Abstract
Purpose
In this study, we aimed to evaluate the epidemiology and antimicrobial resistance (AMR) patterns of bacterial pathogens in COVID-19 patients and to compare the results with control groups from the pre-pandemic and pandemic era.
Methods
Microbiological database records of all the COVID-19 diagnosed patients in the Ege University Hospital between March 15, 2020, and June 15, 2020, evaluated retrospectively. Patients who acquired secondary bacterial infections (SBIs) and bacterial co-infections were analyzed. Etiology and AMR data of the bacterial infections were collected. Results were also compared to control groups from pre-pandemic and pandemic era data.
Results
In total, 4859 positive culture results from 3532 patients were analyzed. Fifty-two (3.59%) patients had 78 SBIs and 38 (2.62%) patients had 45 bacterial co-infections among 1447 COVID-19 patients. 22/85 (25.88%) patients died who had bacterial infections. The respiratory culture-positive sample rate was 39.02% among all culture-positive samples in the COVID-19 group. There was a significant decrease in extended-spectrum beta-lactamase (ESBL)-producing Enterobacterales (8.94%) compared to samples from the pre-pandemic (20.76%) and pandemic era (20.74%) (p = 0.001 for both comparisons). Interestingly, Acinetobacter baumannii was the main pathogen in the respiratory infections of COVID-19 patients (9.76%) and the rate was significantly higher than pre-pandemic (3.49%, p < 0.002) and pandemic era control groups (3.11%, p < 0.001).
Conclusion
Due to the low frequency of SBIs reported during the ongoing pandemic, a more careful and targeted antimicrobial prescription should be taken. While patients with COVID-19 had lower levels of ESBL-producing Enterobacterales, the frequency of multidrug-resistant (MDR) A. baumannii is higher.
Similar content being viewed by others
Introduction
Antimicrobial Resistance (AMR) is recognized as a public threat with constantly increasing urgency [1]. It is estimated that by the year 2050, 10 million deaths and an economic loss of $100 billion would be expected annually due to multidrug-resistant (MDR) (resistant to more than three or more antimicrobial categories) infections [2]. It is widely accepted that antimicrobial surveillance is crucial for tackling AMR globally [3]. The current pandemic, a consequence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is associated with high mortality, morbidity, and healthcare-related costs [4]. Recent data shows that more than 175 million people have so far been infected and 3.7 million of them died [5]. Secondary bacterial infections (SBIs) result in higher mortality rates in patients with COVID-19 [6]. As previously reported in recent pandemics [7, 8], viral infections can also promote the development of bacterial invasive respiratory infections by impairing the immune response, enhancing the destruction of cells and tissue.
In the pandemic era, deaths and hospitalizations have been reported across all age groups, with a higher frequency in the elderly (> 60 years) patients [9]. SBIs have previously been reported in patients with COVID-19 [6, 10, 11]. It was recently shown that SBIs were observed in 15% of COVID-19 patients, while the SBIs were associated with 50% of all deaths [12]. Therefore, it is crucial to consider SBIs in order to improve the outcome of COVID-19. Consequently, patients with COVID-19 are treated with prophylactic broad-spectrum antibiotics in order to prevent and treat possible SBIs [13,14,15,16]. Recently, other approaches including phage therapeutics have been suggested as possible non-antibiotic treatment options [17].
Hygiene procedures such as hand hygiene, usage of disinfectants, personal protective equipment (PPE) are significantly changed due to the COVID-19 pandemic [18].
In environments where personnel and personal protective equipment (PPE) are insufficient, hygienic conditions may deteriorate, as well as increased use of PPE in interventions may prevent the increase of SBIs and the spread of common resistant bacterial strains. A previous study from Italy has suggested that lack of PPE, and lack of healthcare professionals associated with increased risk of spreading the carbapenem-resistant Klebsiella pneumoniae in the intensive care units (ICUs) [19].
It is important to evaluate the etiology and resistance patterns of SBIs as well as to compare the data with other patients before and during the pandemic. There is scarce data on SBI etiology and antimicrobial susceptibility data [10, 16]. However, hitherto published studies have not analyzed the changes in AMR in patients with COVID-19 and controls. In addition, there is no published data from developing countries on SBIs where high AMR is prevalent. The data is crucial for establishing effective antibiotic therapy as well as avoiding unnecessary treatment [20].
