Abstract
Background
Mycobacterium goodii is an infrequent human pathogen which has been implicated in prosthesis related infections and penetrating injuries. It is often initially misidentified as a gram-positive rod by clinical microbiologic laboratories and should be considered in the differential diagnosis.
Case presentation
We describe here the second reported case of M. goodii endocarditis. Species level identification was performed by 16S rDNA (ribosomal deoxyribonucleic acid) gene sequencing. The patient was successfully treated with mitral valve replacement and a prolonged combination of ciprofloxacin and trimethoprim/sulfamethoxazole.
Conclusion
Confirmation of the diagnosis utilizing molecular techniques and drug susceptibility testing allowed for successful treatment of this prosthetic infection.
Similar content being viewed by others
Background
Mycobacterium goodii is a rapidly growing non-tuberculous mycobacterium (NTM) belonging to the Mycobacterium smegmatis [1] group. Its importance has become increasingly appreciated as a pathogen over the last 20 years, with a predilection towards infecting tissues at the site of penetrating injuries. Antibacterial treatment strategies against this pathogen are diverse but reported case cure rates are high. Here we describe what the authors believe to be the second reported case of M. goodii endocarditis ever reported (first time involving a ring annuloplasty).
Case presentation
A 67-year-old Caucasian man, retired financier, with a history of severe mitral regurgitation status post ring annuloplasty repair complicated by right sided hemothorax requiring two reoperations to achieve hemostasis, presented to an outside hospital 3 weeks postoperatively with fever, loss of appetite, and gait disturbance.
On examination the patient vital signs were normal, lungs were clear, a mild 1/6 systolic murmur was appreciated at the apex, and a drain was in place for a groin seroma related to recent left heart catheterization. He had an unsteady gait and exhibited mild left lower extremity weakness (4/5). His brain magnetic resonance imaging showed multiple ring-enhancing lesions in the pons and posterior fossa suggestive of septic emboli. Transthoracic echocardiography showed moderate mitral regurgitation without any vegetation. Blood cultures grew gram-positive rods suspicious for Actinomyces spp. and he was started on vancomycin and ampicillin/sulbactam. He developed a morbilliform cutaneous eruption felt to be related to the ampicillin and was switched to vancomycin/ceftriaxone. A computed tomography scan of the chest (Fig. 1) was done which showed bilateral infiltrates and mild pleural effusions.
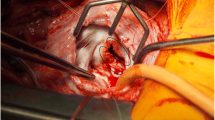
The patient was then transferred to our hospital on day 14 for further management. A transesophageal echocardiogram (TEE) (Fig. 2) showed vegetations on the P3 annulus and evidence of ring dehiscence in A2, A3, and P3 areas. He completed penicillin desensitization and was successfully narrowed to penicillin G to be optimally treated for presumptive actinomycotic endocarditis and both vancomycin and ceftriaxone were stopped. On hospital day 18 he underwent mitral valve replacement with a bioprosthetic valve (27 mm. St. Jude prosthesis). Intraoperatively, vegetations were confirmed on the mitral valve and tissue cultures from the explanted native mitral valve suggested a rapid growing mycobacterium rather than an Actinomyces spp. Empiric treatment with meropenem (1 g IV thrice a day)/amikacin (1 g IV per day)/clarithromycin (500 mg oral twice a day)/ciprofloxacin (400 mg IV twice a day) was initiated pending final confirmation and susceptibility testing. On day 21 it was confirmed that the gram-positive isolate was a 100% match to the M. goodii strain (American Type Culture Collection or ATCC #700504) using 16S sequencing (MicroSeq 500 bp 16S rDNA kit), but M. smegmatis could not be ruled out due to a high-level sequence homology [99.5% match to M. smegmatis type strain (ATCC 19420) with two mismatches]. Serial blood cultures sterilized on hospital day 26 and he was transferred to a nursing facility after repeat TEE showed a normally functioning prosthetic mitral valve.
On the day following discharge into the rehabilitation facility, the patient developed a maculopapular eruption involving his flanks and back, which progressed to involve his anterior trunk and all four limbs. He presented to the infectious diseases clinic 3 days after discharge where the rash was suspected of being related to the meropenem and tigecycline was substituted; however, he had an acute anaphylactoid reaction (involving dyspnea and hypotension) during the loading dose of tigecycline (100 mg once) which was subsequently replaced with linezolid (600 mg oral twice a day). His susceptibility reports returned which showed the mycobacterium was susceptible to trimethoprim–sulfamethoxazole, amikacin, doxycycline, ciprofloxacin, imipenem, linezolid and resistant to clarithromycin. In accordance, his regimen was changed to ciprofloxacin (500 mg oral twice a day)/trimethoprim–sulfamethoxazole (1 DS tablet oral twice a day).
