Abstract
Objectives
Among patients with haematological malignancy, bacteraemia is a common complication during chemotherapy-induced neutropenia. Resistance of gram-negative bacteria (GNB) to third-generation cephalosporins (3GC) is increasing. In order to explore the value of using surveillance cultures to guide empirical treatment e.g. choosing between carbapenem versus ceftazidime- we aimed to assess the distribution of pathogens causing bacteraemia in patients with haematological malignancy, and the proportion of 3GC-resistant GNB (3GC-R GNB) bacteraemia that was preceded by 3GC-R GNB colonization.
Methods
Using 11 years of data (2008–2018) from the Dutch national antimicrobial resistance surveillance system, we assessed the prevalence of 3GC-R GNB in episodes of bacteraemia, and the proportion of 3GC-R GNB bacteraemia that was preceded by 3GC-R GNB colonization. Colonization was defined as availability of any GNB surveillance isolate in the year before, independent of the causative micro-organism (time-paired isolates).
Results
We included 3887 patients, representing 4142 episodes of bacteraemia. GNB were identified in 715/4142 (17.3%), of which 221 (30.9%) were 3GC-R GNB. In 139 of these 221 patients a time-paired surveillance culture was available. In 76.2% (106/139) of patients these surveillance cultures already showed 3GC-R GNB isolates in the year prior to the culture date of the 3GC-R GNB positive blood isolate.
Conclusions
This multi-centre study shows that in patients with haematological malignancy, the majority of 3GC-R GNB bacteraemia is preceded by 3GC-R GNB colonization. Prospective clinical studies are needed to assess the safety and benefits of the use of surveillance-cultures to guide empirical therapy to restrict the empirical use of carbapenems in this population.
Similar content being viewed by others
Background
Fever frequently complicates chemotherapy-induced neutropenia in patients with haematological malignancy [1]. Half of febrile neutropenic (FN) episodes remain of unknown origin. In less than a quarter (20–23%) of FN episodes, blood cultures are positive for possible causative pathogens [2, 3]. Prompt initiation of antibiotics, with activity against important gram-negative bacteria (e.g. Pseudomonas aeruginosa), is critical in case of bloodstream infection [4,5,6,7,8]. An important source of bacteraemia in chemotherapy-induced FN is thought to be the gut [9]. Colonization with resistant bacteria is considered a major risk factor for bloodstream infection with resistant bacteria [10,11,12,13]. In Dutch hospitals treating high-risk neutropenic patients, surveillance cultures (e.g. on oral and rectal swabs) are performed to identify patients colonized with resistant microorganisms, and modify empirical antibiotic therapy accordingly. Apart from the Fourth European Conference on Infections in Leukaemia (ECIL-4) guideline, guidelines do not recommend to rely on surveillance cultures to guide the choice of empirical antibiotic therapy for FN, e.g. the choice between carbapenem versus ceftazidime [7, 8]. Prospective studies assessing the effectiveness of surveillance-culture-guided empirical therapy in patients with FN are scarce [14].
In order to provide rationale for surveillance-culture-guided empirical therapy for FN, we performed a multi-centre study among patients with haematological malignancy. Since 2008, data of Dutch medical microbiology laboratories are collected in the Infectious Diseases Surveillance Information System–Antimicrobial Resistance (ISIS-AR) [15]. In 2018, 47/54 (87%) laboratories were connected to ISIS-AR. Using ISIS-AR data, we aimed to assess the distribution of pathogens causing bacteraemia in patients with haematological malignancy, and the proportion of 3GC-R GNB bacteraemia that was preceded by 3GC-R GNB colonization.
Methods
We performed a descriptive retrospective study of routine microbiological surveillance data collected through the Dutch national surveillance system for antimicrobial resistance over an 11-year period (2008–2018). ISIS-AR collects all positive microbiological culture results with antimicrobial susceptibility test derived using automated systems, gradient tests and/or the disk diffusion method, including minimum inhibitory concentration (MIC) values and inhibition zone diameters, of isolates routinely tested in medical microbiology laboratories in the Netherlands [15]. ISIS-AR contains data from university and non-university hospitals, as well as general practices and long-term care facilities. Basic patient information such as age, sex and hospital ward is available, but does not include clinical variables (e.g. diagnosis, comorbidities, and treatment regimens). ISIS-AR does not contain data about negative culture results, or about cultured isolates without phenotypical antimicrobial susceptibility test.
