Abstract
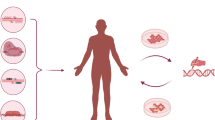
Cancer is a severe disease that substantially jeopardizes global health. Although considerable efforts have been made to discover effective anti-cancer therapeutics, the cancer incidence and mortality are still growing. The personalized anti-cancer therapies present themselves as a promising solution for the dilemma because they could precisely destroy or fix the cancer targets based on the comprehensive genomic analyses. In addition, genome editing is an ideal way to implement personalized anti-cancer therapy because it allows the direct modification of pro-tumor genes as well as the generation of personalized anti-tumor immune cells. Furthermore, non-viral delivery system could effectively transport genome editing tools (GETs) into the cell nucleus with an appreciable safety profile. In this manuscript, the important attributes and recent progress of GETs will be discussed. Besides, the laboratory and clinical investigations that seek for the possibility of combining non-viral delivery systems with GETs for the treatment of cancer will be assessed in the scope of personalized therapy.
Similar content being viewed by others
Background
Cancer is a very prevalent disease and is also the leading cause of death worldwide [1]. According to Global Cancer Statistics 2020, there were about 19.3 million new cancer cases in 2020. Moreover, an estimated 10.0 million cancer deaths occurred in the same year [2]. Besides, the incidence and mortality of cancer are growing year by year [3,4,5]. Therefore, to control the growing mortality and incidence of cancer more effectively, innovative and potent therapeutic methods need to be developed [6]. Up to date, a series of novel anti-cancer approaches have been proposed [7]. They are characterized by improved efficiency and safety, such as personalized therapy [8], immunotherapy [9], targeted therapy [10], combination therapy [11], and gene therapy [12]. Among them, personalized therapy is distinct because its development does not heavily rely on the major technological breakthrough in a specific field but requires the harmonious collaboration of multiple disciplines including diagnostics, genome sequencing, target screening, and treatment designing [13]. Since the carcinogenic factors (e.g., oncogenes, cancer stem cells) are different from patients to patients [14, 15], personalized therapies present themselves as a promising solution for tumor heterogeneity because they make it possible to precisely destroy or fix the neoplastic genes based on the comprehensive genomic analyses of different patients and tumors [16].
Genome editing is an ideal way to implement personalized anti-cancer therapy because it provides the possibility of directly modifying the pro-tumor genes [17]. In addition, genome editing can also be used to develop personalized immunotherapies by reprogramming the immune cells [18]. In comparison to early gene engineering methods that randomly insert genes into the host genome [19], genome editing is carried out by precisely inserting, deleting, modifying or replacing DNA or RNA sequences at specific sites in the genome [20, 21]. Generally, the procedure of most genome editing mechanisms consists of three steps: recognition, cleavage, and repair [22]. The genome editing tools (GETs) could precisely recognize the target site where the double strand break (DSB) would then be generated [23]. Subsequently, the DSB would be repaired by homology-directed repair (HDR) or nonhomologous end-joining (NHEJ) [24]. In particular, HDR mediates the insertion or replacement of genes [25], while NHEJ induces the disruption of genes [26]. The four major genome editing platforms include mega-nucleases, zinc-finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs), and clustered regularly interspaced short palindromic repeats (CRISPR)/Cas9 [27, 28]. While all of them have been considered as potential weapons in the battle against cancer, the accurate [29], convenient and effective CRISPR-Cas9 system is the most advanced one [30]. Additionally, the prerequisite for successful genome editing is the efficient delivery of GETs into the cell nucleus [31].
The delivery systems for genome editing therapies are commonly classified into viral delivery systems and non-viral delivery systems [32]. Although viral vectors are widely used for the delivery of gene therapies [33,34,35], they are associated with flaws like carcinogenesis [36], genotoxicity, immunogenicity [37], and insertional mutagenesis [38]. Compared to viral delivery systems, non-viral delivery systems have fewer safety concerns [39]. Furthermore, non-viral approaches can carry larger GETs and provide more stable control over the duration time the GETs stay in cells [40]. Therefore, it is conceivable that combining GETs with non-viral delivery systems may be a prospective strategy for the personalized and targeted cancer medicine. In this review, the important attributes and recent progress of GETs will be evaluated in terms of mechanisms and genome editing efficiency. In addition, the studies that combined non-viral delivery systems with GETs for the treatment of cancer will be assessed. Further, the clinical trials designed to appraise the efficacy and safety of anti-cancer therapies which combine GETs with non-viral delivery systems will be discussed according to published information.
Genome editing in the development of personalized anti-cancer therapies
The 21st centuray has witnessed spectacular upgrades of anti-cancer approaches, being genome editing-based personalized therapy deemed as one of the most promising strategies. Mega-nuclease, ZFN, TALEN, and CRISPR-Cas9 are the currently major genome editing platforms. While mega-nucleases are considered as the earliest GETs, ZFNs and TALENs manifest higher feasibility and editing efficiency. However, boosted by the unparalleled simplicity and convenience, CRISPR-Cas9 system has become the most prevelantly used GET at present. Moreover, since genome editing can be leveraged for the disruption or correction of oncogenes [41, 42], reprogramming of anti-cancer immune cells [43], and establishment of cancer models [44], it emerge as a powerful and versatile tool in the development of anti-cancer therapies.
Mega-nucleases
Mega-nuclease is a family of endodeoxyribonucleases that are characterized by a large (12-40 bps) recognition site [45]. Based on sequential and structural characteristics, the family could be divided into five sub-groups: LAGLIDADG, GIY-YIG, HNH, His-Cys box and PD-(D/E)XK [46]. Among them, the nucleases in the LAGLIDADG family were the most used and well-studied GETs [47]. Notably, mega-nucleases were also the first biological molecules being used for precise modification of genes, which, in another word, led to the arrival of genome editing era [48]. LAGLIDADG proteins have two important properties: first, they could engage in the splicing of their own introns as RNA maturases; second, they could recognize and cut the exon-exon junction sequence wherein their introns could be inserted [49]. In addition, two of the most popular LAGLIDADG proteins are I-SceI (Fig. 1a) and I-CreI [50]. Their abilities to recognize and cleave the target genes allow them to exert therapeutic functions such as gene correction and insertion of therapeutic genes.
Schematic diagram of the four GETs and the basic mechanisms of genome editing. a I-SceI: one of the most popular mega-nucleases. b The DNA binding domain of ZFNs and TALENs are both modular, the Fokl nuclease can create DSB. c CRSPR/Cas9 system comprises a Cas9 endonuclease and a sgRNA that target the sequence next to PAM site. d Following the creation of DSB, it would be repaired by HDR or NHEJ
However, the further applications of mega-nucleases in personalized anti-cancer therapies are being hampered by several drawbacks. Firstly, given the fact that all types of cancers are caused by certain oncological mutations, such genetic variations differ from patients to patients [51,52,53]. But natural mega-nucleases could only create DSBs in the specific recognition sites that do not exist in oncological genes [45], which means it is difficult to apply such natural mega-nucleases for the correction of cancer-associated mutations. Nevertheless, this problem could be overcome by the engineered mega-nucleases, as they can target sequences other than natural recognition sites with considerable efficiency. For example, it has been reported that, by using I-CreI of LAGLIDADG family as scaffold, the engineered mega-nuclease could target human RAG1 gene and induce the homologous recombination in 6% of transfected human cells [54]. Hence, the development of mega-nuclease engineering techniques would provide more feasibilities in terms of personalized anti-cancer therapies. Secondly, the gene targeting efficiency is relatively low. Reportedly, the highest targeting efficiency of mega-nuclease is 66% in human 293H cell line [55], however, a majority of studies just obtained 1%-20% efficiency in human cells [56,57,58,59]. Besides, the off-target issues are also hampering the further translation of mega-nuclease-based applications [60, 61], especially for the personalized anti-cancer therapies like correction of personal somatic mutations that cause cancers [62].
Zinc-finger nucleases
ZFN was first discovered in 1985 from Xenopus oocytes [63]. The consecutive structural analysis revealed that it comprised a site-specific DNA binding domain and a cleavage domain, and both of two are loaded on a zinc-finger (Fig. 1b). The abilities of ZFNs to recognize specific DNA sequence and create DSB make it an ideal platform for genome engineering [64]. Theoretically, the zinc finger protein can be designed to target any sites of genome [65]. In addition, such genomic modifications could be achieved through NHEJ and HDR [66]. While the NHEJ is mainly used to perform gene knockout, HDRs induced by ZFNs could be leveraged for gene correction or gene addition if proper templates were provided [64]. For example, to conduct gene knockout through NHEJ, Liu et. al. have successfully targeted and cleaved three independent genes using ZFNs. However, the frequencies of the obtained knockouts were above 1% [67]. Also, it was reported that, by inducing HDR using ZFNs and donor DNA, the “pro-stemness” gene was added to the genome of human embryonic stem cells with a frequency of 5% [68]. Hence, the abilities to elicit gene knockout, gene correction, and gene addition make ZFNs potential tool for personalized anti-cancer therapies.
