Abstract
Background
The emergence of multidrug-resistant (MDR) strains of genital pathogens, notably Mycoplasma genitalium and Ureaplasma spp., constitutes a significant global threat today. The present study aimed to evaluate the prevalence and trend of changes in MDR mycoplasma and ureaplasma strains.
Methods
An exhaustive search was performed across the ISI Web of Science, PubMed, Scopus, ScienceDirect, and Google Scholar databases to accumulate relevant studies without restrictions until April 2023. We used event rate and corresponding 95% confidence intervals to determine the frequency of resistance-related mutations and examine the trend of antibiotic resistance changes.
Results
The data from 27 studies, including 24,662 patients across 14 countries, were evaluated. Out of the total studies, 20 focused on M. genitalium infections, and five on Ureaplasma spp. The frequency of resistance-associated mutations to macrolides, tetracyclines, and fluoroquinolones in clinical strains of M. genitalium was 43.5%, 13.1%, and 18.6%, respectively. The prevalence of M. genitalium strains with double resistance and MDR was 11.0% and 17.4%, respectively. The incidence of both double-drug-resistant and MDR strains was higher in the World Health Organization (WHO) Western Pacific Region than in European and American populations. For Ureaplasma strains, resistance-associated mutations to macrolides, tetracyclines, and fluoroquinolones were 40.8%, 25.7%, and 90.3%, respectively. The rate of antibiotic resistance was higher in the African population compared to the European and WHO Western Pacific Regions. The rate of MDR Ureaplasma infections was 13.2%, with a higher incidence in the African population compared to the WHO Western Pacific and European regions.
Conclusion
The proliferation and spread of MDR Mycoplasma and Ureaplasma strains present a significant public health challenge. The situation is indeed alarming, and the rising trend of MDR M. genitalium and MDR Ureaplasma infections suggests that therapies involving macrolides and fluoroquinolones may become less effective.
Similar content being viewed by others
Background
In response to the escalating issue of antibiotic resistance among infectious agents, a high-priority health crisis concern, the World Health Organization (WHO) recently initiated a project entitled “Global health sector strategies on HIV, viral hepatitis, and sexually transmitted infections (STIs) for the period 2022–2023” [1]. Especially troublesome are microorganisms like mycoplasmas and ureaplasmas, which are STIs associated with the Mollicutes class and the Mycoplasmataceae family. These pathogens quickly develop resistance to antimicrobial agents, propagating antibiotic resistance within their populations [2]. Mycoplasma genitalium was first isolated from the urethral swabs of two males exhibiting non-gonococcal urethritis (NGU) symptoms in 1980 [3]. Due to the bacterium’s fastidious nature and cultivation difficulties, its pathogenic role remained ambiguous for several years. Now, M. genitalium is recognized as a crucial sexually transmitted pathogen, infecting or colonizing over 3% of the global population [4]. This particular pathogen is associated with NGU in men and conditions such as endometritis, salpingitis, cervicitis, pelvic inflammatory disease, and preterm birth in women [5, 6].
Given M. genitalium’s lack of peptidoglycan in its cell wall, it exhibits resistance to β-lactam antibiotics. Antibiotics that disrupt protein synthesis and DNA synthesis inhibitors are the most effective treatment options currently available for M. genitalium infections [4]. Until early 2016, when the status of macrolide resistance was still undefined, the International Union against STI (IUSTI) European guidelines recommended doxycycline 100 mg twice daily or 200 mg once daily orally for seven days [7]. However, early randomized controlled clinical trials indicated that azithromycin was superior to doxycycline [8]. Consequently, most regional and international guidelines now consider azithromycin (as a one-time dose of 1 g) as the primary treatment for M. genitalium infections, and moxifloxacin (400 mg daily for seven days) as the secondary treatment [9]. Nonetheless, numerous studies reveal a rising resistance to macrolides and fluoroquinolones in M. genitalium isolates, with macrolide resistance exceeding 50% in some regions [10]. Fluoroquinolone resistance can reach 20% in the Asia-Pacific region, increasing treatment failure rates to more than 30% of cases [11,12,13,14,15]. The emergence of multidrug-resistant (MDR) M. genitalium strains and cases of co-infection with Chlamydia trachomatis further complicate treatment [4, 16].
Ureaplasmas, free-living pathogens like Ureaplasma parvum (UPA) and Ureaplasma urealyticum (UUA), invade the lower urogenital tract in approximately 20–29% of healthy women [17]. Infections with these agents increase the risk of adverse pregnancy outcomes such as miscarriage, stillbirth, chorioamnionitis, and preterm labor [18, 19]. Clinical samples from patients with urethritis, endometritis, chronic prostatitis, and bacterial vaginosis often isolate genital ureaplasmas. These infections elevate the risk of infertility in couples [20]. Moreover, these pathogens can cause severe illnesses in infants, including pneumonia, bacteremia, meningitis, and chronic lung disease [21]. Ureaplasmas, like mycoplasmas, lack a cell-wall structure, making β-lactam antibiotics and glycopeptides ineffective against these pathogens; unfortunately, these organisms are intrinsically resistant to lincosamides such as clindamycin [22]. Consequently, the treatment of Ureaplasma infections is restricted to bacteriostatic agents like protein synthesis inhibitors (e.g., tetracyclines and macrolides) and DNA replication inhibitors (e.g., fluoroquinolones). However, resistance to these antibiotics is rising due to the creation of single nucleotide polymorphisms (SNPs) and the spread of resistance genes [23, 24]. Although antibiotic resistance in ureaplasmas has been observed globally, the resistance burden varies geographically due to differences in antibiotic consumption and histories of previous antimicrobial exposure. However, data on the antibiotic resistance pattern of ureaplasmas remain sparse in many parts of the world, especially in economically disadvantaged nations. Developing appropriate treatment strategies necessitates understanding and evaluating current antibiotic resistance trends [25].
The decline in the efficacy of antibiotic regimens against mycoplasmas and ureaplasmas signifies an emerging public health crisis. Surveillance and analysis of resistance rates are critical steps towards optimizing guidelines for treating these infections effectively. In this study, we assess the rate and trend of dual resistance and MDR in mycoplasma and ureaplasma infections and measure primary treatment failure in cases of infection with these strains.
Methods
Throughout the course of this research, all the steps encompassing literature search in databases, selection criteria establishment, data extraction, and statistical analysis were rigorously conducted in line with the guidelines proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standard [26].
Literature search
A systematic search was executed across various databases such as ISI Web of Science, PubMed, Scopus, Science Direct, and Google Scholar to gather publications appraising the resistance of mycoplasmas and ureaplasmas to macrolides, tetracycline, and fluoroquinolones. Until April 2023, our search methodology utilized MeSH keywords such as “Mycoplasma”, “M. genitalium”, “M. pneumonia”, “M. hominis”, “M. salivarium”, “Ureaplasma”, “U. parvum”, “U. urealyticum”, “Drug resistant”, “Multi-drug resistant”, “MDR”, “Macrolides”, “Tetracyclines,“ and “Fluoroquinolones”. This phase was completed by two separate authors, disregarding language or publication date limitations. In order to ensure comprehensive coverage, we manually verified the bibliographies of the included studies to gather all pertinent articles.