Data was extracted on positive cultures with a sampling date between 2008 and 2018 from both adult and paediatric patients admitted to a haematology ward at the date of sampling or for whom the culture was requested by a haematologist. As the sole indication to obtain surveillance cultures on the haematology ward in the Netherlands is the weekly assessment of colonization status in patients receiving high-risk chemotherapy (myelosuppressive chemotherapy resulting in myelosuppression and mucositis), we used surveillance samples gathered on the haematology ward as a proxy to identify patients that received high-risk chemotherapy [16]. In some hospitals surveillance cultures are also used to identify colonization with other pathogenic micro-organisms (e.g. Candida species). As surveillance cultures are also obtained on the Dutch Intensive Care units (ICUs) in non-haematology patients we excluded culture from ICU patients. Because most high-risk neutropenic patients are treated in-hospital we also excluded cultures from outpatients. We extracted data on isolates taken for non-diagnostic, specified as such by the laboratory, often based on (a combination of) specimen type, specialty and specific culture requests (e.g. targeted screening for resistant microorganisms). These isolates, the majority consisting of rectal or pharyngeal/upper airway tract cultures, are further referred to as surveillance isolates and considered a proxy for colonization status. We also extracted data on diagnostic blood isolates submitted only by those laboratories for which data on surveillance cultures were available at any time between 2008 and 2018. We categorized all isolates as Gram-positive, Gram-negative or not applicable/unknown and by (group of) microorganism based on clinical and/or microbiological relevance. Isolates of GNB were categorized by their susceptibility to third-generation cephalosporins (3GC) and carbapenems, after reinterpretation of MIC values according to clinical breakpoints set by the European Committee on Antimicrobial Susceptibility Testing (EUCAST, version 8.0; 2018), and prioritizing results from gradient tests over automated MIC results. Zone diameter values were excluded, as methods for disk diffusion are not harmonized across laboratories, changed over time, and exact inhibition zone diameters are often not reported to ISIS-AR. For microorganisms without EUCAST breakpoints, or isolates without MIC values, the S/I/R interpretation as reported by the laboratory was used, if available. A GNB isolate was categorized as 3GC-R if intermediately susceptible or resistant (I + R) to ceftriaxone, cefotaxime or ceftazidime, and otherwise as 3GC-S. GNB isolates without susceptibility testing for any of these antimicrobials were excluded from the analysis. Enterobacterales species with constitutive AmpC production -e.g. Citrobacter freundii, Enterobacter cloacae complex, Klebsiella aerogenes and Serratia marcescens- were regarded as intrinsically resistant and labelled as 3GC-R regardless of MIC, since selection of AmpC de-repressed cephalosporin-resistant mutants can occur during therapy. Stenotrophomonas maltophilia isolates were also categorized as 3GC-R, regardless of MIC [17]. GNB were categorized carbapenem-resistant if intermediately susceptible or resistant (I + R) to meropenem or imipenem, and otherwise as non-carbapenem-resistant (i.e. carbapenem-susceptible or unknown).