The patient was ultimately treated with a total of 6 months of therapy. He followed up in infectious diseases clinic on days 61 and 135 and was contacted by phone 137 weeks post valve replacement and there were no complaints or signs of intervening relapse, was highly active and back to all his prior recreational activities.
Discussion
A broad literature search was done from PubMed, Scopus and OvidSP databases containing the search terms M. goodii to try and identify all human infections with this organism. M. goodii was proposed as a new rapidly growing species related to M. smegmatis based on gene sequencing work by Brown et al. [1] in 1999 in continuation to the work done by Wallace et al. [2]. We have summarized to the best of our knowledge all the published reports about M. goodii infections (Table 1) after Brown [1]. A total of 45 cases (including our patient) have been reported to date. Eleven (25%) cases were wound/bone infections due to trauma. Twenty-two (49%) cases were iatrogenic, with eighteen (38%) involving infection of prosthetic materials. Eight (18%) cases were pulmonary, which were strongly associated with histological findings of lipoid or granulomatous pneumonias. Four (9%) cases had unclear clinical diagnosis but were confirmed to be M. goodii microbiologically.
Since there is no available clinical trial or prospective data to guide therapy for this infection, we extrapolated a treatment approach from the accumulated experience with other more common rapid growing NTM species to treat our patient with this incredibly rare disease. Our empiric regimen selection was further made challenging by the development of a second drug eruption and an anaphylactoid infusional reaction, both of which required cessation of drugs and subsequent drug substitution.
Conclusions
Rapid growing mycobacteria should be suspected in trauma or prosthetic related infections not responding to initial empiric therapies. Molecular techniques are rapid and reliable for confirmation of rapid growing mycobacterial infections and are recommended by the Infectious Diseases Society of America guidelines [3]. Once rapid growing mycobacteria are suspected, 16S ribosomal sequencing should be used if available for species level identification. 16S rRNA gene sequences contain hypervariable regions that can provide species-specific signature sequences useful for identification of bacteria [4]. Since M. goodii has the ability to form biofilms [5], prosthesis removal is indicated to achieve cure if feasible. Macrolides should not be included in the empirical/definitive treatment since it has been shown that the organism has intrinsic macrolide resistance conferred by novel rRNA methylase genes erm(38) and erm(39) [6, 7]. This has also been seen widely in the susceptibility testing for the organism. The organism is usually susceptible to sulfonamides, amikacin, doxycycline, imipenem, fluoroquinolones and they should be optimized for dose and duration according to the severity and comorbidities.
Abbreviations
- ATCC:
-
American Type Culture Collection
- rDNA:
-
ribosomal deoxyribonucleic acid
- TEE:
-
transesophageal echocardiogram
References
Brown BA, Springer B, Steingrube VA, Wilson RW, Pfyffer GE, Garcia MJ, Menendez MC, Rodriguez-Salgado B, Jost KC Jr, Chiu SH, et al. Mycobacterium wolinskyi sp. nov. and Mycobacterium goodii sp. nov., two new rapidly growing species related to Mycobacterium smegmatis and associated with human wound infections: a cooperative study from the International Working Group on Mycobacterial Taxonomy. Int J Syst Bacteriol. 1999;49(Pt 4):1493–511.
Wallace RJ, Nash DR, Tsukamura M, Blacklock ZM, Silcox VA. Human disease due to Mycobacterium smegmatis. J Infect Dis. 1988;158(1):52–9.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416.
Kolbert CP, Persing DH. Ribosomal DNA sequencing as a tool for identification of bacterial pathogens. Curr Opin Microbiol. 1999;2(3):299–305.
Esteban J, Martin-de-Hijas NZ, Kinnari TJ, Ayala G, Fernandez-Roblas R, Gadea I. Biofilm development by potentially pathogenic non-pigmented rapidly growing mycobacteria. BMC Microbiol. 2008;8:184.
Nash KA, Andini N, Zhang Y, Brown-Elliott BA, Wallace RJ Jr. Intrinsic macrolide resistance in rapidly growing mycobacteria. Antimicrob Agents Chemother. 2006;50(10):3476–8.
