Abstract
This review focuses on antisense oligonucleotides and small interfering ribonucleic acid therapies approved or under development for the management of lipid disorders. Recent advances in RNA-based therapeutics allow tissue-specific targeting improving safety. Multiple potential target proteins have been identified and RNA-based therapeutics have the potential to significantly improve outcomes for patients with or at risk for atherosclerotic cardiovascular disease. The advantages of RNA-based lipid modifying therapies include the ability to reduce the concentration of almost any target protein highly selectively, allowing for more precise control of metabolic pathways than can often be achieved with small molecule-based drugs. RNA-based lipid modifying therapies also make it possible to reduce the expression of target proteins for which there are no small molecule inhibitors. RNA-based therapies can also reduce pill burden as their administration schedule typically varies from weekly to twice yearly injections. The safety profile of most current RNA-based lipid therapies is acceptable but adverse events associated with various therapies targeting lipid pathways have included injection site reactions, inflammatory reactions, hepatic steatosis and thrombocytopenia. While the body of evidence for these therapies is expanding, clinical experience with these therapies is currently limited in duration and the results of long-term studies are eagerly awaited.
Similar content being viewed by others
Introduction
Cardiovascular disease remains the leading cause of mortality globally, accounting for approximately 17.9 million deaths in 2016 [1]. Approximately 85% of these deaths were due to myocardial infarction or stroke. The European Society of Cardiology estimates that more than one in three of all potential years of life lost can be attributed to death from cardiovascular disease [2]. Unfavorable concentrations of plasma lipoproteins such as low-density lipoprotein (LDL), remnant lipoproteins or lipoprotein (a) (Lp(a)) contribute causally to the pathogenesis of atherosclerotic cardiovascular disease (ASCVD). While a healthy lifestyle can reduce the risk of cardiovascular disease, some individuals require medication, such as statins, to lower atherogenic lipoproteins sufficiently.
Pharmacotherapy for cardiovascular diseases was for many years almost entirely reliant on small molecules with antibody-based therapies introduced less than 10 years ago. While these therapies are highly effective in many conditions, the identification of novel drug targets brought the need for highly targeted RNA-based therapies treatments to the fore [3]. The stability of RNA-based therapies, and concerns regarding the potential for late complications of drugs with long half-lives as well as the need to demonstrate improved clinical outcomes have resulted in an extended development period for these treatments (Fig. 1) [3].
Development of RNA-based therapies for the treatment of cardiovascular and other disorders. AsO: antisense oligonucleotides; FDA: Food and Drug Administration; EMA: European Medicines Agency; CV: cardiovascular; HoFH: homozygous familial hypercholesterolemia; siRNA: small interfering ribonucleic acids; hATTR: hereditary transthyretin amyloidosis; Lp(a): lipoprotein(a)
Nucleic acid-based therapies, including antisense oligonucleotides (AsO) and small interfering ribonucleic acids (siRNA) strategies, allow for selective gene silencing, therefore preventing production of proteins that may cause or exacerbate disease states. Figure 2 illustrates the mechanisms of action of AsO and siRNA therapies.
The RNase-mediated mechanism of action of AsOs is demonstrated here. AsOs are administered as chemically stabilized single stranded oligonucleotides that bind to target mRNA and thereafter recruit RNase H to cleave the target mRNA. RNA interference treatments are administered as double stranded mRNA. After administration, the passenger strand dissociates while the guide strand binds to the RNA-induced silencing (RISC) complex resulting in cleavage of target mRNA.
AsO: antisense oligonucleotides; ssDNA: single strand deoxyribonucleic acid; mRNA: messenger ribonucleic acid; RISC: RNA-induced silencing complex.
While both these strategies silence the expression of a particular gene, there are important differences between them. AsOs are chemically stabilized, single-stranded oligonucleotides that that selectively inhibit the translation of mRNA through a variety of mechanisms, including RNase H1-mediated cleavage of mRNA as illustrated above, alteration of pre-mRNA splicing and modulation of mRNA translation [4,5,6,7]. siRNA therapeutics, on the other hand, are double stranded RNA fragments that are incorporated into the RNA-induced silencing complex (RISC) resulting in selective cleaving of mRNA [6, 7]. The resulting cleaved mRNA sequences are not translated to the target protein.
FDA approval has been granted to several RNA-based therapies (Table 1). Several other RNA-based therapies are currently undergoing clinical development and show potential as treatment for cardiovascular diseases.
This review focuses on AsO and siRNA therapies under development for the management of lipid disorders (Table 2).
Targeting LDL
LDL is the most abundant of the ApoB-containing lipoproteins and is widely recognized as a modifiable risk factor for ASCVD [21]. Data from epidemiological studies, Mendelian randomization studies, animal studies and clinical trials show conclusively that elevated levels of LDL cholesterol (LDL-C) and duration of exposure to these elevated levels are causally related to the risk of developing atherosclerotic cardiovascular disease [22, 23]. Indeed, in a meta-regression analysis of 49 clinical trials with 312,175 participants, each 1-mmol/L (38.7-mg/dL) reduction in LDL-C level was associated with a relative risk (RR) of major vascular events of 0.77 (95% CI, 0.71 to 0.84; P < .001) for statins and 0.75 (95% CI, 0.66 to 0.86; P = .002) for established non-statin interventions that act primarily via upregulation of LDL receptor expression [24].
Current European lipid treatment guidelines suggest an LDL-C target of 1.8 mmol/L and 1.4 mmol/L for high-risk patients and very high-risk patients, respectively [25]. Additionally, LDL-C should be reduced by at least 50% from the untreated baseline [25]. While lipid-lowering therapy such as statins and ezetimibe are sufficient for goal attainment in many patients, markedly elevated LDL-C at baseline, as seen for instance in patients with familial hypercholesterolemia (FH), often prevents patients from reaching their LDL-C goal. Furthermore, poor adherence to treatment, tolerability concerns and elevated expression of PCSK9 as result of statin treatment may detract from effective management of hyperlipidemia [26]. For these patients inhibitors/neutralizers of PCSK9, such as the monoclonal antibodies alirocumab and evolocumab, or RNA-based therapy such as inclisiran may be considered [25].
PCSK-9 targeted RNA-based therapy
CiVi007
Background information
CiVi007 is a third generation AsO targeted against PCSK9 mRNA [13]. Administration of an AsO such as CiVi007 results in reduced hepatic production of PCSK9 protein, decreased degradation of LDL receptors (LDLR) and an increased number of LDLR on the hepatic cell surface available to bind circulating LDL [14]. The subsequent reduction in plasma LDL-C concentration is longer lasting than that achieved with traditional small molecules such as statins.
Interestingly, this molecule is under development in subcutaneous and oral formulations and a once monthly dosing schedule is expected [27].
Clinical development: efficacy
A phase 1, first in human, placebo-controlled, single blind, randomized study was recently completed in 36 patients with elevated LDL-C (NCT03427710). This study assessed the safety, tolerability as well as pharmacokinetic and pharmacodynamic characteristics of CiVi007. Subsequently a phase 2a, placebo-controlled, randomized study assessing safety, tolerability and pharmacokinetic and pharmacodynamic characteristics of CiVi007 in patients on concomitant statin therapy has also recently been completed (NCT04164888). Results of these studies are not currently available.
Clinical development: safety
Safety information for CiVi007 is currently unavailable.
Inclisiran
Background information
The siRNA inclisiran silences the intracellular translation of PCSK9 mRNA by mimicking the physiological process of RNA interference. Inclisiran consists of a double-stranded siRNA conjugated to a synthetic ligand, GalNAc, which binds selectively to the asialoglycoprotein receptor (ASGPR) expressed mainly on the surface of hepatocytes [28, 29].
Once inclisiran is internalised into hepatocytes through endocytosis, the guide (antisense) strand dissociates from the passenger strand and enters the RISC. This complex selectively binds to PCSK9 mRNA and cleaves it, thereby inhibiting the translation of its protein [30]. As the complex of inclisiran siRNA in the RISC complex is not readily degraded by cellular nucleases, its effect on PCSK9 levels is durable: it has been reported that PCSK9 levels are reduced by approximately 50% from baseline for up to 180 days after subcutaneous administration of 300 mg of inclisiran sodium [14, 31].