Selection criteria
To examine studies that assessed multiple antibiotic resistances of mycoplasmas and ureaplasmas in clinical samples, two independent authors participated; disagreements were resolved through deliberation between these authors. All gathered papers were imported into Endnote software. The titles, abstracts, and full texts of all articles were scrutinized, and those meeting our pre-defined criteria were deemed eligible. Our inclusion criteria included: (1) Articles that evaluated antibiotic resistance mutations in clinical isolates of mycoplasmas and ureaplasmas, including 2058 and 2059 mutations in the 23 S rRNA, S83L, S83R, D87N, and D87Y mutations in parC, and all mutations in gyrA, gyrB, and parE genes, (2) Publications discussing antibiotic resistance in mycoplasmas and ureaplasmas, (3) Original studies adopting cross-sectional, case-control, and longitudinal designs, (4) Research articles based on human clinical samples containing clinical DNA samples and/or culture-based DNA samples, (5) Studies utilizing standard consensus microbiological methodologies. Conversely, in vitro or animal model publications, duplicate studies, articles with incomplete results, and non-original articles were excluded.
Quality assessment and data extraction
The Joanna Briggs Institute’s (JBI) critical appraisal checklist was employed to evaluate the quality of the studies. This checklist assesses indicators such as population size, research objectives, sample collection method, and statistical analysis approach, assigning scores to each element. Any study achieving at least six points was included in the analysis. As indicated in Table 1, data concerning the first author, study location, study year, gender distribution of patients, type of infections, patient symptoms, antibiotic resistance detection method, infection rate, resistance rate to macrolide, tetracycline, and fluoroquinolones, MDR rate, and primary treatment failure rate were extracted from eligible studies.
Statistical analysis
We utilized the Comprehensive Meta-Analysis (CMA) software version 2.2 (Biostat, Englewood, NJ, USA) to compile data and evaluate the global burden of MDR infections in mycoplasmas and ureaplasmas. Furthermore, the incidence of dual resistance to macrolides and fluoroquinolones in human infections was investigated. In cases of significant heterogeneity (I2 index greater than 50, Cochrane p-value greater than 0.05), a random-effects meta-analysis was employed to generate overall estimates. The data was further divided into subgroups according to WHO geographical regions, time periods (2003–2015, 2016–2019, 2020–2023), and men who have sex with men (MSM). Sensitivity analyses were performed using the leave-one-out approach to minimize heterogeneity. Primary treatment failure in MDR infections, along with instances of dual macrolide and fluoroquinolone resistance, were also evaluated. The funnel plot’s asymmetry was examined to assess potential publication bias.“
Results
Literature search and study characteristics
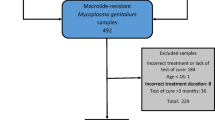
As illustrated in Fig. 1, a database search yielded 631 articles. Upon review of titles and abstracts, 456 studies were deemed irrelevant to our criteria and thus excluded. The full text of the remaining 79 articles was examined, and coupled with studies included from reference list reviews, a total of 27 studies were determined to be eligible for inclusion [20, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51].
Table 1 presents the salient features of these selected studies. A total of 27 studies involving 24,662 patients from 14 disparate countries were analyzed. Patients exhibiting symptoms such as NGU, cervicitis, pelvic inflammatory disease, chronic urogenital inflammatory diseases, invasive infections, and infertility, along with asymptomatic partners, were evaluated for mycoplasma and ureaplasma infections. Of the total participants, 86.94% were male, while the remaining 13.06% were female. Furthermore, four additional studies assessed M. genitalium infection and antibiotic resistance among HIV-positive MSM. Among the included studies, nine were conducted in European countries, three in the WHO Western Pacific region, and one each in the WHO Americas and African regions. Twenty investigations focused on M. genitalium infections, five on Ureaplasma spp., one on M. hominis, and one on M. salivarium.
To diagnose mycoplasma and ureaplasma infections, the studies employed various methods, including culture, serology, and molecular techniques. Antibiotic resistance in mycoplasmas and ureaplasmas was ascertained using broth microdilution, Sanger sequencing, Reverse transcription polymerase chain reaction (RT-PCR), real-time PCR, and real-time probe simultaneous amplification and testing. Potential sources of bias for the included studies could include lack of random selection, low and diverse population sizes in some studies, variety in clinical samples, and differences in methods used to diagnose mycoplasma and ureaplasma infections. Some studies also evaluated infections among stored banks of samples. Despite these potential biases, the infection rate for M. genitalium and Ureaplasma spp. in the included studies was estimated to be 21.0% (95% CI: 10-38.9) and 28.9% (95% CI: 13.0-52.4), respectively. Moreover, the rate of M. genitalium infection in MSM individuals was estimated to be around 11.5% (95% CI: 5.3–23.1).
Characteristics of mycoplasmas antibiotic resistance
We conducted a comprehensive analysis of data from 20 trials encompassing 9058 patients spanning 12 countries between the years 2013 and 2023. The prevalence of mutations linked to M. genitalium resistance to macrolides, tetracyclines, and fluoroquinolones was found to be 43.5% (95% CI: 33.1–54.5), 13.1% (95% CI: 3.8–36.8), and 18.6% (95% CI: 13.2–25.5), respectively, as demonstrated in Fig. 2.
The incidence of mutations linked to M. genitalium resistance to macrolides in European countries was 47.1% (95% CI: 32.7–61.9), 30.3% (95% CI: 17.2–47.6) in the WHO Western Pacific region, and 65.2% (95% CI: 58.3–71.5) in the WHO Americas region. Moreover, mutations associated with macrolide resistance were discerned in 70.9% of MSM individuals (95% CI: 66.2–75.1). The overall estimates corroborate both the regional and temporal trends. Our findings indicate that the prevalence of mutations tied to macrolide resistance has surged in recent years, manifesting in 25.6% (95% CI: 13.3–43.6) during 2003–2015, 41.5% (95% CI: 62.2–23.4) during 2016–2019, and 56.6% (95% CI: 43.5–68.9) during 2020–2023. During the subgroup analysis focused on mutations related to tetracycline resistance, the prevalence of mutations linked to M. genitalium resistance to tetracyclines in European regions and the WHO Western Pacific region was recorded as 6.8% (95% CI: 3.2–13.7) and 22.5% (95% CI: 15.4–31.7), respectively. Based on the statistical analysis, the prevalence of mutations associated with resistance was 13.1% (95% CI: 3.8–36.8) between 2020 and 2023. Unfortunately, due to data insufficiency, we were unable to discern trends in the mutations associated with tetracycline resistance in previous periods.