In this study, we aimed to evaluate the etiologies of SBIs and co-infections and AMR profiles of the bacterial pathogens causing these infections in patients with COVID-19. Also, our secondary aim was to reveal the differences in the AMR between patients with COVID-19 and other patients from the pre-pandemic and pandemic era.
Methods
Study design
This study was performed at Ege University Hospital, Izmir, with a total of 2426 patient beds. The study covers the data between December 15, 2019, and June 15, 2020, which can be considered as the preceding three months, and the first three months of the COVID-19 pandemic in Turkey.
Study population
COVID-19 group
During the pandemic peak for SARS-CoV-2, real-time reverse transcription PCR (RT-PCR) assay positive and negative patients with symptoms consistent with COVID-19 were included. The RT-PCR assay negative patients had radiological imaging findings meeting the Ministry of Health's probable case [21] criteria for COVID-19 and therefore were included in the COVID-19 patient group (Additional file 2). SBIs are defined as infections occurring two days or more after patients were admitted to the hospital. Infections occurring not more than two days of hospitalization were defined as co-infections.
Control group
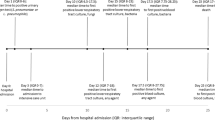
This study included two control groups, i.e., one pre-pandemic era group with clinical microbiology culture results registered between December 15, 2019–March 15, 2020, and one pandemic era group with microbiology culture results registered between March 15, 2020–June 15, 2020, with no clinical and/or laboratory diagnosis of COVID-19 (Fig. 1).
Laboratory methods
Bacterial culture
The investigation of bacterial pathogens in clinical samples was conducted with standard procedures as requested by the attending physician and was evaluated by microbiologists (Additional file 1). Identification and antimicrobial susceptibility testing of the isolates were performed using MALDI-TOF MS (Matrix-Assisted Laser Desorption/Ionization-Time of Flight Mass Spectrometry) (BioMérieux, France) and VITEK 2 (BioMérieux, France) automated systems, respectively. For viridans group streptococci, Haemophilus spp., Corynebacterium striatum, Streptococcus pneumoniae, and Stenotrophomonas maltophilia, the international Kirby Bauer disk diffusion method was used. All the susceptibility results were evaluated in accordance with the EUCAST criteria [22]. When imipenem or meropenem resistance was detected in Enterobacterales strains with the automated system, the result was confirmed by gradient test (BioMérieux, France). Antibiotic MIC values were confirmed by gradient test when isolates were determined resistant to vancomycin, teicoplanin, linezolid, tigecycline with VITEK 2 automated system. The VITEK 2 cefoxitin screen test was used to detect MRSA strains. Only one isolate per patient was studied.
SARS-CoV-2 RT-PCR
For PCR tests, DirectDetect™ SARS-CoV-2 Detection Kit (Coyote Bioscience Co, China) and Bio-Speedy SARS-COV2 (2019-nCoV) qPCR Detection Kit (Bioeksen R&D Technologies Ltd, Turkey) was used and according to the manufacturers’ recommendations. The PCR tests were performed with Qiagen Rotorgene Q-5 Plex-HRM Thermal Cycler (Qiagen, Belgium).
Data collection
Blood, respiratory tract, urinary tract, and other samples such as gastrointestinal tract, tissue, normally sterile fluids cultures sent from patients were evaluated and susceptibility test results were collected from the microbiology laboratory database.
Statistical analysis
Statistical analyses were performed using Microsoft Excel 2016 and IBM SPSS Statistics Version 18.0 (IBM Corp, Armonk, NY). Cross tables were created for categorical variables and chi-square analysis was performed. Categorical variables were shown as numbers and %, numerical variables as median (min., max.). A. baumannii changes between different groups were analyzed with two-tailed Fisher's exact test. Other comparisons (e.g., etiological changes, multidrug-resistant bacteria changes) were done with two-tailed Pearson's chi-squared test. A p value < 0.05 was considered statistically significant.