Clinical development: efficacy
The clinical development of inclisiran started in 2011 with a small dose finding study in healthy volunteers [32] and is currently still ongoing in the ORION and VICTORION programs [33]. At the time of publication results of the trials in the VICTORION program are unavailable. A diverse population of hypercholesterolemic patients including patients with homozygous familial hypercholesterolemia (HoFH) and heterozygous familial hypercholesterolemia (HeFH) participated in the ORION program and the results of the phase 3 studies will be briefly discussed (also see Table 3).
The efficacy of inclisiran in patients diagnosed with HoFH was investigated in the ORION-2 and the ongoing ORION-5 studies [44]. The proof-of-concept ORION-2 single-arm, open-label, multicenter study enrolled four HoFH patients who received inclisiran sodium 300 mg as add-on to background lipid-lowering therapy consisting of high-intensity statins and ezetimibe. PCSK9 was reduced in all patients (− 40.2 to − 80.5% at day 180), while LDL-C reductions of − 17.5 to − 37.0% were reported for patients B, C and D at day 180, and no effect was observed in patient A. Patient A had a history of poor responses to both alirocumab and evolocumab [44]. As inclisiran and monoclonal antibodies directed against PCSK9 both work by indirectly upregulating LDL receptors, inclisiran is unlikely to be effective in patients with HoFH who do not have residual LDL receptor function. Based on the efficacy and safety reported in ORION-2, the ORION-5 study was initiated in 2019 and is currently ongoing (NCT03851705).
Results from three phase 3 studies, ORION-9, − 10 and − 11, were published recently [45, 46] and all demonstrate the efficacy of inclisiran in lowering LDL-C over a period of 510 days. In these studies, patients were randomized to receive inclisiran (300 mg SC) or placebo on days 1, 90, 270 and 450 as add-on to statin and/or ezetimibe treatment. A between-group difference in LDL-C of − 47.9% (95% CI, − 53.5 to − 42.3; P < 0.001) was observed at day 510 in patients with HeFH in ORION-9 [28]. Ray and colleagues (2020) [46] reported a between-group difference in LDL-C of − 52.3% (95% CI, − 55.7 to − 48.8; P < 0.001) at day 510 in patients with established ASCVD in the ORION-10 study. Similarly, a between-group difference of − 49.9% in LDL-C at day 510 (95% CI, − 53.1 to − 46.6; P < 0.001) was reported in a patient population with established ASCVD or ASCVD risk equivalents in ORION-11 [45]. The ORION-8 study, an open-label extension of ORION-9, − 10 and − 11, evaluating long-term safety is currently ongoing (NCT03814187).
Two cardiovascular outcomes trials (CVOT), ORION-4 (NCT03705234) and VICTORION-2 PREVENT (NCT05030428), comparing inclisiran to placebo in patients with established ASCVD with background lipid-lowering therapy are currently ongoing.
Clinical development: safety
Overall, inclisiran is well tolerated [32, 45, 46]. Adverse events reported by patients receiving inclisiran included injection site reactions, headache [32], nasopharyngitis, back pain, bronchitis and upper respiratory tract infections [45, 46]. Of these, mild and moderate injection site reactions are the most noteworthy. Antidrug antibodies were detected in fewer than 2.6% of patients but did not appear to affect pharmacokinetic variables or efficacy [45, 46].
In the ORION-10 study, a risk ratio of 0.7 (95% CI, 0.5 to 1.0) was reported for the prespecified exploratory cardiovascular endpoint, which included death due to CV causes, cardiac arrest, nonfatal myocardial infarction and stroke [46]. The study investigators highlighted that the overall number of events was too limited to make firm conclusions regarding improvements in cardiovascular endpoints [46].
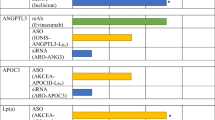
Additional LDL-C-lowering therapeutic options under development
Vupanorsen, a second generation AsO [18], and ARO-ANG3, an siRNA [37], both selectively inhibit hepatic translation of ANGPTL3 mRNA and are currently under development for the management of elevated triglycerides and LDL-C. These molecules are described in greater detail in the section on drugs interfering with the metabolism of triglyceride-rich lipoproteins.
Apo-B targeted RNA-based therapy
The apolipoprotein B (ApoB) gene is located on chromosome 2 and contains 29 exons [18]. ApoB RNA editing results in two distinct forms of apoB: ApoB100 and ApoB48 [47]. ApoB100 is expressed in the liver and is the structural apoprotein of very-low-density lipoproteins (VLDL) and ultimately LDL, while ApoB48 is expressed in the intestinal tract and is essential for the formation of chylomicrons (CM) [48].
ApoB100 is found in VLDL, IDL, LDL and Lp(a). Each lipoprotein particle contains a single apoB100 molecule. ApoB100 binds to the LDLR allowing for the clearance of ApoB-containing lipoproteins from the circulation. Inhibition of ApoB production (either in the liver or intestines) would result in reduced export of either VLDL and/or chylomicrons providing a lipid-lowering mechanism that is independent of receptor mediated lipoprotein clearance.
Mipomersen (ISIS301012)
Background information
The AsO, mipomersen, selectively silences the mRNA responsible for the coding of ApoB100, thereby reducing ApoB100 concentrations [34].
Mipomersen is administered at a dose of 200 mg once weekly and has shown LDL-C reductions of approximately 30% in various patient populations [34, 35, 49].
Clinical development: efficacy
Raal and colleagues (2010) [34] conducted a multicenter, randomized, double-blind study to investigate the efficacy of mipomersen at 200 mg once weekly in 49 patients with HoFH over a 26-week period. Mean reductions in LDL-C from baseline were 24.7% for mipomersen, and 3.3% for placebo (P = 0.0003) [34]. The response to mipomersen was highly variable, ranging from a decrease of 82% to an increase of 2%.
The efficacy of mipomersen in patients with severe hypercholesterolemia (LDL-C at baseline ≥5.1 mmol/L) was evaluated in a randomized, multicenter, double-blind study comparing mipomersen 200 mg SC weekly with placebo in 58 patients on background lipid-lowering therapy [35]. At the end of the 26-week study period, LDL-C levels were reduced by 35.9% with mipomersen treatment (baseline LDL-C of 7.2 mmol/dL) and by 12.5% with placebo treatment (baseline LDL-C of 6.5 mmol/dL) (P < 0.001) [35]. Stein et al., (2012) [50] conducted a similar 26-week, multicenter, double-blind, randomized study in patients with HeFH and coronary artery disease on background statin therapy. An LDL-C reduction of 28% was demonstrated with mipomersen treatment, compared with 5.2% for placebo (P < 0.001) [50]. A systematic review and meta-analysis of mipomersen trials is presented in [51].
Key mipomersen studies are briefly summarized in Table 3.
Clinical development: safety
The most commonly reported adverse events during the clinical development program of mipomersen included injection site reactions (erythema, pruritus, pain and post-inflammatory hyperpigmentation), fatigue, pyrexia, chills, malaise, myalgia, and arthralgia [34, 35, 49]. Hepatic AEs (alanine aminotransferase (ALT) elevations and hepatic steatosis) were common in the mipomersen arm. The incidence of renal adverse events was similar across both the mipomersen and placebo arms [35]. The occurrence of cardiac events, including angina, MI, cardiac failure, CAD, and supraventricular extrasystoles was higher in the mipomersen arm (12 events vs one event) [35].
Based on these results the FDA issued a black box warning for mipomersen, stipulating increased risk for hepatotoxicity due to the association of mipomersen with elevated ALT and hepatic steatosis [50]. Hepatotoxicity was noted as early as 6 months after treatment initiation [52]. The European Medicines Agency did not grant mipomersen marketing approval because of concerns regarding high dropout rates from clinical trials over a period of 2 years, hepatic toxicity and increased cardiovascular event rates [53]. Marketing of mipomersen has subsequently been discontinued.
Lp(a)-targeted RNA-based therapy
Lp(a) consists of one LDL particle covalently bound to apolipoprotein(a) (apo(a)). Lp(a) levels are predominantly genetically determined and may vary several hundredfold amongst individuals. Loop-like structures, referred to as kringles, are present on apo(a) in variable numbers [54]. Genetic studies have demonstrated an association between the number of kringle IV type 2 repeats and the risk for coronary heart disease [55]. Lp(a) is rich in oxidized phospholipids and has proatherogenic, proinflammatory and prothrombotic effects and is recognized as an inherited, independent and causal risk factor for cardiovascular disease [56, 57].
