Abstract
Aim
The aim of the present study is to compare the performance of 16S rRNA Nanopore sequencing and conventional culture in detecting infectious pathogens in patients with suspected meningitis in a resource-limited setting without extensive bioinformatics expertise.
Methods
DNA was isolated from the cerebrospinal fluid (CSF) of 30 patients with suspected bacterial meningitis. The isolated DNA was subjected to 16S sequencing using MinION™. The data were analysed in real time via the EPI2ME cloud platform. The Nanopore sequencing was done in parallel to routine microbiological diagnostics.
Results
Nanopore sequencing detected bacterial pathogens to species level in 13 of 30 (43%) samples. CSF culture showed 40% (12/30) positivity. In 21 of 30 patients (70%) with suspected bacterial meningitis, both methods yielded concordant results. About nine of 30 samples showed discordant results, of these five were false positive and four were false negative. In five of the culture negative results, nanopore sequencing was able to detect pathogen genome, due to the higher sensitivity of the molecular diagnostics. In two other samples, the CSF culture revealed Cryptococcus neoformans and Streptococcus pneumoniae, which were not detected by Nanopore sequencing. Overall, using both the cultures and 16S Nanopore sequencing, positivity rate increased from 40% (12/30) to 57% (17/30).
Conclusion
Next-generation sequencing could detect pathogens within six hours and could become an important tool for both pathogen screening and surveillance in low- and middle-income countries (LMICs) that do not have direct access to extensive bioinformatics expertise.
Similar content being viewed by others
Introduction
Bacteria, viruses, fungi and protozoa are common causes of sepsis and meningitis. The majority of cases result from bacterial infections. It is estimated that 48.9 million cases and 11 million of the sepsis-related fatalities reported worldwide in 2017 accounted for 20% of all global deaths [1]. Further, meningitis caused an estimated 250,000 deaths in 2019 [2]. The infections are highly prevalent in low and middle-income countries (LMIC), and the lack of infrastructure and appropriate diagnostic facilities leads to the high morbidity and mortality [3, 4]. Both bacterial meningitis and septic shock are life-threatening emergencies; therefore, quick and accurate diagnoses are essential. Cerebrospinal fluid (CSF) and blood cultures are the diagnostic gold standards; however, cultures are time-consuming. Any delay in the diagnosis increases mortality and hospital stays, but also health care expenditures [5,6,7]. Several studies that have compared the yield of bacterial cultures with PCR-based diagnosis have found that 30–50% of culture-negative CSF specimens are positive when applying molecular tools [8, 9]. These discrepancies may be explained by the empiric use of antibiotics, a low bacterial count, low blood volume, or non-culturable and fastidious organisms that require special growth conditions [10]. RT-PCR for detecting bacteria are now rapidly being used and offer a quick alternative in the timely diagnosis of a causative pathogen, thus reasonably complementing culture-based microbiological diagnostics.
Recently, several commercial 16S PCR platforms have been made available for sepsis diagnosis, including Universal digital high-resolution melt (U-dHRM), SepsiTest™, LightCycler™ SeptiFast, and the IRIDICA system [11]. The initial hardware and recurring expenses are high, rendering these systems largely unaffordable in most LMIC. The 16S rRNA gene has proven to be useful in diagnosing bacterial infections [6, 10]. Next-generation sequencing (NGS) technologies are now becoming an important diagnostic tool in detecting infectious diseases, directly from patient samples [12,13,14]. The Oxford Nanopore Technologies (ONT) NGS is gaining attention as it has several advantages compared to other sequencing platforms. It is a portable device, requires manageable financial investment and low maintenance costs. Moreover, it provides a rapid turnaround time with user-friendly EPI2ME cloud-based bioinformatics pipelines [12]. A previous disadvantage of this technology was that it had a high sequencing error rate of 5–15% [15]. Meanwhile the technology has improved significantly with far lower error rate, i.e., < 3.5% [16]. High throughput sequencing using the Flongle™ flowcell will considerably reduce the costs per sample and thus allowing the use of such technology in a LMIC setting.