Ethical approval
This study has been approved by the Ege University Medical Research Ethics Committee (20–9T/75) and Turkish Ministry of Health.
Results
In total, 4859 culture-positive samples from 3532 patients were studied. The samples were collected between December 15, 2019, and June 15, 2020. The pre-pandemic era control group consists of 3034 samples from 2143 patients and the pandemic era control group included 1702 samples from 1304 patients. 1447 COVID-19 diagnosed patients’ data were evaluated separately, and 85 of them had 123 bacterial infections.
Of the 2143 patients in the pre-pandemic group, 1057 (49.32%) were female, 1086 (50.68%) were male, and the median age of these patients was 52 (0–99 years). Of the 1304 patients in the pandemic group, 630 (48.31%) were female, 674 (51.69%) were male, and the median age of these patients was 55 (0–100 years). 85 patients evaluated as COVID-19 patients, 45 (52.94%) were female and 40 (47.06%) were male and the median age of the patients was 61 (9 months-99 years). The mortality rate was 25.88% in COVID-19 patients who had been diagnosed with bacterial infections and 64 (38–96 years) was the median age among deaths.
Pre-pandemic control group
During the three months before the pandemic (December 15, 2019–March 15, 2020), microbiological data from 2143 patients were evaluated, and 3034 culture-positive samples were detected. Strains were mostly isolated from urine (1472, 48.52%), respiratory tract samples (e.g., sputum, bronchoalveolar lavage) (540, 17.32%), and blood samples (442, 14.57%). Other isolated samples came from different tissue samples such as wound swabs and sterile body fluids (455, 14.9%), stool (96, 3.1%), cerebrospinal fluid (29, 0.9%). The most common strains were Escherichia coli (766, 23.55%), K. pneumoniae (324, 11.56%), and Pseudomonas aeruginosa (254, 8.37%) (Fig. 2.). Extended-spectrum beta-lactamase ESBL-producing Enterobacterales were the most common (630, 20.76%) MDR bacteria among the strains isolated from these samples.
Pandemic era control group
Microbiological data from 1304 patients were evaluated and 1702 culture-positive samples were included in the pandemic era control group. Strains were obtained from urine (796, 46.77%), blood (276, 16.22%), lower respiratory tract samples (261, 15.33%), and others (e.g., feces, tissue, and sterile fluid). The most common isolated strains were E. coli (447, 26.26%), K. pneumoniae (197, 11.57%), and P. aeruginosa (136, 7.99%) (Table 1). ESBL-producing Enterobacterales were the most common (353, 20.74%) type of MDR strain, followed by carbapenem-resistant Enterobacterales (CRE) (62, 3.64%).
COVID-19 patients
The existence of bacterial infections in 1447 COVID-19 patients (both inpatient and outpatient) were evaluated. In total, 52/1447 (3.59%) patients had SBIs and 38/1447 (2.62%) had bacterial co-infections. Bacterial isolates were detected in 123 clinical samples. A secondary bacterial infection developed in five patients with bacterial co-infection during their follow-up. 28 (32.94%) patients had multiple bacterial, and 57 (67.05%) patients had mono-bacterial infections. The most common MDR organisms were ESBL-producing Enterobacterales (11, 8.94%) (Fig. 3).
In total, 78/123 (63.41%) bacterial strains were obtained two days after hospitalization of the patients and described as hospital-acquired infections while 45/123 (36.59%) were community-acquired infections. The most common bacteria was A. baumannii (10, 9.76%) among all respiratory tract samples (Table 2).
Discussion
Viral respiratory infections have been associated with an increased risk of bacterial infections. During the 2009 H1N1 outbreak, within 72 h of intensive care unit (ICU) admission, 30.3% of cases had bacterial co-infection [23]. Pandemics and seasonal flu data suggest that bacterial infections can worsen viral diseases and causes severe outcomes. Patients receiving invasive mechanical ventilation in other SARS and MERS epidemics developed secondary infections and had higher mortality [24].
