Abstract
Background
Klebsiella aerogenes has been reclassified from Enterobacter to Klebsiella genus due to its phenotypic and genotypic similarities with Klebsiella pneumoniae. It is unclear if clinical outcomes are also more similar. This study aims to assess clinical outcomes of bloodstreams infections (BSI) caused by K. aerogenes, K. pneumoniae and Enterobacter cloacae, through secondary data analysis, nested in PRO-BAC cohort study.
Methods
Hospitalized patients between October 2016 and March 2017 with monomicrobial BSI due to K. aerogenes, K. pneumoniae or E. cloacae were included. Primary outcome was a composite clinical outcome including all-cause mortality or recurrence until 30 days follow-up. Secondary outcomes were fever ≥ 72 h, persistent bacteraemia, and secondary device infection. Multilevel mixed-effect Poisson regression was used to estimate the association between microorganisms and outcome.
Results
Overall, 29 K. aerogenes, 77 E. cloacae and 337 K. pneumoniae BSI episodes were included. Mortality or recurrence was less frequent in K. aerogenes (6.9%) than in E. cloacae (20.8%) or K. pneumoniae (19.0%), but statistical difference was not observed (rate ratio (RR) 0.35, 95% CI 0.08 to 1.55; RR 0.42, 95% CI 0.10 to 1.71, respectively). Fever ≥ 72 h and device infection were more common in K. aerogenes group. In the multivariate analysis, adjusted for confounders (age, sex, BSI source, hospital ward, Charlson score and active antibiotic therapy), the estimates and direction of effect were similar to crude results.
Conclusions
Results suggest that BSI caused by K. aerogenes may have a better prognosis than E. cloacae or K. pneumoniae BSI.
Similar content being viewed by others
Background
Bloodstream infection (BSI) is one of the infectious syndrome with the highest health burden and is associated with important costs to the healthcare system, [1,2,3,4]and in the last years the incidence of Enterobacterales BSI has been increasing [5,6,7,8,9,10,11,12,13].
Studies estimate that overall mortality in K. pneumoniae BSI can range from 20 to 54%, being particularly high in KPC-producing K. pneumoniae infections [12, 14,15,16,17,18,19,20]. Enterobacter cloacae BSI mortality seems to be lower than K. pneumoniae, ranging from 19 to 33%, [14, 21,22,23,24] with a risk of recurrence between 11 to 21%, higher in cases with extended-spectrum beta-lactamase (ESBL) production [22, 24,25,26]. Most of the studies report K. aerogenes outcomes aggregated in Enterobacter genus. Though, K. aerogenes BSI mortality appears to be lower than in Enterobacter spp. infections, between 10 and 21% [21, 27].
Since 1971, taxonomic studies have suggested that Enterobacter aerogenes should be classified into Klebsiella genus, due to its phenotypic and genotypic similarities to K. pneumoniae [28,29,30,31]. Recently, Tindall et al. has proposed to officially change its name to K. aerogenes and Clinical and Laboratory Standards Institute (CLSI) and European Committee on Antimicrobial Susceptibility Testing (EUCAST) have implemented it in their official documents [32, 33]. Genomic data also suggest that K. aerogenes could be more virulent than E. cloacae, since it possess virulence-encoding genes that were also identified in K. pneumoniae, but not described in E. cloacae [34,35,36]. If these similarities between K. aerogenes and K. pneumoniae translate into similar clinical outcomes is still to be determined. Some studies had tried to compare outcomes in K. aerogenes and E. cloacae BSI, but their findings have been contradictory and inconclusive [37,38,39,40]. We didn’t find any study comparing clinical outcomes in K. aerogenes and K. pneumoniae BSI.
This study aims to assess the clinical outcomes in patients with BSI caused by K. aerogenes, K. pneumoniae and E. cloacae, by exploring the association between a clinical composite outcome (mortality or recurrence) and these pathogens.
Methods
Study design
A secondary data analysis, nested in the PRO-BAC observational cohort study was performed. PRO-BAC was a Spanish multicentre study that prospectively included episodes of microbiological confirmed bacteraemia in hospitalised patients between 1st October 2016 and 31st March 2017 (Clinicaltrials.gov NCT03148769; Register date 05/04/2017) [41]. Screening was done by daily review of blood culture results; individuals without systemic signs or symptoms of infection and subsequent episodes caused by the same microorganism within three months of the primary episode were also excluded [41]. Microorganism identification and susceptibility testing was performed according to the local laboratory guidelines that were aligned with the 2016 EUCAST recommendations or the CLSI guidelines. Clinical outcomes such as fever ≥ 72 h, complications secondary to treatment and metastatic infections were recorded at 30-days follow-up after bacteraemia diagnosis or hospital discharge. Mortality and BSI recurrence were assessed at 30-days, with post-discharge follow-up done by reviewing medical records and national death registry [41].