Lp(a) values > 50 mg/dL in Caucasians are associated with increased cardiovascular risk [58]. Currently there are no approved pharmacological therapies that target Lp(a). The only highly effective option for lowering Lp(a) is lipoprotein apheresis which results in a time-averaged 30–35% reduction in Lp(a) [59]. Treatment with niacin or PCKS9 mAbs lowers Lp(a) modestly by 20–30% [60, 61] which is unlikely to provide significant clinical benefit as a Mendelian randomization analysis indicates that large absolute reductions in Lp(a) are likely required to meaningfully reduce the risk of coronary artery disease [62].
Pelacarsen (TQJ230/AKCEA-APO(a)-LRx/IONIS-APO(a)-LRx)
Background information
The AsO pelacarsen selectively inhibits the production of apo(a) by targeting LPA mRNA. Conjugation to the synthetic GalNAc ligand ensures selective inhibition of hepatic apo(a) synthesis, the main site of Lp(a) synthesis [16, 28, 29].
The extended half-life of pelacarsen of approximately 1 month translates into infrequent administration.
Clinical development: efficacy
Several clinical studies evaluating the efficacy and safety of pelacarsen have been completed. A dose-ranging phase 2 trial was conducted in patients with established CVD and Lp(a) > 60 mg/dL. Patients were randomly assigned to treatment with varying doses of pelacarsen (20 mg QW or Q2W or Q4W, 40 mg Q4W, 60 mg Q4W) over a six-month period [63]. Reduction in Lp(a) levels of 72% was observed in patients receiving 60 mg Q4W while patients treated with 20 mg QW showed an 80% reduction in Lp(a) (Table 3). This effect became apparent by Week 4, with near maximal effect reached by Week 16 after the last dose [16].
A phase 3 CVOT (Lp(a) HORIZON, NCT04023552) evaluating the effect of pelacarsen on major cardiovascular events in patients with Lp(a) ≥ 70 or ≥ 90 mg/dL is currently underway.
Clinical development: safety
Thus far, clinical experience with pelacarsen indicates that the treatment is well-tolerated. The most common adverse events reported to date are injection site reactions, flu-like symptoms, headache, urinary tract infections and fatigue [16]. No marked effects on liver function, renal function or platelet count have been reported [16].
Olpasiran (AMG890)
Background information
Olpasiran is an siRNA which selectively inhibits the transcription of LPA mRNA restricting production of Lp(a) [17, 63].
Studies indicate sustained Lp(a) reduction of up to 80% for 6 months after administration of a single dose of olpasiran [17].
Clinical development: efficacy
Results from a phase 1 study in 64 healthy adults demonstrated that a single dose of olpasiran at 9 or 75 mg reduced Lp(a) levels after 43 days by 75 and 89%, respectively [64] (refer to Table 3). Phase 1 and 2 clinical trials are presently ongoing to determine the safety and tolerability of olpasiran in patients with elevated plasma Lp(a) (NCT03626662, NCT04270760). Primary completion for the phase 2 study (NCT04270760) was reached in December 2021; however, at time of submission full results were not yet available.
Clinical development: safety
Adverse events reported during the phase 1 study included headache (10% AMG890, 25% placebo) and upper respiratory tract infections (15% AMG890, 13% placebo). No serious safety concerns were identified [17].
Triglyceride-rich lipoprotein targeted RNA based therapy
It was previously thought that reduced levels of high-density lipoprotein (HDL-C) are causally associated with increased cardiovascular risk. However, an inverse relationship between HDL-C and triglycerides (TG) exists [65, 66] and new evidence suggest that hypertriglyceridemia and the concomitant increase in remnant cholesterol, rather than low levels of HDL-C, are causally linked to cardiovascular disease [67, 68].
Remnant cholesterol is defined as the cholesterol content of all triglyceride-rich lipoproteins, i.e., chylomicron remnants, VLDL, and intermediate-density lipoproteins (IDL) in the fasting or non-fasting states [68]. Triglyceride-rich lipoproteins are larger than LDL and carry 5–20 times more cholesterol per particle [69]. Triglycerides in triglyceride-rich lipoproteins are enzymatically degraded by various lipases such as lipoprotein lipase and hepatic lipase resulting in the formation of smaller, denser lipoproteins enriched in cholesterol. Cholesterol in these remnant lipoproteins readily accumulates in intimal foam cells contributing to plaque formation [68]. Dysregulation of triglyceride metabolism is associated with increased cardiovascular risk and therefore presents a potential therapeutic target. Indeed, results from the LURIC study demonstrated that low levels of hepatic lipase, the enzyme responsible for facilitating clearance of triglycerides from intermediate-density lipoprotein (IDL) to form LDL, are associated with increased cardiovascular risk [70].
Mendelian randomization studies have demonstrated that modulation of lipoprotein lipase (LPL) levels reduces cardiovascular risk [71]. In addition, other genes affecting triglyceride metabolism and thus cardiovascular risk have also been identified: APOA5, APOC3 and TRIB1 [67]. Two of these genes are currently being investigated as potential targets for modulating triglyceride metabolism using nucleic acid-based therapies: angiopoietin-like protein 3 (ANGPTL3) and apolipoprotein C3 (apoC3).
Angiopoietin-like protein 3 (ANGPTL3) is expressed and secreted by the liver and affects lipolysis and clearance of triglyceride-rich lipoproteins and remnants through reversible inhibition of LPL, inhibition of endothelial lipase and activation of lipolysis in adipocytes [18, 72]. Genetic studies have demonstrated that individuals with loss-of-function mutations in ANGPTL3 have extremely low levels of most plasma lipoproteins and a reduced risk of coronary artery disease [73, 74]. ANGPTL3 levels in the circulation can be reduced with monoclonal antibodies, such as evinacumab, or by reducing production either with an antisense oligonucleotide or small interfering RNA approach. ANGPTL4 is also involved in the regulation of lipolysis and clearance of triglyceride-rich lipoproteins and is thus a potentially promising target but ANGPTL4-null mice display an adverse phenotype characterized by growth arrest, anorexia, intestinal fibrosis and ultimately death making ANGPTL3 the more attractive target [18, 75].
Apolipoprotein C3 (apoC3) is an apoprotein found predominantly on triglyceride-rich lipoproteins and inhibits lipoprotein lipase mediated lipolysis [76], thereby increasing plasma triglyceride levels. Additionally, apolipoprotein C3 is implicated in impairing the hepatic uptake and degradation of triglyceride-rich lipoproteins by LDL receptors [77], suggesting that inhibition of apoC3 may reduce residual cardiovascular risk. Indeed, genome-wide association studies have demonstrated that a null mutation in the APOC3 gene results in reduced expression of apolipoprotein C3, extremely low levels of triglycerides and reduced risk of cardiovascular disease [78,79,80].
Treatment goals specific for triglyceride levels in cardiovascular risk reduction have not yet been set in all lipid guidelines, though the American College of Cardiology recently published a consensus treatment pathway for patients with ASCVD and persistent hypertriglyceridemia [25, 81]. If TG remain persistently elevated (> 1.7 mmol/L) despite lifestyle modification pharmacological intervention should be considered. Several therapies are currently available to lower TG levels including fibrates, icosapent ethyl and statins [25] while four RNA-based therapies with potent TG reducing potential are under development.
Vupanorsen (IONIS ANGPTL3-LRX/AKCEA-ANGPTL3-LRX/ISIS 703802)
Background information
Vupanorsen is a second generation AsO selective for ANGPTL3 mRNA and is conjugated to GalNAc to ensure selective hepatic uptake [18]. A advantage of the AsO strategy is that immune responses, which may be induced by monoclonal antibodies, are avoided [72].
Vupanorsen has been investigated as a weekly or monthly dose and TG lowering more than 60% has been reported [36, 82].
Clinical development: efficacy
The results of a double blind, placebo-controlled, randomized phase 1 study have been published [82]. Forty-four healthy participants were randomly assigned to receive a single dose of ANGPTL3-LRX (20, 40, or 80 mg), multiple doses (10, 20, 40, or 60 mg once weekly) or placebo over a six-week period. In patients receiving a single injection (n = 9 vupanorsen, n = 3 placebo), dose dependent decreases in ANGPTL3 protein, triglycerides, VLDL cholesterol, non-HDL cholesterol and total cholesterol were observed in the vupanorsen treatment group. In patients receiving multiple doses of vupanorsen (n = 24 active, n = 8 placebo), significant, dose dependent reductions in ANGPTL3 protein levels were observed at day 43 [82]. Patients receiving the highest dose of vupanorsen (60 mg) showed a reduction of almost 85% in ANGPTL3 protein levels as compared to baseline. A substantial 63.1% reduction in triglycerides from baseline was observed [82].