Nash KA. Intrinsic macrolide resistance in Mycobacterium smegmatis is conferred by a novel erm gene, erm(38). Antimicrob Agents Chemother. 2003;47(10):3053–60.
Jonsson G, Rydberg J, Sturegard E, Christensson B. A case of Mycobacterium goodii prosthetic valve endocarditis in a non-immunocompromised patient: use of 16S rDNA analysis for rapid diagnosis. BMC Infect Dis. 2012;12:301.
Marchandin H, Battistella P, Calvet B, Darbas H, Frapier JM, Jean-Pierre H, Parer S, Jumas-Bilak E, Van de Perre P, Godreuil S. Pacemaker surgical site infection caused by Mycobacterium goodii. J Med Microbiol. 2009;58(Pt 4):517–20.
Chrissoheris MP, Kadakia H, Marieb M, Libertin C. Pacemaker pocket infection due to Mycobacterium goodii: case report and review of the literature. Conn Med. 2008;72(2):75–7.
Toda H, Sato K, Iimori M, Yamazumi T, Furuta I, Satoh A, Katsukawa C. A case of Mycobacterium goodii infection wifh isolation from blood and a pacemaker lead. Kansenshogaku Zasshi. 2006;80(3):262–6.
Yoo DK, Hosseini-Moghaddam SM. Pacemaker pocket infection due to Mycobacterium goodii, a rapidly growing mycobacteria. BMJ Case Reports. 2017. doi:10.1136/bcr-2016-218323
Uche C, Silibovsky R, Jungkind D, Measley R. Ventriculoperitoneal shunt-associated Mycobacterium goodii infection. Infect Dis Clin Pract. 2008;16(2):129–30.
Sohail MR, Smilack JD. Hernia repair mesh-associated Mycobacterium goodii infection. J Clin Microbiol. 2004;42(6):2858–60.
Ferguson DD, Gershman K, Jensen B, Arduino MJ, Yakrus MA, Cooksey RC, Srinivasan A. Mycobacterium goodii infections associated with surgical implants at Colorado hospital. Emerg Infect Dis. 2004;10(10):1868–71.
Hougas JE, Bruneteau RJ, Varman M. Mycobacterium goodii infection of skin graft in an immunocompetent child. Infect Dis Clin Pract. 2011;19(2):146–7.
Ahmad S, Khakoo RA. Left knee prosthesis-related Mycobacterium goodii infection. Int J Infect Dis. 2010;14(12):e1115–6.
Friedman ND, Sexton DJ. Bursitis due to Mycobacterium goodii, a recently described, rapidly growing mycobacterium. J Clin Microbiol. 2001;39(1):404–5.
Spencer TS, Teske MP, Bernstein PS. Postcataract endophthalmitis caused by Mycobacterium goodii. J Cataract Refract Surg. 2005;31(6):1252–3.
Martinez-Gonzalez D, Franco J, Navarro-Ortega D, Munoz C, Marti-Obiol R, Borras-Salvador R. Achalasia and Mycobacterium goodii pulmonary infection. Pediatr Infect Dis J. 2011;30(5):447–8.
Buijtels PC, Petit PL, Verbrugh HA, van Belkum A, van Soolingen D. Isolation of nontuberculous mycobacteria in Zambia: eight case reports. J Clin Microbiol. 2005;43(12):6020–6.
Authors’ contributions
RP authored the main text and conducted the literature review. MG was the consultant physician, oversaw the management of this patient and edited/revised several versions of the case report and literature review. Both the authors read and approved the final manuscript.
Acknowledgements
We thank David Ryan Peaper for providing the details about the bacterial identification process and Dr. Elise M Meoli for providing the transesophageal echocardiography images.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The production of this manuscript did not involve the production of any data sets.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Consent for publication
The patient in the case report provided both verbal and written consent to access his entire medical record as well as verbally consented to publishing his case in a de-identified manner.
Ethics approval and consent to participate
The study contains exclusively de-identified patient data from a single case report and a retrospective review of previously published human cases, therefore poses no hazard directly or indirectly to any living persons and is exempt from ethics approval.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Parikh, R.B., Grant, M. Mycobacterium goodii endocarditis following mitral valve ring annuloplasty. Ann Clin Microbiol Antimicrob 16, 14 (2017). https://doi.org/10.1186/s12941-017-0190-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-017-0190-4