Inclusion criteria for this study was adult individuals (≥ 18 years old) with BSI caused by K. aerogenes, K. pneumoniae or E. cloacae, each a different exposure group. Polymicrobial bacteraemia episodes were excluded. Primary outcome was a composite clinical outcome that includes all-cause mortality or recurrence within 30 days after BSI diagnosis. BSI recurrence was defined as bacteraemia with the same microorganism after negative blood cultures or clinical improvement and completion of active antimicrobial therapy [42]. Secondary outcomes were persistent fever, persistent BSI, and device infection secondary to BSI. Persistent fever was defined as fever ≥ 72 h in patients treated with an in vitro active antimicrobial drug [42]. Persistent BSI was defined as positive blood culture with the same microorganism after 72 h of active antibiotic therapy [42]. Secondary infection included endovascular or orthopaedic devices infection secondary to BSI [42].
Setting of BSI acquisition was considered nosocomial if BSI occurred more than 48 h after hospital admission. Episodes were considered HAI if any of the following was present: intravenous therapy, wound care or specialized nursing care at home, dialysis, radiotherapy or chemotherapy, two or more attendances to specialized outpatient clinic, residency in a nursing home or long term care facility in the 30 days before BSI; major surgery 30 days before BSI (90 days if implant); or hospitalization for more than 2 days in acute or chronic care hospital in the 90 days before BSI. Episodes that don’t fulfil these criteria were considered community acquired.
Date of blood sample collection was considered the start of follow-up. In individuals with a primary outcome event, end of follow-up was considered when one of the events from the composite outcome was reached (death or recurrence), whatever happens first. In individuals without primary outcome, the date of last assessment was considered as the end of follow-up. In case of missing data in this variable, the date of hospital discharge was considered. Follow-up was right censored at 30 days after blood culture collection, according to the original study protocol. Loss to follow-up was considered when there was neither the date of last assessment nor date of hospital discharge.
Statistical analysis
Frequencies and proportions were used to describe the cohort characteristics and reported through tabulation of categorical variables by the exposure variable (K. aerogenes, E. cloacae and K. pneumoniae), including missing data. Median and interquartile range were calculated to describe non-normally distributed data and stratified by the microorganism group. All records in the final sample size for data analysis were included in the univariate and multivariate analysis, regardless of missing data in covariates.
To assess the impact of potential bias caused by excluding individuals with missing data on follow-up time, patients included in the final analysis were compared with the patients excluded. Differences in these groups were inspected and assessed using Pearson chi-squared test for categorical variables and Wilcoxon rank-sum test for continuous skewed variables (Additional file 1: Table S1).
Univariate analysis used two models: model 1 compares outcomes in K. aerogenes and E. cloacae groups with a baseline group of K. pneumoniae; model 2 compares outcomes in K. aerogenes and K. pneumoniae groups with a baseline group of E. cloacae. Rate of the outcome per 1000 persons-day and the 95% confidence interval for the exposure variable and other independent variables was calculated. Rate ratio and the 95% confidence interval of the association between the composite clinical outcome and the different microorganism’s groups and other independent variables was calculated using a multilevel mixed-effect Poisson regression model considering hospital as the first level, assuming clustering of observations within hospital. Wald test was used to test for association.
A direct acyclic diagram (DAG) was built to describe the conceptual framework between potential confounders and other independent variables in the association between exposure (K. aerogenes, K. pneumoniae or E. cloacae BSI) and outcome (death or recurrence), based on literature review (Additional file 1: Fig. S1). Possible confounders identified in the conceptual framework were BSI source, hospital ward, comorbidities, age, and antibiotic therapy. DAG was useful to exclude other independent variables from the multivariate model that can be in the causal pathway (severity) or ancestors of the exposure and/or outcome (BSI acquisition, antibiotic resistance, devices, and procedures). Disease severity is a mediator of the association between the exposure (microorganisms) and the outcome (death or recurrence), which may bias the results if included in the analysis. Ancestors are variables that are indirectly associated with the exposure or outcome through confounders; their inclusion in the model is redundant and can compromise model stability when missing data is an issue.
Multilevel mixed-effect Poisson regression model was used to calculate the crude and adjusted rate ratio for each possible confounder. Multicollinearity was checked by using variance inflation factor and variables with cut-off higher than 10 were excluded. The final multivariate model included all the variables without multicollinearity defined a priori as confounders (age and sex) and identified through the conceptual framework (BSI source, hospital ward, Charlson score and active antibiotic therapy).
Results
Descriptive analysis
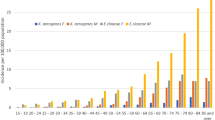
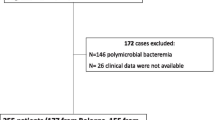
From the 664 records in the PRO-BAC dataset with BSI caused by the microorganisms of interest, 132 were excluded due to exclusion criteria (131 polymicrobial BSI and 1 age < 18-year-old) and 89 were excluded due to missing data on follow-up time. The final sample size for analysis included 443 BSI episodes: 29 K. aerogenes, 77 E. cloacae and 337 K. pneumoniae (Additional file 1: Fig. S2).