We performed two analyses to answer two research questions. In analysis 1, to assess the distribution of microorganisms and the prevalence of 3GC-R GNB in bacteraemia, we approximated a representative sample of bacteraemia episodes, in different stages of treatment, by including the first blood isolate—regardless of the microorganism or its resistance profile- within a period of six months for each patient. Herewith we aimed to avoid oversampling of patients with recurrent or persistent infections and provide an unbiased distribution of pathogens causing bacteraemia in this patient population. We calculated the distribution of (groups of) microorganisms and the proportion of 3GC-R GNB found during bacteraemia. Among isolates of 3GC-R GNB, we counted specific species, and the number of carbapenem-resistant isolates. In analysis 2, to determine the proportion of 3GC-R GNB bacteraemia preceded by 3GC-R GNB colonization, we combined data on all surveillance and blood isolates per patient. In this combined dataset, we identified patients with paired GNB surveillance and blood isolates, defined as patients having a GNB surveillance isolate, followed by a GNB blood isolate in the 3–365 days thereafter. This pair was made independent of exact causative micro-organism, since colonization with any 3GC-R GNB pathogen could result in a change of antibiotic management. If multiple isolates per patient were available, either from the same or from different cultures, we prioritized 3GC-R GNB over 3GC-S GNB. If multiple pairs were eligible for a patient we selected the pair of isolates with the shortest time interval. Patients with a paired surveillance and blood isolate were categorized according to 3GC susceptibility of both isolates: neither 3GC-R, either the surveillance isolate or blood isolate 3GC-R, or both 3GC-R. Among patients with a 3GC-R GNB blood isolate and a paired GNB surveillance isolate, we calculated the median number of days between both isolates. To assess the influence of the maximum time interval—between a paired surveillance and blood isolate (365 days)—on the proportion of 3GC-R GNB bacteraemia preceded by 3GC-R GNB colonization, we performed a sensitivity analysis using a 30-day maximum interval. In identifying patients with paired surveillance and blood isolates, we selected patients with a paired GNB surveillance and GNB blood isolate, rather than patients with any reported surveillance isolate regardless of the microorganism and a GNB blood isolate. Due to selective culture methods used by most laboratories to detect colonization with GNB (or other pathogenic microorganisms, varying between laboratories), and since cultures without antimicrobial susceptibility test results are not available in the ISIS-AR database, the total number of reported surveillance isolates is an underestimation of the true number of colonized patients and was therefore not used in this analysis.
All analyses were performed using SAS software (version 9.4; SAS Institute, Cary, North Carolina). As no identifiable personal data are collected, individual patient consent was not required for this study.
Results
Between 2008 and 2018, 12,191 blood isolates from 3887 patients and 21,383 surveillance isolates from 4790 patients were available in the ISIS-AR database. These data were submitted by eleven laboratories representing 13 hospitals. Of 3887 patients with bacteraemia, 3074 (79.0%) were treated in tertiary care or specialized hospitals.
Distribution of pathogens and proportion of 3GC-R GNB in blood isolates
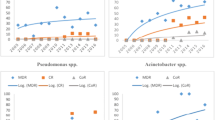
In total, 4142 of 12,191 blood isolates were identified and included as representative of an episode of bacteraemia. The majority of isolates (3369, 81.3%) comprised Gram-positive bacteria, 715 (17.3%) were Gram-negative bacteria, and for 58 isolates (1.4%) Gram stain categorization was not possible (e.g. due to incomplete microorganism identification) or not applicable (Fig. 1A). Among Gram-negative bacteria, Enterobacterales species not constitutively producing AmpC were most frequently isolated (464, 64.9% of GNB, 11.2% of the bacteraemia episodes), whereas P. aeruginosa (86, 12.0% of GNB, 2.1% of the bacteraemia episodes) and Enterobacterales species constitutively producing AmpC (76, 10.6% of GNB, 1.8% of the bacteraemia episodes) were less frequently found (Table 1, Fig. 1B). Among Gram-positive species, Staphylococcus spp. non-aureus (i.e. mainly coagulase-negative staphylococci) comprised the majority of isolates (1957, 58.1%), followed by Streptococcus spp. (574, 17.0%). Staphylococcus aureus was less frequently isolated (149, 4.4%, Fig. 1C). Candida species were found in 48 blood isolates (82.8% of isolates with unknown or non-applicable Gram stain, 1.2% of the bacteraemia episodes, Fig. 1D).
In total, 221 isolates were 3GC-R GNB, which is 30.9% of GNB isolates and 5.3% of the bacteraemia episodes. The most commonly isolated species among 3GC-R GNB were Enterobacterales not constitutively producing AmpC (85, 38.5%) and Enterobacterales constitutively producing AmpC (76, 34.4%, Table 1). The proportion of 3GC-R among Enterobacterales not constitutively producing AmpC, i.e. likely extended-spectrum beta-lactamase (ESBL)-producing Enterobacterales, was 18.3% (85/464, Table 1). Carbapenem resistance was present in 38/221 (17.2%) isolates (Table 1), the majority (57.9%) due to 22 S. maltophilia isolates regarded as intrinsically resistant to beta-lactam antibiotics. Five out of eight 3GC-R P. aeruginosa isolates were also resistant to carbapenems.
