessive GWG and advanced age. Although the results showed a reverse association between maternal cholesterol levels and LGA incidence, it is important to control cholesterol levels during pregnancy given that abnormal elevation showed an adverse effect on birthweight, which may result in fetal growth restriction, low birth weight and SGA.
Comparisons with other studies and what does the current work add to the existing knowledge
Previous studies have typically focused on TC and HDL-c levels in mid-pregnancy or late pregnancy and explored their relationship with birthweight. The present study focused on maternal HDL2-c concentrations in the first trimester and found a negative association with the risk of LGA.
Study strength and limitations
The present study not only found a negative association between maternal HDL-c concentration and LGA incidence, but also revealed that maternal HDL2-c concentration in the first trimester was negatively associated with the risk of LGA. However, this study had some limitations. First, when exploring the association between HDL2-c concentration and birthweight, SGA infants were excluded. In addition, information on pregnant women lifestyle wasn’t collected. For instance, pregnancy diet and physical activity, and these may be confounders. It is necessary to explore the relationship between maternal HDL2-c concentration and SGA incidence to elucidate its effect on birthweight, and maternal lifestyle should be taken into account in these studies.
Conclusion
In conclusion, high maternal HDL-c and HDL2-c levels in the first trimester were negatively correlated with the risk of LGA. For pregnant women, it is important to detect and monitor maternal HDL2-c concentrations in the early pregnancy to evaluate embryonic and fetal development and avoid adverse birth outcomes.
Availability of data and materials
The datasets analyzed during the current study are not publicly available because they are also part of an ongoing study but are available from the corresponding author on reasonable request.
Abbreviations
- AGA:
-
Appropriate for gestational age
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- FF:
-
Follicular fluid
- GWG:
-
Gestational weight gain
- HDL-c:
-
High-density lipoprotein cholesterol
- HDL2-c:
-
High-density lipoprotein 2 cholesterol
- HDL3-c:
-
High-density lipoprotein 3 cholesterol
- LDL-c:
-
Low-density lipoprotein cholesterol
- LGA:
-
Large for gestational age
- OR:
-
Odds ratio
- SGA:
-
Small for gestational age
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
References
Misra VK, Trudeau S, Perni U. Maternal serum lipids during pregnancy and infant birth weight: the influence of prepregnancy BMI. Obesity. 2011;19(7):1476–81.
Wang H, Dang Q, Zhu H, et al. Associations between maternal serum HDL-c concentrations during pregnancy and neonatal birth weight: a population-based cohort study. Lipids Health Dis. 2020;19(1):93.
Wang J, Moore D, Subramanian A, et al. Gestational dyslipidaemia and adverse birthweight outcomes: a systematic review and meta-analysis. Obes Rev. 2018;19(9):1256–68.
Zeljkovic A, Vekic J, Spasic S, et al. Changes in LDL and HDL subclasses in normal pregnancy and associations with birth weight, birth length and head circumference. Matern Child Health J. 2013;17(3):556–65.
Catov JM, Mackey RH, Scifres CM, Bertolet M, Simhan HN. Lipoprotein heterogeneity early in pregnancy and preterm birth. Am J Perinatol. 2017;34(13):1326–32.
Zhu L, et al. Chinese neonatal birth weight curve for different gestational age. Zhonghua Er Ke Za Zhi. 2015;53(2):97–103.
Spellacy WN, Miller S, Winegar A, Peterson PQ. Macrosomia–maternal characteristics and infant complications. Obstet Gynecol. 1985;66(2):158–61.
Boulet SL, Salihu HM, Alexander GR. Mode of delivery and birth outcomes of macrosomic infants. J Obstet Gynaecol. 2004;24(6):622–9.
Eriksson J, Forsén T, Tuomilehto J, Osmond C, Barker D. Size at birth, childhood growth and obesity in adult life. Int J Obes Relat Metab Disord. 2001;25(5):735–40.
Jin WY, Lin SL, Hou RL, et al. Associations between maternal lipid profile and pregnancy complications and perinatal outcomes: a population-based study from China. BMC Pregnancy Childbirth. 2016;16:60.