The median follow-up time was 30 days (IQR 11, 71) and similar between exposure groups (K. pneumoniae 31 days vs E. cloacae 26 days vs. K. aerogenes 30 days) (Table 1).
Comparing between groups, patients with E. cloacae BSI had more frequent nosocomial infections (K. pneumoniae 46.0%, n = 155 vs. E. cloacae 71.4%, n = 55 vs. K. aerogenes 41.4%, n = 12), less common BSI secondary to urinary source (K. pneumoniae 41.8%, n = 141 vs. E. cloacae 18.2%, n = 14 vs. K. aerogenes 37.9%, n = 11) and the length of hospital stay was longer (K. pneumoniae 14 days vs. E. cloacae 21 days vs. K. aerogenes 11 days); on the other hand, in K. pneumoniae group, antibiotic resistance was more common (ESBL: K. pneumoniae 23.4%, n = 79 vs. E. cloacae 2.6%, n = 2 vs. K. aerogenes 0%, n = 0; carbapenemase production: K. pneumoniae 8.8%, n = 33 vs. E. cloacae 0%, n = 0 vs. K. aerogenes 3.4%, n = 1) but active empiric antibiotic therapy more frequent (K. pneumoniae 74.2%, n = 250 vs. E. cloacae 61.0%, n = 47 vs. K. aerogenes 65.5%, n = 19) (Table 1).
The primary composite outcome was less frequent in K. aerogenes group (K. pneumoniae 19.0%, n = 64 vs. E. cloacae 20.8%, n = 16 vs. K. aerogenes 6.9%, n = 2) reflecting the findings of all-cause mortality (K. pneumoniae 18.4%, n = 62 vs. E. cloacae 19.5%, n = 15 vs. K. aerogenes 6.9%, n = 2) and BSI recurrence (K. pneumoniae 4.5%, n = 15 vs. E. cloacae 10.4%, n = 8 vs. K. aerogenes 0%, n = 0). Persistent BSI was also less frequent in K. aerogenes group, while other secondary outcomes were more common (Table 1).
Variables with more than 10% of missing data were ESBL production (26.4%, n = 117), carbapenemase production (33.2%, n = 147), active empiric antibiotic therapy (12.9%, n = 57) and time to start antibiotic (11.1%, n = 49) (Additional file 1: Table S1). Missing data were similar between groups, except in active empiric antibiotic therapy, in which the proportion of missing data was higher in the E. cloacae group (Table 1).
Survival analysis
In total, 436 episodes were included in the survival analysis, corresponding to 75 events for a total time at risk of 9360 days (8 events per 1000 person-days). Seven BSI episodes (six K. pneumoniae and one E. cloacae) were excluded due to death at day 0.
The Kaplan–Meier curve shows a similar survival in E. cloacae and K. pneumoniae groups until day 17 (around 87.5% survival). After day 17 the survival for E. cloacae group is slightly lower than in K. pneumoniae group, reaching around 75% in both groups at day 30. The K. aerogenes survival curve is difficult to interpret because only two events occurred in the early follow-up period (Fig. 1). There was no evidence of difference between groups in the log-rank test (p-value 0.337).
Univariate analysis
Patients with K. aerogenes BSI were 58% and 65% less likely to die or have recurrence, when compared with K. pneumoniae (rate ratio (RR) 0.42; 95% CI 0.10 to 1.71) and E. cloacae (RR 0.35; 95% CI 0.08 to 1.55), respectively, without statistical evidence for an association between microorganisms and outcome (p-value 0.379) (Table 2). Individuals with E. cloacae BSI were 18% more likely of having the outcome of interest (RR 1.18; 95% CI 0.67 to 2.10), when compared to K. pneumoniae group, without statistical evidence of an association (p-value 0.379) (Table 2).
Men were 31% less likely to develop the composite outcome, when compared to women, without evidence of an association (RR 0.69; 95% CI 0.43 to 1.09; p-value 0.110) (Table 2). Compared to patients aged 18 to 59 years, individuals aged 70 to 79 years and over 80 years were 2.21 times (RR 2.21; 95% CI 1.12 to 4.36) and 2.14 times (RR 2.14; 95% CI 1.02 to 4.46) more likely to die or have recurrence, respectively, with evidence for this association (p-value 0.039) (Table 2).