In terms of mutations connected with fluoroquinolone resistance, the prevalence in European countries, the WHO Western Pacific region, and the United States was 13.6% (95% CI: 8.3–21.3), 28.4% (95% CI: 16.9–43.7), and 19.0% (95% CI: 6.7–43.5), respectively. Globally, the trend of mutations associated with fluoroquinolone resistance decreased from 23.2% (95% CI: 11.2–42.0) in 2003–2015 to 17.6% (95% CI: 11.9–25.4) in 2016–2019, with 18.3% (95% CI: 7.6–37.7) remaining relatively stable until 2020–2023. M. salivarium antibiotic resistance mutations for macrolides, tetracyclines, and fluoroquinolones were reported to be 100%, 14.3%, and 25.7%, respectively. Recent observations of dual resistance to macrolides and fluoroquinolones in clinical isolates of M. genitalium have amplified concerns regarding treatment failure with both options. The incidence of mutations linked to resistance to two drugs in the WHO Western Pacific region was found to be about 14.6% (95% CI: 8.7–23.6), which exceeded that in European regions (10.0%; 95% CI: 4.7–20.0) and America (4.1; 95% CI: 0.4–32.3). According to our trend analysis, the frequency of resistance has tapered off in recent years, with a non-significant decline from 17.1% (95% CI: 10.1–27.4) in 2003–2015 to 7.2% (95% CI: 3.2–15.1) in 2016–2019, and 11.1% (95% CI: 4.1–26.7) in 2020–2023.
Regrettably, the prevalence of mutations linked to MDR M. genitalium strain infection escalated from 18.5% (95% CI: 10.9–29.6) in 2016–2019 to 32.6% (95% CI: 26.0–40.0) in 2020–2023, a trend that is disconcerting. The global rate of MDR M. genitalium infection was estimated to be 17.4% (95% CI: 9.2–30.5); the rate of MDR strain infection in the WHO Western Pacific region exceeded that in the European region (29.1% (95% CI: 10.7–58.4) vs. 12.2% (95% CI: 5.3–25.5), respectively). Sensitivity analyses, performed subsequent to the identification of the source of variability, revealed no significant changes in pooled values. For M. salivarium and M. hominis, the rates of infection with MDR strains were determined to be 14.3% and 33.78%, respectively. Unfortunately, only a single study evaluated the multiple resistances of these two pathogens, thereby precluding the calculation of the infection rate and trend.
Our findings highlighted that the prevalence of MDR M. genitalium in the MSM population was approximately 19.2% (95% CI: 8.7–37.2). Furthermore, the rate of primary treatment failure in MDR M. genitalium infections was measured at 12.8% (95% CI: 6.9–22.6). Thus, the rate of primary treatment failure in MDR M. genitalium isolates among WHO western Pacific patients was about 18.1% (95% CI: 7.1–38.9), consistent with the rate observed in the European population (13.2% (95% CI: 6.3–25.7)). Gratifyingly, the global trend of MDR M. genitalium infection between 2016 and 2019 was in the same range as 2020–2023 (19.7% (95% CI: 11.2–32.2) vs. 18.1 (95% CI: 13.3–24.2)).
Characteristics of ureaplasmas antibiotic resistance
This comprehensive quantitative analysis incorporates data from five articles, which include 7826 clinical samples sourced from four different countries, spanning the years 2003 to 2021. The pooled prevalence of mutations associated with resistance to three antibiotics—macrolides, tetracyclines, and fluoroquinolones—was calculated as 40.8% (95% CI: 23.6–60.7), 25.7% (95% CI: 15.4–39.6), and 90.3% (95% CI: 43.1–99.1), respectively (Fig. 3).
In the African region, the rate of mutations connected with macrolide resistance in clinical isolates of ureaplasmas was near total at 99.5% (95% CI: 92.6–100). Comparatively, in European countries and the WHO Western Pacific region, this rate was considerably lower at 30.8% (95% CI: 17.3–48.6) and 33.0% (95% CI: 24.5–42.7), respectively. Between 2020 and 2023, mutations associated with macrolide resistance were prevalent in 52.9% of cases (95% CI: 27.3–77.1). A notable rise in mutations tied to tetracycline resistance was observed in recent years, surging from 19.5% (95% CI: 12.9–28.4) in 2003 to 32.8% (95% CI: 18.5–51.1) in 2023. The rate of mutations resistant to this antibiotic was estimated at 31.6% (95% CI: 11.7–61.7) in Europe, 17.4% (95% CI: 11.2–26.1) in the WHO Western Pacific, and 37.6% (95% CI: 28.7–47.5) in African regions. The prevalence of fluoroquinolone resistance is particularly concerning. In Europe, this was measured at 96.4% (95% CI: 90.3–98.7), in the Western Pacific it was 89.9% (95% CI: 82.3–94.5), and in Africa, it reached 99.5% (95% CI: 92.6–100). In the period from 2020 to 2023, the resistance rate of ureaplasmas was 95.6% (95% CI: 85.8–98.8), suggesting that fluoroquinolones have become ineffective for treating human Ureaplasma infections worldwide. The data insufficiently cover temporal trends in other regions or time periods. Notwithstanding the substantial heterogeneity, sensitivity analyses indicated that summary values were stable.
The global rate of MDR Ureaplasma infection was assessed to be 13.2% (95% CI: 5.4–28.7). The prevalence of MDR Ureaplasma strains was approximately 9.4% (95% CI: 0.3–76.6) in WHO European regions, 4.9% (95% CI: 0.3–43.7) in the WHO Western Pacific regions, and 37.6% (95% CI: 28.7–47.5) in African regions. Alarmingly, the trend of MDR Ureaplasma infection has escalated sharply from 1.6% (95% CI: 0.3–7.2) in 2003–2015 to 28.6% (95% CI: 16.8–44.3), signaling a serious concern for health authorities. Regrettably, due to insufficient information, we could not calculate the rate of primary treatment failure among MDR Ureaplasma infections.
Publication bias
Our study’s funnel plots exhibited asymmetry in certain instances, suggesting a notable bias in some overall estimates. Nevertheless, the instances of significant asymmetry were assessed using the trim-and-fill method. This method, applied across all cases, revealed no substantial or meaningful alterations to the summary estimates (as depicted in Fig. 4).
Discussion
Presently, the ongoing emergence and steady proliferation of antibiotic resistance in bacterial agents implicated in both simple and complex forms of urogenital infections, notably mycoplasmas and ureaplasmas, has triggered a persistent decline in the efficacy of treatments for these infections, thereby posing a global challenge. This has been underscored by two extensive epidemiological studies that have sounded the alarm about the escalating prevalence of antibiotic resistance in M. genitalium, especially within European territories [52, 53].