Rapid identification of infectious disease and access to their genomes is essential for establishing successful therapeutic and preventive measures [17]. Several studies have shown that the portable Nanopore sequencing system can be used for rapid and accurate diagnosis of bacterial meningitis, sepsis, and other infections from a variety of samples in both developed and LMIC countries [18,19,20,21,22,23,24].
The Nanopore system has been used extensively for infectious disease surveillance and diagnosis. It has been used in low-resource settings to monitor and sequence ZIKA, EBOV, and SARS-CoV-2 viral genomes during outbreaks in Brazil, Guinea, and worldwide [25,26,27,28]. Despite these successes of nanopore sequencing, limitations remain, such as the limited sample size used in most studies and the use of in-house bioinformatics pipelines that require bioinformatics expertise [18, 19]. Some of these studies were performed with positive blood cultures rather than directly with clinical samples [20, 21], which is time consuming. Since only a few studies have been conducted to date, further studies are needed to validate the Nanopore system and assess its sensitivity, specificity, and utility in clinical applications.
The aim of the present study was to use the Nanopore MinION™ NGS tool for direct diagnosis and genotyping of bacterial meningitis in patients with suspected bacterial meningitis in CSF samples based on 16S rRNA sequencing using the Nanopore EPI2ME cloud without specific on-site bioinformatics expertise. The 16S rRNA results shall be compared with culture methods routinely used to screen for pathogens.
Methods and materials
Study cohort
The retrospective hospital-based cohort study was collected between 2019 and 2020 at 108 Military Central Hospital, a referral hospital for adults with a catchment area including Hanoi and the northern provinces of Vietnam. Microbiological examination was performed by microscopy of CSF according to the hospital routine standards. All recruited patients were admitted to the infectious diseases department and aged 15 years or older, with symptomatic meningitis based on criteria for a central nerval system (CNS) infection and eligible for inclusion [29]. The inclusion criteria were clinical signs of CNS infection such as fever, headache, vomiting, neck stiffness, elevated C-reactive protein, procalcitonin, white blood cell count, focal neurological signs including seizures and altered consciousness, and/or elevated white blood cell count (WBC) in CSF. Patients with other etiologies as a cause for the neurological disorder were excluded.
The diagnostic results of the CSF from the patients in the study were available from the routine microbiological diagnostics. However, the diagnostic results were blinded until Nanopore sequencing was completed. In this retrospective study we included specimens from 30 patients with the clinical diagnosis of bacterial meningitis based on routine laboratory parameters summarized in Table 1. Two of the 30 (7%) patients with suspected bacterial meningitis had lethal outcome.
For microbiology cultures and molecular assessment, at least 2 mL of CSF was obtained by lumbar puncture. Samples were stored at − 80 °C until further use. According to international standards, clinical cases were categorized in three distinct groups by CSF values [29]. Bacterial CNS infection were defined by WBC > 10 predominance of polymorphonucleocytes, protein > 1 g/L, and glucose < 40 mg/dL; aseptic/viral CNS infection (VI) defined by WBC > 10, predominance of lymphocytes, protein < 2 g/L, and normal glucose levels; tuberculous CNS infection defined by WBC > 10, predominance of lymphocytes, protein > 1 g/L, and glucose < 40 mg/dL.
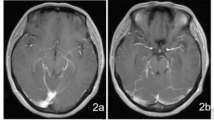
Diagnostic procedures and treatment of patients followed the clinical routine. Demographic and clinical data, routine hematology, and clinical biochemistry parameters as well as blood culture results were recorded. In addition, computed tomography (CT) or magnetic resonance imaging (MRI) was performed. The CSF patients were treated with ceftriaxone, meropenem, vancomycin, colistin, levofloxacin, and moxifloxacin antibiotics. Sepsis patients were treated with levofloxacin, amikacin, moxifloxacin, linezolid, vancomycin, ceftazidime, piperacillin-tazobactam, tiepenem, meropenem, cefoxitin, doripenem, and ampicillin-sulbactam. In total 30 samples from 30 patients were included in the study.