Paired GNB surveillance and blood isolates
Paired GNB surveillance and blood isolates, i.e. any GNB surveillance isolate, followed by any GNB blood isolate, were identified for 321 patients (Fig. 2), of which 43.3% (139/321) had a 3GC-R GNB blood isolate. In those 139 patients with 3GC-R GNB blood isolate, the blood isolate was found after a median of 10 days (IQR 5–23 days) after the GNB surveillance isolate. In 76.2% (106/139), the 3GC-R GNB blood isolate was preceded by a GNB surveillance isolate that was also 3GC-R. When reducing the maximum interval between the paired isolates to 30 days instead of 365 days in a sensitivity analysis, the percentage of 3GC-R GNB bacteraemia preceded by 3GC-R GNB surveillance cultures was similar (75.4%, 86/114). In 54.8% (176/321) of the patients with paired isolates, a 3GC-R GNB surveillance isolate was present.
Schematic overview1 of numbers of patients with (3GC-R GNB) blood and surveillance isolates, and patients with any GNB surveillance isolate followed by any GNB blood culture within 1 year (time pair) between 2008 and 2018. In total, 321 patients with time-paired isolates were identified, represented by the grey overlay. In 139 patients with 3GC-R GNB blood isolates a time-paired surveillance isolate was available, represented with the slash up to the right. In 106/139 the 3GC-R GNB blood isolates was preceded by a 3GC-R GNB surveillance isolate, represented by the crossed lines. 1The overview is included for illustrative purposes, the proportions displayed in this diagram are only an approximation of true proportions. 3GC-R third-generation cephalosporin-resistant. GNB Gram-negative bacteria
Discussion
In this multi-centre study among patients with haematological malignancy admitted to Dutch hospitals -in the past decade- the overall proportion of 3GC-R GNB bacteraemia was 5.3%. In a subset of 321 patients with paired isolates -patients with a GNB surveillance isolate followed by a GNB blood isolate within a year- 76.2% of 3GC-R GNB bacteraemia was preceded by 3GC-R GNB colonization as identified using surveillance cultures.
In the first analysis, based on a representative sample of bacteraemia episodes in different stages of treatment of malignancy, 81.3% of blood isolates were Gram-positive isolates. As the etiological relevance of these species could not be determined, contamination rather than bacteraemia could not be ruled out. Nonetheless, Gram-negative bacteria were retrieved in a minority (17.3%) of positive blood cultures, and etiological relevance of these bacteria as causative agents of bacteraemia is not debated. Interestingly, 18.3% of Enterobacterales not constitutively producing AmpC was 3GC-R. This is higher than the ≤ 9% observed among E. coli, K. pneumoniae and P. mirabilis in the general inpatient population in the Netherlands in 2019 and the 4% ESBL Escherichia coli found in a survey in 2003–2010 in France [18, 19]. The substantially higher GNB resistance rate found in our study is likely explained by high prophylactic and therapeutic antimicrobial consumption in this population, compared to the general inpatient population [20, 21]. In our study, 30.9% of all GNB blood isolates was 3GC-R GNB which is similar to the prevalence of 27.6% among hematopoietic stem cell transplantation recipients in northwest Europe [22]. The prevalence of 3GC-R GNB is significantly higher in southeast Europe, with rates up to 47% in an Italian study [23], which corresponds to the median of 43% 3GC-R GNB bacteraemia among adult haematology and cancer patients worldwide [24]. Of note, the definition used for 3GC-R GNB in these studies is based on susceptibility testing of GNB and does not include intrinsically resistant GNB. Therefore, resistance is expected to be even higher if the definition of 3GC-R GNB used in our study would be applied.
Our finding that 76.2% of 3GC-R GNB bacteraemia was preceded by 3GC-R GNB colonization, is in line with previous studies. [10,11,12, 25,26,27,28] In these studies, the sensitivity of colonization with multidrug-resistant (MDR) bacteria for MDR blood stream infection ranged from 45 to 91%. For ESBL-producing Enterobacterales (ESBL-E) bacteraemia, 73.9–99.8% were preceded by ESBL-E colonization, indicating that bacteraemia in the absence of known colonization is uncommon [11, 12, 25,26,27].