Based on these studies, macrolide resistance in M. genitalium, with a particular focus on azithromycin resistance, is attributed to point mutations occurring in the V region of the 23s rRNA gene at positions 2058 and 2059, as per Escherichia coli numbering [54, 55]. Additionally, amino acid modifications in parC, namely S83L, S83R, D87N, or D87Y, are frequently correlated with failed ciprofloxacin therapy [32, 56]. Within the scope of this systematic review and meta-analysis, we examined the prevalence of antibiotic resistance mutations in clinical isolates of M. genitalium and ureaplasmas, making a novel contribution to the field by quantifying the MDR burden and tracking its geographical variations for the first time. As per our analysis, the collective prevalence of mutations associated with resistance to macrolides, tetracyclines, and fluoroquinolones was estimated at 43.5%, 13.1%, and 18.6% respectively. Our analysis of resistance to tetracyclines in M. genitalium is based on only two reports, which may not reflect the true prevalence and diversity of resistance mechanisms in such bacterium. Therefore, we caution that more studies are needed to confirm and expand our findings. Our scrutiny of the temporal trajectory of macrolide resistance revealed a marked surge in resistance, increasing from 25.6% in the period 2003–2015 to 56.6% in 2020–2023. Given that single-dose azithromycin has been commonly adopted as the primary treatment for STIs in various global regions since the early 1990s, it is anticipated that the escalating trend of mutations related to macrolide resistance in M. genitalium will precipitate a continual decline in the annual success rate of treatments [57,58,59]. Supporting this conjecture, a meta-analysis by Lau et al. found a steady rise over time in the treatment failure rates of M. genitalium infections administered with azithromycin, mirroring the trend identified in our analysis [60]. This annual increase in macrolide resistance can largely be attributed to the absence of drug sensitivity tests for M. genitalium, the implementation of inappropriate treatment protocols, and the dearth of large-scale surveillance to gauge the antibiotic resistance of M. genitalium.
Our study indicates that the prevalence of mutations linked to macrolide resistance is more pronounced in the American and European regions compared to the WHO Western Pacific region. The discrepancy in resistance levels across various geographical areas can primarily be traced back to the differences in antimicrobial usage, treatment guidelines, and the diversity of local antimicrobial stewardship programs implemented in these areas. For instance, doxycycline is typically designated as the frontline treatment in countries with low macrolide resistance, while azithromycin tends to be the first choice in nations that demonstrate substantial resistance to this class of antibiotics [33, 61]. Further analysis of our data revealed that the incidence of mutations related to macrolide resistance in clinical strains of M. genitalium isolated from MSM significantly surpasses that found in heterosexual men, at a rate of 70.9%. This upswing in macrolide resistance within this demographic can be ascribed to asymptomatic infections of this pathogen and the recurrent use of azithromycin to treat frequent instances of chlamydia and Neisseria gonorrhoeae infections [62]. This notion is substantiated by numerous studies conducted within the MSM community, which have identified a high prevalence of macrolide resistance in syphilis and gonorrhea infections [63, 64]. Interestingly, our results showed a higher rate of tetracycline resistance in the WHO Western Pacific countries than in European regions. Current research suggests that tetracycline is extensively utilized in Asian regions, resulting in a considerable resistance burden to tetracyclines in Southeast Asian territories [65, 66]. With significant Asian populations migrating to Australia and the WHO Western Pacific regions, the resistance burden in these areas is further exacerbated. Consequently, the emergence of tetracycline resistance should be anticipated in clinical isolates from the WHO Western Pacific region.
Our analysis demonstrates that the occurrence of mutations linked to fluoroquinolone resistance in M. genitalium samples from the WHO Western Pacific population is approximately twice to thrice the resistance burden found in European and American regions. This area also exhibits the highest rate of gonorrhea resistance to fluoroquinolones [67, 68]. Most of the studies incorporated in our analysis originated from Japan, where fluoroquinolones such as levofloxacin, gatifloxacin, and moxifloxacin are commonly employed in treating NGU and M. genitalium infections [32]. Also other studies demonstrated that sitafloxacin could be an alternative to moxifloxacin as an antimicrobial agent for a second-line treatment of M. genitalium infections unsuccessfully treated with azithromycin regimens [69, 70]. As a consequence, the frequency of mutations connected to fluoroquinolones is anticipated to be higher in the WHO Western Pacific region than in the European region.
Our study also discovered that the rate of fluoroquinolone-related mutations has remained relatively stable over the past 16 years, indicating no significant shifts in resistance. These findings align with those reported by Machalek and colleagues [15]. Additionally, our study shows a higher rate of dual resistance and MDR M. genitalium in the WHO Western Pacific populations compared to the WHO European populations. This rise in resistance mirrors the rate of antibiotic misuse, history of antimicrobial exposure, and treatment guidelines for STIs in the WHO Western Pacific region, particularly in Japan and China. It also contributes to an increase in MDR in clinical isolates of M. genitalium [4, 16]. It is intriguing to note that the rates of MDR M. genitalium are higher in the MSM community than in other patient demographics. We infer that MSM patients bear a higher MDR burden than heterosexual men, primarily due to the frequent exposure to azithromycin because of co-infection of M. genitalium with chlamydia or N. gonorrhea. Regrettably, the trend of MDR M. genitalium infection has been on the rise in recent years, and if the current scenario persists, the efficacy of these antibiotic classes in treating M. genitalium infection will be lost. Consequently, utilizing innovative technologies for simultaneous pathogen detection and resistance biomarker identification could lead to more precise resistance status evaluations and the selection of the most effective initial treatment for these infections [71, 72]. Also with considering only a single study, we concluded that the rate of infection with MDR M. hominis was determined to be 33.78%. in another study, midrange resistance rates for M. hominis to tetracycline, doxycycline and minocycline were 50.0%, 9.0% and 16.7%, respectively [73]. Because of the relationship of M. hominin with genital infections and the importance of the issue, more investigations must be conducted to determine antibiotic resistance status more precisely [74]. In our study, we have discerned that the prevalence of infection involving MDR M. salivarium stands at 14.3%. Despite the long-held assumption regarding the non-pathogenic nature of M. salivarium, it has been found that this bacterium is a common inhabitant of dental plaque and gingival sulci [75, 76]. Moreover, while extra-oropharyngeal infections involving M. salivarium are considered rare, M. salivarium has also been identified in infections at other body sites [77,78,79]. Despite these findings, the understanding of the antibiotic resistance characteristics of M. salivarium remains limited, with only a single study having evaluated its multidrug resistance profile to date. Therefore, there is a pressing need for additional research that focuses on exploring the antibiotic resistance of this bacterium.
Likewise, ureaplasma resistance has become widespread in many global regions due to the overuse of antibiotics and the implementation of empirical therapies without drug susceptibility testing [80]. Ureaplasma spp. are divided into 14 different serovars across two species, UUA and UPA. Current studies show that the trend towards increasing minimum inhibitory concentration (MIC) is greater in UUA than in UPA [81, 82]. According to our research, the rate of mutations connected to resistance to macrolides and fluoroquinolones was 52.8% (95% CI: 22.8–81.0) and 97.2% (95% CI: 92.8–98.9), respectively. However, the prevalence of resistance-related mutations in Ureaplasma spp. was 40.8% for macrolides, 25.7% for tetracyclines, and 90.3% for fluoroquinolones. Hence, our findings align with prior research demonstrating that the antibiotic resistance status in UUA is more severe than in other pathogens in this family (UPA) [83, 84]. Also, Ahmadi MH, operating a meta-analysis study, calculated the midrange resistance rates for UUA/UPA to tetracycline, doxycycline, and minocycline as 43.3%, 28.6%, and 9.0%, respectively. The related maximum resistance rates were 86.5, 57.1, and 16.2, respectively [73]. Our research revealed a high prevalence of macrolide resistance burden in clinical isolates of ureaplasmas isolated from African patients. Due to widespread antibiotic misuse in African populations and the absence of a comprehensive surveillance system to monitor antibiotic resistance status in this region, the antibiotic resistance status in these regions is typically more severe than in other parts of the world [85, 86].