Microbiological diagnostic of CSF culture
The microbiological diagnostic was performed in the routine diagnostics following the current diagnostical standards. Identification of bacterial species was performed using the VITEK® 2 automated system (BioMérieux, Craponne, France).
DNA isolation
DNA was extracted from one mL of CSF from patient samples using the SaMag bacterial DNA extraction kit (Sacace Biotechnologies S.r.l., Como, Italy) [30]. Human DNA in the samples was depleted using mammalian cell lysis buffer 1 (2 M Na2CO2 pH 9.8, 1% Triton-X100) before proceeding with the SaMag extraction kit as described previously [31]. DNA quality and quantity was assessed with the Qubit™ 4 fluorometer using the Qubit™ dsDNA BR Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA).
16S rRNA sequencing with nanopore MinION™
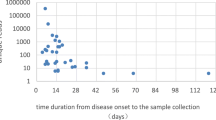
For multiplex sequencing, the16S rRNA gene was PCR-amplified from CSF sample DNA using the 16S barcoding kit SQK-16S024 (Oxford Nanopore Technologies, Oxford, UK) following the manufacturer’s instructions. The 16S barcoding kit includes 16S primers covering full-length 16SrRNA (~ 1500 bp) (16S-27F—AGRGTTTGATYHTGGCTCAG 16S-1492R-TACCTTGTTAYGACTT) [32, 33]. The PCR was performed using 10 μL of DNA sample (concentration range < 1–50 ng/µL) per reaction, including a blood culture positive control of an Acinetobacter baumannii strain and a non-template control. Amplicons were purified using AMPure XP beads, quantified using the Qubit™ 4 fluorometer with the Qubit™ dsDNA BR Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA), and pooled having total 100 ng of the 16S PCR amplicons in 10 µL (5 ng /sample). Sequencing was performed with the R9.4.1 MinION™ system for six hours (Oxford Nanopore Technologies, Oxford, UK) and data collected using fast-basecalling by the MinKNOW software (v.18.01.6). Data generated by MinKNOW was analyzed in real-time on the Nanopore EPI2ME cloud. The EPI2ME analysis was performed using complete sequencing data generated from sequencing run and 200 NGS reads/sample, and the read length cut-off was set to min 1400 bp to max 1700 bp (sequencing statistics are summarized in Additional file 1: Table S1).
Results
Pathogens identified by CSF culture and blood culture
Of the 30 CSF specimens, 12 (40%) yielded positive result from CSF cultures and the pathogens included Streptococcus pneumoniae (n = 4), Streptococcus suis (n = 4), Streptococcus mitis (n = 1), Pseudomonas aeruginosa (n = 1), Aeromonas Sobria (n = 1) and Cryptococcus neoformans (n = 1). S. pneumoniae and S. suis were the most common pathogen (33%; 4/12 for each species) identified by CSF culture. In 5/30 (17%) patients, the same bacterial species were also detected in blood culture, they included: S. pneumoniae (n = 2), S. suis (n = 3), and Staphylococcus xylosus (n = 1).
Pathogens identified using 16S Nanopore sequencing
On screening the 30 patient specimens for pathogenic bacteria, we observed a 16S-PCR positivity of 43% (13/30) using the Oxford Nanopore 16S Barcoding Kit (SQK-16S024). EPI2ME cloud data analysis results were identical when using all reads generated per sample (Additional file 1: Table S1) or using only the first 200 reads per sample. Therefore, our data suggests that 200 reads/sample may be sufficient for reliable pathogen detection. Further reduction to 100 reads per sample would also have produced identical results. However, we arbitrarily retained the 200 reads per sample. The pathogens identified include S. suis (n = 5), S. pneumoniae (n = 4), Enterococcus hirae (n = 1), Neisseria gonorrhoeae (n = 1), Klebsiella pneumoniae (n = 1), Aeromonas jandaei (n = 1). Multiplex sequencing of 16S PCR amplicons from all samples in a single run with Nanopore MinION sequencing and real-time NGS data analysis on EPI2ME Cloud detected bacterial pathogens at the species level within one hour. The DNA concentration for each sample is summarized in Table 3. The bacterial species identified by Nanopore sequencing of all the 16S PCR positive samples are summarized in Table 2. S. suis and S. pneumoniae were the most common pathogen (5/30; 17% and 4/30; 13%, respectively) detected using this method.