Hirano T, Nohtomi K, Koba S, Muroi A, Ito Y. A simple and precise method for measuring HDL-cholesterol subfractions by a single precipitation followed by homogenous HDL-cholesterol assay. J Lipid Res. 2008;49(5):1130–6.
Jaspard B, Collet X, Barbaras R, et al. Biochemical characterization of pre-beta 1 high-density lipoprotein from human ovarian follicular fluid: evidence for the presence of a lipid core. Biochemistry. 1996;35(5):1352–7.
Fujimoto VY, Kane JP, Ishida BY, Bloom MS, Browne RW. High-density lipoprotein metabolism and the human embryo. Hum Reprod Update. 2010;16(1):20–38.
Browne RW, Shelly WB, Bloom MS, et al. Distributions of high-density lipoprotein particle components in human follicular fluid and sera and their associations with embryo morphology parameters during IVF. Hum Reprod. 2008;23(8):1884–94.
Rincón J, Madeira EM, Campos FT, et al. Exogenous paraoxonase-1 during oocyte maturation improves bovine embryo development in vitro. Reprod Domest Anim. 2016;51(5):827–30.
Kramer MS, Kahn SR, Dahhou M, et al. Maternal lipids and small for gestational age birth at term. J Pediatr. 2013;163(4):983–8.
Hou RL, Zhou HH, Chen XY, Wang XM, Shao J, Zhao ZY. Effect of maternal lipid profile, C-peptide, insulin, and HBA1c levels during late pregnancy on large-for-gestational age newborns. World J Pediatr. 2014;10(2):175–81.
Brites F, Martin M, Guillas I, Kontush A. Antioxidative activity of high-density lipoprotein (HDL): Mechanistic insights into potential clinical benefit. BBA Clin. 2017;8:66–77.
Alvarez JJ, Montelongo A, Iglesias A, Lasunción MA, Herrera E. Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women. J Lipid Res. 1996;37(2):299–308.
Merzouk H, Meghelli-Bouchenak M, Loukidi B, Prost J, Belleville J. Impaired serum lipids and lipoproteins in fetal macrosomia related to maternal obesity. Biol Neonate. 2000;77(1):17–24.
Kontush A, Therond P, Zerrad A, et al. Preferential sphingosine-1-phosphate enrichment and sphingomyelin depletion are key features of small dense HDL3 particles: relevance to antiapoptotic and antioxidative activities. Arterioscler Thromb Vasc Biol. 2007;27(8):1843–9.
Davidson WS, Silva RA, Chantepie S, Lagor WR, Chapman MJ, Kontush A. Proteomic analysis of defined HDL subpopulations reveals particle-specific protein clusters: relevance to antioxidative function. Arterioscler Thromb Vasc Biol. 2009;29(6):870–6.
Kontush A, Chantepie S, Chapman MJ. Small, dense HDL particles exert potent protection of atherogenic LDL against oxidative stress. Arterioscler Thromb Vasc Biol. 2003;23(10):1881–8.
Martin SS, Jones SR, Toth PP. High-density lipoprotein subfractions: current views and clinical practice applications. Trends Endocrinol Metab. 2014;25(7):329–36.
Hart B, Morgan E, Alejandro EU. Nutrient sensor signaling pathways and cellular stress in fetal growth restriction. J Mol Endocrinol. 2019;62(2):R155–65.
Acknowledgements
We thank the participants in the study for their support and the staff of the laboratory and Obstetrical Department at Fuxing Hospital for their help.
Funding
This work was supported by the National Natural Science Foundation of China [No. 8187120380].
Author information
Authors and Affiliations
Contributions
HLY and DXH designed the study. QYD, YDZ and DXH analyzed the data. DXH drafted the manuscript. HYZ, QY, XXC, NL, HLW, XYZ, and YDZ helped in collecting blood samples and data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved in accordance with the requirements of the Ethics Committee of Capital Medical University (2018SY04). Informed consent for the scientific use of biological materials was obtained from all patients before enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests with respect to this research study and paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, D., Zhu, H., Zhu, Y. et al. Association of maternal HDL2-c concentration in the first trimester and the risk of large for gestational age birth. Lipids Health Dis 21, 71 (2022). https://doi.org/10.1186/s12944-022-01688-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01688-w