There was evidence that participants with a Charlson comorbidity index ≥ 5 were 3.56 times more likely of dying or having recurrence, when compared to index < 5 (RR 3.56; 95% CI 2.11 to 6.01; p-value 0.001) (Table 2). Compared with individuals admitted to medical wards, patients in surgical departments were 47% less likely to die or recurrence (RR 0.53; 95% 0.27 to 1.06), without statistical evidence of an association (p-value 0.198) (Table 2). Individuals with catheter associated BSI were 49% less likely to have the composite outcome (RR 0.51; 95% CI 0.19 to 1.38), while respiratory tract were 35% more likely (RR 1.35; 95% CI 0.56 to 3.24), when compared to abdominal source, without statistical evidence of an association (p-value 0.598) (Table 2). There was no association between active empiric antibiotic and the outcome under study (RR 0.94; 95% CI 0.49 to 1.81, p-value 0.863) (Table 2).
Multivariate analysis
In the adjusted analysis the association between microorganisms and clinical outcome was slightly decreased towards the null, when compared to the crude analysis. Individuals with K. aerogenes were 56% and 52% less likely to die or having recurrence, when compared to K. pneumoniae (RR 0.44; 95% CI 0.11 to 1.84; p-value 0.262) and E. cloacae (RR 0.48; 95% CI 0.10 to 2.30; p-value 0.361), respectively, without statistical evidence of an association (Table 3).
Men were 24% less likely to develop the composite outcome, when compared to women (RR 0.76; 95% CI 0.44 to 1.31; p-value 0.330) (Table 3). Compared to the age group 18 to 59 years, individuals between 60 to 69 years were 27% less likely to die or have recurrence (RR 0.73; 95% CI 0.30 to 1.78; p-value 0.483), while individuals between 70 to 79 years old were 32% more likely (RR 1.32; 95% CI 0.59 to 2.93; p-value 0.499) (Table 3).
Charlson comorbidity index equal or above 5 was associated with a 3.87-fold increase in the risk of death or recurrence, when compared to patients with a lower index (RR 3.87; 95% CI 1.94 to 7.69; p < 0.001) (Table 3). Patients admitted to surgical had 34% less risk of worse outcome, when compared to individuals in the medical ward (RR 0.66; 95% CI 0.29 to 1.52; p-value 0.331) (Table 3). The risk of death or recurrence was 39% higher in BSI secondary to respiratory tract infection, when compared to abdominal source (RR 1.39; 95% CI 0.50 to 3.82; p-value 0.527) (Table 3). Patients treated with active empiric therapy seems to have a lower risk of death or recurrence, without statistical evidence of an association (RR 0.84; 95% CI 0.41 to 1.72; p-value 0.634) (Table 3).
Discussion
In this cohort study, individuals with K. aerogenes BSI were 58% and 65% less likely to die or have recurrence, when compared to K. pneumoniae and E. cloacae, respectively, although there was no evidence for an association. After adjusting for possible confounders, the rate ratio decreased towards the null effect. Despite the structural and genetic similarities between K. aerogenes and K. pneumoniae, this study demonstrates that K. aerogenes infection might have better outcomes.
In the survival analysis E. cloacae and K. pneumoniae groups have similar survival proportion. In fact, in the univariate analysis, the difference between these pathogens was very small; patients with E. cloacae BSI were 18% more likely of dying or having recurrence, when compared to K. pneumoniae group, without statistical evidence of an association. In our study, patients with E. cloacae BSI had more frequent nosocomial infections and catheter-associated BSI, when compared to other groups, which might be indicators of worse prognosis in these patients.
Previous studies have found a trend in the opposite direction, with higher mortality in K. aerogenes when compared to E. cloacae BSI, without statistical evidence of difference between groups. [37, 40] A multicentre case–control study conducted in five Spanish hospitals have assessed all-cause mortality at 30-day follow-up in cases with K. aerogenes or E. cloacae BSI with a control group of individuals without BSI matched by age, sex, and hospital area. [37] The authors reported no difference in 30-day mortality between these two pathogens and E. cloacae and K. aerogenes groups were similar in terms of place of acquisition, BSI source, severity, and antibiotic resistance. [37] The higher mortality in this study can be due to higher proportion of nosocomial K. aerogenes infections. [37] A single centre cohort study in the USA compared in-hospital all-cause mortality in patients with K. aerogenes and E. cloacae BSI. [40] When assessing a composite outcome of death before discharge, recurrence and/or complications, K. aerogenes group had a worse clinical outcome, when compared to E. cloacae [40]. The worst clinical outcome in the K. aerogenes group can be due to higher proportion of acute kidney injury in these patients, an outcome that was not included in the PRO-BAC analysis [40]. Proportion of recurrence was very low in both groups, when compared to PRO-BAC results [40]. The single centre design and the long period of enrolment can justify this difference, for example through spread of more virulent clones in the USA centre, differences in healthcare services through time or higher severity of patients admitted to this institution. This study also has the limitations of not considering the differences in length of hospital stay and it is not clear if these events have occurred before or after 30-days follow-up. An older cohort study from 2010, compared mortality in individuals admitted to a single centre in Seoul with K. aerogenes and E. cloacae BSI [39]. In this Korean study, there was statistical evidence of a higher mortality in the K. aerogenes group at 7-, 14- and 21-days follow-up [39]. Even though the proportion of septic shock is similar in both studies, the differences in results can be due to a higher proportion of ESBL production and nosocomial infections in the K. aerogenes group in the Korean study, when compared to PRO-BAC dataset [39]. The single centre design is a limitation of this study that could have influenced the higher proportion of ESBL-producing bacteria and nosocomial infections, more common in centres with inefficient infection prevention and control measures [43, 44]. Additionally, the analysis was not adjusted for confounding and K. aerogenes group was more frequently treated with inappropriate therapy, which could have biased the results [39].