According to our findings, the rate of mutations associated with tetracycline resistance in Ureaplasma spp. isolates from African regions was higher than in the WHO European and Western Pacific regions. Tetracyclines are commonly used as the first line of treatment for Ureaplasma infections in African regions, and thus it is logical to presume that the tetracycline resistance burden in these regions is higher than the global average [87]. Unfortunately, the number of mutations linked to tetracycline resistance has been steadily increasing, primarily due to empirical therapy without assessing the antibiotic resistance pattern of Ureaplasma spp. isolates.
Our analysis also revealed a high level of fluoroquinolone resistance across the globe, with the pooled prevalence of mutations linked to fluoroquinolone resistance in Europe, the WHO Western Pacific, and Africa being 96.4%, 89.9%, and 99.5%, respectively. The widespread use of fluoroquinolones to treat various infectious diseases can lead to high fluoroquinolone resistance [23]. MDR Ureaplasma infection was found in 13.2% of the population, and the prevalence of MDR Ureaplasma spp. strains in the African population is much higher than in the European and WHO Western Pacific populations. Prior research supports our findings, indicating that Ureaplasma antibiotic resistance is higher in developing countries than in developed ones [88]. Regrettably, the global trend of MDR Ureaplasma has risen from 1.6% to 2013 to 28.6% in 2023. The excessive use of antibiotics and a lack of local antimicrobial resistance surveillance contribute to an uncontrollable increase in antibiotic resistance.
As a result, the present study assists clinicians in refining treatment guidelines to circumvent and manage the emergence of antibiotic-resistant strains by illuminating the epidemiological traits of MDR M. genitalium and Ureaplasma strains. Despite this, our study has certain limitations; (1) Our investigation assessed the prevalence of antibiotic resistance mutations in samples from symptomatic patients, hence, our findings have implications for STI clinics, but cannot be generalized to the wider population, (2) Despite our utilization of a random-effects model, high heterogeneity was observed. Various factors such as clinical, methodological, and statistical can contribute to this heterogeneity in pooled estimates. Clinical heterogeneity can arise due to characteristics such as participant characteristics, socioeconomic status, body mass index, gender, age, symptoms, HIV status, infection site, and mutation identification methods. Statistical heterogeneity may lead to inconsistent results in subgroup analyses; sensitivity analysis might not significantly reduce the heterogeneity, (3) The WHO American and African regions have been underrepresented in the research, with no studies conducted in Southeast Asian or Eastern Mediterranean nations, (4) Our research only identified a few mutations for resistance to macrolides and fluoroquinolones, hence, we did not investigate mutations outside these regions associated with resistance and treatment failure, (5) Despite the inclusion of research focusing on various Mycoplasma species in our investigative analysis, only two studies pertaining to M. hominis and M. salivarium met the eligibility criteria. Consequently, to apply these findings more broadly to other Mycoplasma species, additional research must be conducted to validate and support these interpretations. Lastly, despite our re-evaluation and adjustment of the pooled estimates of bias instances using the trim-and-fill method, significant publication bias was observed in our selected research.
Conclusion
The increasing prevalence of antibiotic resistance in Mycoplasma and Ureaplasma infections is a significant yet underappreciated challenge; if unchecked, it may escalate into a global problem. Current treatment guidelines for Mycoplasma and Ureaplasma largely rely on anecdotal evidence rather than drug susceptibility testing. Our results underscore the need to reevaluate the use of empirical antibiotic therapy with single-dose azithromycin for the treatment of these infections. Minimizing the use of macrolides and fluoroquinolones, employing resistance-guided treatment guidelines, adopting combination therapy with new classes of antimicrobial agents, implementing simultaneous detection methods for infection and antibiotic resistance mutations, and carrying out epidemiological surveillance of antibiotic resistance can aid clinicians not only in effectively treating Mycoplasma and Ureaplasma treatment-resistant infections but also in mitigating the rise in antibiotic resistance.
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- M. genitalium :
-
Mycoplasma genitalium
- MDR:
-
Multidrug-resistant
- MSM:
-
Men who have sex with men
- WHO:
-
World Health Organization
- NGU:
-
Non-gonococcal urethritis
- UPA:
-
Ureaplasma parvum
- UUA:
-
Ureaplasma urealyticum
- SNPs:
-
Single nucleotide polymorphisms
- PRISMA:
-
Reporting Items for Systematic Reviews and Meta-Analyses
- JBI:
-
Joanna Briggs Institute’s
- CMA:
-
Comprehensive Meta-Analysis
- CI:
-
Confidence interval
References
Organization WH. Global health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022–2030. 2022.
Yang T, Pan L, Wu N, Wang L, Liu Z, Kong Y, Ruan Z, Xie X, Zhang J. Antimicrobial resistance in clinical Ureaplasma spp. and Mycoplasma hominis and structural mechanisms underlying quinolone resistance. Antimicrob Agents Chemother. 2020;64(6):e02560–02519.
Tully J, Cole R, Taylor-Robinson D, Rose D. A newly discovered mycoplasma in the human urogenital tract. The Lancet. 1981;317(8233):1288–91.
van der Schalk TE, Braam JF, Kusters JG. Molecular basis of antimicrobial resistance in Mycoplasma genitalium. Int J Antimicrob Agents. 2020;55(4):105911.
Lis R, Rowhani-Rahbar A, Manhart LE. Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis. Clin Infect Dis. 2015;61(3):418–26.
Taylor-Robinson D, Jensen JS. Mycoplasma genitalium: from Chrysalis to multicolored butterfly. Clin Microbiol Rev. 2011;24(3):498–514.
Horner PJ, Blee K, Falk L, van der Meijden W, Moi H. 2016 european guideline on the management of non-gonococcal urethritis. Int J STD AIDS. 2016;27(11):928–37.
Mena LA, Mroczkowski TF, Nsuami M, Martin DH. A randomized comparison of azithromycin and doxycycline for the treatment of Mycoplasma genitalium–positive urethritis in men. Clin Infect Dis. 2009;48(12):1649–54.
Jensen JS, Cusini M, Gomberg M, Moi H. 2016 european guideline on Mycoplasma genitalium infections. J Eur Acad Dermatol Venereol. 2016;30(10):1650–6.