ZFNs could be applied in the treatment of neoplastic diseases in three different ways. First, by specifically introducing DSBs, ZFNs could knockout oncogenes. However, Shankar et. al. have demonstrated that the ZFN-mediated editing efficiencies in some cancer cells lines were low (negligible – 6%). Besides, a substantial level of off-target events were detected by in silico analysis of DNA binding prediction [69]. These results indicate that more efforts need to be devoted to improving the targeting specificity and editing efficiency of the ZFNs used in this study. Although positive results have yet to be obtained from studies using ZFNs to knockout pro-tumor genes, this strategy remain to be promising for personalized anti-cancer therapy because the genetic backgrounds and the mutations that lead to cancers are different from patients to patients. Second, ZFNs could also be used to inhibit etiological factors of cancer like human papillomavirus (HPVs). Reportedly, the antitumor effect of the combination therapy comprising HPV E7-targeting ZFNs and chemotherapy has been evaluated. According to the report, the ability of the combination therapy to inhibit the cancer cell viability was much higher than that of chemotherapy alone. Moreover, the combination therapy also significantly suppressed the tumor growth in xenograft models [70]. Third, in anti-cancer immunotherapies, ZFNs could be used to edit the genome of immune cells to enhance their tumor-inhibitory capacities [71]. For instance, it has been shown that, knocking out the gene encoding programmed cell death-1 (PD-1) in tumor infiltrating lymphocytes (TIL) through ZFN-mediated genome editing before adoptive cell transfer leads to a 76% reduction in PD-1 surface-expression. Collectively, ZFN technology is another tool for genome editing-based anti-cancer therapies. It also holds considerable promise for the development of personalized anti-cancer therapies because it could be modified to target variable sites on the genome with favorable feasibility.
Transcription activator-like effector nucleases
Transcription activator-like effector nuclease (TALEN) system is established by fusing transcription activator-like effector (TALE) with DNA cleavage domain [72]. Like ZFNs, TALENs also need to be engineered to target different DNA sites. The TALE comprises three domains: a carboxyl-terminal domain, an amino-terminal domain, and a DNA-binding domain which contains a region that it is capable of conferring specificity to adenine (A), cytosine (C), guanine (G), and thymine (T) [73]. Moreover, although the DNA binding domain of ZFNs and TALENs are both modular (Fig. 1b). Each module of a TALE recognizes one nucleotide, while the recognition mediated by each zinc-finger module needs 3 nucleotides [74]. Hence, by reorganizing the TALE modules, researchers could engineer TALENs with more convenience. Besides, thanks to the previous studies on mega-nucleases and ZFNs, substantial understandings with respect to the optimization and application of such GETs have significantly facilitate the development of and technical maturation of TALEN system [72]. So far, the TALEN-mediated genome modification has been successfully performed in a variety of animals and cells [75,76,77,78,79,80].
Equipped with the superior properties such as higher efficacy, cheaper price, and improved feasibility, TALEN emerges as a better GET for personalized cancer therapeutics than ZFN [81]. However, the anti-tumor strategies of TALEN- and ZFN-based therapies are similar. For example, it was reported that the expression of IL-6 in hepatocellular carcinoma could be disrupted by TALENs. Furthermore, by analyzing the genome edited cancer cells, it was demonstrated that IL-6 promotes apoptosis and facilitate the expression level of IL-33 and VEGF-A. Finally, it was also shown that combining the genome editing with sorafenib and/or IFNα therapy significantly increased the anti-tumor effects [82]. This study suggests that TALEN could be used as personalized monotherapy or combined with other targeted therapies for the treatment of cancer. The TALEN-mediated gene disruption can also help to decipher the carcinogenic trajectories in different individuals. Moreover, TALENs were also implemented to target HPV E7. It was observed that the editing efficiency of E7 gene in cervical cancer cells was around 10-12%. In addition, the cell death induced by TALEN editing was shown to be tightly associated with cell necrosis [83]. Interestingly, in the previously mentioned study that used ZFNs to target HPV E7, the cell deaths were induced by apoptosis [70]. This discrepancy indicates that the consequences of TALEN- and ZFN-mediated knockout in cervical cancer cells might be differential, and it would be interesting to explore the mechanisms that cause this discrepancy. Furthermore, TALENs can also be used to modulate the phenotype of immune cells. Menger et. al. have performed TALEN-mediated knocking out of gene encoding PD-1 in tumor-reactive lymphocytes (TRLs) to confer resistant to PD-1 signaling on TRLs. This approach effectively enhanced the persistence of melanoma-reactive CD8 positive T cells and fibrosarcoma-reactive T cells at tumor sites [84]. In summary, the current applications of TALENs and ZFNs in cancer therapies are sharing similar mechanisms. Nevertheless, the improved module-recognizing specify, and the convenience of TALEN-mediated targeting makes them better option for developing personalized anti-tumor strategies.
CRISPR-Cas9 system
The first discovery of CRISPR dates back to 1987. Ishino and his colleague identified a sequence that contains five homologous sequences of 29 nucleotides, and these homologous sequences are separated by spacers [85]. Unfortunately, this study did not illustrate the biological significance of CRISPR. Later on, similar regularly spaced repeated sequences have been identified in a series of studies [86]. As a consequence, increasing attentions were focused on CRISPR, and its values in genome editing have been unveiled [87]. The natural CRISPR-Cas system acts as an adaptive immune system in prokaryotes. It could protect prokaryotes from phage infection by storing memory in host chromosomes. It consists of viral DNA and repetitive nucleotide sequences surrounding the viral DNA. These repetitive nucleotide sequences are termed direct repeats, they are surrounded at the near end by sequences encoding proteins called Cas proteins. In addition, the guide RNA of this system can be artificially manipulated for the targeting of different genes. Comparing to TALEN, CRISPR-Cas9 system is way more cost effective, it is 3-6 fold cheaper per reaction [88]. Furthermore, the generation and modification of gRNAs are also more convenient [89]. Therefore, CRISPR-Cas9 system is now deemed as the prior option for performing genome editing in laboratory studies. However, impaired by the affinity of the single guide RNA recognition, off-targeting effect is a major drawback that hinders the clinical translation [90].
The genome editing of CRISPR-Cas9 system is mediated by its two components: a Cas9 endonuclease and a single-stranded guide RNA (sgRNA) [91]. The sgRNA can recognize and bind to target sites, and the Cas9 endonuclease can then cleave the DNA (Fig. 1c). Moreover, it has been well documented that the cutting site of Cas9 endonuclease is 3 base pairs upstream of an “NGG” protospacer adjacent motif (PAM). Following the cleavage, the DSB would be repaired by NHEJ or HDR (Fig. 1d) [92].
Moreover, some recent progress made in CRISPR-Cas9-based techniques have paved the way for the development of personalized therapies. In 2016, David. Liu et. al. developed an adenine base editor system which can induce the conversion from adenine (A) to guanine (G) on DNA through rearranging the atoms, thereby easily installing point mutations in cells. In another word, this first version of base editor system can change A•T base pair into G•C base pair [93]. In 2017, the same group developed the upgraded version of base editor that can convert C:G base pair into T:A base pair with higher efficiency and product purity [94]. In the same year, Zhang et. al. structured an RNA editing system that can induce the A to inosine (I) replacement, this system can be used to edit full-length transcripts containing pathogenic mutations. It was shown that the RNA editing system is capable of robustly knockout genes and performing RNA editing in mammalian cells [95]. In 2019, they further upgraded this RNA editing system. The new system is named RESCUE, this new generation of RNA editing system kept the capacity of converting A to I, and it could also perform C-to-U and A-to-I editing [96]. In 2021, CRISPR C-to-G base editors for inducing targeted DNA transversions in human cells have been reported. The engineered base editors can efficiently induce targeted C-to-G base transversions in human cells [97]. All the new techniques mentioned above can be considered as promising tools for future personalized therapies against cancer because they can precisely modify single nucleotides, which maximize the possibilities for therapeutic genome editing. Recently, Lei et. al. reported that knocking out ATP‐binding cassette (ABC) B1 in colorectal cancer cells results in the restoration of the sensitivity to paclitaxel, suggesting that this approach is an promising way to deal with multidrug resistance [98].
On the top of that, CRISPR-Cas system has also been repurposed to perform epigenetic engineering [99]. For instance, accumulating studies have shown that manipulating the DNA-regulatory elements using CRISPR-Cas system is an efficient method to trigger epigenetic changes [100]. In particular, the CRISPR-dCas9 system contains a CRISPR guide and a variant of Cas9 protein whose endonuclease activity is lost. The CRIPSR-dCas9 serves as an ideal gene targeting platfrom for epigenetic modulators [101]. Moreover, cancer is associated with epigenetic changes such as aberrant histone modifications and DNA methylations [102]. In a previous study, dCas9 was linked with a epigenetic modulator which induces demethylation. This system induced demethylation A549 lung cancer cells with considerable efficiency [103]. In another study, the sgRNA-dCas9 targetng the protumor Granulin gene was conjugated with three different epigenetic suppressors: DNMT3a, KRAB, and EZH2. It was observed that, after treating the liver cancer cell Hep3B with the dCas9-epigenetic suppressor systems, the methylation level of the promoter for the target gene was elevated. Furthermore, the proliferation, invasion, tumor sphere formation the Hep3B were substantially inhibited by the suppressors [104].
In conclusion, genome editing is a straight-forward way to treat the diseases associated with genetic aberrations such as cancer. Mega-nuclease, ZFN, TALEN, and CRISPR-Cas9 are four major types of GETs. Although each of them has its pros and cons, efforts need to be devoted to improving the editing efficiency and minimalizing the off-targeting effect. Besides, except reconstructing and upgrading GETs themselves, designing and choosing appropriate delivery system is also a way to optimize the genome editing [105,106,107].