A phase 2 study investigated vupanorsen given subcutaneously at doses of 40 or 80 mg once monthly or 20 mg once weekly in 105 patients with elevated fasting plasma TG, a confirmed diagnosis of type 2 diabetes, hepatic steatosis and BMI between 27 and 40 kg/m2 [36]. After a 6-month treatment period, the greatest reduction in triglyceride levels (53% reduction from baseline) and ANGPTL3 levels (62% reduction from baseline) was reported in the group receiving 80 mg vupanorsen once monthly [36]. This study is summarised in Table 3.
Several small studies assessing vupanorsen’s efficacy and safety in patients with familial partial lipodystrophy (NCT03514420), familial chylomicronemia syndrome (NCT03360747) and patients diagnosed with type 2 diabetes, hypertriglyceridemia and nonalcoholic fatty liver disease (NCT03371355) have recently been completed and preliminary results indicate reduction in fasting triglycerides ranging from 33 to 60%.
Another dose-ranging study (TRANSLATE-TIMI 70; NCT04516291) as well as a phase 1 study in healthy, adult Japanese participants (NCT04459767) have been completed, however results are yet to be published. A study evaluating the safety and efficacy of vupanorsen in patients with familial hypercholesterolemia (NCT02709850) is ongoing.
Clinical development: safety
No serious adverse events were reported during the phase 1 study [82]. Adverse events recorded in the multiple-dose arm and included headache (three reports) and dizziness (three reports) [82]. Adverse events reported during the phase 2 study were mostly mild in nature and included injection site reactions (20.5% of all vupanorsen-treated patients), urine protein/creatinine ratio > 325 mg/g (11.5% of vupanorsen-treated patients) and urine albumin/creatinine ratio > 165 mg/g (9.0% of all vupanorsen-treated patients) [36].
Pfizer announced in January 2022 that they would be returning the rights for vupanorsen to IONIS following a careful review of the TRANSLATE-TIMI 70 results. Pfizer stated that ‘the study met its primary endpoint, achieving a statistically significant reduction in non-high density lipoprotein cholesterol (non-HDL-C) — as well as statistically significant reductions in triglycerides (TG) and angiopoietin-like 3 (ANGPTL3). However, the magnitude of non-HDL-C and TG reduction observed did not support continuation of the clinical development program for CV risk reduction or severe hypertriglyceridemia’. Vupanorsen was also associated with dose-dependent increases in liver fat, and higher doses were associated with elevations in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) [83].
ARO-ANG3
Background information
The siRNA therapy, ARO-ANG3, selectively inhibits hepatic translation of ANGPTL3 mRNA. ARO-ANG3 is conjugated to GalNAc ensuring selective binding to the hepatic ASGPR only [19].
Available data suggest potent reduction in systemic ANGPTL3 after monthly administration of ARO-ANG3 [37].
Clinical development: efficacy
Studies in non-human primates demonstrated that a single dose of 2 mg/kg resulted in a maximum reduction in systemic ANGPTL3 levels of 75%. This effect was sustained over a period of 7 weeks [84].
Preliminary results for a phase 1 study in healthy adult volunteers or patients with dyslipidemia, including familial hypercholesterolemia and severe hypertriglyceridemia, indicate potent and prolonged inhibition of ANGPTL3 levels (up to 93%) after two doses of ARO-ANG3 [37, 38]. Interestingly, the mean reduction in LDL-C, TG and ANGPTL3 observed in these studies were similar in healthy volunteers and patients with heterozygous familial hypercholesterolemia. Full results of this study have not yet been published.
Further details are shown in in Table 3.
Clinical development: safety
Headache, upper respiratory tract infections and injection site reactions were the most commonly reported adverse events during the phase 1 study for ARO-ANG3. No serious adverse events were reported in the preliminary results [27, 38].
Volanesorsen and olezarsen
Background information
Volanesorsen is a second generation AsO that selectively inhibits apoC3 synthesis [20]. A second- generation, GalNAc-conjugated version of volanesorsen, olezarsen, is also currently under development [85].
Studies reported reduction in TG levels of up to 53% in response to once weekly or once monthly administration of volanesorsen [36]. Reduction in TG levels up to 60% has been reported after monthly administration of olezarsen [42].
Clinical development: efficacy
A phase 1 double blind, placebo-controlled, dose escalation study (ISIS 304801-CS1) was conducted in 33 healthy volunteers [20]. Volunteers assigned to the multiple dose cohorts received six doses of volanesorsen at 50, 100, 200 or 400 mg over a five-week period. TG levels were reduced by up to 40% [20].
The efficacy of volanesorsen in patients with familial chylomicronemia syndrome (FCS) was investigated in the phase 3, randomized, double-blind, placebo-controlled APPROACH study [39]. A total of 66 patients were randomized to receive volanesorsen at 300 mg weekly or placebo over a 52-week period (please see Table 3). Triglyceride levels were lowered by 77% in the volanesorsen-treated group at month three, corresponding to a mean reduction of 19.3 mmol/L [39]. After 3 months of treatment, apoC3 levels were reduced by more than 80%. After completion of the APPROACH study, patients had the option of enrolling in the APPROACH open label extension (OLE) study (NCT2658175). Results for the OLE study are not yet available.
Results from the phase 3 randomized, double-blind, placebo-controlled COMPASS study indicated that volanesorsen at a dose of 300 mg once weekly reduced TG levels by a mean of 72.7 ± 17.4% from baseline to month 3 in 75 patients with predominantly non-FCS hypertriglyceridemia [40]. These effects were sustained to study end at 26 weeks.
The phase 2/3 BROADEN study (NCT02527343) evaluated the efficacy of volanesorsen in patients with partial lipodystrophy [41]. After a 52-week period, an 88% reduction in fasting triglycerides was reported for patients randomized to weekly administration of 300 mg volanesorsen with a 22% reduction in patients receiving placebo [41]. A two-year open-label extension study (NCT02639286) is planned.
Volanesorsen therapy was associated with increases in LDL-C of 135.6 and 95.5%, respectively in the APPROACH and COMPASS studies. However, increases in apoB, and thus particle numbers, were much smaller at 19.5 and 5.8%, respectively and the baseline LDL-C was low in both studies [39, 40]. Clinicians should re-evaluate lipids carefully following initiation of therapy with volanesorsen and consider whether a statin is required for LDL-C reduction or not.
A phase 2 dose-ranging study with olezarsen in patients with established ASCVD and elevated triglyceride levels was recently completed [42]. A reduction in mean triglyceride levels of up to 60% were reported for both weekly and monthly administration of olezarsen.
Clinical development: safety
Volanesorsen is mostly well-tolerated except for the occurrence of severe thrombocytopenia in some patients with FCS during the APPROACH study. The most commonly reported adverse event was mild injection site reaction (52% of volunteers in the Phase 1 study, 61% of patients in the APPROACH study and 23.5% of patients in the COMPASS study) [20, 39, 40]. In the APPROACH study severe thrombocytopenia (< 25,000 platelets per microliter) developed in two patients and subsequent cases of thrombocytopenia resulted in treatment discontinuation in nine patients [39]. Thrombocytopenia leading to treatment discontinuation was not reported in the COMPASS study [40].
Other adverse events reported during the clinical development program of volanesorsen included transient elevation of C-reactive protein [20], abdominal pain [39] and one potentially related case of serum sickness that occurred 2 weeks after the final dose [40].
Mild erythema at the injection site was the most frequently reported adverse event for patients treated with olezarsen [42].
ARO-APOC3
Background information
The siRNA ARO-APOC3 selectively silences apoC3 expression in the liver as it is conjugated to GalNAc which binds to the hepatic ASGPR [19].
Studies are currently investigating monthly administration of ARO-APOC3 and a marked reduction in apoC3 levels was reported [43].
Clinical development: efficacy
A phase 1 study to investigate the safety, tolerability, pharmacokinetics and pharmacodynamics of ARO-APOC3 is currently underway (see Table 3). Healthy volunteers as well as patients with severe hypertriglyceridemia and familial chylomicronemia syndrome were included in this dose-finding study. Preliminary results indicate that apoC3 levels were reduced between 60 and 90% for up to 10 weeks while TGs were reduced by 72% for up to 8 weeks after two doses of 50 mg of ARO-APOC3 in healthy volunteers [43]. Similar efficacy was observed in participants with hypertriglyceridemia: a mean reduction in TG of 78% was observed 4 weeks after treatment with ARO-APOC3 at a dose of 50 mg [86]. In patients with multifactorial chylomicronemia a mean reduction of 97% in TG levels were observed a month after ARO-APOC3 was administered [87]. Full results are yet to be published.
