Abstract
Aztreonam-avibactam is an important option against Enterobacterales producing metallo-β-lactamases (MBLs). We obtained an aztreonam-avibactam-resistant mutant of an MBL-producing Enterobacter mori strain by induced mutagenesis. Genome sequencing revealed an Arg244Gly (Ambler position) substitution of SHV-12 β-lactamase in the mutant. Cloning and susceptibility testing verified that the SHV-12 Arg244Gly substitution led to significantly reduced susceptibility to aztreonam-avibactam (MIC, from 0.5/4 to 4/4 mg/L) but with the loss of resistance to cephalosporins as tradeoff. Arg244 of SHV involves in the binding of avibactam by forming an arginine-mediated salt bridge and is a critical residue to interact with β-lactams. Molecular modeling analysis demonstrated that the Arg244Gly substitution hindered the binding of avibactam to SHV with higher binding energy (from − 5.24 to -4.32 kcal/mol) and elevated inhibition constant Ki (from 143.96 to 677.37 µM) to indicate lower affinity. This substitution, however, resulted in loss of resistance to cephalosporins as tradeoff by impairing substrate binding. This represents a new aztreonam-avibactam resistance mechanism.
Similar content being viewed by others
Enterobacter, a genus of the family Enterobacteriaceae, is a group of important human pathogens [1]. Carbapenems are the major choices to treat severe infections caused by Enterobacter, but carbapenem-resistant Enterobacter has been increasingly reported [1]. Production of metallo-β-lactamases (MBLs) such as NDM, VIM, and IMP is a major mechanism mediating carbapenem resistance in Enterobacter [1]. Avibactam (AVI) is a non-β-lactam β-lactamase inhibitor able to inhibit serine-based β-lactamases but not MBLs [2], while aztreonam (ATM) is stable to the hydrolysis by MBLs [3, 4]. The combination of aztreonam-avibactam (ATM-AVI) has activity against Enterobacter isolates producing either serine-based β-lactamases or MBLs or both and has been used to treat carbapenem-resistant Enterobacter [5, 6]. However, ATM-AVI resistance has also emerged [7,8,9] but the mechanism for resistance remains largely unknown in Enterobacter. In this study, we report a novel mechanism mediating reduced susceptibility to ATM-AVI but with increased susceptibility to cephalosporins as tradeoff.
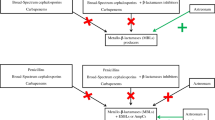
An ATM-AVI-resistant mutant was obtained from a carbapenem-resistant Enterobacter mori clinical strain
Carbapenem-resistant Enterobacter strain 020047 was recovered from urine of a patient in Sichuan, China, in 2016. Genome sequence of 020047 was obtained using a HiSeq X10 sequencer (Illumina, San Diego, CA). Strain 020047 was identified as Enterobacter mori based on the draft genome using FastANI v1.33 [10]. Antimicrobial resistance genes were identified using ResFinder (http://genomicepidemiology.org/). Strain 020047 has five β-lactamase-encoding genes, i.e., blaTEM−1B encoding a broad-spectrum β-lactamase, blaCTX−M−3 and blaSHV−12 encoding extended-spectrum β-lactamases (ESBLs), and two MBL-encoding genes blaIMP−4 and blaNDM−1. MIC of ATM-AVI was 1/4 mg/L (Table 1) as determined using broth microdilution according to the Clinical and Laboratory Standards Institute (CLSI) [11]. We conducted multi-step mutant selection experiments as described previously [12] to examine whether 020047 could develop resistance to ATM-AVI and if yes, to investigate the resistance mechanism. Briefly, 108 cfu of strain 020047 was inoculated in 2 mL LB broth (Sigma; St. Louis, MO) containing 0.5/4 mg/L ATM-AVI (0.5 × MIC) and 0.5 mg/L 5-azacytidine (Mce; Shanghai, China), an anticancer drug to increase the mutation rate of bacteria through inducing the SOS reaction [12]. After overnight culture, a 100-µl aliquot was streaked on a LB agar plate with doubled concentrations of ATM from 1 mg/L and fixed 4 mg/L AVI and 0.5 mg/L azacytidine and a colony was collected. The procedure from overnight culture was repeated in each day until ATM reached 16 mg/L as colonies grew in the presence of 8/4 mg/L ATM-AVI were obtained but no colonies could grow in ATM-AVI at 16 mg/L or higher concentrations. An ATM-AVI-resistant mutant, assigned 020047R here, was obtained from the LB agar plate containing 8/4 mg/L ATM-AVI. MIC of ATM-AVI for 020047R was 16/4 mg/L (Table 1) as determined using CLSI broth microdilution [11].