Comparison of conventional microbiology and Nanopore sequencing
Overall, 21 of 30 CSF samples displayed concordant results between Nanopore sequencing and conventional culture. Nanopore sequencing was able to detect eight of 12 (67%) culture positive samples correctly. Nine of thirty (30%) samples showed discordant results, of these five were culture negative and yielded positive signal in the Nanopore and four were culture positive but yielded negative signal in the Nanopore. In five of the 18 (28%) culture negative results, nanopore yielded positive signals, indicating that the Nanopore sequencing was able to detect pathogens in additional samples, due to the higher sensitivity of the 16S PCR. Overall, using both the cultures and 16S Nanopore sequencing, positivity rate increased from 40% (12/30) to 57% (17/30). In four of 12 samples, Nanopore did not yield positive results for S. pneumoniae (C7 and C14), P. aeruginosa (C12) and C. neoformans (C19). In the two culture-positive and Nanopore-negative samples, S. pneumonia were plausible since S. pneumoniae were also detected in the blood culture of these patients. For the culture-positive Nanopore-negative with P. aeruginosa (C12), the CSF culture and the blood culture delivered diverging results so that the reliability and the plausibility of this results is questionable. In sample C19, a Nanopore-negative and culture-positive results was expected since C. neoformans is a fungus and thus would not be detected by 16S-based sequencing. For samples C6 and C30, the culture and Nanopore sequencing results were divergent at the species level but not the genus level. A potential explanation may be the limited accuracy of biochemical identification to the species level. However, since the genus of these bacteria were concordant and thus these were interpreted as concordant results (Table 3).
Discussion
This study demonstrated that 16S multiplex sequencing using Nanopore sequencing was able to detect pathogens rapidly and inexpensively at the species level directly from CSF samples in a LMIC setting. Nanopore 16S sequencing was able to identify pathogens that were not detected by routine diagnostic methods. Predominant bacteria in CSF samples were S. pneumoniae and S. suis. This is consistent with results of a recent study of CSF samples in Vietnam [19]. Furthermore, in Vietnam, S. suis has been reported to be the most commonly diagnosed bacterium in bacterial meningitis of adults [34, 35], consistent with our results. S. suis is widely distributed in East and Southeast Asia, where there is a high density of pigs. Distinct S. suis serotypes are known to be highly virulent and to cause severe infections in pigs and humans [36, 37].
Our results are concordant with previous studies, which showed superior performance of NGS-based detection method in detecting pathogens in patients with central nervous system infections [9, 38, 39]. Implementation of molecular-based method as a complimentary method to conventional culture may improve the sensitivity of pathogen detection as indicated by our study. Cerebrospinal fluid (CSF) and blood cultures have been the diagnostic gold standard; however, cultures are time-consuming. Our findings suggest that ≤ 200 reads per sample generated are sufficient to identify bacteria at the species level within an hour using the Nanopore EPI2ME cloud. Rapid identification of bacterial pathogens in bloodstream infections within 6–12 h can accelerate the initiation of appropriate treatment to improve the clinical outcome [40,41,42].