Non-viral delivery platforms for genome editing in the treatment of cancer
GETs are made of proteins and nucleic acid, which makes it challenging to efficiently and safely deliver them into the cell nucleus [108]. Although viral vectors were widely used in laboratories and clinical trials to deliver genome editing therapies, the potential immunogenic issues surrounding viral vectors significantly hindered the translation of such therapies [109]. Nevertheless, non-viral delivery systems present themselves as a prospective choice. Although delivery efficiency is slightly lower than that of viral delivery systems [110], non-viral delivery systems could be artificially synthesized and are associated with fewer safety issues [111]. More importantly, the quick development in materials science and molecular biology may substantially facilitate the improvement of deliver efficiency of non-viral systems. In addition, the accumulation of the understanding about how cells uptake and process the non-viral vectors would also help researchers to develop more efficient delivery systems. So far, a variety of molecular modulators, including microtubules, Niemann-Pick type C protein 1, and Heat shock protein 70, have been reported to contribute to the delivery of non-viral vectors [112].
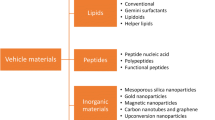
Generally, there are five major groups of non-viral delivery systems: peptide-based delivery system, lipid-based delivery system, inorganic delivery system, and polymeric delivery system, and electroporation. They have been used to deliver GETs for the direct editing of pathogenic cells in cancer therapies or ex vivo editing of immune cells. This section is focused on the current developments of these non-viral delivery systems in GET-based anti-cancer therapies. In addition, the advantages and limitations of this delivery system are also discussed.
Cell-penetrating peptide for the delivery of GETs into cancer cells
It has been well documented that cell-penetrating peptides (CPPs) can facilitate the cellular intake and uptake of molecules. Conjugating CPPs with therapeutic reagents could result in more efficient delivery [113]. Thus, they have been used as a delivery system for gene editing tools. It was demonstrated that CPPs could safely and effectively deliver ZFNs into cells. In addition, the cell-penetrating capacity of ZFN-CPP conjugates was observed to be much higher than that of ZFN alone [114]. It was also reported that the cell-penetrating poly-Arg peptide conjugating to a surface-exposed Cys residue present on each TAL effector repeat have superior cell-penetrating activity than that of purified TALEN proteins. This TALEN-CPP system was used to successfully knock out CCR5 and BMPR1A genes [115]. Further, Jain et. al. complexed CRISPR-Cas9 with an engineered, modular tandem peptide nanocomplex system. They showed that this CPP delivery system significantly contributes to the cell-targeting capacity and genome editing efficiency in OVCAR8 cells, HeLa cells, and 3TZ cells [116].
Inspired by the advantages of CPPs, they are also considered as a potential delivery system for personalized anti-cancer therapies. For example, an amphiphilic penetrating peptide has been synthesized by inducing the formation of hydrazone bond between a cationic peptide scaffold and a hydrophobic aldehyde tail. It was used to deliver Cas9 protein into human lung cancer A549 cells to delete the gene encoding hypoxanthine phosphoribosyltransferase 1 (Fig. 2b). The resultant high knockout efficiency indicates that CPPs can facilitate genome modification in cancer cells [117]. In another study, the CPP PTD4 was fused with an endosomolytic peptide CM18 and a 6x histidine-rich domain. The upgraded CPP-based non-viral delivery system was found to facilitate genome editing in different hard-to-modify cells including cancer cells including THP-1, Jurkat, and CA46 cells [118]. Additionally, CPP has been constructed into a self-assembling Cas9 ribonucleoprotein complex to act as a delivery system for genome-editing therapy against lung cancer. The self-assembling complex, named Cas9-LMWP comprises a nuclear localization sequence and a low-molecular-weight protamine (LMWP). This complex induced a 43.9 indels rates in KRAS gene of A549 lung cancer cells. Moreover, in xenograft lung cancer models established in female BALB/c nude mice, Cas9-LMWP exerted strong anti-cancer effects [119].
Schematic illustration of electroporation- and CPP-mediated delivery of GETs. a The activated human T cells reprogrammed by electroporation-mediated genome editing reduce the tumor burden of melanoma-bearing mice. b CPPs facilitate the genome editing in cancer cells which could be used to establish xenograft models
However, although CPPs present themselves as potential delivery systems for GETs, the intricate mechanism through which CPP enter cells is still unclear [120] and the clinical application of CPP is still hindered by the limited stability, selectivity and delivery efficiency [121]. Therefore, actions could be taken to explore solutions for such drawbacks.
Lipid-based delivery system for the delivery of GETs into cancer cells
Lipid nanoparticles are a clinically approved drug delivery system [122]. These spherical vesicles enclosed by a lipid bilayer membrane are biodegradable and biocompatible [123, 124]. However, the application of lipid-based systems for the delivery of GETs is hampered by shortcomings including limited half-life, stability, and encapsulation efficiency [125, 126]. The cationic lipids have been utilized to deliver Cas9-sgRNA nuclease complexes into cultured human cells and resulted in an 80% genome modification. Further, the cationic lipids also efficiently deliver different genome-editing proteins into the human cells and the mouse inner ear. The delivery of Cas9:sgRNA complexes led to a 80% genome modification in vitro and 20% in vivo [127]. As a carrier for therapeutic GET, cationic lipids were complexed with Cas9-sgRNA to treat autosomal dominant hearing loss in mice. The Cas9-sgRNA complex was engineered to target and disrupt the mutant Tmc1Bth allele. This strategy significantly reduced the progressive hearing loss, and substantially enhanced acoustic startle responses were observed in mice in treatment group. These findings suggest that the combination of lipid-based delivery system and GET may exert important roles in the treatment of the diseases caused by pathological gene mutations.
In personalized anti-cancer therapies, several strategies have been applied to improve the delivery efficiency of lipid-based carriers [128]. It has been reported that, equipped with amino-ionizable lipid nanoparticles, Cas9 mRNA and sgRNAs targeting PLK1 could be effectively delivered into aggressive orthotopic glioblastoma, and inhibit the tumor growth (Fig. 3a). By analyzing the tumors, it was found that up to 70% of gene editing had been achieved in Eight-week-old female C57BL/6JOlaHsd mice [122]. To be noticed, except developing personalized therapies according to the mutations identified in tumors and the genetic background of patients, establishing accurate cancer models that could recapitulate the characteristics the tumor in different patients is also an important step for designing personalized regimens and therapies. Daniel J. Siegwart and his colleague used their modified lipid nanoparticles as carriers for delivering Cas9-sgRNA ribonucleoprotein complexes into mouse tissues (Fig. 3b). Through this way, the Cas9-sgRNA ribonucleoprotein complexes could induce the cancer related mutations through editing the genome of cells. Consequently, organ-specific cancer models in livers and lungs were successfully generated [129]. Potentially, this approach can also be used to establish cancer models that recapitulate the patient-specific characteristics in mice, which is very helpful for the quick screening of drugs.
Schematic examples showing different applications of lipid-based delivery system for GETs. a CRISPR-Cas9 genome editing complexed with targeted lipid nanoparticles inhibit the growth of glioblastoma ovarian tumors. b Combing CRISPR-Cas9 with lipid nanoparticles for the tissue-specific gene editing or the generation of tumor models
Inorganic vectors for the delivery of GETs into cancer cells
Armed with advantages including stability, biocompatibility and large loading capacity, inorganic vectors emerge as a novel drug delivery platform [130]. The recently popular inorganic delivery systems can be classified into four types: black phosphorus, graphene oxide, mesoporous silica nanoparticles, and gold nanoparticles [131,132,133,134]. More importantly, they are also employed to deliver GETs into cells (Fig. 4). For instance, gold nanoparticles possess a special ability to penetrate cell membranes. In addition, gold is generally well tolerated by the human body and can be easily conjugated with DNA. It was reported that Cas9-sgRNA was co-assembled with the cationic arginine gold nanoparticles gold nano-carriers and then delivered into Hela cells, human embryonic kidney cells (HEK-293T), and mouse macrophage (Raw 264.7) cells. As a result, around 90% Cas9-sgRNA complexes were delivered into the cells and led to successful genome editing with up to 30% efficiency [135]. In addition, the metal-organic frameworks represent another important delivery system based on inorganic vectors because they have sufficient surface area with adjustable shapes. Moreover, their porosities and biodegradability also make them ideal delivery systems for GETs. Khashab et. al. have developed a nanoscale zeolitic imidazole framework to deliver CRISPR-Cas9 into Chinese hamster ovary cells. It was demonstrated that the loading efficiency was 17% and after 4 days, the the yielded gene editing efficiency of this system was 37% [136]. Furthermore, black phosphorus nanosheets (BPs) is a new version of two-dimensional biomaterial for drug delivery. They have good element biocompatibility and are non-toxic [137]. Also, the proteins could tightly bind to the periodic atomic grooves on surfaces of BPs [138]. These properties make BPs suitable for delivering GETs. In a previous study, the engineered Cas9 ribonucleoproteins were loaded on BPs, and it was shown that BP system could deliver the Cas9 ribonucleoproteins into MCF-7 cells and resulted in 26.7-32.1% indel frenquency in vitro. In addtion, the administration of BP + engineered Cas9 ribonucleoproteins also led to the significant reduction of EGFP signals in A549/EGFP tumor-bearing nude mice [139].