A nonsynonymous mutation was identified in bla SHV−12 in the ATM-AVI- resistant mutant
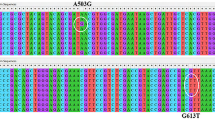
Like strain 020047, 020047R was also subjected to whole-genome sequencing using HiSeq X10. Reads were assembled using SPAdes v3.14.0 [13] and the genome sequence was annotated using Prokka v1.13 [14]. Single nucleotide polymorphisms (SNP) between 020047 and 020047R were called using Snippy v4.6.0 (https://github.com/tseemann/snippy) and were filtered to remove recombination using Gubbins v2.4.1 [15]. Compared to 020047, 020047R has five SNPs with three in non-coding regions. One SNP was present in a gene encoding a transposase of the Tn3 transposon family resulting in a Thr to Ala amino acid substitution. The remaining SNP occurred in blaSHV−12 (C715G, numbered from the ATG start codon) resulting in an Arg to Gly amino acid substitution at position 239 (Ambler position 244, Arg244Gly). By Blast, it becomes evident that among all reported naturally-occurring SHV β-lactamases the Arg244Gly substitution has not been found before. We then focused on the mutation of blaSHV−12 and performed cloning experiments.
The Arg244Gly mutation of bla SHV−12 mediates reduced susceptibility to ATM-AVI but with loss of resistance to cephalosporins as tradeoff
The − 10, and − 35 boxes within the promotor of blaSHV−12 were predicted using BPROM (http://www.softberry.com/berry.phtml?topic=bprom&group=programs&subgroup=gfindb). Together with the promoter sequence, blaSHV−12 in 020047 and its variant (assigned blaSHV−12R here) in 020047R were amplified with primers SHV-12-PROF (5’-AACCATATGATGATAAGTTTATCACCACCG, with restriction site is underlined) and SHV-12-PROR (5’-AACGAATTCAATACAATCAGGTGGCCAC) using PrimeSTAR Max DNA Polymerase (Takara; Dalian, China). Purified amplicons and the vector pET-28a(+) (Miaolingbio; Wuhan, China) were restricted by NdeI and EcoRI (Takara, Dalian, China), respectively, and were ligated using T4 ligase (Takara) to construct pET-SHV12 and pET-SHV12R. pET-SHV12 and pET-SHV12R were separately transformed into Escherichia coli DH5α using the chemical method [16]. Potential transformants were selected on LB agar plates containing 50 mg/L kanamycin. The presence of blaSHV−12 or blaSHV−12R in the corresponding transformant DH5::SHV-12 and DH5::SHV-12R was verified by PCR using Primers T7 (5’-TAATACGACTCACTATAGGG) and T7ter (5’-TGCTAGTTATTGCTCAGCGG) and subsequent Sanger sequencing.