Manhart LE, Jensen JS. Quinolone Resistance–Associated mutations in Mycoplasma genitalium: not ready for Prime Time. Sex Transm Dis. 2020;47(3):199.
Terada M, Ohki E, Yamagishi Y, Izumi K, Mikamo H. Antimicrobial efficacies of several antibiotics against uterine cervicitis caused by Mycoplasma genitalium. J Infect Chemother. 2012;18(3):313–7.
Couldwell DL, Tagg KA, Jeoffreys NJ, Gilbert GL. Failure of moxifloxacin treatment in Mycoplasma genitalium infections due to macrolide and fluoroquinolone resistance. Int J STD AIDS. 2013;24(10):822–8.
Bissessor M, Tabrizi SN, Twin J, Abdo H, Fairley CK, Chen MY, Vodstrcil LA, Jensen JS, Hocking JS, Garland SM. Macrolide resistance and azithromycin failure in a Mycoplasma genitalium–infected cohort and response of azithromycin failures to alternative antibiotic regimens. Clin Infect Dis. 2015;60(8):1228–36.
Bradshaw CS, Jensen JS, Waites KB. New horizons in Mycoplasma genitalium treatment. J Infect Dis. 2017;216(suppl2):412–S419.
Machalek DA, Tao Y, Shilling H, Jensen JS, Unemo M, Murray G, Chow EP, Low N, Garland SM, Vodstrcil LA. Prevalence of mutations associated with resistance to macrolides and fluoroquinolones in Mycoplasma genitalium: a systematic review and meta-analysis. Lancet Infect Dis. 2020;20(11):1302–14.
Braam J, van Dommelen L, Henquet C, van de Bovenkamp J, Kusters J. Multidrug-resistant Mycoplasma genitalium infections in Europe. Eur J Clin Microbiol Infect Dis. 2017;36:1565–7.
Paralanov V, Lu J, Duffy LB, Crabb DM, Shrivastava S, Methé BA, Inman J, Yooseph S, Xiao L, Cassell GH. Comparative genome analysis of 19 Ureaplasma urealyticum and Ureaplasma parvumstrains. BMC Microbiol. 2012;12(1):1–20.
Waites KB, Katz B, Schelonka RL. Mycoplasmas and ureaplasmas as neonatal pathogens. Clin Microbiol Rev. 2005;18(4):757–89.
Murtha AP, Edwards JM. The role of Mycoplasma and Ureaplasma in adverse pregnancy outcomes. Obstet Gynecol Clin. 2014;41(4):615–27.
Zhu X, Li M, Cao H, Yang X, Zhang C. Epidemiology of Ureaplasma urealyticum and Mycoplasma hominis in the semen of male outpatients with reproductive disorders. Experimental and Therapeutic Medicine. 2016;12(2):1165–70.
Waites KB, Schelonka RL, Xiao L, Grigsby PL, Novy MJ. Congenital and opportunistic infections: Ureaplasma species and Mycoplasma hominis. Seminars in fetal and neonatal medicine: 2009: Elsevier; 2009: 190–9.
Redelinghuys MJ, Ehlers MM, Dreyer AW, Lombaard HA, Kock MM. Antimicrobial susceptibility patterns of Ureaplasma species and Mycoplasma hominis in pregnant women. BMC Infect Dis. 2014;14:1–6.
Song T, Ye A, Xie X, Huang J, Ruan Z, Kong Y, Song J, Wang Y, Chen J, Zhang J. Epidemiological investigation and antimicrobial susceptibility analysis of ureaplasma species and Mycoplasma hominis in outpatients with genital manifestations. J Clin Pathol. 2014;67(9):817–20.
Dégrange S, Renaudin H, Charron A, Bébéar C, Bébéar C. Tetracycline resistance in Ureaplasma spp. and Mycoplasma hominis: prevalence in Bordeaux, France, from 1999 to 2002 and description of two tet (M)-positive isolates of M. hominis susceptible to tetracyclines. Antimicrob Agents Chemother. 2008;52(2):742–4.
Waites KB, Crabb DM, Bing X, Duffy LB. In vitro susceptibilities to and bactericidal activities of garenoxacin (BMS-284756) and other antimicrobial agents against human mycoplasmas and ureaplasmas. Antimicrob Agents Chemother. 2003;47(1):161–5.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W–65.
Li L, Yuan Y, He W, Zheng L, Wang Q. Emerging multidrug resistance contributes to treatment failure in Mycoplasma genitalium infected patients in China. Diagn Microbiol Infect Dis. 2023;105(2):115854.
Barberá M-J, Fernández-Huerta M, Jensen J-S, Caballero E, Andreu A. Mycoplasma genitalium Macrolide and Fluoroquinolone Resistance. Sex Transm Dis. 2017;44(8):457–62.
Xiao L, Geisler WM, Waites KB, Aaron KJ, Dionne-Odom JA. Lb3. 260 Multidrug resistant mycoplasma genitalium in hiv-infected men who have sex with men (MSM) in the united states. In.: BMJ Publishing Group Ltd; 2017.
Dumke R, Spornraft-Ragaller P. Antibiotic resistance and genotypes of Mycoplasma genitalium during a resistance-guided treatment regime in a german university hospital. Antibiotics. 2021;10(8):962.
Dionne-Odom J, Geisler WM, Aaron KJ, Waites KB, Westfall AO, Van Der Pol B, Xiao L. High prevalence of multidrug-resistant Mycoplasma genitalium in human immunodeficiency virus-infected men who have sex with men in Alabama. Clin Infect Dis. 2018;66(5):796–8.
Hamasuna R, Le PT, Kutsuna S, Furubayashi K, Matsumoto M, Ohmagari N, Fujimoto N, Matsumoto T, Jensen JS. Mutations in ParC and GyrA of moxifloxacin-resistant and susceptible Mycoplasma genitalium strains. PLoS ONE. 2018;13(6):e0198355.
Shipitsyna E, Rumyantseva T, Golparian D, Khayrullina G, Lagos AC, Edelstein I, Joers K, Jensen JS, Savicheva A, Rudneva N. Prevalence of macrolide and fluoroquinolone resistance-mediating mutations in Mycoplasma genitalium in five cities in Russia and Estonia. PLoS ONE. 2017;12(4):e0175763.
Mulligan V, Lynagh Y, Clarke S, Unemo M, Crowley B. Prevalence, macrolide resistance, and fluoroquinolone resistance in Mycoplasma genitalium in men who have sex with men attending an sexually transmitted disease clinic in Dublin, Ireland in 2017–2018. Sex Transm Dis. 2019;46(4):e35–7.
Xiao L, Waites KB, Van Der Pol B, Aaron KJ, Hook EW III, Geisler WM. Mycoplasma genitalium infections with macrolide and fluoroquinolone resistance-associated mutations in heterosexual african american couples in Alabama. Sex Transm Dis. 2019;46(1):18.
Boujemaa S, Mlik B, Ben Allaya A, Mardassi H, Ben Abdelmoumen Mardassi B. Spread of multidrug resistance among Ureaplasma serovars, Tunisia. Antimicrob Resist Infect Control. 2020;9:1–10.