While the high resistance rates found in GNB in our study can be used to justify carbapenem usage for all haematological patients with FN. This carbapenem for all approach has many disadvantages. First, carbapenems are last-resort antibiotics and using them for all patients with FN—the majority with negative blood cultures and in case of positive blood cultures only a minority is positive with 3GC-R GNB isolates (5.3% of bacteraemia episodes in our study)—could potentially induce or select multidrug-resistant bacteria. Second, the use of carbapenems is associated with the predisposition to fungal infections and development of Clostridium difficile-associated diarrhoea [2, 3, 29,30,31,32]. Our study illustrates that the value of a surveillance-culture-guided approach, to restrict carbapenems for patients colonized with 3GC-R GNB, is that 76.2% (106/139) of 3GC-R GNB bacteraemia are anticipated by surveillance cultures and would therefore receive appropriate treatment. This approach thereby reduces the risk of inappropriately treated 3GC-R GNB bacteraemia without the necessity to administer carbapenems to all high-risk neutropenic patients with fever. Considering patients with paired isolates, 139/321 (43.3%) patients with 3GC-R GNB bacteraemia would have received inappropriate empirical antimicrobial therapy if ceftazidime was the standard. With surveillance-culture-guided empirical therapy this number can be reduced to 33/321 (10.3%), given the fact that in 106/139 (76.2%) patients 3GC-R GNB colonization had been identified. Considering that 20–23% of blood cultures during FN episodes are positive for possible causative pathogens [2, 3], and that, in our study, 17.3% of these blood cultures are positive for GNB, this would result in 0.4% inappropriate empirical antimicrobial therapy per FN episode. At the same time, 145/321 (47.2%) patients were not colonized with 3GC-R GNB, and would receive ceftazidime in a surveillance-culture guided approach, substantially reducing carbapenem usage compared to an empirical regimen with standard carbapenem for all patients with FN.
This multi-centre study allowed us, for the first time in the Netherlands, to identify the distribution of pathogens in bacteraemia among patients admitted to haematology wards. The large and complete microbiological dataset reflects routine clinical practice as all consecutive surveillance and blood isolates with antimicrobial susceptibility tests were available. In this large dataset with structured and complete data on both surveillance and blood isolates, we were also able to identify patients in which bacteraemia was preceded by colonization. However, this study also has limitations. Due to limited clinical data we had to use a proxy to identify patients that received high-risk chemotherapy. Therefore the results are only representative of the inpatient haematology population. Furthermore, we only assessed concordance between surveillance and blood isolates in patients in whom GNB were isolated in both cultures, thus narrowing the scope of these results. However, because surveillance cultures are performed routinely in high-risk neutropenic patients in the Netherlands, this scope is of interest as it reflects this specific patient population. The time interval of one year between paired GNB isolates was based upon ESBL-carriage in travellers in whom most (88.7%) decolonized within one year [33]. This choice did not influence the outcome, as our sensitivity analysis shortening the interval to one month yielded similar results.
Conclusion
In this study, we found a high 3GC-R GNB bacteraemia prevalence in the haematology population compared to the general in hospital population. The majority of these 3GC-R GNB bacteraemia are preceded by 3GC-R GNB colonization. Therefore, in centres in which routine surveillance cultures are performed, a surveillance-culture guided empirical therapy could be a viable strategy to restrict the empirical use of carbapenems in this population. However, prospective clinical studies are needed to further assess the safety and benefits of this approach.
Availability of data and materials
We will share aggregated, anonymized data, which have been used for this publication, upon reasonable request.
References
Kuderer NM, et al. Mortality, morbidity, and cost associated with febrile neutropenia in adult cancer patients. Cancer. 2006;106(10):2258–66.
Klastersky J, et al. Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents. 2007;30(Suppl 1):S51–9.
Piukovics K, et al. Evaluation of bloodstream infections during chemotherapy-induced febrile neutropenia in patients with malignant hematological diseases: single center experience. Eur J Microbiol Immunol (Bp). 2015;5(3):199–204.
Averbuch D, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica. 2013;98(12):1826–35.