Thus, the inorganic vectors are also implemented into genome editing therapies for personalized anti-cancer therapies. The metal-organic framework has been modified to facilitate the gene editing in cancer cells. To improve the cell-entering capacity of zeolitic imidazolate frameworks, a research group coated them with the membrane of cancer cells. This approach significantly increased the uptake of the zeolitic imidazolate frameworks encapsulating CRISPR-Cas9 by MCF-7 cells. In animal studies, it was further confirmed that the zeolitic imidazolate frameworks coated by the membrane of MCF7 tumor cells selectively accumulate in MCF7 cells [140]. Besides, up-conversion nanoparticles represent a novel inorganic delivery system which could convert near-infrared (NIR) light into local ultraviolet light, thus making it possible for the cleavage of photosensitive molecules in a controlled manner [141]. This strategy has been used to achieve the on-demand release of genome editing therapy against cancer. Song et. al. reported that they had complexed the up-conversion nanoparticles with CRISPR-Cas9 system targeting tumor gene polo-like kinase-1, and successfully turned on the gene editing using NIR light in 293T cells. As for the in vivo investigation, A549 cells were edited using the up-conversion nanoparticles and CRISPR-Cas9 system. Then, the cells were subcutaneously transplanted into the back of BALB/c mice, which resulted in 4.7 to 20.1% indel frequency after different duration of irradiation time [142]. This approach could potentially provide substantial feasibility and convenience to the genome editing in personalized anti-cancer therapies.
Polymeric delivery system for the delivery of GETs into cancer cells
Polymeric drug delivery system is defined as a polymeric formulation that transports the therapeutic substance into the cell or body. Accumulating evidence suggests that polymeric delivery systems are safe, efficient, and could stably control the rate, time, and place of drug release [143,144,145,146,147]. So far, a few types of polymeric systems have been used to deliver GETs (Fig. 4). They are boronic dendrimer [148], nano-clew [149], Cas9 micelles [150], Polyethylenimine complex [151], and polymeric nanocapsules [152]. All of them have been shown to improve the safety or efficiency of GETs. Since polymers have been widely used for drug delivery, their values are well characterized. Therefore, it is conceivable that these polymeric carriers would be quickly translated to clinically appliable delivery systems for therapeutics [153].
With respect to personalized anti-cancer therapy, several types of polymeric delivery systems were employed to improve the editing efficiency and safety of GETs due to their large packaging capacity and safety profile [154]. For example, Ping et. al. have constructed a supramolecular polymer system which allows the controlled delivery of Cas9 ribonucleoprotein targeting mutant KRAS in 293T cells and colorectal cancer cells [155]. By effectively disrupting mutant genes, tumor growth as well as metastasis in the BALB/c nude mice bearing SW-480 CRC cells were significantly inhibited. In addition, a chain-shattering polymeric nanoplatform has been recently developed to deliver the CRISPR-Cas9-based anti-cancer therapy. The chain-shattering polymeric nanoplatform is a trigger-responsive delivery system in which protecting groups regulate the unpack/release of the CRISPR-Cas9 targeting tumor gene EZH2. Armed with this delivery system, the genome editing efficiency of CRISPR-Cas9 in PC3 prostate cancer cell line reached 32.2%. In xenograft tumor model established in BALB/c nude mice (4–5 weeks old, 18–20 g), it resulted in a 21.3% editing efficiency and significantly inhibited tumor growth [156]. This new delivery method is very meaningful for personalized anti-cancer therapy because it provides considerable precision for the modulation of cancer related genes.
Electroportion for ex vivo editing of immune cells
Apart from complexing or conjugating GETs with some non-viral vectors, electroporation can directly increase the permeability of the cell membrane by hitting the cell membrane with electric pulses of sufficient intensity, allowing the penetration of GETs [157]. When the electroporation technique was first reported to be used for delivering GET, an editing frequency of 79% was observed in previously hard-to-transfect cells [158]. Later on, the procedure of electroporation was further optimized to reduce cell death [159]. This delivery system is convenient, effective and is suitable for mass production of genetically edited cells. Hence, it is currently the most used delivery system for ex vivo editing of immune cells [160, 161].
The electroporation technique provides a good platform for the mass production of chimeric antigen receptor (CAR) cells (Fig. 2a). CAR-T cell therapy is important personalized immunotherapeutic approach to treat cancer [162]. With this approach, the T cells could be reprogrammed by GET to effectively kill different types of cancers. Moreover, using genetically edited patient-derived T cells could largely avoid the host-verses-graft-diseases. Marson et. al. have reprogrammed the gene encoding the endogenous T cell receptor (TCR) to improve the cancer-targeting capacity of T cells. It was shown that the genetically edited T cells effectively recognize tumor antigens, leading to the suppression of tumor cell proliferation in vitro and inhibition of tumor growth in vivo [159]. Besides, electroporation-mediated genome editing can be also utilized in patient-derived stem cells which are considered as the cells of cancer origin. By inducing the key carcinogenic mutation in the cancer cell of origin, the personalized cancer models can be quickly established [163, 164].
Although convenient and effective, directly apply electroporation technique in vivo is invasive, which means it is currently not an convinient option for delivering GETs into tumors as personalized gene therapies. However, substantial efforts have been deveoted to developing in vivo electroporation approaches for effective and safe delivery of therapeutic reagents. Recchia et. al. have successfully conducted the CRISPR-mediated the knockout of the RHO gene carrying the P23H mutation in the mouse retina through electroporation. To inject the DNA solution, the sclera was pierced with a 3-gauge needle. Additionally, the pores on cells were opened by five 90 V square pulses of 50 milliseconds duration [165]. For the treatment of tumor, in vivo electroporation has been used to deliver the gene emcoding anticancer protein such as IL-15 [166]. However, the possibility of using intratumoral electroporation for the delivery of GETs to correct neoplastic genes still repuires further explorations.
GETs-based personalized anti-cancer therapies in clinical studies
Gene editing is a promising therapeutic option for the treatment of cancer, considerable efforts have been made to further elucidate the detailed mechanisms by which GETs target and modify human genes [167]. Moreover, the emerging of new generations of mega-nucleases, ZFNs, TALENs, and CRISPR-Cas9 systems have substantially enriched the toolbox for genome editing [168]. As a consequence, although genome editing is still relatively young in comparison to other cancer treatments, a lot of genome editing-based anti-cancer therapeutic methods have already gotten to the stage of clinical assessments. So far, 34 trials assessing the efficacy and safety of the genome editing-based anti-cancer therapies have been registered in the ClinicalTrials.gov database. Among them, the majority of studies are using genetically edited immune cells to fight against cancer. Also, given the fact that mega-nucleases, ZFNs, TALENs, and CRISPR-Cas9 systems have been all reported to efficiently perform genome editing in certain types of cells [169]. CRISPR-Cas9 systems are dominantly used in clinical studies. Notably, the clinical data from a phase I trial evaluating the safety and efficacy of reprogrammed T cells have been published. According to the report, CRISPR-Cas9 was used to knock out PD-1 gene in autologous T lymphocytes. These genetically edited T cells were then transplanted to patients with non-small cell lung cancer. When the trial was complete, no level 3-5 adverse events were observed. Moreover, two out of seven participants experienced stable disease with 17.6 and 22.0 weeks, the other five patients had progression disease. Thus, this cell therapy seems to be safe, but further studies with more rigorous evaluations are needed [170].
Additionally, the delivery systems for GETs of many trials are not specified in their ClinicalTrials.gov webpage. Among all the specified trials, 8 of them used non-viral delivery systems (Table 1). However, only one trial has the published data. In this trial, Cas9 and single guide RNA plasmids were transfected into patient derived T cells through electroporation to disrupt PD-1 gene. The edited T cells were used as immunotherapy for patients with refractory non-small-cell lung cancer. Among all the 12 patients who received the treatment, only grade 1/2 treatment-related adverse events occurred. Besides, the median progression-free survival and median overall survival were 7.7 weeks and 42.6 weeks [171]. These results suggest the encouraging safety and potential efficacy of the therapy. Furthermore, it is quite obvious that the current trend of non-viral delivery of CRISPR-Cas9 system is using electroporation. However, electroporation of T cells is associated with several limitations because it was reported that T cell viability, proliferation and gene expression could be affected by the electroporation procedure [172]. Hence, other non-viral delivery systems also hold promise for further facilitating the clinically applicable personalized anti-cancer therapies.
Conclusions
Personalized therapies provide great hopes for patients with cancer. Genome editing is an ideal way to implement personalized therapies because it makes it possible to modulate pro-tumor genes or reprogram the anti-tumor immune cells. As the most advanced GETs, CRISPR-Cas9-based genome editing is very popular in the field of personalized therapy. Moreover, a variety of non-viral delivery systems including electroporation, CPP, lipid delivery system, inorganic vector, and polymeric delivery system have been used to transport GETs into the cell nucleus. Although it is generously believed that the delivery efficiency of non-viral delivery systems is relatively lower compared to viral delivery systems, they are safer and have better feasibility. Currently, several clinical studies are designed to assess the therapeutic values of genetically edited immune cells. Moreover, electroporation is dominantly used in these trials for the delivery of GETs. It is expectable that more translational studies will be conducted to further evaluate the potential of genome editing in personalized anti-cancer therapies. In addition, future studies may focus on the development of non-toxic, highly efficient non-viral vectors that could mediate the in vivo delivery of GETs.