Clinical development: safety
No serious adverse events were reported during the phase 1 study. However, injection site reactions, headache, upper respiratory tract infection and transient alanine aminotransferase elevation in two patients with familial chylomicronemia were reported [43, 86, 87].
Discussion
During the last century the ability of clinicians to prevent cardiovascular disease or to reduce morbidity and mortality in patients with clinically manifest disease has improved significantly leading to hopes that coronary artery disease may be eradicated by the end of the twentieth century [88]. Unfortunately, these lofty ambitions have not been realized and cardiovascular disease remains the leading cause of mortality worldwide [1].
Limitations of current lipid-modifying therapies including tolerability concerns, poor adherence, lack of options for therapeutic targets such as Lp(a) and funder-associated access restrictions are challenges that must be addressed to reduce the burden of cardiovascular disease.
RNA-based therapies have the potential to address several of these unmet needs as they can be directed highly specifically at targets and pathways that were either previously not accessible to small molecule-based therapies or where such therapies were associated with significant off-target effects. The technologies employed in these novel therapies also reduce the patient’s burden of adherence through marked reduction in administration frequency. RNA-based therapies could potentially be prescribed using a population-based approach. Although the extended duration of action and infrequent dosing of many RNA-based therapies is attractive for clinicians and patients and may improve medication adherence, it may be more difficult to deal with medication-related adverse effects given the long time it will take for many of these drugs to be cleared.
Clinical studies directly comparing antisense oligonucleotide and small interfering RNA therapies are currently unavailable and the best treatment option for each target should be selected based on the available evidence considering safety, efficacy, tolerability, cost and ease of administration. Both approaches were originally associated with safety concerns: drug-induced thrombocytopenia was observed after treatment with several AsOs while peripheral neuropathy was reported after administration of the siRNA revusiran [89]. These concerns were addressed with structural modifications to improve the safety profile through enhance therapeutic specificity [89]. In terms of administration frequency, AsOs are generally administered monthly, while the extended duration of action of siRNA therapies allows for more prolonged periods between administration.
RNA-based therapies are unlikely to displace traditional small molecules. The accessibility, relatively low cost, widespread use and efficacy of small molecules means that RNA-based therapies will likely remain complementary to small molecule-based therapies except in diseases where there are no effective small molecule-based treatments. Furthermore, the cost of RNA-based therapies will likely limit widespread use. Patisiran, the first RNAi therapy approved by the FDA, is priced at an annual cost of US $451,430 – US $677,145 per patient [90]. Such costs may require manufacturers to reduce prices in addition to developing innovative funding strategies to ensure patient access and may restrict use to high and very high-risk patients only.
Future developments in the use of the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system may allow for even greater improvement of therapeutic strategies [91]. CRISPR therapies affect gene expression at the level of transcription, a process that precedes the target of both siRNA and AsO therapies. Thus far the technology is being explored for possible treatment of monogenic disorders, including cardiac arrhythmias caused by mutations in the CALM1, CALM2 or CALM3 genes. Further technological advances are required to ensure selective targeting and resolve challenges with administration [91].
Strengths and limitations of this review
This review illustrates the role various targets play in lipoprotein metabolism and how downregulation of these proteins can influence lipid metabolism and ultimately clinical outcomes. The review is limited in that it is by no means a comprehensive account of the development of RNA-based therapies in the cardiovascular landscape. In this report for instance therapies directed against hepatic TTR synthesis for the treatment of hereditary transthyretin-mediated amyloidosis (hATTR) such as the AsO inotersen [92], the Lp(a) lowering siRNA SLN360 [93] and RNA-based therapies for the treatment of heart failure of ischemic origin, CDR132L, were not discussed. Additionally, for many of the therapeutics discussed there is limited data in the public sphere as the results of many studies are not available or only available in abstract form. RNA-based therapeutics is also a very dynamic area of research and new candidate molecules are regularly announced.
Conclusion and future perspectives
The advent of RNA-based therapies holds great promise to significantly improve outcomes for patients living with cardiovascular conditions. Although a relatively new field of clinical research, these treatment strategies offer highly selective targeting of key genes implicated in cardiovascular diseases with limited adverse effects ushering in a new era in lipid-lowering therapies. RNA-based therapeutics offer hope for patients with genetic lipid disorders such as FCS, HoFH or very high Lp(a) for which there were previously often no or limited therapeutic options. Additionally, the infrequent dosing and high efficacy of many RNA-based therapeutics may benefit many patients with less severe lipid disorders, e.g., patients with polygenic hypercholesterolemia who nonetheless have high cardiovascular risk. Some children and adolescents with milder phenotypes of HeFH could conceivably be conveniently treated with an injection of inclisiran once every 6 months without the need for a daily pill. However, the use of these therapies may well be restricted by cost resulting in limited patient access and widespread adoption can only occur when long-term safety and benefit is confirmed in clinical outcome trials.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- AE:
-
Adverse event
- ALT:
-
Alanine aminotransferase
- ANGPTL3:
-
Angiopoeitin-like protein 3
- ApoB:
-
Apolipoprotein B
- ApoC3:
-
Apolipoprotein C3
- ASCVD:
-
Atherosclerotic cardiovascular disease
- ASGPR:
-
Asialoglycoprotein receptor
- AsO:
-
Antisense oligonucleotide
- BMI:
-
Body mass index
- CM:
-
Chylomicrons
- CMV:
-
Cytomegalovirus
- CRISPR:
-
Clustered Regularly Interspaced Short Palindromic Repeats
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- EMA:
-
European Medicines Agency
- FCS:
-
Familial chylomicronemia syndrome
- FDA:
-
Food and Drug Administration
- FH:
-
Familial hypercholesterolemia
- GalNAc:
-
N-Acetylgalactosamine
- hATTR:
-
Hereditary transthyretin-mediated amyloidosis
- HDL-C:
-
High density lipoprotein
- HeFH:
-
Heterozygous familial hypercholesterolemia
- HoFH:
-
Homozygous familial hypercholesterolemia
- IDL:
-
Intermediate-density lipoprotein
- LDL:
-
Low-density lipoprotein
- LDLR:
-
Low-density lipoprotein receptor
- LNA:
-
Locked nucleic acid
- Lp(a):
-
Lipoprotein(a)
- LPL:
-
Lipoprotein lipase
- mRNA:
-
Messenger ribonucleic acid
- OLE:
-
Open label extension
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- QW:
-
Once weekly
- Q2W:
-
Every two weeks
- Q4W:
-
Every four weeks
- RISC:
-
RNA-induced silencing complex
- RNA:
-
Ribonucleic acid
- RR:
-
Relative risk
- SC:
-
Subcutaneous
- siRNA:
-
Small interfering ribonucleic acid
- ssDNA:
-
Single-stranded deoxyribonucleic acid
- TG:
-
Triglycerides
- VLDL:
-
Very-low-density lipoprotein
- WHO:
-
World Health Organization
References
World Health Organisation. Cardiovascular Diseases: Key Facts. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed August 2020.
Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, et al. European Society of Cardiology: cardiovascular disease statistics 2019. Eur Heart J. 2020;41(1):12–85. https://doi.org/10.1093/eurheartj/ehz859.
Landmesser U, Poller W, Tsimikas S, Most P, Paneni F, Lüscher TF. From traditional pharmacological towards nucleic acid-based therapies for cardiovascular diseases. Eur Heart J. 2020;41(40):3884–99. https://doi.org/10.1093/eurheartj/ehaa229.
Crooke ST. Molecular mechanisms of antisense oligonucleotides. Nucleic Acid Ther. 2017;27(2):70–7. https://doi.org/10.1089/nat.2016.0656.
Uhlmann E, Peyman A. Antisense oligonucleotides: a new therapeutic principle. Chem Rev. 1990;90(4):543–84. https://doi.org/10.1021/cr00102a001.
Achenbach TV, Brunner B, Heermeier K. Oligonucleotide-based knockdown technologies: antisense versus RNA interference. Chembiochem. 2003;4(10):928–35. https://doi.org/10.1002/cbic.200300708.