Zuckermann J, et al. Compliance with a critical pathway for the management of febrile neutropenia and impact on clinical outcomes. Ann Hematol. 2008;87(2):139–45.
Mokart D, et al. Neutropenic cancer patients with severe sepsis: need for antibiotics in the first hour. Intensive Care Med. 2014;40(8):1173–4.
Freifeld AG, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56-93.
Kochanek M, et al. Management of sepsis in neutropenic cancer patients: 2018 guidelines from the Infectious Diseases Working Party (AGIHO) and Intensive Care Working Party (iCHOP) of the German Society of Hematology and Medical Oncology (DGHO). Ann Hematol. 2019;98(5):1051–69.
Herbers AHE, et al. Bacteraemia coincides with low citrulline concentrations after high-dose melphalan in autologous HSCT recipients. Bone Marrow Transplant. 2008;42(5):345–9.
Forcina A, et al. Clinical impact of pretransplant multidrug-resistant gram-negative colonization in autologous and allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24(7):1476–82.
Satlin MJ, et al. Colonization with levofloxacin-resistant extended-spectrum β-lactamase-producing enterobacteriaceae and risk of bacteremia in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2018;67(11):1720–8.
Vehreschild MJ, et al. A multicentre cohort study on colonization and infection with ESBL-producing Enterobacteriaceae in high-risk patients with haematological malignancies. J Antimicrob Chemother. 2014;69(12):3387–92.
Wingard JR, et al. Antibiotic-resistant bacteria in surveillance stool cultures of patients with prolonged neutropenia. Antimicrob Agents Chemother. 1986;30(3):435–9.
Khanam A, et al. Outcome of surveillance stool culture guided selection of antibiotics during febrile neutropenia in patient with acute leukaemia? Curr Tr Clin & Med Sci. 2020. https://doi.org/10.33552/CTCMS.2020.01.000515.
Altorf-van der Kuil W, et al. National laboratory-based surveillance system for antimicrobial resistance: a successful tool to support the control of antimicrobial resistance in the Netherlands. Euro Surveill 2017. https://doi.org/10.2807/1560-7917.ES.2017.22.46.17-00062
Huls GA, et al. Guidelines Acute myeloid leukemia (AML): guidelines for diagnosis and treatment. Netherland Journal of Haematology (NTVH), 2018. https://www.ariez.nl/wp-content/uploads/2018/10/NTVH7_2018_Art._Huls_AML.pdf. Accessed 11 Oct 2019.
EUCAST. Intrinsic resistance & unusual phenotypes v 3.2 February 2020. https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Expert_Rules/2020/Intrinsic_Resistance_and_Unusual_Phenotypes_Tables_v3.2_20200225.pdf. Accessed 3 Mar 2020.
de Greeff, S., A. Schoffelen, and C. Verduin, NethMap 2020: Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands in 2019 / MARAN 2020: monitoring of Antimicrobial Resistance and Antibiotic Usage in Animals in the Netherlands in 2019. 2020, Rijksinstituut voor Volksgezondheid en Milieu RIVM.
Bousquet A, et al. An 8-year survey of strains identified in blood cultures in a clinical haematology unit. Clin Microbiol Infect. 2014;20(1):O7-12.
Mikulska M, et al. Fluoroquinolone prophylaxis in haematological cancer patients with neutropenia: ECIL critical appraisal of previous guidelines. J Infect. 2018;76(1):20–37.
Verlinden A, et al. Clinical and microbiological impact of discontinuation of fluoroquinolone prophylaxis in patients with prolonged profound neutropenia. Eur J Haematol. 2014;93(4):302–8.
Averbuch D, et al. Antimicrobial resistance in gram-negative rods causing bacteremia in hematopoietic stem cell transplant recipients: intercontinental prospective study of the infectious diseases working party of the European Bone Marrow Transplantation Group. Clin Infect Dis. 2017;65(11):1819–28.
Girmenia C, et al. Incidence, risk factors and outcome of pre-engraftment gram-negative bacteremia after allogeneic and autologous hematopoietic stem cell transplantation: an Italian Prospective Multicenter Survey. Clin Infect Dis. 2017;65(11):1884–96.
Mikulska M, et al. Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Infect. 2014;68(4):321–31.