Availability of data and materials
Not applicable.
Abbreviations
- GET:
-
Genome editing tool
- DSB:
-
Double strand break
- HDR:
-
Homology-directed repair
- NHEJ:
-
Nonhomologous end joining
- ZFN:
-
Zinc-finger nuclease
- TALEN:
-
Transcription activator-like effector nuclease
- CRISPR:
-
Clustered regularly interspaced short palindromic repeats
- HPV:
-
Human papillomavirus
- PD-1:
-
Programmed cell death-1
- TIL:
-
Tumor infiltrating lymphocyte
- TALE:
-
Transcription activator-like effector
- A:
-
Adenine
- C:
-
Cytosine
- G:
-
Guanine
- T:
-
Thymine
- TRL:
-
Tumor-reactive lymphocyte
- sgRNA:
-
Single guide RNA
- PAM:
-
Protospacer adjacent motif
- I:
-
Inosine
- CAR:
-
Chimeric antigen receptor
- TCR:
-
T cell receptor
- CPP:
-
Cell-penetrating peptide
- LMWP:
-
Low-molecular-weight protamine
- BP:
-
Black phosphorus
- NIR:
-
Near infrared
References
Nolen SC, Evans MA, Fischer A, Corrada MM, Kawas CH, Bota DA. Cancer-Incidence, prevalence and mortality in the oldest-old. A comprehensive review Mech Ageing Dev. 2017;164:113–26.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trendì An Update. Cancer Epidemiol Biomark Prev. 2015;25:16–27.
Pucci C, Martinelli C, Ciofani G. Innovative approaches for cancer treatment: current perspectives and new challenges. Ecancermedicalscience. 2019;13:961-.
Schirrmacher V. From chemotherapy to biological therapy: A review of novel concepts to reduce the side effects of systemic cancer treatment (Review). Int J Oncol. 2019;54(2):407–19.
Pakkala S, Ramalingam SS. Personalized therapy for lung cancer: striking a moving target. JCI Insight. 2018;3(15):e120858.
Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol. 2020;20(11):651–68.
Xie YH, Chen YX, Fang JY. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct Target Ther. 2020;5(1):22.
Bayat Mokhtari R, Homayouni TS, Baluch N, Morgatskaya E, Kumar S, Das B, et al. Combination therapy in combating cancer. Oncotarget. 2017;8(23):38022–43.
Lan T, Chen L, Wei X. Inflammatory Cytokines in Cancer: Comprehensive Understanding and Clinical Progress in Gene Therapy. Cells. 2021;10(1):100.
Jackson SE, Chester JD. Personalised cancer medicine. Int J Cancer. 2015;137(2):262–6.
Das PK, Islam F, Lam AK. The Roles of Cancer Stem Cells and Therapy Resistance in Colorectal Carcinoma. Cells. 2020;9(6):1392.
Kontomanolis EN, Koutras A, Syllaios A, Schizas D, Mastoraki A, Garmpis N, et al. Role of Oncogenes and Tumor-suppressor Genes in Carcinogenesis: A Review. Anticancer Res. 2020;40(11):6009–15.
Anwer F, Gee KM, Iftikhar A, Baig M, Russ AD, Saeed S, et al. Future of Personalized Therapy Targeting Aberrant Signaling Pathways in Multiple Myeloma. Clin Lymphoma Myeloma Leuk. 2019;19(7):397–405.
Hazafa A, Mumtaz M, Farooq MF, Bilal S, Chaudhry SN, Firdous M, et al. CRISPR/Cas9: A powerful genome editing technique for the treatment of cancer cells with present challenges and future directions. Life Sci. 2020;263:118525-.
Sterner RC, Sterner RM. CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J. 2021;11(4):69.
Gonçalves GAR, Paiva RdMA. Gene therapy: advances, challenges and perspectives. Einstein (Sao Paulo Brazil). 2017;15(3):369–75.
Bosch JA, Birchak G, Perrimon N. Precise genome engineering in Drosophila using prime editing. Proc Natl Acad Sci U S A. 2021;118(1):e2021996118.
Nyerges Á, Csörgő B, Nagy I, Bálint B, Bihari P, Lázár V, et al. A highly precise and portable genome engineering method allows comparison of mutational effects across bacterial species. Proc Natl Acad Sci U S A. 2016;113(9):2502–7.
Ormond KE, Bombard Y, Bonham VL, Hoffman-Andrews L, Howard H, Isasi R, et al. The clinical application of gene editing: ethical and social issues. Per Med. 2019;16(4):337–50.
Gaj T, Gersbach CA, Barbas CF 3rd. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 2013;31(7):397–405.
Zaboikin M, Zaboikina T, Freter C, Srinivasakumar N. Non-Homologous End Joining and Homology Directed DNA Repair Frequency of Double-Stranded Breaks Introduced by Genome Editing Reagents. PLoS ONE. 2017;12(1):e0169931.
Kaniecki K, De Tullio L, Greene EC. A change of view: homologous recombination at single-molecule resolution. Nat Rev Genet. 2018;19(4):191–207.
Kim H, Kim J-S. A guide to genome engineering with programmable nucleases. Nat Rev Genet. 2014;15(5):321–34.
Doudna JA. The promise and challenge of therapeutic genome editing. Nature. 2020;578(7794):229–36.
Fernández A, Josa S, Montoliu L. A history of genome editing in mammals. Mamm Genome. 2017;28(7–8):237–46.
Maeder ML, Gersbach CA. Genome-editing Technologies for Gene and Cell Therapy. Mol Ther. 2016;24(3):430–46.
Chen M, Mao A, Xu M, Weng Q, Mao J, Ji J. CRISPR-Cas9 for cancer therapy: Opportunities and challenges. Cancer Lett. 2019;447:48–55.
Yin H, Kauffman KJ, Anderson DG. Delivery technologies for genome editing. Nat Rev Drug Discov. 2017;16(6):387–99.
He ZY, Men K, Qin Z, Yang Y, Xu T, Wei YQ. Non-viral and viral delivery systems for CRISPR-Cas9 technology in the biomedical field. Sci China Life Sci. 2017;60(5):458–67.
Lundstrom K. Viral Vectors in Gene Therapy. Diseases (Basel, Switzerland). 2018;6(2):42.
Redd Bowman KE, Lu P, Vander Mause ER, Lim CS. Advances in delivery vectors for gene therapy in liver cancer. Ther Deliv. 2020;11(1):833–50.
Rittiner JE, Moncalvo M, Chiba-Falek O, Kantor B. Gene-Editing Technologies Paired With Viral Vectors for Translational Research Into Neurodegenerative Diseases. Front Mol Neurosci. 2020;13:148.
Yokoo T, Kamimura K, Abe H, Kobayashi Y, Kanefuji T, Ogawa K, et al. Liver-targeted hydrodynamic gene therapy: Recent advances in the technique. World J Gastroenterol. 2016;22(40):8862–8.
Monahan PE, Négrier C, Tarantino M, Valentino LA, Mingozzi F. Emerging Immunogenicity and Genotoxicity Considerations of Adeno-Associated Virus Vector Gene Therapy for Hemophilia. J Clin Med. 2021;10(11):2471.
Schlimgen R, Howard J, Wooley D, Thompson M, Baden LR, Yang OO, et al. Risks Associated With Lentiviral Vector Exposures and Prevention Strategies. J Occup Environ Med. 2016;58(12):1159–66.
Nayerossadat N, Maedeh T, Ali PA. Viral and nonviral delivery systems for gene delivery. Adv biomedical Res. 2012;1:27-.
Ramamoorth M, Narvekar A. Non viral vectors in gene therapy- an overview. J Clin Diagn research: JCDR. 2015;9(1):GE01–6.
Won EJ, Park H, Chang SH, Kim JH, Kwon H, Cho YS, et al. One-shot dual gene editing for drug-resistant pancreatic cancer therapy. Biomaterials. 2021;279:121252.
Wen L, Zhao C, Song J, Ma L, Ruan J, Xia X, et al. CRISPR/Cas9-Mediated TERT Disruption in Cancer Cells. Int J Mol Sci. 2020;21(2):653.
Puig-Saus C, Ribas A. Gene editing: Towards the third generation of adoptive T-cell transfer therapies. Immuno-Oncology Technology. 2019;1:19–26.
Platt RJ, Chen S, Zhou Y, Yim MJ, Swiech L, Kempton HR, et al. CRISPR-Cas9 knockin mice for genome editing and cancer modeling. Cell. 2014;159(2):440–55.
Tröder SE, Zevnik B. History of genome editing: From meganucleases to CRISPR. Lab Anim. 2021;0(0):1–9.
Silva G, Poirot L, Galetto R, Smith J, Montoya G, Duchateau P, et al. Meganucleases and other tools for targeted genome engineering: perspectives and challenges for gene therapy. Curr Gene Ther. 2011;11(1):11–27.
Stoddard BL. Homing endonucleases: from microbial genetic invaders to reagents for targeted DNA modification. Structure (London, England : 1993). 2011;19(1):7–15.
Pâques F, Duchateau P. Meganucleases and DNA double-strand break-induced recombination: perspectives for gene therapy. Curr Gene Ther. 2007;7(1):49–66.