On the other hand, findings from a more recent Korean case–control study are similar to the PRO-BAC analysis; there was statistical evidence of a higher mortality in E. cloacae group, when compared to K. aerogenes in the propensity score matched analysis [38]. Compared to PRO-BAC cohort, patients in Korean study have more frequent healthcare-associated infections and resistance to 3rd generation cephalosporins, while a higher proportion was treated with appropriate empiric therapy [38]. Even though the single centre design could be a limitation to results generalizability, the propensity score matched analysis reduces bias due to confounding. We didn’t find any study comparing clinical outcomes in K. aerogenes with K. pneumoniae BSI.
Our study uses a composite outcome that includes mortality or BSI recurrence at 30-day follow-up which may be consider an advantage, allowing to reflect a wider spectrum of clinical outcomes and increase the statistical study power, by allowing a higher number of outcome events per exposure group [45, 46]. The use of conceptual framework to decide which potential confounders should be included in the adjusted analysis improved the reliability of results, by avoiding over adjusting, increases the transparency of the analysis and supports the interpretation of the study results [47, 48].
The main limitation of our study is the small sample size and the low number of events in the three pathogens groups (particularly in the K. aerogenes group). The outcome assessment was done by review of medical records and national death registry, so we don’t expect that misclassification of the outcome have been an important cause of bias. Additionally, seven observations were excluded from the analysis, due to death at day 0, which could represent severe ill patients infected by a more virulent pathogen. However, most of them were infected by K. pneumoniae, which might have biased the results towards the null. Another relevant weakness was the exclusion of a high number of BSI episodes that didn’t have the date of entry or exit in the study. When comparing patients included and excluded from the analysis, the groups are very similar, only different in terms of antibiotic resistance and comorbidities (Additional file 1: Table S1). The impact of these differences is difficult to predict; patients excluded could be less severe due to lower proportion of comorbidities or more severe due to higher presence of carbapenemase.
Reporting the results using rate per 1000 person-days provides an adjusted analysis for the time at risk. The fact that the analysis didn’t take into consideration the possibility of competing events probably hasn’t affected the results because the overall mortality in PRO-BAC dataset is lower than in previous studies.
Due to small sample size this study results might not be generalizable. Nevertheless, the high proportion of death and recurrence in general in K. aerogenes, E. cloacae and K. pneumoniae BSI, should raising awareness about the burden of these pathogens and the importance of appropriate therapy. The study findings stress the need to develop and implement rapid diagnostic tools in BSI, which could help in early prescription of appropriate target therapy. Other strategies, for example, antimicrobial stewardship programs, can also be important to support clinicians when deciding empirical therapy, taking into consideration local epidemiological data.
Conclusions
This study suggests that BSI caused by K. aerogenes may have a better prognosis than E. cloacae or K. pneumonia; and that E. cloacae BSI may have a similar prognosis as K. pneumoniae.
New studies with bigger sample size and focused on other populations (e.g., paediatrics) will be useful to clarify the contradictory findings described in literature. It would be interesting to have more studies using composite outcomes, since they represent a wider variety of possible outcomes, reflecting the natural history of this disease.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMS/IPC:
-
Antimicrobial stewardship and infection prevention and control
- ATB:
-
Antibiotic
- BSI:
-
Bloodstream infection
- CI:
-
Confidence interval
- DAG:
-
Directed acyclic diagram
- ESBL:
-
Extended spectrum beta-lactamase
- HAI:
-
Healthcare-associated infection
- ICU:
-
Intensive care unit
- KPC:
-
Klebsiella pneumoniae carbapenemase
- MDR:
-
Multidrug resistance
References
Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–9.
Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399(10325):629–55.
Digiovine B, Chenoweth C, Watts C, Higgins M. The attributable mortality and costs of primary nosocomial bloodstream infections in the intensive care unit. Am J Respir Crit Care Med. 1999;160(3):976–81.
Riu M, Chiarello P, Terradas R, Sala M, Garcia-Alzorriz E, Castells X, et al. Cost attributable to nosocomial bacteremia: analysis according to microorganism and antimicrobial sensitivity in a University Hospital in Barcelona. PLoS ONE. 2016;11(4): e0153076.