In the present study, 2.62% of patients with COVID-19 had bacterial co-infections whereas 3.59% of them had secondary bacterial infections. In total, 22/85 (25.88%) COVID-19 patients with bacterial infections died. Recent studies from Turkey showed that the overall mortality rate in patients with COVID-19 is 4.5% [25, 26]. Therefore, it is reasonable to suggest that bacterial infections are related to higher mortality rates in patients with COVID-19. UTI was the most common infection type (45.5%) and followed by RTI (39.02%) which was significantly higher than the two control groups. Previous studies analysing SBIs in patients with COVID-19 are contradictory. He et al. showed that 50% of the patients with COVID-19 had a SBI or carried bacterial pathogens [27]. However, in a recent meta-analysis, it was reported that the SBI rate in COVID-19 patients was between 4.7 and 19.5% and was associated with an increased risk of severe course or fatal outcomes [28, 29]. The underlying reason for low bacterial infection rates in the present study is not known. It might be related to several factors including the severity of the disease in patients included prior antimicrobial therapy or stringent local hygiene protocols applied during the pandemic era [30]. The observation of 3.59% of SBI suggests that empiric antibiotic treatment may not be necessary for all COVID-19 patients, since proven bacterial infections are relatively rare.
The most common pathogens in the COVID-19 study group were E. coli (22, 17.89%), K. pneumonieae (15, 12.2%), A. baumannii (12, 9.76%), and S. aureus (11, 8.94%). Detection of E. coli (22, 17.89%) was significantly lower in patients with COVID-19, compared to the pandemic era control group (447, 26.26%) (p = 0.04). In contrast, detection of A. baumannii in patients with COVID-19 was higher than in the two control groups.
In lower respiratory tract infections, the most detected pathogens were Gram-negative bacteria (32, 66.66%), following by Gram-positive bacteria (16, 33.33%). In Gram-negative bacteria, the most common isolated strains were A. baumannii (10/32, 31.25%), followed by P. aeruginosa (5/32, 15.63%). Among Gram-positive bacteria, S. aureus (7/16, 43.75%) was the most common isolated strain. Although the distribution of Gram-negative and Gram-positive bacteria were similar, a higher A. baumannii occurrence as observed in our COVID-19 study group and needs further evaluation with comprehensive clinical data. A recent study from China showed that the most common bacterial pathogens isolated from respiratory tract samples were Gram-negative bacteria (26, 65%), following by Gram-positive bacteria (14, 34.99%). In that study, the most common bacterial pathogens encompassed K. pneumoniae (n = 11), E. faecium (n = 9), followed by A. baumannii (n = 8) [6]. The underlying reason for discrepant results between the present study and the previous report might be associated with differences in colonisation of bacteria types between centers, patients’ clinical profile as well as administration of prophylactic antibiotics.
ESBL-producing Enterobacterales were significantly lower in COVID-19 compared to pre-pandemic (p = 0.001) and pandemic era control group (p = 0.002). In a recent study which is reported from Egypt, Gram-negative isolates were mostly ESBL- or carbapenemase-producers which differs from our study [31]. The distinction may be due to the difference in the drug resistance profile between countries and/or local hygiene measures taken for patients with COVID-19. MDR A. baumannii was the most common bacteria (9.76%) in respiratory tract samples (39.02%) from COVID-19 patients, and this rate was significantly higher than that in the pre-pandemic (3.49%) (p = 0.002) and pandemic (3.11%) (p = 0.001) era control groups. In another study from New Jersey, when COVID-19 cases surge, increased carbapenem-resistant A. baumannii (CRAB) counts were reported. CRABs were mostly observed among COVID-19 patients admitted to ICUs and receiving ventilation therapy [32]. In both cases, the increase in intervention needed for COVID-19 patients may have led to a deterioration in hygiene conditions and an increase in the spread of MDR A. baumannii.
The present study has some limitations. First, not all COVID-19 patients were confirmed by PCR to be SARS-CoV-2 positive, and the comprehensive clinical data and disease severity of these patients were not studied. Secondly, a limited number of patients were available in our single-center study. However, we followed the official guidelines for the diagnosis of COVID-19, and it is highly unlikely that the patients with typical COVID-19 radiological findings had other infections. The lack of clinical severity data might be important, but the study focuses on the description of the prevalence of microorganisms and AST results in patients with COVID-19 in general. In addition, the sample size covers a period of 3 months in the pandemic era. The study has the following strengths: First, unlike other studies, we compared both the prevalence of bacterial infections and antimicrobial resistance patterns in patients with COVID-19 and control groups. Also, this study is the first comparative study presented from Turkey which is a developing country with a general high MDR bacteria profile.