Gogarten JP, Hilario E. Inteins, introns, and homing endonucleases: recent revelations about the life cycle of parasitic genetic elements. BMC Evol Biol. 2006;6:94.
Arbuthnot P. Chapter 3 - Engineering Sequence-Specific DNA Binding Proteins for Antiviral Gene Editing. In: Arbuthnot P, editor. Gene Therapy for Viral Infections. Amsterdam: Academic Press; 2015. p. 63–94.
Lin Y, Wu Z, Guo W, Li J. Gene mutations in gastric cancer: a review of recent next-generation sequencing studies. Tumour Biol. 2015;36(10):7385–94.
Prior IA, Lewis PD, Mattos C. A comprehensive survey of Ras mutations in cancer. Can Res. 2012;72(10):2457–67.
Santos C, Martínez M, Lima M, Hao YJ, Simões N, Montiel R. Mitochondrial DNA mutations in cancer: a review. Curr Top Med Chem. 2008;8(15):1351–66.
Grizot S, Smith J, Daboussi F, Prieto J, Redondo P, Merino N, et al. Efficient targeting of a SCID gene by an engineered single-chain homing endonuclease. Nucleic Acids Res. 2009;37(16):5405–19.
Muñoz IG, Prieto J, Subramanian S, Coloma J, Redondo P, Villate M, et al. Molecular basis of engineered meganuclease targeting of the endogenous human RAG1 locus. Nucleic Acids Res. 2011;39(2):729–43.
Donoho G, Jasin M, Berg P. Analysis of gene targeting and intrachromosomal homologous recombination stimulated by genomic double-strand breaks in mouse embryonic stem cells. Mol Cell Biol. 1998;18(7):4070–8.
Elliott B, Richardson C, Winderbaum J, Nickoloff JA, Jasin M. Gene conversion tracts from double-strand break repair in mammalian cells. Mol Cell Biol. 1998;18(1):93–101.
Gouble A, Smith J, Bruneau S, Perez C, Guyot V, Cabaniols JP, et al. Efficient in toto targeted recombination in mouse liver by meganuclease-induced double-strand break. J Gene Med. 2006;8(5):616–22.
Szczepek M, Brondani V, Büchel J, Serrano L, Segal DJ, Cathomen T. Structure-based redesign of the dimerization interface reduces the toxicity of zinc-finger nucleases. Nat Biotechnol. 2007;25(7):786–93.
Wang L, Smith J, Breton C, Clark P, Zhang J, Ying L, et al. Meganuclease targeting of PCSK9 in macaque liver leads to stable reduction in serum cholesterol. Nat Biotechnol. 2018;36(8):717–25.
Yee JK. Off-target effects of engineered nucleases. Febs j. 2016;283(17):3239–48.
Gambardella V, Tarazona N, Cejalvo JM, Lombardi P, Huerta M, Roselló S, et al. Personalized Medicine: Recent Progress in Cancer Therapy. Cancers (Basel). 2020;12(4):1009.
Klug A. The discovery of zinc fingers and their development for practical applications in gene regulation and genome manipulation. Q Rev Biophys. 2010;43(1):1–21.
Urnov FD, Rebar EJ, Holmes MC, Zhang HS, Gregory PD. Genome editing with engineered zinc finger nucleases. Nat Rev Genet. 2010;11(9):636–46.
Gaj T, Gersbach CA, Barbas CF 3rd. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 2013;31(7):397–405.
Jabalameli HR, Zahednasab H, Karimi-Moghaddam A, Jabalameli MR. Zinc finger nuclease technology: Advances and obstacles in modelling and treating genetic disorders. Gene. 2015;558(1):1–5.
Liu PQ, Chan EM, Cost GJ, Zhang L, Wang J, Miller JC, et al. Generation of a triple-gene knockout mammalian cell line using engineered zinc-finger nucleases. Biotechnol Bioeng. 2010;106(1):97–105.
Lombardo A, Genovese P, Beausejour CM, Colleoni S, Lee YL, Kim KA, et al. Gene editing in human stem cells using zinc finger nucleases and integrase-defective lentiviral vector delivery. Nat Biotechnol. 2007;25(11):1298–306.
Shankar S, Sreekumar A, Prasad D, Das AV, Pillai MR. Genome editing of oncogenes with ZFNs and TALENs: caveats in nuclease design. Cancer Cell Int. 2018;18(1):169.
Ren C, Gao C, Li X, Xiong J, Shen H, Wang L, et al. The Antitumor Efficiency of Zinc Finger Nuclease Combined with Cisplatin and Trichostatin A in Cervical Cancer Cells. Anticancer Agents Med Chem. 2020;20(17):2125–35.
Zhao J, Lin Q, Song Y, Liu D. Universal CARs, universal T cells, and universal CAR T cells. J Hematol Oncol. 2018;11(1):132-.
Joung JK, Sander JD. TALENs: a widely applicable technology for targeted genome editing. Nat Rev Mol Cell Biol. 2013;14(1):49–55.
Nemudryi AA, Valetdinova KR, Medvedev SP, Zakian SM. TALEN and CRISPR/Cas Genome Editing Systems: Tools of Discovery. Acta naturae. 2014;6(3):19–40.
Khan SH. Genome-Editing Technologies: Concept, Pros, and Cons of Various Genome-Editing Techniques and Bioethical Concerns for Clinical Application. Mol Ther Nucleic Acids. 2019;16:326–34.
Cermak T, Doyle EL, Christian M, Wang L, Zhang Y, Schmidt C, et al. Efficient design and assembly of custom TALEN and other TAL effector-based constructs for DNA targeting. Nucleic Acids Res. 2011;39(12):e82.
Hockemeyer D, Wang H, Kiani S, Lai CS, Gao Q, Cassady JP, et al. Genetic engineering of human pluripotent cells using TALE nucleases. Nat Biotechnol. 2011;29(8):731–4.
Li T, Huang S, Zhao X, Wright DA, Carpenter S, Spalding MH, et al. Modularly assembled designer TAL effector nucleases for targeted gene knockout and gene replacement in eukaryotes. Nucleic Acids Res. 2011;39(14):6315–25.
Liu J, Li C, Yu Z, Huang P, Wu H, Wei C, et al. Efficient and specific modifications of the Drosophila genome by means of an easy TALEN strategy. J Genet Genomics. 2012;39(5):209–15.
Miller JC, Tan S, Qiao G, Barlow KA, Wang J, Xia DF, et al. A TALE nuclease architecture for efficient genome editing. Nat Biotechnol. 2011;29(2):143–8.
Wood AJ, Lo TW, Zeitler B, Pickle CS, Ralston EJ, Lee AH, et al. Targeted genome editing across species using ZFNs and TALENs. Science. 2011;333(6040):307.
Li H, Yang Y, Hong W, Huang M, Wu M, Zhao X. Applications of genome editing technology in the targeted therapy of human diseases: mechanisms, advances and prospects. Signal Transduct Target Ther. 2020;5(1):1.
Zhuang P-Y, Zhang K-W, Wang J-D, Zhou X-P, Liu Y-B, Quan Z-W, et al. Effect of TALEN-mediated IL-6 knockout on cell proliferation, apoptosis, invasion and anti-cancer therapy in hepatocellular carcinoma (HCC-LM3) cells. Oncotarget. 2017;8(44):77915–27.
Shankar S, Prasad D, Sanawar R, Das AV, Pillai MR. TALEN based HPV-E7 editing triggers necrotic cell death in cervical cancer cells. Sci Rep. 2017;7(1):5500.
Menger L, Sledzinska A, Bergerhoff K, Vargas FA, Smith J, Poirot L, et al. TALEN-Mediated Inactivation of PD-1 in Tumor-Reactive Lymphocytes Promotes Intratumoral T-cell Persistence and Rejection of Established Tumors. Can Res. 2016;76(8):2087–93.
Ishino Y, Shinagawa H, Makino K, Amemura M, Nakata A. Nucleotide sequence of the iap gene, responsible for alkaline phosphatase isozyme conversion in Escherichia coli, and identification of the gene product. J Bacteriol. 1987;169(12):5429–33.
Jore MM, Brouns SJ, van der Oost J. RNA in defense: CRISPRs protect prokaryotes against mobile genetic elements. Cold Spring Harb Perspect Biol. 2012;4(6):a003657.
Nidhi S, Anand U, Oleksak P, Tripathi P, Lal JA, Thomas G, et al. Novel CRISPR-Cas Systems: An Updated Review of the Current Achievements, Applications, and Future Research Perspectives. Int J Mol Sci. 2021;22(7):3327.
Uddin F, Rudin CM, Sen T. CRISPR Gene Therapy: Applications, Limitations, and Implications for the Future. Frontiers in oncol. 2020;10:1387.
Jiang F, Doudna JA. CRISPR–Cas9 Structures and Mechanisms. Annu Rev Biophys. 2017;46(1):505–29.
Lino CA, Harper JC, Carney JP, Timlin JA. Delivering CRISPR: a review of the challenges and approaches. Drug Deliv. 2018;25(1):1234–57.
Cong L, Ran FA, Cox D, Lin S, Barretto R, Habib N, et al. Multiplex genome engineering using CRISPR/Cas systems. Science. 2013;339(6121):819–23.