Oxford Nanopore Technologies (ONT) NGS system is gaining attention as it has several advantages compared to other sequencing platforms. It is a portable device, requires manageable financial investment and low maintenance costs. Moreover, it provides a rapid turnaround time with user-friendly bioinformatics pipelines [12]. Multiplexing sequencing using the MinION system will considerably reduce the costs per sample. For example, the cost of sequencing to detect the bacterial pathogen in any given sample using Oxford Nanopore's 16S barcoding kit is $10. In addition, there is no need for annual instrument maintenance or the use of a bioinformatician, as the data can be analysed directly on Oxford Nanopore's EPI2ME cloud data analysis platform. This additionally reduces the overall cost of maintaining and sustaining Nanopore NGS in LMICs. Furthermore, coinfections or mixed bacterial infections are common in clinics and hospitals and particularly common in the lower respiratory tract and intestinal tract [43, 44]. These coinfections or mixed bacterial infections can be detected using Nanopore NGS shotgun metagenomics or 16S rRNA metagenomic sequencing [45]. As Nanopore NGS has potential to give ultralong reads and real-time data, turnover time can be reduced significantly and thus shorter time-to-result. Additionally, metagenomics approach may provide additional genomic information such as clonal assignment and in-silico analysis of antimicrobial resistance determinants [44].
There are several limitations of the study. First, the study was performed using a small sample size of 30 samples. The small sample size was largely indebted to the limited number of patients with the clinical diagnosis of meningitis admitted to the hospital. Nonetheless, the laboratory parameters of these patients were consistent with the expected laboratory parameters of patients with bacterial meningitis. Furthermore, most studies on the performance of NGS-based detection method were not performed in resource-limited settings. Our study indicates that 16S Nanopore sequencing can be used in resource-limited setting to complement or improve the sensitivity of microbiological diagnostics for bacterial meningitis. In this study, we did not perform metagenomics sequencing. However, as a perspective, metagenomics using nanopore sequencing could be implemented in routine diagnostics for a non-biased pathogen identification and in-silico antibiotic resistance analysis and should be validated in further studies [46].
Conclusion
The results of this study demonstrate that the 16S multiplex Nanopore sequencing for pathogen detection directly from CSF samples is feasible within six hours without the need of extensive bioinformatics expertise and high-end computing capacities. 16S nanopore sequencing can be a rapid alternative or complementary detection method to conventional microbiological cultures and aid in the timely diagnosis of a causative pathogen in both developed and LMIC countries. Minor optimizations in DNA isolation methodology and increase in sample volumes may be necessary to increase the sensitivity. Acceleration of microbiological diagnostics through the implementation of modern technologies is important and may have a significant impact in improving the clinical management and outcome of severe infections.
Availability of data and materials
Not applicable. The authors confirm that the data supporting the findings of this study are available within the article and in its supplementary material.
Abbreviations
- 16S rRNA:
-
16S ribosomal RNA
- ONT:
-
Oxford Nanopore Technologies
- NAT:
-
Nucleic acid test
- CSF:
-
Cerebrospinal fluid
- LMIC:
-
Low and middle-income countries
- NGS:
-
Next-generation sequencing
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- WBC:
-
White blood cells
- CNS:
-
Central nerval system
- bp:
-
Base pair
References
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer S, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11.
Defeating meningitis by 2030: baseline situation analysis. https://www.who.int/initiatives/defeating-meningitis-by-2030. Accessed 27 June 2022.
McGloughlin S, Richards GA, Nor MBM, Prayag S, Baker T, Amin P. Sepsis in tropical regions: report from the task force on tropical diseases by the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2018;46:115–8.
Kumalo A, Kassa T, Mariam ZS, Daka D, Tadesse AH. Bacterial profile of adult sepsis and their antimicrobial susceptibility pattern at Jimma University specialized hospital, south West Ethiopia. Health Sci J. 2016;10(2):1.
Grumaz S, Grumaz C, Vainshtein Y, Stevens P, Glanz K, Decker SO, Hofer S, Weigand MA, Brenner T, Sohn K. Enhanced performance of next-generation sequencing diagnostics compared with standard of care microbiological diagnostics in patients suffering from septic shock. Crit Care Med. 2019;47(5):e394–402.