Conclusion
In conclusion, the present study shows that SBIs and bacterial coinfections were low in COVID-19 patients; but when present, it causes severe outcomes and is related to mortality. With these results, the administration of empirical broad spectrum antimicrobials to COVID-19 patients should be evaluated more carefully as the excessive use of antimicrobials could lead to a surge of antimicrobial resistance [33]. Also, while it was observed that COVID-19 patients had a lower risk of infected with ESBL-producing Enterobacterales; a significant increase in the MDR A. baumannii rates and increase of respiratory tract samples was observed and needs further evaluation. The present study will have an impact on diagnosis, possible treatments, and evaluating the existing sanitation measures in the hospitals. Further studies with larger sample size and detailed clinical data are warranted.
Availability of data and materials
Authors can confirm that all relevant data are included in the article and/or its additional information files.
References
Nieuwlaat R, Mbuagbaw L, Mertz D, Burrows LL, Bowdish DME, Moja L, et al. Coronavirus Disease 2019 and antimicrobial resistance: parallel and interacting health emergencies. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciaa773.
Neill JO’. Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations The Review on Antimicrobial Resistance Chaired. 2014.
Ahmad M, Khan AU. Global economic impact of antibiotic resistance: a review. J Glob Antimicrob Resist. 2019;19:313–6.
Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–12.
(OMS) WHO. COVID-19 Weekly Epidemiological Update. 2020;(November):1;4.
Zhang H, Zhang Y, Wu J, Li Y, Zhou X, Li X, et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020. https://doi.org/10.1080/22221751.2020.1812437.
Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol. 2017. https://doi.org/10.3389/fmicb.2017.01041.
Liderot K, Ahl M, Özenci V. Secondary bacterial infections in patients with seasonal influenza a and pandemic H1N1. Biomed Res Int. 2013. https://doi.org/10.1155/2013/376219.
Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–8.
Li J, Wang J, Yang Y, Cai P, Cao J, Cai X, et al. Etiology and antimicrobial resistance of secondary bacterial infections in patients hospitalized with COVID-19 in Wuhan, China: a retrospective analysis. Antimicrob Resist Infect Contr. 2020. https://doi.org/10.1186/s13756-020-00819-1.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. www.thelancet.com. 2020;395:497.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. www.thelancet.com. 2020. DOI: https://doi.org/10.1016/S0140-6736(20)30566-3.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020. https://doi.org/10.1016/S2213-2600(20)30079-5.
Rothe K, Feihl S, Schneider J, Wallnöfer F, Wurst M, Lukas M, et al. Rates of bacterial co-infections and antimicrobial use in COVID-19 patients: a retrospective cohort study in light of antibiotic stewardship. Eur J Clin Microbiol Infect Dis. 2020;40(4):859–69.
Sivapalan P, Sivapalan P, Ulrik CS, Bojesen RD, Lapperre TS, Eklöf JV, et al. Proactive Prophylaxis with Azithromycin and HydroxyChloroquine in Hospitalised Patients with COVID-19 (ProPAC-COVID): a structured summary of a study protocol for a randomised controlled trial. Trials. 2020;21(1):1–4.
Manohar P, Loh B, Nachimuthu R, Hua X, Welburn SC, Leptihn S. Secondary bacterial infections in patients with viral pneumonia. Front Med. 2020;7(August):2013–6.
Manohar P, Loh B, Athira S, Nachimuthu R, Hua X, Welburn SC, et al. Secondary bacterial infections during pulmonary viral disease: phage therapeutics as alternatives to antibiotics? Front Microbiol. 2020;11(June):1–11.
Metin N, Turan Ç, Utlu Z. Changes in dermatological complaints among healthcare professionals during the COVID-19 outbreak in Turkey. Acta Dermatovenerologica Alpina, Pannonica Adriat. 2020;29(3):115–22.