Pawelczak KS, Gavande NS, VanderVere-Carozza PS, Turchi JJ. Modulating DNA Repair Pathways to Improve Precision Genome Engineering. ACS Chem Biol. 2018;13(2):389–96.
Komor AC, Kim YB, Packer MS, Zuris JA, Liu DR. Programmable editing of a target base in genomic DNA without double-stranded DNA cleavage. Nature. 2016;533(7603):420–4.
Komor AC, Zhao KT, Packer MS, Gaudelli NM, Waterbury AL, Koblan LW, et al. Improved base excision repair inhibition and bacteriophage Mu Gam protein yields C:G-to-T:A base editors with higher efficiency and product purity. Sci Adv. 2017;3(8):eaao4774.
Cox DBT, Gootenberg JS, Abudayyeh OO, Franklin B, Kellner MJ, Joung J, et al. RNA editing with CRISPR-Cas13. Science. 2017;358(6366):1019–27.
Abudayyeh OO, Gootenberg JS, Franklin B, Koob J, Kellner MJ, Ladha A, et al. A cytosine deaminase for programmable single-base RNA editing. Science. 2019;365(6451):382–6.
Kurt IC, Zhou R, Iyer S, Garcia SP, Miller BR, Langner LM, et al. CRISPR C-to-G base editors for inducing targeted DNA transversions in human cells. Nat Biotechnol. 2021;39(1):41–6.
Lei Z-N, Teng Q-X, Wu Z-X, Ping F-F, Song P, Wurpel JND, et al. Overcoming multidrug resistance by knockout of ABCB1 gene using CRISPR/Cas9 system in SW620/Ad300 colorectal cancer cells. MedComm. 2021;2(4):765–77.
Nakamura M, Gao Y, Dominguez AA, Qi LS. CRISPR technologies for precise epigenome editing. Nat Cell Biol. 2021;23(1):11–22.
Gasperini M, Hill AJ, McFaline-Figueroa JL, Martin B, Kim S, Zhang MD, et al. A Genome-wide Framework for Mapping Gene Regulation via Cellular Genetic Screens. Cell. 2019;176(1–2):377-90.e19.
Jusiak B, Cleto S, Perez-Piñera P, Lu TK. Engineering Synthetic Gene Circuits in Living Cells with CRISPR Technology. Trends Biotechnol. 2016;34(7):535–47.
Perdigoto CN. Epigenetic cancer evolution, one cell at a time. Nat Rev Genet. 2019;20(8):434–5.
Morita S, Noguchi H, Horii T, Nakabayashi K, Kimura M, Okamura K, et al. Targeted DNA demethylation in vivo using dCas9–peptide repeat and scFv–TET1 catalytic domain fusions. Nat Biotechnol. 2016;34(10):1060–5.
Wang H, Guo R, Du Z, Bai L, Li L, Cui J, et al. Epigenetic Targeting of Granulin in Hepatoma Cells by Synthetic CRISPR dCas9 Epi-suppressors. Molecular Therapy - Nucleic Acids. 2018;11:23–33.
Liu C, Zhang L, Liu H, Cheng K. Delivery strategies of the CRISPR-Cas9 gene-editing system for therapeutic applications. J Control Release. 2017;266:17–26.
Gong J, Wang HX, Lao YH, Hu H, Vatan N, Guo J, et al. A Versatile Nonviral Delivery System for Multiplex Gene-Editing in the Liver. Adv Mater. 2020;32(46):e2003537.
Wilbie D, Walther J, Mastrobattista E. Delivery Aspects of CRISPR/Cas for in Vivo Genome Editing. Acc Chem Res. 2019;52(6):1555–64.
Rui Y, Wilson DR, Green JJ. Non-Viral Delivery To Enable Genome Editing. Trends Biotechnol. 2019;37(3):281–93.
Li J, Røise JJ, He M, Das R, Murthy N. Non-viral strategies for delivering genome editing enzymes. Adv Drug Deliv Rev. 2021;168:99–117.
Faneca H. Non-Viral Gene Delivery Systems Pharmaceutics. 2021;13(4):446.
Wang M, Glass ZA, Xu Q. Non-viral delivery of genome-editing nucleases for gene therapy. Gene Ther. 2017;24(3):144–50.
Van de Vyver T, De Smedt SC, Raemdonck K. Modulating intracellular pathways to improve non-viral delivery of RNA therapeutics. Adv Drug Delivery Rev. 2022;181:114041.
Böhmová E, Machová D, Pechar M, Pola R, Venclíková K, Janoušková O, et al. Cell-penetrating peptides: a useful tool for the delivery of various cargoes into cells. Physiol Res. 2018;67(Suppl 2):S267–79.
Gaj T, Guo J, Kato Y, Sirk SJ, Barbas CF 3rd. Targeted gene knockout by direct delivery of zinc-finger nuclease proteins. Nat Methods. 2012;9(8):805–7.
Liu J, Gaj T, Patterson JT, Sirk SJ, Barbas CF III. Cell-penetrating peptide-mediated delivery of TALEN proteins via bioconjugation for genome engineering. PLoS ONE. 2014;9(1):e85755.
Jain PK, Lo JH, Rananaware S, Downing M, Panda A, Tai M, et al. Non-viral delivery of CRISPR/Cas9 complex using CRISPR-GPS nanocomplexes. Nanoscale. 2019;11(44):21317–23.
Lostalé-Seijo I, Louzao I, Juanes M, Montenegro J. Peptide/Cas9 nanostructures for ribonucleoprotein cell membrane transport and gene edition. Chem Sci. 2017;8(12):7923–31.
Del’Guidice T, Lepetit-Stoffaes JP, Bordeleau LJ, Roberge J, Théberge V, Lauvaux C, et al. Membrane permeabilizing amphiphilic peptide delivers recombinant transcription factor and CRISPR-Cas9/Cpf1 ribonucleoproteins in hard-to-modify cells. PLoS ONE. 2018;13(4):e0195558.
Kim SM, Shin SC, Kim EE, Kim S-H, Park K, Oh SJ, et al. Simple in Vivo Gene Editing via Direct Self-Assembly of Cas9 Ribonucleoprotein Complexes for Cancer Treatment. ACS Nano. 2018;12(8):7750–60.
Ruseska I, Zimmer A. Internalization mechanisms of cell-penetrating peptides. Beilstein J Nanotechnol. 2020;11:101–23.
Kamei N, Bech Nielsen EJ, Nakakubo T, Aoyama Y, Rahbek UL, Pedersen BL, et al. Applicability and Limitations of Cell-Penetrating Peptides in Noncovalent Mucosal Drug or Carrier Delivery Systems. J Pharm Sci. 2016;105(2):747–53.
Rosenblum D, Gutkin A, Kedmi R, Ramishetti S, Veiga N, Jacobi AM, et al. CRISPR-Cas9 genome editing using targeted lipid nanoparticles for cancer therapy. Sci Adv. 2020;6(47):eabc9450.
Shrestha H, Bala R, Arora S. Lipid-Based Drug Delivery Systems. J Pharm. 2014;2014:801820-.
Ashok B, Peppas NA, Wechsler ME. Lipid- and polymer-based nanoparticle systems for the delivery of CRISPR/Cas9. J Drug Deliv Sci Technol. 2021;65:102728.
Naseri N, Valizadeh H, Zakeri-Milani P. Solid Lipid Nanoparticles and Nanostructured Lipid Carriers: Structure. Preparation and Application Adv Pharm Bull. 2015;5(3):305–13.
Müller RH, Radtke M, Wissing SA. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv Drug Deliv Rev. 2002;54(Suppl 1):S131–55.
Zuris JA, Thompson DB, Shu Y, Guilinger JP, Bessen JL, Hu JH, et al. Cationic lipid-mediated delivery of proteins enables efficient protein-based genome editing in vitro and in vivo. Nat Biotechnol. 2015;33(1):73–80.
Duan L, Ouyang K, Xu X, Xu L, Wen C, Zhou X, et al. Nanoparticle Delivery of CRISPR/Cas9 for Genome Editing. Front Genet. 2021;12(788):1-10.
Wei T, Cheng Q, Min Y-L, Olson EN, Siegwart DJ. Systemic nanoparticle delivery of CRISPR-Cas9 ribonucleoproteins for effective tissue specific genome editing. Nat Commun. 2020;11(1):3232.
Shi Z, Zhou Y, Fan T, Lin Y, Zhang H, Mei L. Inorganic nano-carriers based smart drug delivery systems for tumor therapy. Smart Materials in Medicine. 2020;1:32–47.
Wang W, Wang J, Ding Y. Gold nanoparticle-conjugated nanomedicine: design, construction, and structure–efficacy relationship studies. Journal of Materials Chemistry B. 2020;8(22):4813–30.
Ye X, Liang X, Chen Q, Miao Q, Chen X, Zhang X, et al. Surgical Tumor-Derived Personalized Photothermal Vaccine Formulation for Cancer Immunotherapy. ACS Nano. 2019;13(3):2956–68.
Zeng X, Li G, Song D, Li S, Li G, Li L. Control and Simulation of Auxiliary Drive and Regenerative Brake for Hydraulic Hub-motor Hybrid System. Hunan Daxue Xuebao/Journal of Hunan University Natural Sciences. 2017;44(10):9–16 and 24.
Zhang X, Luo L, Li L, He Y, Cao W, Liu H, et al. Trimodal synergistic antitumor drug delivery system based on graphene oxide. Nanomed Nanotechnol Biol Med. 2019;15(1):142–52.