Cornejo-Juárez P, et al. Fecal ESBL Escherichia coli carriage as a risk factor for bacteremia in patients with hematological malignancies. Support Care Cancer. 2016;24(1):253–9.
Kömürcü B, et al. Rectal colonization with multidrug-resistant gram-negative bacteria in patients with hematological malignancies: a prospective study. Expert Rev Hematol. 2020. https://doi.org/10.1080/17474086.2020.1787145.
Liss BJ, et al. Intestinal colonisation and blood stream infections due to vancomycin-resistant enterococci (VRE) and extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBLE) in patients with haematological and oncological malignancies. Infection. 2012;40(6):613–9.
Nesher L, et al. Fecal colonization and infection with Pseudomonas aeruginosa in recipients of allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2015;17(1):33–8.
Gudiol C, et al. Bacteraemia due to multidrug-resistant Gram-negative bacilli in cancer patients: risk factors, antibiotic therapy and outcomes. J Antimicrob Chemother. 2011;66(3):657–63.
Ben-Ami R, et al. Antibiotic exposure as a risk factor for fluconazole-resistant candida bloodstream infection. Antimicrob Agents Chemother. 2012;56(5):2518–23.
Satlin MJ, et al. Bacteremia due to carbapenem-resistant Enterobacteriaceae in neutropenic patients with hematologic malignancies. J Infect. 2016;73(4):336–45.
Ballo O, et al. Use of carbapenems and glycopeptides increases risk for Clostridioides difficile infections in acute myeloid leukemia patients undergoing intensive induction chemotherapy. Ann Hematol. 2020;99(11):2547–53.
Arcilla MS, et al. Import and spread of extended-spectrum β-lactamase-producing Enterobacteriaceae by international travellers (COMBAT study): a prospective, multicentre cohort study. Lancet Infect Dis. 2017;17(1):78–85.
Acknowledgements
Members of the ISIS-AR study group are listed in the acknowledgements section.
Members of the ISIS-AR study group:
J.W.T. Cohen Stuart, Noordwest Ziekenhuisgroep, Department of Medical Microbiology, Alkmaar; D.C. Melles, Meander Medical Center, Department of Medical Microbiology, Amersfoort; K. van Dijk, Amsterdam UMC, Universiteit van Amsterdam, Department of Medical Microbiology and Infection Prevention, Amsterdam Infection and Immunity Institute, Amsterdam; A. Alzubaidy, Atalmedial, Department of Medical Microbiology, Amsterdam; B.F.M. Werdmuller, Public Health Service, Public Health Laboratory, Amsterdam; G.J. Blaauw, Gelre Hospitals, Department of Medical Microbiology and Infection prevention, Apeldoorn; B.M.W. Diederen, Bravis Hospital, Department of Medical Microbiology, Bergen op Zoom; ISIS-AR project team: H.J. Alblas, W. Altorf-van der Kuil, S.M. Bierman, S.C. de Greeff, S.R. Groenendijk, R. Hertroys, E.J. Kuijper, J.C. Monen, D.W. Notermans, W.J. van den Reek, A.F. Schoffelen, A.E. Smilde, C.C.H. Wielders, S.H.S. Woudt, R.E. Zoetigheid, Centre for Infectious Disease Control (CIb), National Institute for Public Health and the Environment (RIVM), Bilthoven; W. van den Bijllaardt, Microvida Amphia, Laboratory for Microbiology and Infection Control, Breda; E.M. Kraan, IJsselland hospital, Department of Medical Microbiology, Capelle a/d IJssel; E.E. Mattsson, Reinier de Graaf Groep, Department of Medical Microbiology, Delft; J.M. da Silva, Deventer Hospital, Department of Medical Microbiology, Deventer; E. de Jong, Slingeland Hospital, Department of Medical Microbiology, Doetinchem; B. Maraha, Albert Schweitzer Hospital, Department of Medical Microbiology, Dordrecht; A.J. van Griethuysen, Gelderse Vallei Hospital, Department of Medical Microbiology, Ede; G.J. van Asselt, SHL-Groep, Etten-Leur; A. Demeulemeester, SHL-Groep, Etten-Leur; B.B. Wintermans, Admiraal De Ruyter Hospital, Department of Medical Microbiology, Goes; M. van Trijp, Groene Hart Hospital, Department of Medical