Kole R, Krainer AR, Altman S. RNA therapeutics: beyond RNA interference and antisense oligonucleotides. Nat Rev Drug Discov. 2012;11(2):125–40. https://doi.org/10.1038/nrd3625.
Perry CM, Balfour JAB. Fomivirsen. Drugs. 1999;57(3):375–80. https://doi.org/10.2165/00003495-199957030-00010.
Sharad S, Kapur S. Antisense therapy: an overview. Antisense Therapy. Norderstedt, Germany, Books on Demand; 2019.
US Food and Drug Administration. FDA approves first-of-its kind targeted RNA-based therapy to treat a rare disease. https://www.fda.gov/news-events/press-announcements/fda-approves-first-its-kind-targeted-rna-based-therapy-treat-rare-disease. Accessed 27 August 2020.
US Food and Drug Administration. FDA approves givosiran for acute hepatic porphyria, US FDA https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-givosiran-acute-hepatic-porphyria. Accessed 27 Aug 2020.
US Food and Drug Administration. FDA approves add-on therapy to lower cholesterol among certain high-risk adults. https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-add-therapy-lower-cholesterol-among-certain-high-risk-adults. Accessed 12 Jan 2022.
Lavecchia A, Cerchia C. Recent advances in developing PCSK9 inhibitors for lipid-lowering therapy. Future Med Chem. 2019;11(5):423–41. https://doi.org/10.4155/fmc-2018-0294.
Fitzgerald K, White S, Borodovsky A, Bettencourt BR, Strahs A, Clausen V, et al. A highly durable RNAi therapeutic inhibitor of PCSK9. NEJM. 2017;376(1):41–51. https://doi.org/10.1056/NEJMoa1609243.
Ito MK. ISIS 301012 gene therapy for hypercholesterolemia: sense, antisense, or nonsense? Ann Pharmacother. 2007;41(10):1669–78. https://doi.org/10.1345/aph.1K065.
Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, Tardif JC, Baum SJ, Steinhagen-Thiessen E, et al. Lipoprotein (a) reduction in persons with cardiovascular disease. NEJM. 2020;382(3):244–55. https://doi.org/10.1056/NEJMoa1905239.
Koren MJ, Moriarty PM, Neutel J, Baum SJ, Hernandez-Illas M, Weintraub HS, et al. Safety, Tolerability and Efficacy of Single-dose Amg 890, a Novel Sirna Targeting Lp (a), in Healthy Subjects and Subjects With Elevated Lp (a). Circulation. 2020;142(Suppl_3):A13951.
Ruscica M, Zimetti F, Adorni MP, Sirtori CR, Lupo MG, Ferri N. Pharmacological aspects of ANGPTL3 and ANGPTL4 inhibitors: new therapeutic approaches for the treatment of atherogenic dyslipidemia. Pharmacol Res. 2020;153:104653. https://doi.org/10.1016/j.phrs.2020.104653.
Wong SC, Li Z, Given B, Seefeld M, Andersen A, Zhu R, et al. Personalized medicine for dyslipidemias by RNA interference-mediated reductions in apolipoprotein C3 or angiopoietin-like protein 3. J Clin Lipidol. 2019;13(3):e15. https://doi.org/10.1016/j.jacl.2019.04.033.
Graham MJ, Lee RG, Bell TA III, Fu W, Mullick AE, Alexander VJ, et al. Antisense oligonucleotide inhibition of apolipoprotein C-III reduces plasma triglycerides in rodents, nonhuman primates, and humans. Circ Res. 2013;112(11):1479–90. https://doi.org/10.1161/CIRCRESAHA.111.300367.
Linton MRF, Yancey PG, Davies SS, Jerome WG, Linton EF, Song WL, et al. The Role of Lipids and Lipoproteins in Atherosclerosis. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth, MDText.com, Inc.; 2000. 251–306.
Pedersen TR, Olsson AG, Færgeman O, Kjekshus J, Wedel H, Berg K, et al. Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian simvastatin survival study (4S). Circulation. 1998;97(15):1453–60. https://doi.org/10.1161/01.CIR.97.15.1453.
Carballo D, Mach F. Intensive LDL-cholesterol lowering and inhibition of inflammation to further reduce cardiovascular risk? J Cardiovasc Med. 2018;21(12):310–5. https://doi.org/10.4414/cvm.2018.02003.
Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–97. https://doi.org/10.1001/jama.2016.13985.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European atherosclerosis society (EAS). Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Taylor BA, Thompson PD. Statins and their effect on PCSK9 - impact and clinical relevance. Curr Atheroscler Rep. 2016;18(8):46. https://doi.org/10.1007/s11883-016-0604-3.
Biopharma C. CiVi 007. Civi Biopharma. https://www.civibio.com/pipeline/civi-007/. Accessed 17 Dec 2020.
Chiu MH, Tamura T, Wadhwa MS, Rice KG. In vivo targeting function of N-linked oligosaccharides with terminating galactose and N-acetylgalactosamine residues. J Biol Chem. 1994;269(23):16195–202. https://doi.org/10.1016/S0021-9258(17)33992-3.
Sato H, Kato Y, Hayashi E, Tabata T, Suzuki M, Takahara Y, et al. A novel hepatic-targeting system for therapeutic cytokines that delivers to the hepatic asialoglycoprotein receptor, but avoids receptor-mediated endocytosis. Pharm Res. 2002;19(11):1736–44. https://doi.org/10.1023/A:1020773800358.
Khvorova A. Oligonucleotide therapeutics - a new class of cholesterol-lowering drugs. NEJM. 2017;376(1):4–7. https://doi.org/10.1056/NEJMp1614154.
Stoekenbroek RM, Kallend D, Wijngaard PL, Kastelein JJ. Inclisiran for the treatment of cardiovascular disease: the ORION clinical development program. Futur Cardiol. 2018;14(6):433–42. https://doi.org/10.2217/fca-2018-0067.
Fitzgerald K, Frank-Kamenetsky M, Shulga-Morskaya S, Liebow A, Bettencourt BR, Sutherland JE, et al. Effect of an RNA interference drug on the synthesis of proprotein convertase subtilisin/kexin type 9 (PCSK9) and the concentration of serum LDL cholesterol in healthy volunteers: a randomized, single-blind, placebo-controlled, phase 1 trial. Lancet. 2014;383(9911):60–8. https://doi.org/10.1016/S0140-6736(13)61914-5.
Scicchitano P, Milo M, Mallamaci R, De Palo M, Caldarola P, Massari F, et al. Inclisiran in lipid management: a literature overview and future perspectives. Biomed Pharmacother. 2021;143:1–15. https://doi.org/10.1016/j.biopha.2021.112227.
Raal FJ, Santos RD, Blom DJ, Marais AD, Charng MJ, Cromwell WC, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, for lowering of LDL cholesterol concentrations in patients with homozygous familial hypercholesterolemia: a randomized, double-blind, placebo-controlled trial. Lancet. 2010;375(9719):998–1006. https://doi.org/10.1016/S0140-6736(10)60284-X.
McGowan MP, Tardif JC, Ceska R, Burgess LJ, Soran H, Gouni-Berthold I, et al. Randomized, placebo-controlled trial of mipomersen in patients with severe hypercholesterolemia receiving maximally tolerated lipid-lowering therapy. PLoS One. 2012;7(11):e49006. https://doi.org/10.1371/journal.pone.0049006.
Gaudet D, Karwatowska-Prokopczuk E, Baum SJ, Hurh E, Kingsbury J, Bartlett VJ, et al. Vupanorsen, an N-acetyl galactosamine-conjugated antisense drug to ANGPTL3 mRNA, lowers triglycerides and atherogenic lipoproteins in patients with diabetes, hepatic steatosis, and hypertriglyceridaemia. Eur Heart J. 2020;00(40):1–10. https://doi.org/10.1093/eurheartj/ehaa689.
Watts GF, Schwabe C, Scott R, Gladding P, Sullivan D, Baker J, et al. Pharmacodynamic Effect of ARO-ANG3, an Investigational RNA Interference Targeting Hepatic Angiopoietin-like Protein 3, in Patients With Hypercholesterolemia. Circulation. 2020;142(Suppl 3):A15751.
Watts GF, Schwabe C, Scott R, Gladding P, Sullivan D, Baker J, et al. RNAi inhibition of angiopoietin-like protein 3 (ANGPTL3) with ARO-ANG3 mimics the lipid and lipoprotein profile of familial combined hypolipidemia. Eur Heart J. 2020;41(Suppl 2):ehaa946–3331.