Mout R, Ray M, Yesilbag Tonga G, Lee Y-W, Tay T, Sasaki K, et al. Direct Cytosolic Delivery of CRISPR/Cas9-Ribonucleoprotein for Efficient Gene Editing. ACS Nano. 2017;11(3):2452–8.
Alsaiari SK, Patil S, Alyami M, Alamoudi KO, Aleisa FA, Merzaban JS, et al. Endosomal Escape and Delivery of CRISPR/Cas9 Genome Editing Machinery Enabled by Nanoscale Zeolitic Imidazolate Framework. J Am Chem Soc. 2018;140(1):143–6.
Zhou Q, Chen Q, Tong Y, Wang J. Light-Induced Ambient Degradation of Few-Layer Black Phosphorus: Mechanism and Protection. Angew Chem Int Ed Engl. 2016;55(38):11437–41.
Zhang W, Huynh T, Xiu P, Zhou B, Ye C, Luan B, et al. Revealing the importance of surface morphology of nanomaterials to biological responses: Adsorption of the villin headpiece onto graphene and phosphorene. Carbon. 2015;94:895–902.
Zhou W, Cui H, Ying L, Yu X-F. Enhanced Cytosolic Delivery and Release of CRISPR/Cas9 by Black Phosphorus Nanosheets for Genome Editing. Angew Chem Int Ed. 2018;57(32):10268–72.
Alyami MZ, Alsaiari SK, Li Y, Qutub SS, Aleisa FA, Sougrat R, et al. Cell-Type-Specific CRISPR/Cas9 Delivery by Biomimetic Metal Organic Frameworks. J Am Chem Soc. 2020;142(4):1715–20.
Chen G, Qiu H, Prasad PN, Chen X. Upconversion nanoparticles: design, nanochemistry, and applications in theranostics. Chem Rev. 2014;114(10):5161–214.
Pan Y, Yang J, Luan X, Liu X, Li X, Yang J, et al. Near-infrared upconversion-activated CRISPR-Cas9 system: A remote-controlled gene editing platform. Science advances. 2019;5(4):eaav7199-eaav.
Nam K, Jung S, Nam J-P, Kim SW. Poly(ethylenimine) conjugated bioreducible dendrimer for efficient gene delivery. J Control Release. 2015;220:447–55.
Onishi H, Machida Y. Biodegradation and distribution of water-soluble chitosan in mice. Biomaterials. 1999;20(2):175–82.
Park MR, Han KO, Han IK, Cho MH, Nah JW, Choi YJ, et al. Degradable polyethylenimine-alt-poly(ethylene glycol) copolymers as novel gene carriers. J Control Release. 2005;105(3):367–80.
Verma IM, Somia N. Gene therapy - promises, problems and prospects. Nature. 1997;389(6648):239–42.
Wang S, Tan M, Zhong Z, Chen M, Wang Y. Nanotechnologies for Curcumin: An Ancient Puzzler Meets Modern Solutions. J Nanomaterials. 2011;2011:723178.
Liu C, Wan T, Wang H, Zhang S, Ping Y, Cheng Y. A boronic acid–rich dendrimer with robust and unprecedented efficiency for cytosolic protein delivery and CRISPR-Cas9 gene editing. Science Advances. 2019;5(6):eaaw8922.
Sun W, Ji W, Hall JM, Hu Q, Wang C, Beisel CL, et al. Self-Assembled DNA Nanoclews for the Efficient Delivery of CRISPR–Cas9 for Genome Editing. Angew Chem Int Ed. 2015;54(41):12029–33.
Tan Z, Jiang Y, Ganewatta MS, Kumar R, Keith A, Twaroski K, et al. Block Polymer Micelles Enable CRISPR/Cas9 Ribonucleoprotein Delivery: Physicochemical Properties Affect Packaging Mechanisms and Gene Editing Efficiency. Macromolecules. 2019;52(21):8197–206.
Yue H, Zhou X, Cheng M, Xing D. Graphene oxide-mediated Cas9/sgRNA delivery for efficient genome editing. Nanoscale. 2018;10(3):1063–71.
Chen G, Abdeen AA, Wang Y, Shahi PK, Robertson S, Xie R, et al. A biodegradable nanocapsule delivers a Cas9 ribonucleoprotein complex for in vivo genome editing. Nat Nanotechnol. 2019;14(10):974–80.
Lima SAC, Reis S. Polymeric Carriers for Biomedical and Nanomedicine Application. Polymers. 2021;13(8):1261.
Peng L, Wagner E. Polymeric Carriers for Nucleic Acid Delivery: Current Designs and Future Directions. Biomacromol. 2019;20(10):3613–26.
Wan T, Chen Y, Pan Q, Xu X, Kang Y, Gao X, et al. Genome editing of mutant KRAS through supramolecular polymer-mediated delivery of Cas9 ribonucleoprotein for colorectal cancer therapy. J Control Release. 2020;322:236–47.
Zhang Q, Kuang G, He S, Liu S, Lu H, Li X, et al. Chain-shattering Pt(IV)-backboned polymeric nanoplatform for efficient CRISPR/Cas9 gene editing to enhance synergistic cancer therapy. Nano Res. 2021;14(3):601–10.
Kaneko T. Genome Editing in Mouse and Rat by Electroporation. Methods Mol Biol. 2017;1630:81–9.
Kim S, Kim D, Cho SW, Kim J, Kim J-S. Highly efficient RNA-guided genome editing in human cells via delivery of purified Cas9 ribonucleoproteins. Genome Res. 2014;24(6):1012–9.
Roth TL, Puig-Saus C, Yu R, Shifrut E, Carnevale J, Li PJ, et al. Reprogramming human T cell function and specificity with non-viral genome targeting. Nature. 2018;559(7714):405–9.
Bailey SR, Maus MV. Gene editing for immune cell therapies. Nat Biotechnol. 2019;37(12):1425–34.
Robbins GM, Wang M, Pomeroy EJ, Moriarity BS. Nonviral genome engineering of natural killer cells. Stem Cell Res Ther. 2021;12(1):350-.
Cruz-Ramos M, García-Foncillas J. CAR-T cell and Personalized Medicine. Adv Exp Med Biol. 2019;1168:131–45.
Feng W, Cao Z, Lim PX, Zhao H, Luo H, Mao N, et al. Rapid interrogation of cancer cell of origin through CRISPR editing. Proc Natl Acad Sci U S A. 2021;118(32):e2110344118.
Callahan SJ, Tepan S, Zhang YM, Lindsay H, Burger A, Campbell NR, et al. Cancer modeling by Transgene Electroporation in Adult Zebrafish (TEAZ). Dis Model Mech. 2018;11(9):dmm034561.
Latella MC, Di Salvo MT, Cocchiarella F, Benati D, Grisendi G, Comitato A, et al. In vivo Editing of the Human Mutant Rhodopsin Gene by Electroporation of Plasmid-based CRISPR/Cas9 in the Mouse Retina. Mol Therapy - Nucleic Acids. 2016;5:e389.
Ugen KE, Kutzler MA, Marrero B, Westover J, Coppola D, Weiner DB, et al. Regression of subcutaneous B16 melanoma tumors after intratumoral delivery of an IL-15-expressing plasmid followed by in vivo electroporation. Cancer Gene Ther. 2006;13(10):969–74.
Khalil AM. The genome editing revolution: review. J Genet Eng Biotechnol. 2020;18(1):68.
Siva N, Gupta S, Gupta A, Shukla JN, Malik B, Shukla N. Genome-editing approaches and applications: a brief review on CRISPR technology and its role in cancer. 3 Biotech. 2021;11(3):146.
Rodríguez-Rodríguez DR, Ramírez-Solís R, Garza-Elizondo MA, Garza-Rodríguez MDL, Barrera-Saldaña HA. Genome editing: A perspective on the application of CRISPR/Cas9 to study human diseases (Review). Int J Mol Med. 2019;43(4):1559–74.
Lu Y, Xue J, Deng T, Zhou X, Yu K, Huang M, et al. A phase I trial of PD-1 deficient engineered T cells with CRISPR/Cas9 in patients with advanced non-small cell lung cancer. J Clin Oncol. 2018;36(15_suppl):3050-.
Lu Y, Xue J, Deng T, Zhou X, Yu K, Deng L, et al. Safety and feasibility of CRISPR-edited T cells in patients with refractory non-small-cell lung cancer. Nat Med. 2020;26(5):732–40.
Shi J, Ma Y, Zhu J, Chen Y, Sun Y, Yao Y, et al. A Review on Electroporation-Based Intracellular Delivery. Molecules (Basel, Switzerland). 2018;23(11):3044.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Science Foundation for Excellent Young Scholars (32122052) and National Natural Science Foundation Regional Innovation and Development (No. U19A2003).
Author information
Authors and Affiliations
Contributions
X.W. and X.Z. designed this study. T.L. and H.Q. drafted the manuscript. T.L. and H.Q. and M.L. revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
No ethics approval was required for this review that did not involve patients or patient data.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lan, T., Que, H., Luo, M. et al. Genome editing via non-viral delivery platforms: current progress in personalized cancer therapy. Mol Cancer 21, 71 (2022). https://doi.org/10.1186/s12943-022-01550-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12943-022-01550-8