Deguchi T, Kikuchi M, Yasuda M, Ito S. Multidrug-resistant Mycoplasma genitalium is increasing. Clin Infect Dis. 2016;62(3):405–6.
Braam JF, Zondag HC, van Dam AP, de Vries HJ, Vergunst C, Hetem D, van der Loeff MFS, Bruisten SM. Prevalence of fluoroquinolone resistance-associated mutations in Mycoplasma genitalium among clients of two sexual health centres in the Netherlands: a cross-sectional study. BMJ open. 2022;12(12):e066368.
Ma H, Zhang X, Shi X, Zhang J, Zhou Y. Phenotypic antimicrobial susceptibility and genotypic characterization of clinical ureaplasma isolates circulating in Shanghai, China. Front Microbiol. 2021;12:724935.
Gamova N. Drug sensitivity of Ureaplasma urealyticum, persisting in patients with chronic inflammatory diseases of the urogenital tract. Zh Mikrobiol Epidemiol Immunobiol 2003(4):81–5.
Xiao L, Totten AH, Crabb DM, Atkinson TP, Waites KB. Antimicrobial susceptibilities and mechanisms of resistance of commensal and invasive Mycoplasma salivarium isolates. Front Microbiol 2022:2677.
BIYIK İ, KESKİN N, GÜLCAN A, Onur İ, ERTEN Ö. Coinfection of Ureaplasma urealyticum/Mycoplasma hominis in HPV positive women: frequency, risk factors and multidrug resistance. J Clin Obstet Gynecol. 2020;30(3):92–9.
Pitt R, Fifer H, Woodford N, Alexander S. Detection of markers predictive of macrolide and fluoroquinolone resistance in Mycoplasma genitalium from patients attending sexual health services in England. Sex Transm Infect. 2018;94(1):9–13.
Deguchi T, Yasuda M, Horie K, Seike K, Kikuchi M, Mizutani K, Tsuchiya T, Yokoi S, Nakano M, Hoshina S. Drug resistance–associated mutations in Mycoplasma genitalium in female sex workers, Japan. Emerg Infect Dis. 2015;21(6):1062.
Le Roy C, Hénin N, Pereyre S, Bebear C. Fluoroquinolone-resistant Mycoplasma genitalium, southwestern France. Emerg Infect Dis. 2016;22(9):1677.
Murray GL, Bradshaw CS, Bissessor M, Danielewski J, Garland SM, Jensen JS, Fairley CK, Tabrizi SN. Increasing macrolide and fluoroquinolone resistance in Mycoplasma genitalium. Emerg Infect Dis. 2017;23(5):809.
De Baetselier I, Vuylsteke B, Reyniers T, Smet H, Van den Bossche D, Kenyon C, Crucitti T. Worryingly high prevalence of resistance-associated mutations to macrolides and fluoroquinolones in Mycoplasma genitalium among men who have sex with men with recurrent sexually transmitted infections. Int J STD AIDS. 2022;33(4):385–90.
Nijhuis R, Duinsbergen R, Pol A, Godschalk P. Prevalence of Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium and trichomonas vaginalis including relevant resistance-associated mutations in a single center in the Netherlands. Eur J Clin Microbiol Infect Dis. 2021;40:591–5.
Kikuchi M, Ito S, Yasuda M, Tsuchiya T, Hatazaki K, Takanashi M, Ezaki T, Deguchi T. Remarkable increase in fluoroquinolone-resistant Mycoplasma genitalium in Japan. J Antimicrob Chemother. 2014;69(9):2376–82.
Tagg KA, Jeoffreys NJ, Couldwell DL, Donald JA, Gilbert GL. Fluoroquinolone and macrolide resistance-associated mutations in Mycoplasma genitalium. J Clin Microbiol. 2013;51(7):2245–9.
Edelstein IA, Guschin AE, Romanov AV, Negasheva ES, Kozlov RS. Genetic determinants of Macrolide and Fluoroquinolone Resistance in Mycoplasma genitalium and their prevalence in Moscow, Russia. Pathogens. 2023;12(3):496.
Fernández-Huerta M, Barberá MJ, Serra-Pladevall J, Esperalba J, Martínez-Gómez X, Centeno C, Pich OQ, Pumarola T, Espasa M. Mycoplasma genitalium and antimicrobial resistance in Europe: a comprehensive review. Int J STD AIDS. 2020;31(3):190–7.
Cazanave C, Manhart L, Bébéar C. Mycoplasma genitalium, an emerging sexually transmitted pathogen. Médecine et maladies infectieuses. 2012;42(9):381–92.
Bébéar C, Pereyre S. Mechanisms of drug resistance in Mycoplasma pneumoniae. Curr Drug Targets-Infectious Disorders. 2005;5(3):263–71.
Jensen JS, Bradshaw CS, Tabrizi SN, Fairley CK, Hamasuna R. Azithromycin treatment failure in Mycoplasma genitalium–positive patients with nongonococcal urethritis is associated with induced macrolide resistance. Clin Infect Dis. 2008;47(12):1546–53.
Mondeja BA, Rodríguez NM, Barroto B, Blanco O, Jensen JS. Antimicrobial susceptibility patterns of recent cuban Mycoplasma genitalium isolates determined by a modified cell-culture-based method. PLoS ONE. 2016;11(9):e0162924.
Horner P, Ingle SM, Garrett F, Blee K, Kong F, Muir P, Moi H. Which azithromycin regimen should be used for treating Mycoplasma genitalium? A meta-analysis. Sex Transm Infect. 2018;94(1):14–20.
Sethi S, Zaman K, Jain N. Mycoplasma genitalium infections: current treatment options and resistance issues. Infect drug Resist 2017:283–92.
Nijhuis R, Severs T, Van der Vegt D, Van Zwet A, Kusters J. High levels of macrolide resistance-associated mutations in Mycoplasma genitalium warrant antibiotic susceptibility-guided treatment. J Antimicrob Chemother. 2015;70(9):2515–8.
Lau A, Bradshaw CS, Lewis D, Fairley CK, Chen MY, Kong FY, Hocking JS. The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis. 2015;61(9):1389–99.
Guschin A, Ryzhikh P, Rumyantseva T, Gomberg M, Unemo M. Treatment efficacy, treatment failures and selection of macrolide resistance in patients with high load of Mycoplasma genitalium during treatment of male urethritis with josamycin. BMC Infect Dis. 2015;15(1):1–7.
Read TR, Murray GL, Danielewski JA, Fairley CK, Doyle M, Worthington K, Su J, Mokany E, Tan L, Lee D. Symptoms, sites, and significance of Mycoplasma genitalium in men who have sex with men. Emerg Infect Dis. 2019;25(4):719.
Day MJ, Spiteri G, Jacobsson S, Woodford N, Amato-Gauci AJ, Cole MJ, Unemo M. Stably high azithromycin resistance and decreasing ceftriaxone susceptibility in Neisseria gonorrhoeae in 25 european countries, 2016. BMC Infect Dis. 2018;18(1):1–8.