Jordana-Lluch E, Gimenez M, Quesada MD, Ausina V, Martro E. Improving the diagnosis of bloodstream infections: PCR coupled with mass spectrometry. Biomed Res Int. 2014;2014: 501214.
Weiss SL, Fitzgerald JC, Balamuth F, Alpern ER, Lavelle J, Chilutti M, Grundmeier R, Nadkarni VM, Thomas NJ. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. 2014;42(11):2409–17.
Obaro S. Updating the diagnosis of bacterial meningitis. Lancet Infect Dis. 2019;19(11):1160–1.
Wilson MR, Sample HA, Zorn KC, Arevalo S, Yu G, Neuhaus J, Federman S, Stryke D, Briggs B, Langelier C, et al. Clinical metagenomic sequencing for diagnosis of meningitis and encephalitis. N Engl J Med. 2019;380(24):2327–40.
Mishra D, Satpathy G, Wig N, Fazal F, Ahmed NH, Panda SK. Evaluation of 16S rRNA broad range PCR assay for microbial detection in serum specimens in sepsis patients. J Infect Public Health. 2020;13(7):998–1002.
Sinha M, Jupe J, Mack H, Coleman TP, Lawrence SM, Fraley SI. Emerging technologies for molecular diagnosis of sepsis. Clin Microbiol Rev. 2018. https://doi.org/10.1128/CMR.00089-17.
Petersen LM, Martin IW, Moschetti WE, Kershaw CM, Tsongalis GJ. Third-generation sequencing in the clinical laboratory: exploring the advantages and challenges of Nanopore sequencing. J Clin Microbiol. 2019. https://doi.org/10.1128/JCM.01315-19.
Goldberg B, Sichtig H, Geyer C, Ledeboer N, Weinstock GM. Making the leap from research laboratory to clinic: challenges and opportunities for next-generation sequencing in infectious disease diagnostics. mBio. 2015;6(6):e01888-01815.
Forbes JD, Knox NC, Ronholm J, Pagotto F, Reimer A. Metagenomics: the next culture-independent game changer. Front Microbiol. 2017;8:1069.
Rang FJ, Kloosterman WP, de Ridder J. From squiggle to basepair: computational approaches for improving nanopore sequencing read accuracy. Genome Biol. 2018;19(1):90.
Gonzalez-Recio O, Gutierrez-Rivas M, Peiro-Pastor R, Aguilera-Sepulveda P, Cano-Gomez C, Jimenez-Clavero MA, Fernandez-Pinero J. Sequencing of SARS-CoV-2 genome using different nanopore chemistries. Appl Microbiol Biotechnol. 2021;105(8):3225–34.
Cao Y, Li J, Chu X, Liu H, Liu W, Liu D. Nanopore sequencing: a rapid solution for infectious disease epidemics. Sci China Life Sci. 2019;62(8):1101–3.
Nakagawa S, Inoue S, Kryukov K, Yamagishi J, Ohno A, Hayashida K, Nakazwe R, Kalumbi M, Mwenya D, Asami N, et al. Rapid sequencing-based diagnosis of infectious bacterial species from meningitis patients in Zambia. Clin Transl Immunol. 2019;8(11): e01087.
Hong NTT, Nghia HDT, Thanh TT, Lan NPH, Ny NTH, Ngoc NM, Hang VTT, Chau LTM, Quynh VX, Diem LT, et al. Cerebrospinal fluid MinION sequencing of 16S rRNA gene for rapid and accurate diagnosis of bacterial meningitis. J Infect. 2020;80(4):469–96.
Ashikawa S, Tarumoto N, Imai K, Sakai J, Kodana M, Kawamura T, Ikebuchi K, Murakami T, Mitsutake K, Maesaki S, et al. Rapid identification of pathogens from positive blood culture bottles with the MinION nanopore sequencer. J Med Microbiol. 2018;67(11):1589–95.