Witztum JL, Gaudet D, Freedman SD, Alexander VJ, Digenio A, Williams KR, et al. Volanesorsen and triglyceride levels in familial chylomicronemia syndrome. NEJM. 2019;381(6):531–42. https://doi.org/10.1056/NEJMoa1715944.
Gouni-Berthold I, Alexander VJ, Yang Q, Hurh E, Steinhagen-Thiessen E, Moriarty PM, et al. Witztum JL; COMPASS study group. Efficacy and safety of volanesorsen in patients with multifactorial chylomicronaemia (COMPASS): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2021;9(5):264–75. https://doi.org/10.1016/S2213-8587(21)00046-2.
O’Dea L, Tami J, Alexander V, Watts L, Hurh E, Hubbard B, et al. Efficacy and safety of volanesorsen for the treatment of metabolic complications in patients with familial partial lipodystrophy: results of the BROADEN study. In: 22nd European Congress of Endocrinology [Internet], 2020 September 5–9, online. United Kingdom; BioScientifica; 2020; vol 70. Available from: Endocrine Abstracts doi: https://doi.org/10.1530/endoabs.70.OC3.7.
Tardif J, Karwatowska-Prokopczuk E, Amour ES, Ballantyne CM, Shapiro MD, Moriarty PM, et al. Apolipoprotein C-III reduction in subjects with moderate hypertriglyceridaemia and at high cardiovascular risk. Eur Heart J. 2022;00(14):1–13. https://doi.org/10.1093/eurheartj/ehab820.
Schwabe C, Scott R, Sullivan D, Baker J, Clifton P, Hamilton J, et al. RNA interference targeting apolipoprotein C-III with ARO-APOC3 in healthy volunteers mimics lipid and lipoprotein findings seen in subjects with inherited apolipoprotein C-III deficiency. Eur H J. 2020;41(Suppl 2):ehaa946–3330.
Hovingh GK, Lepor NE, Kallend D, Stoekenbroek RM, Wijngaard PL, Raal FJ. Inclisiran durably lowers low-density lipoprotein cholesterol and Proprotein convertase Subtilisin/Kexin type 9 expression in homozygous familial hypercholesterolemia: the ORION-2 pilot study. Circulation. 2020;141(22):1829–31. https://doi.org/10.1161/CIRCULATIONAHA.119.044431.
Raal FJ, Kallend D, Ray KK, Turner T, Koenig W, Wright RS, et al. Inclisiran for the treatment of heterozygous familial hypercholesterolemia. NEJM. 2020;382(16):1520–30. https://doi.org/10.1056/NEJMoa1913805.
Ray KK, Wright RS, Kallend D, Koenig W, Leiter LA, Raal FJ, et al. Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. NEJM. 2020;382(16):1507–19. https://doi.org/10.1056/NEJMoa1912387.
Young SG. Recent progress in understanding apolipoprotein B. Circulation. 1990;82(5):1574–94. https://doi.org/10.1161/01.CIR.82.5.1574.
McLeod RS and Yao Z. Assembly and secretion of triglyceride-rich lipoproteins. In: Ridgway ND, McLeod RS, editors. Biochemistry of lipids, lipoproteins and membranes, sixth edition. Amsterdam: Elsevier; 2016. p. 459–488, DOI: https://doi.org/10.1016/B978-0-444-63438-2.00016-X.
Kastelein JJ, Wedel MK, Baker BF, Su J, Bradley JD, Yu RZ, et al. Potent reduction of apolipoprotein B and low-density lipoprotein cholesterol by short-term administration of an antisense inhibitor of apolipoprotein B. Circulation. 2006;114(16):1729–35. https://doi.org/10.1161/CIRCULATIONAHA.105.606442.
Stein EA, Dufour R, Gagne C, Gaudet D, East C, Donovan JM, et al. Apolipoprotein B synthesis inhibition with mipomersen in heterozygous familial hypercholesterolemia: results of a randomized, double-blind, placebo-controlled trial to assess efficacy and safety as add-on therapy in patients with coronary artery disease. Circulation. 2012;126(19):2283–92. https://doi.org/10.1161/CIRCULATIONAHA.112.104125.
Fogacci F, Ferri N, Toth PP, Ruscica M, Corsini A, Cicero AF. Efficacy and safety of mipomersen: a systematic review and meta-analysis of randomized clinical trials. Drugs. 2019;79(7):751–66. https://doi.org/10.1007/s40265-019-01114-z.
Genzyme Corporation. Kynamro Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/203568s000lbl.pdf. .
European Medicines Agency. Kynamro. https://www.ema.europa.eu/en/medicines/human/EPAR/kynamro Accessed 26 May 2021.
Eaton DL, Fless GM, Kohr WJ, McLean JW, Xu QT, Miller CG, et al. Partial amino acid sequence of apolipoprotein (a) shows that it is homologous to plasminogen. PNAS. 1987;84(10):3224–8. https://doi.org/10.1073/pnas.84.10.3224.
Kraft HG, Lingenhel A, Kochl S, Hoppichler F, Kronenberg F, Abe A, et al. Apolipoprotein (a) kringle IV repeat number predicts risk for coronary heart disease. Arterioscler Thromb Vasc Biol. 1996;16(6):713–9. https://doi.org/10.1161/01.ATV.16.6.713.
Nordestgaard BG, Langsted A. Lipoprotein (a) as a cause of cardiovascular disease: insights from epidemiology, genetics, and biology. J Lipid Res. 2016;57(11):1953–75. https://doi.org/10.1194/jlr.R071233.
Ruscica M, Sirtori CR, Corsini A, Watts GF, Sahebkar A. Lipoprotein (a): knowns, unknowns and uncertainties. Pharmacol Res. 2021;173:105812. https://doi.org/10.1016/j.phrs.2021.105812.
Wilson DP, Jacobson TA, Jones PH, Koschinsky ML, McNeal CJ, Nordestgaard BG, et al. Use of lipoprotein (a) in clinical practice: a biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol. 2019;13(3):374–92. https://doi.org/10.1016/j.jacl.2019.04.010.
Tsimikas S. A test in context: lipoprotein (a) diagnosis, prognosis, controversies, and emerging therapies. JACC. 2017;69(6):692–711. https://doi.org/10.1016/j.jacc.2016.11.042.
Guyton JR. Niacin in cardiovascular prevention: mechanisms, efficacy, and safety. Curr Opin Lipidol. 2007;18(4):415–20. https://doi.org/10.1097/MOL.0b013e3282364add.
Raal FJ, Honarpour N, Blom DJ, Hovingh GK, Xu F, Scott R, et al. Inhibition of PCSK9 with evolocumab in homozygous familial hypercholesterolaemia (TESLA part B): a randomized, double-blind, placebo-controlled trial. Lancet. 2015;385(9965):341–50. https://doi.org/10.1016/S0140-6736(14)61374-X.
Burgess S, Ference BA, Staley JR, Freitag DF, Mason AM, Nielsen SF, et al. Association of LPA variants with risk of coronary disease and the implications for lipoprotein(a)-lowering therapies: a Mendelian randomization analysis. JAMA Cardiol. 2018;3(7):619–27. https://doi.org/10.1001/jamacardio.2018.1470.
Koren MJ, Moriarty PM, Baum SJ, Neutel J, Hernandez-Illas M, Weintraub HS, et al. Preclinical development and phase 1 trial of a novel siRNA targeting lipoprotein(a). Nat Med. 2022;28(1):96–103. https://doi.org/10.1038/s41591-021-01634-w.
Melquist S, Wakefield D, Hamilton H, Chapman C, Grondolsky J, Schienebeck C, et al. Targeting apolipoprotein (a) with a novel RNAi delivery platform as a prophylactic treatment to reduce risk of cardiovascular events in individuals with elevated lipoprotein (a). Circulation. 2016;134(Suppl 1):A17167.
Nordestgaard BG, Tybjærg-Hansen A. Genetic determinants of LDL, lipoprotein (a), triglyceride-rich lipoproteins and HDL: concordance and discordance with cardiovascular disease risk. Curr Opin Lipidol. 2011;22(2):113–22. https://doi.org/10.1097/MOL.0b013e32834477d2.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. JACC. 2013;61(4):427–36. https://doi.org/10.1016/j.jacc.2012.08.1026.
Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45(11):1345–52. https://doi.org/10.1038/ng.2795.
Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626–35. https://doi.org/10.1016/S0140-6736(14)61177-6.