MICs of cephalothin (CEP), cefuroxime (FUR), cefotaxime (CTX), piperacillin-tazobactam (PIP-TAZ), ceftazidime (CAZ), ceftazidime-avibactam (CAZ-AVI), ATM, ATM-AVI, ATM-clavulanic acid (ATM-CLA), ATM-sulbactam (ATM-SUL), ATM-tazobactam (ATM-TAZ), and imipenem (IMP) against strain 020047, 020047R, DH5::SHV-12 and DH5::SHV-12R were determined using the CLSI broth microdilution [11]. The breakpoints of ATM defined by CLSI were applied for ATM-AVI, ATM-CLA, ATM-SUL, and ATM-TAZ. MIC of ATM-AVI against DH5::SHV-12R was 4/4 mg/L, which was 8-fold higher than DH5::SHV-12 (0.5/4 mg/L, Table 1). However, compared to those against DH5::SHV-12, MICs of cephalosporins were 32- (FUR) to 512-fold (CEP) lower and that of ATM was 16-fold lower against DH5::SHV-12R (Table 1). The above findings suggest that the Arg244Gly substitution of SHV-12 mediates reduced susceptibility to ATM-AVI but leads to loss of resistance to cephalosporins as tradeoff.
The Arg244Gly substitution of SHV-12 altered the AVI binding pocket and impaired affinity for cephalosporins and ATM
The Arg244Gly substitution occurs in the region to form a β sheet but does not alter the predicted secondary structure of SHV-12 (Fig. 1). The enzyme conformation may change during the process of docking to ligand and there is no crystal structure of SHV-12 β-lactamase bound to AVI in the Protein Data Bank (PDB). The structure of SHV-12 and SHV-12R were predicted using the modelling tool SWISS-MODEL (https://swissmodel.expasy.org/interactive) based on the crystal structure of SHV-1 β-lactamase bound to AVI (PDB: 4ZAM) as template. The ligand, water molecules of SHV-12 and SHV-12R were removed using Pymol (Schrödinger, www.pymol.org). SHV-12 and SHV-12R were then prepared by adding hydrogen atoms with gasteiger charges by AutoDockTools of MGLTools 1.5.6 [17]. The structure of AVI (PubChem CID: 9,835,049) was obtained from the PubChem (https://pubchem.ncbi.nlm.nih.gov/). Ligands were regarded as flexible during docking in default settings using AutoDockTools. AutoGrid and genetic algorithm [18] were used to evaluate the binding energies and intermolecular forces. Grid box was set as 155 × 126 × 126 with a 0.375 Å grid point spacing and default docking parameters. Molecular docking of SHV-12 and AVI was modeled using AutoDock 4.2.6 [17]. The conformation of docking that contained part of known binding sites such as Ser70 [19] (see below) and had lower binding energy and lower inhibition constant Ki (lower Ki means higher affinity), which were determined using AutoDock 4.2.6, was selected. Docking structure was visualized using Pymol (www.pymol.org).
Secondary structure of SHV-12 and SHV-12R. The alignment of amino acid sequences and the prediction of secondary structures were performed using ENDscript 2 [30]. Secondary structure elements, α helixes, β sheets, and 310-helixes (representing by η), are indicated. β-strands are rendered as arrows, and strict β-turns are shown as TT letters
Ser70 (Ambler position, hereinafter) is the active site to hydrolyze β-lactams of SHV-1, SHV-12 and SHV-12R by querying the UniProt database (https://www.uniprot.org/). In previous structure studies [20, 21], Ser70 is covalently bonded to AVI and Arg244 in SHV-1 formed an arginine-mediated salt bridge interacting with the sulfate moiety of AVI. In addition, Arg244 and several other amino acids (Ser130, Asn132, Glu166, Thr167, Asn170, Thr235, and Ala237) of SHV-1 formed hydrogen bonds to AVI (Fig. 2 panel A). In strain 020047R, Arg244 substituted by a shorter Gly239 results in transformation of AVI binding (Fig. 2 panel B), hindering the binding of AVI to SHV-12R. Analysis of binding energy showed that the estimated binding energy increased from − 5.24 kcal/mol in SHV-12 to -4.32 kcal/mol in SHV-12R. The inhibition constant Ki also increased from 143.96 µM in SHV-12 to 677.37 µM in SHV-12R, suggesting lower affinity to AVI. In addition, the pocket accommodating AVI (Fig. 2 panel C) vanished from SHV-12R in the presence of the Arg244Gly substitution (Fig. 2 panel D).