Anson LW, Chau K, Sanderson N, Hoosdally S, Bradley P, Iqbal Z, Phan H, Foster D, Oakley S, Morgan M, et al. DNA extraction from primary liquid blood cultures for bloodstream infection diagnosis using whole genome sequencing. J Med Microbiol. 2018;67(3):347–57.
Udaondo Z, Jenjaroenpun P, Wongsurawat T, Meyers E, Anderson C, Lopez J, Mohan M, Tytarenko R, Walker B, Ussery D, et al. Two cases of vancomycin-resistant Enterococcus faecium bacteremia with development of daptomycin-resistant phenotype and its detection using oxford nanopore sequencing. Open Forum Infect Dis. 2020;7(6):180.
Grumaz C, Hoffmann A, Vainshtein Y, Kopp M, Grumaz S, Stevens P, Decker SO, Weigand MA, Hofer S, Brenner T, et al. Rapid next-generation sequencing-based diagnostics of bacteremia in septic patients. J Mol Diagn. 2020;22(3):405–18.
Moon J, Kim N, Kim TJ, Jun JS, Lee HS, Shin HR, Lee ST, Jung KH, Park KI, Jung KY, et al. Rapid diagnosis of bacterial meningitis by nanopore 16S amplicon sequencing: a pilot study. Int J Med Microbiol. 2019;309(6): 151338.
Faria NR, Sabino EC, Nunes MR, Alcantara LC, Loman NJ, Pybus OG. Mobile real-time surveillance of Zika virus in Brazil. Genome Med. 2016;8(1):97.
Quick J, Loman NJ, Duraffour S, Simpson JT, Severi E, Cowley L, Bore JA, Koundouno R, Dudas G, Mikhail A, et al. Real-time, portable genome sequencing for Ebola surveillance. Nature. 2016;530(7589):228–32.
Bull RA, Adikari TN, Ferguson JM, Hammond JM, Stevanovski I, Beukers AG, Naing Z, Yeang M, Verich A, Gamaarachchi H, et al. Analytical validity of nanopore sequencing for rapid SARS-CoV-2 genome analysis. Nat Commun. 2020;11(1):6272.
Freed NE, Vlkova M, Faisal MB, Silander OK. Rapid and inexpensive whole-genome sequencing of SARS-CoV-2 using 1200 bp tiled amplicons and Oxford Nanopore Rapid Barcoding. Biol Methods Protoc. 2020;5(1):bpaa014.
Mount HR, Boyle SD. Aseptic and bacterial meningitis: evaluation, treatment, and prevention. Am Fam Physician. 2017;96(5):314–22.
Trung NT, Hien TT, Huyen TT, Quyen DT, Van Son T, Hoan PQ, Phuong NT, Lien TT, Binh MT, Van Tong H, et al. Enrichment of bacterial DNA for the diagnosis of blood stream infections. BMC Infect Dis. 2016;16:235.
Trung NT, Thau NS, Bang MH, Song LH. PCR-based Sepsis@Quick test is superior in comparison with blood culture for identification of sepsis-causative pathogens. Sci Rep. 2019;9(1):13663.
Zeng YH, Koblizek M, Li YX, Liu YP, Feng FY, Ji JD, Jian JC, Wu ZH. Long PCR-RFLP of 16S-ITS-23S rRNA genes: a high-resolution molecular tool for bacterial genotyping. J Appl Microbiol. 2013;114(2):433–47.
Klindworth A, Pruesse E, Schweer T, Peplies J, Quast C, Horn M, Glockner FO. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. 2013;41(1): e1.
Wertheim HF, Nguyen HN, Taylor W, Lien TT, Ngo HT, Nguyen TQ, Nguyen BN, Nguyen HH, Nguyen HM, Nguyen CT, et al. Streptococcus suis, an important cause of adult bacterial meningitis in northern Vietnam. PLoS ONE. 2009;4(6): e5973.