Tiri B, Sensi E, Marsiliani V, Cantarini M, Priante G, Vernelli C, et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J Clin Med. 2020;9(9):2744.
Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198(7):962–70.
The Republic of Turkey Ministry of Health. COVID-19 (SARS-COV-2 Infection) (Study of Scientific Board) General Information. Epidemiol Diagn. 2020;19(May):1–21.
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0. 2019;9.0:0–99.
Rice TW, Rubinson L, Uyeki TM, Vaughn FL, John BB, Miller RR, et al. Critical illness from pandemic influenza A virus and bacterial coinfection in the United States. Crit Care Med. 2009. https://doi.org/10.1097/CCM.0b013e3182416f23.
Yap FHY, Gomersall CD, Fung KSC, Ho PL, Ho OM, Lam PKN, et al. Increase in methicillin-resistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin Infect Dis. 2004. https://doi.org/10.1086/422641.
Durusoy R, Ata A, Geçim C, Filis N, Fidan E, Şimşek S, et al. The surveillance, exposure investigation and contact tracing of COVID-19 cases at Ege University Medical School’s Hospital. Türkiye Halk Sağlığı Derg. 2020;18:25–39.
Kokturk N, Babayigit C, Kul S, Duru P, Atis S. The predictors of COVID-19 mortality in a nationwide cohort of Turkish patients. Respir Med. 2021;183:106433.
He F, Xia X, Nie D, Yang H, Jiang Y, Huo X, et al. Respiratory bacterial pathogen spectrum among COVID-19 infected and non–COVID-19 virus infected pneumonia patients. Diagn Microbiol Infect Dis. 2020;98:4. https://doi.org/10.1016/j.diagmicrobio.2020.115199.
Vazzana N, Dipaola F, Ognibene S. Procalcitonin and secondary bacterial infections in COVID-19: association with disease severity and outcomes. Acta Clin Belg. 2020.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;10:5. https://doi.org/10.1016/j.cmi.2020.07.016.
Kodaz H. Successful treatment strategy of turkey against covid-19 outbreak. Eurasian J Med Oncol. 2020. https://doi.org/10.14744/ejmo.2020.12345.
Ramadan HKA, Mahmoud MA, Zakaria M, Elkhawaga AA, El-Mokhtar MA, et al. Predictors of severity and co-infection resistance profile in COVID-19 patients: First report from upper Egypt. Infect Drug Resist. 2020;13:3409–22.
Perez S, Innes GK, Walters MS, Mehr J, Arias J, Greeley R, et al. Increase in hospital-acquired carbapenem-resistant acinetobacter baumannii infection and colonization in an acute care hospital during a surge in COVID-19 Admissions — New Jersey, February–July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(48):1827.
Manohar P, Loh B, Leptihn S. Will the overuse of antibiotics during the coronavirus pandemic accelerate antimicrobial resistance of bacteria? Infect Microbes Dis. 2020;2(3):87–8.
Funding
Open access funding provided by Karolinska Institute. The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
ŞA and VÖ presented the main conceptual ideas. ŞA, VÖ, MYD, MK designed the study. MK, MYD performed the analyses, wrote the first draft, and revised with FÇ, AT, ŞA, VÖ. ŞA and VÖ supervised the findings of this work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Ege University Medical Research Ethics Committee (20 – 9T / 75) and Turkish Ministry of Health. Informed consent was waived by the Ethics Committee because of the retrospective nature of the study. The analysis was done with totally anonymous data.
Consent to publication
Not applicable.
Informed consent
This study was waived by the Ethics Committee because of the retrospective nature of the study. The analysis was done with totally anonymous data.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Media used and incubation times according to sample types.
Additional file 2.
Antimicrobial susceptibility patterns.
Additional file 3: Table S1.
Detailed information on microorganisms and focus of infection isolated from patients with COVID-19.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karataş, M., Yaşar-Duman, M., Tünger, A. et al. Secondary bacterial infections and antimicrobial resistance in COVID-19: comparative evaluation of pre-pandemic and pandemic-era, a retrospective single center study. Ann Clin Microbiol Antimicrob 20, 51 (2021). https://doi.org/10.1186/s12941-021-00454-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-021-00454-7