Binding of AVI to SHV-12 and its variant SHV-12R. The residues interact with AVI are depicted in blue. The amino acid substitution is s depicted in purple and the rest of the protein is in green. Molecular docking of SHV-12 and AVI was modeled using AutoDock 4.2.6 [17]. Docking structure was visualized using Pymol (www.pymol.org). Panel A and C, hydrogen bonds of AVI to SHV-12. Ser70 is the active site to hydrolyze β-lactams. Arg244 and several other amino acids, e.g., Ser130, Asn132, and Thr235, formed hydrogen bonds (shown as a cyan region in panel C) to AVI. Panel B and D, hydrogen bonds of AVI to SHV-12R. The Arg244Gly substitution, indicated by an arrow in panel D, altered hydrogen bonds (shown as a cyan region in panel D) of AVI compared to that in SHV-12 (panel A)
Arg244 of class A β-lactamases including SHV enzymes has been well characterized and is a critical residue to interact with β-lactams and β-lactamase inhibitors, and is involved in recognition, positioning, and turnover of substrates in the active site [22,23,24,25]. It has been shown that various amino acid substitutions of Arg244 including Arg244Gly cause that SHV-1 loses the activity of cephalosporinases due to the impaired affinity and are unable to hydrolyze cephalosporins [23, 25]. The hydrolysis of ATM is also reduced but to a lesser extent in the presence of such substitutions of Arg244 [25]. Instead of a carboxylate group in cephalosporins, ATM has a sulfonic acid group bonded to the lactam ring and Arg244 has a weaker interaction with the sulfonic group than that with carboxylate [25]. Although the hydrolysis of ATM by SHV-12R was reduced, it did not completely compensate the effect of the decreased binding of AVI to inhibit the enzyme. As such, the susceptibility of ATM-AVI was significantly reduced for strains producing SHV-12R. By contrast, the reduced hydrolysis of cephalosporins could compensate impaired binding of AVI to make MICs of CAZ-AVI unaltered. However, it is worth to point out that CAZ-AVI alone has no activity against strain 020040 due to the production of MBLs.
Notably, amino acid substitutions of Arg244 have been well described in TEM β-lactamases including TEM-79 (an Arg244Gly variant of TEM-1) [26] and such substitutions lead to resistance to the inhibition of CLA [27, 28]. In the presence of 4 mg/L ATM, However, the activity of ATM-CLA against SHV-12R and SHV-12 was not significantly different (Table 1). Previous studies [23, 29] have found that different amino acid substitutions of Arg244 of SHV-1 obtained by mutagenesis exhibit varied and even contradictory impact on the inhibition of CLA. Particularly, the Arg244Gly substitution of SHV-1 did not significantly (less than four-fold) alter such inhibition [23, 29]. SHV-12R led to a four-fold lower MIC of ATM-SUL (32/4 mg/L) comparing with SHV-12 (Table 1) and this is consistent with the previous finding of 8-fold increased inhibition of SUL against SHV-1 with the Arg244Gly substitution [29]. The impact of Arg244Gly substitution of SHV β-lactamases on TAZ has not been evaluated before, but in this study SHV-12R led to a 64- or 128-fold lower MIC of ATM-TAZ and PIP-TAZ comparing with SHV-12 (Table 1). The above findings highlight that the impact of Arg244Gly substitution varies according to the β-lactamases (e.g., TEM or SHV) and the β-lactamase inhibitors (AVI, CLA, SUL, and TAZ).
We are aware of limitations of this study. First, multiple colonies grew on the agar plate containing 8/4 mg/L ATM-AVI and we only picked up a single colony as the representative for study. We also did not repeat the mutation experiments. We were therefore unable to uncover the presence of other potential mechanisms for mediating ATM-AVI resistance and to determine the reproducibility of the Arg244Gly substitution of SHV-12 to form SHV-12R. Second, we did not determine enzyme kinetics parameters for SHV-12R in comparison with SHV-12, which could provide complementary data to phenotypic, genetic and structural analyses.