Huong VT, Thanh LV, Phu VD, Trinh DT, Inui K, Tung N, Oanh NT, Trung NV, Hoa NT, Bryant JE, et al. Temporal and spatial association of Streptococcus suis infection in humans and porcine reproductive and respiratory syndrome outbreaks in pigs in northern Vietnam. Epidemiol Infect. 2016;144(1):35–44.
Wertheim HF, Nghia HD, Taylor W, Schultsz C. Streptococcus suis: an emerging human pathogen. Clin Infect Dis. 2009;48(5):617–25.
Goyette-Desjardins G, Auger JP, Xu J, Segura M, Gottschalk M. Streptococcus suis, an important pig pathogen and emerging zoonotic agent-an update on the worldwide distribution based on serotyping and sequence typing. Emerg Microbes Infect. 2014;3(6): e45.
Hasan MR, Sundararaju S, Tang P, Tsui KM, Lopez AP, Janahi M, Tan R, Tilley P. A metagenomics-based diagnostic approach for central nervous system infections in hospital acute care setting. Sci Rep. 2020;10(1):11194.
Stebner A, Ensser A, Geissdorfer W, Bozhkov Y, Lang R. Molecular diagnosis of polymicrobial brain abscesses with 16S-rDNA-based next-generation sequencing. Clin Microbiol Infect. 2021;27(1):76–82.
Morrell M, Fraser VJ, Kollef MH. Delaying the empiric treatment of candida bloodstream infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrob Agents Chemother. 2005;49(9):3640–5.
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–55.
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–44.
Desnos-Ollivier M, Patel S, Spaulding AR, Charlier C, Garcia-Hermoso D, Nielsen K, Dromer F. Mixed infections and In Vivo evolution in the human fungal pathogen Cryptococcus neoformans. mBio. 2010. https://doi.org/10.1128/mBio.00091-10.
Zhu X, Yan S, Yuan F, Wan S. The applications of Nanopore sequencing technology in pathogenic microorganism detection. Can J Infect Dis Med Microbiol. 2020;2020:6675206.
Santibanez P, Garcia-Garcia C, Portillo A, Santibanez S, Garcia-Alvarez L, de Toro M, Oteo JA. What does 16S rRNA gene-targeted next generation sequencing contribute to the study of infective endocarditis in heart-valve tissue? Pathogens. 2021. https://doi.org/10.3390/pathogens11010034.
Morsli M, Kerharo Q, Delerce J, Roche PH, Troude L, Drancourt M. Haemophilus influenzae meningitis direct diagnosis by metagenomic next-generation sequencing: a case report. Pathogens. 2021. https://doi.org/10.3390/pathogens10040461.
Acknowledgements
We thank all study subjects for their participation. The authors acknowledge the support of field workers.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the PAN-ASEAN Coalition for Epidemic and Outbreak Preparedness (PACE-UP; DAAD Project ID: 57592343) and the German Federal Ministry of Education and Research (BMBF01DP17047).
Author information
Authors and Affiliations
Contributions
TPV, LHS and SRP designed the study. LHS, NTT, DVD and TVS recruited patients and collected samples. LTKL, DVD, TVS, DTQ, NTT, PQH, JR, BTS and SRP performed the experiments and interpreted data. SRP wrote the first draft. TPV, DN, SB and CGM revised and finalized the manuscript. TPV, PGK and LHS contributed to materials and reagents. All authors agreed with the results and conclusions. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by Institutional Review Board of the 108 Military Central Hospital, Hanoi, Vietnam (108MCH/RES/MENTNGITIS-V-D3-25-04-2017). All experiments were performed following guidelines and regulations. Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors of this manuscript declare no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Nanopore R9.4.1 flow cell sequencing results generated from EPI2ME cloud analysis of complete fastq reads.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pallerla, S.R., Van Dong, D., Linh, L.T.K. et al. Diagnosis of pathogens causing bacterial meningitis using Nanopore sequencing in a resource-limited setting. Ann Clin Microbiol Antimicrob 21, 39 (2022). https://doi.org/10.1186/s12941-022-00530-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-022-00530-6