Microbiology and Infection Prevention, Gouda; A. Ott, Certe, Department of Medical Microbiology, Groningen; J. Sinnige, Regional Laboratory of Public Health, Haarlem; D.C. Melles, St Jansdal Hospital, Department of Medical Microbiology, Harderwijk; W. Silvis, Laboratory of Medical Microbiology and Public Health, Hengelo; L.J. Bakker, CBSL, Tergooi Hospital, Department of Medical Microbiology, Hilversum; J.W. Dorigo-Zetsma, CBSL, Tergooi Hospital, Department of Medical Microbiology, Hilversum; K. Waar, Izore Centre for Infectious Diseases Friesland, Leeuwarden; A.T. Bernards, Leiden University Medical Center, Department of Medical Microbiology, Leiden; M.A. Leversteijn-van Hall, Alrijne Hospital, Department of Medical Microbiology, Leiden-Leiderdorp; E. Schaftenaar, St Antonius Hospital, Department of Medical Microbiology and Immunology, Nieuwegein; M.H. Nabuurs-Franssen, Canisius Wilhelmina Hospital, Department of Medical Microbiology and Infectious Diseases, Nijmegen; H. Wertheim, Radboud University Medical Center, Department of Medical Microbiology, Nijmegen; B.M.W. Diederen, Bravis Hospital, Department of Medical Microbiology, Roosendaal; L. Bode, Erasmus University Medical Center, Department of Medical Microbiology, Rotterdam; M. van Rijn, Ikazia Hospital, Department of Medical Microbiology, Rotterdam; S. Dinant, Maasstad Hospital, Department of Medical Microbiology, Rotterdam; O. Pontesilli, Maasstad Hospital, Department of Medical Microbiology, Rotterdam; P. de Man, Franciscus Gasthuis and Vlietland, Department of Medical Microbiology and Infection Control, Rotterdam; M. Wong, Haga Hospital, Department of Medical Microbiology, 's-Gravenhage; A.E. Muller, MCH Westeinde Hospital, Department of Medical Microbiology, 's-Gravenhage; N.H. Renders, Jeroen Bosch Hospital, Department of Medical Microbiology and Infection Control, 's-Hertogenbosch; R.G. Bentvelsen, Microvida ZorgSaam, Department of Medical Microbiology, Terneuzen; A.G.M. Buiting, St. Elisabeth Hospital, Department of Medical Microbiology, Tilburg; A.L.M. Vlek, Diakonessenhuis, Department of Medical Microbiology and Immunology, Utrecht; A.J. Stam, Saltro Diagnostic Centre, Department of Medical Microbiology, Utrecht; A. Troelstra, University Medical Center Utrecht, Department of Medical Microbiology, Utrecht; I.T.M.A. Overdevest, PAMM, Department of Medical Microbiology, Veldhoven; M.P.A. van Meer, Rijnstate Hospital, Laboratory for Medical Microbiology and Immunology, Velp; C. Oliveira dos Santos, Isala Hospital, Laboratory of Medical Microbiology and Infectious Diseases, Zwolle; M.J.H.M. Wolfhagen, Isala Hospital, Laboratory of Medical Microbiology and Infectious Diseases, Zwolle
Funding
The Dutch national antimicrobial resistance surveillance system (ISIS-AR) is supported by the Dutch Ministry of Health, Welfare and Sport. This study was conducted as part of the authors’ routine work and the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
Data analysis was performed by SHSW. The first draft of the manuscript was written by JRC and all authors commented on earlier versions of the manuscript. JRC, SHSW, AFS, JH, NAJ, TB, MKB, MMCL, RPS and KCES all contributed to the study concept and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval from the Institutional review boards was not required for this study because we used retrospective, pseudonymised data for quality optimization purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de la Court, J.R., Woudt, S.H.S., Schoffelen, A.F. et al. Third-generation cephalosporin resistant gram-negative bacteraemia in patients with haematological malignancy; an 11-year multi-centre retrospective study. Ann Clin Microbiol Antimicrob 21, 54 (2022). https://doi.org/10.1186/s12941-022-00544-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-022-00544-0