Kenyon C. Prevalence of macrolide resistance in Treponema pallidum is associated with macrolide consumption. J Med Microbiol. 2019;68(2):119–23.
Boyanova L, Mitov I. Geographic map and evolution of primary Helicobacter pylori resistance to antibacterial agents. Expert Rev Anti-Infective Therapy. 2010;8(1):59–70.
Quaik S, Embrandiri A, Ravindran B, Hossain K, Al-Dhabi NA, Arasu MV, Ignacimuthu S, Ismail N. Veterinary antibiotics in animal manure and manure laden soil: scenario and challenges in asian countries. J King Saud University-Science. 2020;32(2):1300–5.
Wi T, Lahra MM, Ndowa F, Bala M, Dillon J-AR, Ramon-Pardo P, Eremin SR, Bolan G, Unemo M. Antimicrobial resistance in Neisseria gonorrhoeae: global surveillance and a call for international collaborative action. PLoS Med. 2017;14(7):e1002344.
Dalhoff A. Resistance surveillance studies: a multifaceted problem—the fluoroquinolone example. Infection. 2012;40:239–62.
Durukan D, Doyle M, Murray G, Bodiyabadu K, Vodstrcil L, Chow EP, Jensen JS, Fairley CK, Aguirre I, Bradshaw CS. Doxycycline and sitafloxacin combination therapy for treating highly resistant Mycoplasma genitalium. Emerg Infect Dis. 2020;26(8):1870.
Ito S, Yasuda M, Seike K, Sugawara T, Tsuchiya T, Yokoi S, Nakano M, Deguchi T. Clinical and microbiological outcomes in treatment of men with non-gonococcal urethritis with a 100-mg twice-daily dose regimen of sitafloxacin. J Infect Chemother. 2012;18(3):414–8.
Unemo M, Jensen JS. Antimicrobial-resistant sexually transmitted infections: gonorrhoea and Mycoplasma genitalium. Nat Reviews Urol. 2017;14(3):139–52.
Doyle M, Vodstrcil LA, Plummer EL, Aguirre I, Fairley CK, Bradshaw CS. Nonquinolone options for the treatment of Mycoplasma genitalium in the era of increased resistance. Open Forum Infectious Diseases: 2020: Oxford University Press US; 2020: ofaa291.
Ahmadi MH. Resistance to tetracyclines among clinical isolates of Mycoplasma hominis and Ureaplasma species: a systematic review and meta-analysis. J Antimicrob Chemother. 2021;76(4):865–75.
Horner P, Donders G, Cusini M, Gomberg M, Jensen J, Unemo M. Should we be testing for urogenital Mycoplasma hominis, Ureaplasma parvum and Ureaplasma urealyticum in men and women?–a position statement from the european STI Guidelines Editorial Board. J Eur Acad Dermatol Venereol. 2018;32(11):1845–51.
Lamster I, Grbic J, Bucklan R, Mitchell-Lewis D, Reynolds H, Zambon J. Epidemiology and diagnosis of HIV‐associated periodontal diseases. Oral Dis. 1997;3(S1):141–S148.
Mizuki H, Abe R, Kogi S, Mikami T. Immunohistochemical detection of Mycoplasma salivarium in oral lichen planus tissue. J Oral Pathol Med. 2017;46(8):649–56.
Büchsel M, Pletschen L, Fleiner M, Häcker G, Serr A. A case of septic arthritis caused by a Mycoplasma salivarium strain resistant towards ciprofloxacin and clarithromycin in a patient with chronic lymphatic leukemia. Diagn Microbiol Infect Dis. 2016;86(1):115–7.
Thoendel M, Jeraldo P, Greenwood-Quaintance KE, Chia N, Abdel MP, Steckelberg JM, Osmon DR, Patel R. A novel prosthetic joint infection pathogen, Mycoplasma salivarium, identified by metagenomic shotgun sequencing. Clin Infect Dis. 2017;65(2):332–5.
Totten AH, Xiao L, Crabb DM, Ratliff AE, Waites KB, Hwangpo T, Atkinson TP. Septic polyarthritis with Mycoplasma salivarium in a patient with common variable immunodeficiency: case report and review of the literature. Access Microbiol 2021, 3(4).
Beeton ML, Spiller OB. Antibiotic resistance among Ureaplasma spp. isolates: cause for concern? J Antimicrob Chemother 2016:dkw425.
Valentine-King MA, Brown MB. Antibacterial resistance in Ureaplasma species and Mycoplasma hominis isolates from urine cultures in college-aged females. Antimicrob Agents Chemother. 2017;61(10):e01104–01117.
Beeton ML, Chalker VJ, Jones LC, Maxwell NC, Spiller OB. Antibiotic resistance among clinical Ureaplasma isolates recovered from neonates in England and Wales between 2007 and 2013. Antimicrob Agents Chemother. 2016;60(1):52–6.
Zhang Y, Hua C, Li S. The relationship between the biovars and the antimicrobial resistance of Ureaplasma urealyticum in female patients with urogenital infections. J Clin Lab Anal. 2018;32(1):e22211.
Ye G, Jiang Z, Wang M, Huang J, Jin G, Lu S. The resistance analysis of Ureaplasma urealyticum and Mycoplasma hominis in female reproductive tract specimens. Cell Biochem Biophys. 2014;68:207–10.
Vlieghe E, Phoba M, Tamfun JM, Jacobs J. Antibiotic resistance among bacterial pathogens in Central Africa: a review of the published literature between 1955 and 2008. Int J Antimicrob Agents. 2009;34(4):295–303.
Wangai FK, Masika MM, Lule GN, Karari EM, Maritim MC, Jaoko WG, Museve B, Kuria A. Bridging antimicrobial resistance knowledge gaps: the east african perspective on a global problem. PLoS ONE. 2019;14(2):e0212131.
Mansour W. Tunisian antibiotic resistance problems: three contexts but one health. Afr Health Sci. 2018;18(4):1202–3.
O’CONNOR S, Rifkin D, Yang Y-H, Wang J-F, Levine OS, Dowell SF. Physician control of pediatric antimicrobial use in Beijing, China, and its rural environs. Pediatr Infect Dis J. 2001;20(7):679–84.
Acknowledgements
We appreciate from both Mashhad University of Medical Sciences and Iranshahr University of Medical Sciences.
Funding
We have not received any funding for this research.
Author information
Authors and Affiliations
Contributions
MA has contributed to design of the work and analysis of data. MA and MK have drafted the work and substantively revised it. MA and MK have reviewed and revised the draft manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable (this paper was provided based on researching in global databases).
Consent for publish
Not Applicable.
Competing interests
There is no any conflict of interest among the all authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abavisani, M., Keikha, M. Global analysis on the mutations associated with multidrug-resistant urogenital mycoplasmas and ureaplasmas infection: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob 22, 70 (2023). https://doi.org/10.1186/s12941-023-00627-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-023-00627-6