Albrecht SJ, Fishman NO, Kitchen J, Nachamkin I, Bilker WB, Hoegg C, et al. Reemergence of gram-negative health care-associated bloodstream infections. Arch Intern Med. 2006;166(12):1289–94.
Diekema DJ, Hsueh PR, Mendes RE, Pfaller MA, Rolston KV, Sader HS, et al. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother. 2019;63(7):e00355-e419.
Lai CC, Chen YH, Lin SH, Chung KP, Sheng WH, Ko WC, et al. Changing aetiology of healthcare-associated bloodstream infections at three medical centres in Taiwan, 2000–2011. Epidemiol Infect. 2014;142(10):2180–5.
Pfaller MA, Jones RN, Doern GV, Kugler K, Group TSP. Bacterial pathogens isolated from patients with bloodstream infection: frequencies of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob Agents Chemother. 1998;42(7):1762–70.
Pien BC, Sundaram P, Raoof N, Costa SF, Mirrett S, Woods CW, et al. The clinical and prognostic importance of positive blood cultures in adults. Am J Med. 2010;123(9):819–28.
Rodríguez-Créixems M, Alcalá L, Muñoz P, Cercenado E, Vicente T, Bouza E. Bloodstream infections: evolution and trends in the microbiology workload, incidence, and etiology, 1985–2006. Medicine. 2008;87(4):234.
Uslan DZ, Crane SJ, Steckelberg JM, Cockerill FR, St. Sauver JL, Wilson WR, et al. Age- and sex-associated trends in bloodstream infection: a population-based study in Olmsted county, Minnesota. Arch Int Med. 2007;167(8):834–9.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39(3):309–17.
Yinnon AM, Butnaru A, Raveh D, Jerassy Z, Rudensky B. Klebsiella bacteraemia: community versus nosocomial infection. QJM. 1996;89(12):933–41.
Aydin M, Ergonul O, Azap A, Bilgin H, Aydin G, Cavus SA, et al. Rapid emergence of colistin resistance and its impact on fatality among healthcare-associated infections. J Hosp Infect. 2018;98(3):260–3.
Kang CI, Kim SH, Bang JW, Kim HB, Kim NJ, Kim EC, et al. Community-acquired versus nosocomial Klebsiella pneumoniae bacteremia: clinical features, treatment outcomes, and clinical implication of antimicrobial resistance. J Korean Med Sci. 2006;21(5):816–22.
Meatherall BL, Gregson D, Ross T, Pitout JDD, Laupland KB. Incidence, risk factors, and outcomes of Klebsiella pneumoniae bacteremia. Am J Med. 2009;122(9):866–73.
Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E, et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56(4):2108–13.
Tsay RW, Siu LK, Fung CP, Chang FY. Characteristics of bacteremia between community-acquired and nosocomial Klebsiella pneumoniae infection: risk factor for mortality and the impact of capsular serotypes as a herald for community-acquired infection. Arch Intern Med. 2002;162(9):1021–7.
Xu L, Sun X, Ma X. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob. 2017;29(16):18.
Zarkotou O, Pournaras S, Tselioti P, Dragoumanos V, Pitiriga V, Ranellou K, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17(12):1798–803.
Chow JW, Fine MJ, Shlaes DM, Quinn JP, Hooper DC, Johnson MP, et al. Enterobacter bacteremia: clinical features and emergence of antibiotic resistance during therapy. Ann Intern Med. 1991;115(8):585–90.
Lee CC, Lee NY, Yan JJ, Lee HC, Chen PL, Chang CM, et al. Bacteremia due to extended-spectrum-β-lactamase-producing enterobacter cloacae: role of carbapenem therapy. Antimicrob Agents Chemother. 2010;54(9):3551–6.
Liu C, Wang N, Lee C, Weng L, Tseng H, Liu C, et al. Nosocomial and community-acquired Enterobacter cloacae bloodstream infection: risk factors for and prevalence of SHV-12 in multiresistant isolates in a medical centre. J Hosp Infect. 2004;58(1):63–77.
Siedner M, Galar A, Guzman-Suarez B, Kubiak D, Baghdady N, Ferraro M, et al. Cefepime vs other antibacterial agents for the treatment of Enterobacter species bacteremia. Clin Infect Dis. 2014;58(11):1554–63.
Harris P, Peri A, Pelecanos A, Hughes C, Paterson D, Ferguson J. Risk factors for relapse or persistence of bacteraemia caused by Enterobacter spp.: a case-control study. Antimicrob Resist Infect Control. 2017;6:1–8.
Qureshi ZA, Paterson DL, Pakstis DL, Adams-Haduch JM, Sandkovsky G, Sordillo E, et al. Risk factors and outcome of extended-spectrum β-lactamase-producing Enterobacter cloacae bloodstream infections. Int J Antimicrob Agents. 2011;37(1):26–32.