Despite the limitations, we identified an amino acid substitution at Arg244 of SHV-12 leading to reduced susceptibility to ATM-AVI, a combination against MBL-producing Enterobacterales but with the expense of losing the ESBL phenotype against cephalosporins. This is the first time to the best of our knowledge that a mutation of blaSHV is associated with reduced susceptibility to ATM-AVI.
Data availability
The draft genome sequences of strain 020047 and 020047R have been deposited into GenBank under the accession no. JAJHUL000000000 and JAJHUM000000000, respectively.
References
Zong Z, Feng Y, McNally A. Carbapenem and colistin resistance in Enterobacter: determinants and clones. Trends Microbiol. 2021;29:473–6.
Livermore DM, Mushtaq S, Warner M, Zhang J, Maharjan S, Doumith M, Woodford N. Activities of NXL104 combinations with ceftazidime and aztreonam against carbapenemase-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2011;55:390–4.
Nordmann P, Poirel L, Walsh TR, Livermore DM. The emerging NDM carbapenemases. Trends Microbiol. 2011;19:588–95.
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. Characterization of a new metallo-β-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–54.
Cairns KA, Hall V, Martin GE, Griffin DWJ, Stewart JD, Khan SF, Abbott IJ, Meher-Homji Z, Morrissey CO, Sia C, et al. Treatment of invasive IMP-4 Enterobacter cloacae infection in transplant recipients using ceftazidime/avibactam with aztreonam: a case series and literature review. Transpl Infect Dis. 2021;23:e13510.
Yasmin M, Fouts DE, Jacobs MR, Haydar H, Marshall SH, White R, D’Souza R, Lodise TP, Rhoads DD, Hujer AM, et al. Monitoring ceftazidime-avibactam and aztreonam concentrations in the treatment of a bloodstream infection caused by a multidrug-resistant Enterobacter sp. carrying both Klebsiella pneumoniae carbapenemase-4 and New Delhi metallo-β-lactamase-1. Clin Infect Dis. 2020;71:1095–8.
Niu S, Wei J, Zou C, Chavda KD, Lv J, Zhang H, Du H, Tang YW, Pitout JDD, Bonomo RA, et al. In vitro selection of aztreonam/avibactam resistance in dual-carbapenemase-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2019;75:559–65.
Alm RA, Johnstone MR, Lahiri SD. Characterization of Escherichia coli NDM isolates with decreased susceptibility to aztreonam/avibactam: role of a novel insertion in PBP3. J Antimicrob Chemother. 2015;70:1420–8.
Russ D, Glaser F, Shaer Tamar E, Yelin I, Baym M, Kelsic ED, Zampaloni C, Haldimann A, Kishony R. Escape mutations circumvent a tradeoff between resistance to a β-lactam and resistance to a β-lactamase inhibitor. Nat Commun. 2020;11:2029.
Jain C, Rodriguez RL, Phillippy AM, Konstantinidis KT, Aluru S. High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat Commun. 2018;9:5114.
CLSI. Performance Standards for Antimicrobial susceptibility testing; thirtieth informational supplement. M100-S30. Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2020.
Hobson CA, Bonacorsi S, Jacquier H, Choudhury A, Magnan M, Cointe A, Bercot B, Tenaillon O, Birgy A. KPC β-lactamases are permissive to insertions and deletions conferring substrate spectrum modifications and resistance to ceftazidime-avibactam. Antimicrob Agents Chemother. 2020;64:e01175–01120.
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19:455–77.
Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–9.
Croucher NJ, Page AJ, Connor TR, Delaney AJ, Keane JA, Bentley SD, Parkhill J, Harris SR. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43:e15.
Sambrook J, Russell DW. Molecular Cloning. A laboratory manual. Volume 1. Cold Spring Harbour, NY: Cold Spring Harbour Laboratory Press; 2001.
Morris GM, Huey R, Lindstrom W, Sanner MF, Belew RK, Goodsell DS, Olson AJ. AutoDock4 and AutoDockTools4: automated docking with selective receptor flexibility. J Comput Chem. 2009;30:2785–91.