Rosenson RS, Davidson MH, Hirsh BJ, Kathiresan S, Gaudet D. Genetics and causality of triglyceride-rich lipoproteins in atherosclerotic cardiovascular disease. JACC. 2014;64(23):2525–40. https://doi.org/10.1016/j.jacc.2014.09.042.
Silbernagel G, Scharnagl H, Kleber ME, Delgado G, Stojakovic T, Laaksonen R, et al. LDL triglycerides, hepatic lipase activity, and coronary artery disease: an epidemiologic and Mendelian randomization study. Atherosclerosis. 2019;282:37–44. https://doi.org/10.1016/j.atherosclerosis.2018.12.024.
Thomsen M, Varbo A, Tybjærg-Hansen A, Nordestgaard BG. Low nonfasting triglycerides and reduced all-cause mortality: a mendelian randomization study. Clin Chem. 2014;60(5):737–46. https://doi.org/10.1373/clinchem.2013.219881.
Geladari E, Tsamadia P, Vallianou NG. ANGPTL3 inhibitors —their role in cardiovascular disease through regulation of lipid metabolism. Circulation. 2019;83(2):267–73. https://doi.org/10.1253/circj.CJ-18-0442.
Romeo S, Yin W, Kozlitina J, Pennacchio LA, Boerwinkle E, Hobbs HH, et al. Rare loss-of-function mutations in ANGPTL family members contribute to plasma triglyceride levels in humans. J Clin Investig. 2009;119(1):70–9.
Musunuru K, Pirruccello JP, Do R, Peloso GM, Guiducci C, Sougnez C, et al. Exome sequencing, ANGPTL3 mutations, and familial combined hypolipidemia. NEJM. 2010;363(23):2220–7. https://doi.org/10.1056/NEJMoa1002926.
Lichtenstein L, Mattijssen F, de Wit NJ, Georgiadi A, Hooiveld GJ, van der Meer R, et al. Angptl4 protects against severe proinflammatory effects of saturated fat by inhibiting fatty acid uptake into mesenteric lymph node macrophages. Cell Metab. 2010;12(6):580–92. https://doi.org/10.1016/j.cmet.2010.11.002.
Ginsberg HN, Le NA, Goldberg IJ, Gibson JC, Rubinstein A, Wang-Iverson P, et al. Apolipoprotein B metabolism in subjects with deficiency of apolipoproteins CIII and AI. Evidence that apolipoprotein CIII inhibits catabolism of triglyceride-rich lipoproteins by lipoprotein lipase in vivo. J Clin Investig. 1986;78(5):1287–95. https://doi.org/10.1172/JCI112713.
Sehayek E, Eisenberg S. Mechanisms of inhibition by apolipoprotein C of apolipoprotein E-dependent cellular metabolism of human triglyceride-rich lipoproteins through the low density lipoprotein receptor pathway. J Biol Chem. 1991;266(27):18259–67. https://doi.org/10.1016/S0021-9258(18)55263-7.
Pollin TI, Damcott CM, Shen H, Ott SH, Shelton J, Horenstein RB, et al. A null mutation in human APOC3 confers a favorable plasma lipid profile and apparent cardioprotection. Science. 2008;322(5908):1702–5. https://doi.org/10.1126/science.1161524.
Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjærg-Hansen A. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. NEJM. 2014;371(1):32–41. https://doi.org/10.1056/NEJMoa1308027.
TG and HDL Working Group of the Exome Sequencing Project, National Heart, Lung, and Blood Institute. Loss-of-function mutations in APOC3, triglycerides, and coronary disease. NEJM. 2014;371(1):22–31. https://doi.org/10.1056/NEJMoa1307095.
Virani SS, Morris PB, Agarwala A, Ballantyne CM, Birtcher KK, Kris-Etherton PM, et al. 2021 ACC expert consensus decision pathway on the management of ASCVD risk reduction in patients with persistent hypertriglyceridemia: a report of the American College of Cardiology Solution set Oversight Committee. JACC. 2021;78(9):960–93. https://doi.org/10.1016/j.jacc.2021.06.011.
Graham MJ, Lee RG, Brandt TA, Tai LJ, Fu W, Peralta R, et al. Cardiovascular and metabolic effects of ANGPTL3 antisense oligonucleotides. NEJM. 2017;377(3):222–32. https://doi.org/10.1056/NEJMoa1701329.
Pfizer. Pfizer and Ionis Announce Discontinuation of Vupanorsen Clinical Development Program. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-ionis-announce-discontinuation-vupanorsen. Accessed 25 Feb. 2022.
Wong SC, Zhu R, Havel PJ, Hamilton J, Graham J, Hegge J, et al. Reduction in Angiopoietin-Like Protein 3 via RNA Interference Improves Dyslipidemias and Hepatic Steatosis. Arteroscler Thromb Vasc Biol. 2019;39(Suppl 1):A492.
Adis Insight. Olezarsen – Ionis Pharmaceuticals. https://adisinsight.springer.com/drugs/800048476. Accessed 19 Jan. 2022.
Clifton P, Sullivan D, Baker J, Schwabe C, Thackwray S, Scott R, et al. Pharmacodynamic Effect of ARO-APOC3, an Investigational Hepatocyte-targeted RNA Interference Therapeutic Targeting Apolipoprotein C3, in Patients With Hypertriglyceridemia and Multifactorial Chylomicronemia. Circulation. 2020;142(Suppl 3):A12594.
Clifton P, Sullivan D, Baker J, Schwabe C, Thackwray S, Scott R, et al. First results of RNA interference against apolipoprotein C3 as a treatment for Chylomicronemia. J Clin Lipidol. 2020;14(4):594. https://doi.org/10.1016/j.jacl.2020.05.078.
Brown MS, Goldstein JL. Heart attacks: gone with the century? Science. 1996;272(5262):629. https://doi.org/10.1126/science.272.5262.629.
Chi X, Gatti P, Papoian T. Safety of antisense oligonucleotide and siRNA-based therapeutics. Drug Discov Today. 2017;22(5):823–33. https://doi.org/10.1016/j.drudis.2017.01.013.
CADTH Common Drug Review. Pharmacoeconomic Review report – Patisiran. 2019. https://www.ncbi.nlm.nih.gov/books/NBK549694/pdf/Bookshelf_NBK549694.pdf. Accessed 26 Oct. 2020.
Rezaei H, Farahani N, Hosseingholi EZ, Sathyapalan T, Hossein Sahebkar A. Harnessing CRISPR/Cas9 technology in cardiovascular disease. Trends in Cardiovasc Med. 2020;30(2):93–101. https://doi.org/10.1016/j.tcm.2019.03.005.
Gertz MA, Scheinberg M, Waddington-Cruz M, Heitner SB, Karam C, Drachman B, et al. Inotersen for the treatment of adults with polyneuropathy caused by hereditary transthyretin-mediated amyloidosis. Expert Rev Clin Pharmacol. 2019;12(8):701–11. https://doi.org/10.1080/17512433.2019.1635008.
Aleku M, Eisermann M, Löffler K, Dames S, Frauendorf C, Lindholm MW, et al. A Novel Short Interfering Ribonucleic Acid Shows Potent and Sustained Reduction of Serum Lipoprotein (a) in Cynomolgus Monkeys. Circulation. 2019;140(Suppl 1):A9538.
Acknowledgements
The authors would like to acknowledge the contribution of Ruan Jacobs to this review.
Funding
Publication fees were covered by Novartis Pharma AG, South Africa. Associates from Novartis South Africa were involved in the design and writing of the manuscript; however the authors retained autonomy as to the content of the manuscript including clinical position of each molecule.
Author information
Authors and Affiliations
Contributions
DJB, ADM, FJR and AvT contributed substantially to the conception of this review. DJB, FJR and AvT drafted the review. All authors contributed to the review of the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
DB reports grants for clinical trials and/or personal fees from Abbott, Akcea, Amgen, Amryt, AstraZeneca, Lib Therapeutics, Novartis, and Sanofi. ADM, RM and NvdM reports no competing interests. AvT is an employee of Novartis South Africa. FJR has received fees for conducting clinical research on inclisiran from The Medicines Company, and has personally received fees from Amgen, Sanofi, Regeneron, Novartis and The Medicines Company for attendance of advisory board meetings and lectures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Blom, D.J., Marais, A.D., Moodley, R. et al. RNA-based therapy in the management of lipid disorders: a review. Lipids Health Dis 21, 41 (2022). https://doi.org/10.1186/s12944-022-01649-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01649-3