Chang EP, Chiang DH, Lin ML, Chen TL, Wang FD, Liu CY. Clinical characteristics and predictors of mortality in patients with Enterobacter aerogenes bacteremia. J Microbiol Immunol Infect. 2009;42(4):329–35.
Bascomb S, Lapage SP, Willcox WR, Curtis MA. Numerical classification of the tribe Klebsielleae. Microbiology. 1971;66(3):279–95.
Chavda KD, Chen L, Fouts DE, Sutton G, Brinkac L, Jenkins SG, et al. Comprehensive genome analysis of carbapenemase-producing Enterobacter spp.: new insights into phylogeny, population structure, and resistance mechanisms. mBio. 2016;7(6):e02093-16.
Diene SM, Merhej V, Henry M, El Filali A, Roux V, Robert C, et al. The rhizome of the multidrug-resistant Enterobacter aerogenes genome reveals how new ‘killer bugs’ are created because of a sympatric lifestyle. Mol Biol Evol. 2013;30(2):369–83.
Izard D, Gavini F, Trinel PA, Krubwa F, Leclerc H. Contribution of DNA–DNA hybridization to the transfer of Enterobacter aerogenes to the Genus Klebsiella as K mobilis. Zentralblatt für Bakteriologie: I Abt Originale C: Allgemeine, angewandte und ökologische Mikrobiologie. 1980;1(3):257–63.
Davin-Regli A, Lavigne JP, Pagès JM. Enterobacter spp.: update on taxonomy, clinical aspects, and emerging antimicrobial resistance. Clin Microbiol Rev. 2019;32(4):e00002-19.
Tindall BJ, Sutton G, Garrity GM. Enterobacter aerogenes Hormaeche and Edwards 1960 (Approved Lists 1980) and Klebsiella mobilis Bascomb et al. 1971 (Approved Lists 1980) share the same nomenclatural type (ATCC 13048) on the Approved Lists and are homotypic synonyms, with consequences for the name Klebsiella mobilis Bascomb et al. 1971 (Approved Lists 1980). Int J Syst Evolut Microbiol. 2017;67(2):502–4.
Azevedo PAA, Furlan JPR, Oliveira-Silva M, Nakamura-Silva R, Gomes CN, Costa KRC, et al. Detection of virulence and β-lactamase encoding genes in Enterobacter aerogenes and Enterobacter cloacae clinical isolates from Brazil. Braz J Microbiol. 2018;49(Suppl 1):224–8.
Compain F, Babosan A, Brisse S, Genel N, Audo J, Ailloud F, et al. Multiplex PCR for detection of seven virulence factors and K1/K2 capsular serotypes of Klebsiella pneumoniae. J Clin Microbiol. 2014;52(12):4377–80.
El Fertas-Aissani R, Messai Y, Alouache S, Bakour R. Virulence profiles and antibiotic susceptibility patterns of Klebsiella pneumoniae strains isolated from different clinical specimens. Pathol Biol. 2013;61(5):209–16.
Álvarez-Marín R, Lepe JA, Gasch-Blasi O, Rodríguez-Martínez JM, Calvo-Montes J, Lara-Contreras R, et al. Clinical characteristics and outcome of bacteraemia caused by Enterobacter cloacae and Klebsiella aerogenes: more similarities than differences. J Glob Antimicrob Resist. 2021;25:351–8.
Jeon M, Huh K, Ko JH, Cho SY, Huh HJ, Lee NY, et al. Difference in the clinical outcome of bloodstream infections caused by Klebsiella aerogenes and Enterobacter cloacae complex. Open Forum Infect Dis. 2021;8(8): ofab390.
Song EH, Park KH, Jang EY, Lee EJ, Chong YP, Cho OH, et al. Comparison of the clinical and microbiologic characteristics of patients with Enterobacter cloacae and Enterobacter aerogenes bacteremia: a prospective observation study. Diagn Microbiol Infect Dis. 2010;66(4):436–40.
Wesevich A, Sutton G, Ruffin F, Park LP, Fouts DE, Fowler VG, et al. Newly named Klebsiella aerogenes (formerly Enterobacter aerogenes) is associated with poor clinical outcomes relative to other Enterobacter species in patients with bloodstream infection. J Clin Microbiol. 2020;58(9):e00582-e620.
Pérez-Crespo PMM, Lanz-García JF, Bravo-Ferrer J, Cantón-Bulnes ML, Sousa Domínguez A, Goikoetxea Aguirre J, et al. Revisiting the epidemiology of bloodstream infections and healthcare-associated episodes: results from a multicentre prospective cohort in Spain (PRO-BAC Study). Int J Antimicrob Agents. 2021;58(1):106352.