Morris GM, Goodsell DS, Halliday RS, Huey R, Hart WE, Belew RK, Olson AJ. Automated docking using a lamarckian genetic algorithm and an empirical binding free energy function. J Comput Biol. 1998;19:1639–62.
Huletsky A, Knox JR, Levesque RC. Role of Ser-238 and Lys-240 in the hydrolysis of third-generation cephalosporins by SHV-type β-lactamases probed by site-directed mutagenesis and three-dimensional modeling. J Biol Chem. 1993;268:3690–7.
Krishnan NP, Nguyen NQ, Papp-Wallace KM, Bonomo RA, van den Akker F. Inhibition of Klebsiella β-Lactamases (SHV-1 and KPC-2) by Avibactam: a structural study. PLoS ONE. 2015;10:e0136813.
Winkler ML, Papp-Wallace KM, Taracila MA, Bonomo RA. Avibactam and inhibitor-resistant SHV β-lactamases. Antimicrob Agents Chemother. 2015;59:3700–9.
Imtiaz U, Billings EM, Knox JR, Manavathu EK, Lerner SA, Mobashery S. Inactivation of class A β-lactamases by clavulanic acid: the role of arginine-244 in a proposed nonconcerted sequence of events. J Am Chem Soc. 1993;115:4435–42.
Thomson JM, Distler AM, Prati F, Bonomo RA. Probing active site chemistry in SHV β-lactamase variants at Ambler position 244. Understanding unique properties of inhibitor resistance. J Biol Chem. 2006;281:26734–44.
Zafaralla G, Manavathu EK, Lerner SA, Mobashery S. Elucidation of the role of arginine-244 in the turnover processes of class A β-lactamases. Biochemistry. 1992;31:3847–52.
Giakkoupi P, Tzelepi E, Legakis NJ, Tzouvelekis LS. Substitution of Arg-244 by cys or ser in SHV-1 and SHV-5 β-lactamases confers resistance to mechanism-based inhibitors and reduces catalytic efficiency of the enzymes. FEMS Microbiol Lett. 1998;160:49–54.
Leflon-Guibout V, Speldooren V, Heym B, Nicolas-Chanoine M. Epidemiological survey of amoxicillin-clavulanate resistance and corresponding molecular mechanisms in Escherichia coli isolates in France: new genetic features of blaTEM genes. Antimicrob Agents Chemother. 2000;44:2709–14.
Drawz SM, Bonomo RA. Three decades of β-lactamase inhibitors. Clin Microbiol Rev. 2010;23:160–201.
Delaire M, Labia R, Samama JP, Masson JM. Site-directed mutagenesis at the active site of Escherichia coli TEM-1 β-lactamase. Suicide inhibitor-resistant mutants reveal the role of arginine 244 and methionine 69 in catalysis. J Biol Chem. 1992;267:20600–6.
Thomson JM, Distler AM, Bonomo RA. Overcoming resistance to β-lactamase inhibitors: comparing sulbactam to novel inhibitors against clavulanate resistant SHV enzymes with substitutions at Ambler position 244. Biochemistry. 2007;46:11361–8.
Robert X, Gouet P. Deciphering key features in protein structures with the new ENDscript server. Nucleic Acids Res. 2014;42:W320–4.
Acknowledgements
Not applicable.
Funding
The relevant works of the authors were supported by the National Natural Science Foundation of China (82172309) and by grants from the West China Hospital of Sichuan University (1.3.5 project for disciplines of excellence, grant number ZYYC08006 and ZYGD22001).
Author information
Authors and Affiliations
Contributions
Z.Z. conceived and designed the study. S.W. and K.M. performed the experiments. S.W., Y.F., and Z.Z. analyzed the data. S.W. and Z.Z. wrote the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, S., Ma, K., Feng, Y. et al. Resistance to aztreonam-avibactam due to a mutation of SHV-12 in Enterobacter. Ann Clin Microbiol Antimicrob 22, 49 (2023). https://doi.org/10.1186/s12941-023-00605-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-023-00605-y