Mussa M, Martínez Pérez-Crespo PM, Lopez-Cortes LE, Retamar-Gentil P, Sousa-Dominguez A, Goikoetxea-Aguirre AJ, et al. Risk factors and predictive score for bacteremic biliary tract infections due to Enterococcus faecalis and Enterococcus faecium: a multicenter cohort study from the PROBAC project. Microbiol Spectr. 2022;10(4):e00051-e122.
Silva JT, Montoro J, Pérez-Jacoiste Asín MA, Fernández-Ruiz M, Polanco N, González E, et al. A joint program of antimicrobial stewardship and hospital-acquired infection control to reduce healthcare-associated infections after kidney transplantation: the Hipomenes study. Am J Transplant. 2023;S1600–6135(23):00581–6.
Bansal N, Goyal P, Basu D, Batra U, Sachdeva N, Joga S, et al. Impact of improving infection control and antibiotic stewardship practices on nosocomial infections and antimicrobial resistance in an oncology centre from India. Indian J Med Microbiol. 2023;45:100383.
Harris PNA, McNamara JF, Lye DC, Davis JS, Bernard L, Cheng AC, et al. Proposed primary endpoints for use in clinical trials that compare treatment options for bloodstream infection in adults: a consensus definition. Clin Microbiol Infect. 2017;23(8):533–41.
Timsit JF, de Kraker MEA, Sommer H, Weiss E, Bettiol E, Wolkewitz M, et al. Appropriate endpoints for evaluation of new antibiotic therapies for severe infections: a perspective from COMBACTE’s STAT-Net. Intensive Care Med. 2017;43(7):1002–12.
Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48.
Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224–7.
Acknowledgements
PROBAC/GEIRAS-SEIMC/SAMAMICEI project: Eva Leon (HU Virgen de Valme), Inés Pérez Camacho (Hospital General de Poniente), David Vinuesa García (HU Clínico San Cecilio), Jordi Cuquet Pedragosa (HU Granollers), Isabel María Reche Molina (HU Torrecárdenas), Alberto Bahamonde-Carrasco (Hospital de El Bierzo), Carmen Herrero Rodríguez (Complejo Hospitalario de Jaén), Marcos Guzmán García (HU Puerto Real), Antonio Sánchez-Porto (Hospital de la Línea de la Concepción), Alejandro Smithson Amat (Fundació Hospital de l’Esperit Sant), Esperanza Merino de Lucas (Hospital Universitario General de Alicante), Jesús Canueto Quintero (Hospital Punta de Europa).
The study has been presented as poster in ECCMID 2024.
Funding
The PRO-BAC project was financed by grants from Plan Nacional de I + D + i 2013–2016, Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Ciencia, Innovación y Universidades [PI16/01432] and the Spanish Network for Research in Infectious Diseases (REIPI) [RD16/0016/0001; RD16/0016/0008], co-financed by the European Development Regional Fund ‘A way to achieve Europe’, Operative program Intelligent Growth 2014–2020.
Author information
Authors and Affiliations
Consortia
Contributions
MG have contributed to the conception and design of the work, data analysis and interpretation, drafted the work and approved the submitted version. DG have contributed to the conception and design of the work, substantial revised the work and approved the submitted version. LELC have contributed to the data acquisition, substantial revised the work and approved the submitted version. JRB have contributed to the conception and design of the work, have substantial revised the work and approved the submitted version. ILH, PMMPC, MTPR, AS, AP, JMRI, LBP, BD, JSB, CAC, FGS, CNK, AJS, JGA, AAA, TMC, AAJ, JFS have contributed to the data acquisition and approved the submitted version. All authors agree to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according with the Declaration of Helsinki and national and institutional standards. PRO-BAC study was approved by the Spanish Medicines Agency and the Ethics Committee of the Hospital Universitario Virgen Macarena with waiver for informed consent (approval reference code: FIS-AMO-201601). Approval was also obtained at each participating centre. This secondary data analysis study was approved by London School of Hygiene and Tropical Medicine research Ethics Committee (approval reference code: 28651).
Consent for publication
Not applicable.
Competing interests
LELC has been scientific advisor for Angelini, speaker for Angelini, ViiV, Gilead and Correvio, and has served as trainer for ViiV. JRB. has received honoraria from Merck for accredited educational activities. The other authors report no conflicts of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Figure S1. Directed acyclic diagram of potential confounders, effect modifiers and other independent variables in the association between K. aerogenes, K. pneumoniae or E. cloacae BSI and clinical outcome (death or recurrence). Figure S2. Inclusion flow diagram for data analysis. Table S1. Characteristics of total sample, episodes included and excluded in analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guedes, M., Gathara, D., López-Hernández, I. et al. Differences in clinical outcomes of bloodstream infections caused by Klebsiella aerogenes, Klebsiella pneumoniae and Enterobacter cloacae: a multicentre cohort study. Ann Clin Microbiol Antimicrob 23, 42 (2024). https://doi.org/10.1186/s12941-024-00700-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-024-00700-8