Abstract
Background
The adverse effect of air pollution on mortality is well documented worldwide but the identification of more vulnerable populations at higher risk of death is still limited. The aim of this study was to evaluate the association between natural mortality (overall and cause-specific) and short-term exposure to five air pollutants (PM2.5, PM10, NO2, O3 and black carbon) and identify potential vulnerable populations in Belgium.
Methods
We used a time-stratified case-crossover design with conditional logistic regressions to assess the relationship between mortality and air pollution in the nine largest Belgian agglomerations. Then, we performed a random-effect meta-analysis of the pooled results and described the global air pollution-mortality association. We carried out stratified analyses by individual characteristics (sex, age, employment, hospitalization days and chronic preexisting health conditions), living environment (levels of population density, built-up areas) and season of death to identify effect modifiers of the association.
Results
The study included 304,754 natural deaths registered between 2010 and 2015. We found percentage increases for overall natural mortality associated with 10 μg/m3 increases of air pollution levels of 0.6% (95% CI: 0.2%, 1.0%) for PM2.5, 0.4% (0.1%, 0.8%) for PM10, 0.5% (-0.2%, 1.1%) for O3, 1.0% (0.3%, 1.7%) for NO2 and 7.1% (-0.1%, 14.8%) for black carbon. There was also evidence for increases of cardiovascular and respiratory mortality. We did not find effect modification by individual characteristics (sex, age, employment, hospitalization days). However, this study suggested differences in risk of death for people with preexisting conditions (thrombosis, cardiovascular diseases, asthma, diabetes and thyroid affections), season of death (May–September vs October–April) and levels of built-up area in the neighborhood (for NO2).
Conclusions
This work provided evidence for the adverse health effects of air pollution and contributed to the identification of specific population groups. These findings can help to better define public-health interventions and prevention strategies.
Similar content being viewed by others
Background
Air pollution is one of the largest environmental risks to health. According to the World Health Organization, ambient (outdoor) air pollution caused worldwide 4.2 million premature deaths in 2019.
A meta-analysis performed by Orellano et al. [1] reported positive associations between all-cause mortality and short-term exposure to particulate matter with aerodynamic diameters less or equal than 2.5 μm and 10 μm (PM2.5, PM10) with relative risks (RR) of, respectively, 1.0065 (95% confidence interval (CI): 1.0044, 1.0086) and 1.0041 (95% CI: 1.0034, 1.0049) for an interquartile range increase in pollutant concentration. Increases in nitrogen dioxide (NO2) (RR: 1.0072, 95% CI: 1.0059, 1.0085) and ozone (O3) (RR: 1.0043, 95% CI: 1.0034, 1.0052) also increased all-cause mortality risk.
PM2.5 is composed of different constituents, among which black carbon (BC). BC as other fine particles can easily pass into the blood stream or enter the respiratory system, leading to adverse health effects. While the adverse effects of PM2.5 are well documented, less is known about the effects of BC [2]. In 2019, Yang et al. carried out a meta-analysis of the association between fine PM constituents, including BC, and all-cause, cardiovascular and respiratory mortality. Significant associations between all-cause mortality as well as cardiovascular mortality and BC were observed but the meta-analysis was based on no more than four studies [3]. Another recent meta-analysis highlighted the need for more studies considering BC as a separate pollutant of PM2.5 [2].
The impact of air pollution on health is documented by studies carried out all over the world [4,5,6]. However, air pollutants levels highly vary across the regions of the world [7]. Belgium is a small but highly urbanized and industrialized country with a high population density and a dense traffic network [8] in which levels of air pollution above the WHO guidelines are frequently recorded [9, 10]. It is of interest to conduct studies in European countries, because the results of North American or Chinese studies may not be applicable to densely populated countries in Europe, such as Belgium.
Individual or environmental factors can play an important role in modifying the association between air pollution and mortality. However, basic characteristics such as age, sex or socioeconomic status are often the only studied factors [11, 12]. Some studies suggested that health effects can be more severe for people with pre-existing medical conditions. For instance, Bateson and Schwartz found that persons with a history of myocardial infarction as well as those with diabetes had a higher risk of death when exposed to PM10 concentrations [13]. In 2016, Alessandrini et al. found increases in natural mortality from PM exposure among people with diabetes and cardiac disorders [14]. However, a recent review conducted by Abed Al Ahad et al. [11] highlighted the lack of studies and a need for further research on individual factors such as pre-existing disease conditions to elucidate their role in the modification of the association between air pollution and mortality, which leads to populations with higher vulnerability to air-pollution.
To fill these gaps, we carried out a multi-city case-crossover analysis at individual level to investigate the impact of short-term exposure to air pollution (PM2.5, PM10, NO2, O3 and BC) on daily natural (overall and cause-specific) mortality in nine Belgian agglomerations. The association was estimated for each pollutant in each of the nine agglomerations. Then, the agglomeration-specific estimates were pooled using a random-effect meta-analysis [15] to describe the global association between each air pollutant and mortality. Finally, we used stratified analyses to assess the potential effect modification of this association by individual characteristics (sex, age, employment hospitalization days and chronic preexisting health conditions), living environment (levels of population density, built-up areas) and season of death.
Methods
Study area and population
The study area includes the nine largest Belgian municipalities and their agglomerations [16] representing 52.9% of the total Belgian population (11,209,044 inhabitants in 2015) (Table S1). People were included in the study if they were residing in the study area at the time of death and died from natural causes between January 1st, 2010 and December 31st, 2015 [17].
Mortality and environmental data
The International Classification of Diseases (10th revision) was used to characterize natural mortality (A00-R99) and cause-specific mortality from cardiovascular diseases (I10-I70), including ischemic heart diseases (IHD) (I20-I25) and cerebrovascular diseases (I60-I69), respiratory diseases (J00-J99) including chronic obstructive pulmonary diseases (COPD) (J40-J44, J47). The date of death, sex, age (5-year age groups), and cause of death were provided by Statbel, the Belgian statistical office.
Environmental exposures were assessed at the geographical coordinates of the residence at the time of death. Daily mean concentrations (in µg/m3) of air pollutants (PM2.5 (including BC), PM10 (including PM2.5 and BC), NO2, O3 and BC) were provided by the Belgian Interregional Environment Agency and estimated by RIO-IFDM models with 100 m spatial resolution [18]. The RIO-IFDM model consists of the RIO background model at 4 km × 4 km, which is a land use regression model interpolating concentration measurements, combined with the IFDM bi-Gaussian dispersion model which calculates the dispersion of road traffic, shipping traffic and large industrial point sources. Other sources such as residential heating or agricultural emissions are included in the RIO background model through the measurements. Finally, we also obtained information on daily mean temperature and relative humidity by the Royal Meteorological Institute of Belgium [17, 19].
Additional data for subgroups analyses
We used indicators of “pseudopathologies” (thrombosis, cardiovascular diseases (CVD), COPD, asthma, diabetes, psychoses, and thyroid affections), based on reimbursed medication dispensed in pharmacies (except those dispensed in hospital settings and some nursing homes) as proxy to determine the presence of preexisting chronic diseases in people. Data on reimbursed medication were obtained from the InterMutualistic Agency (IMA), an organization which hosts exhaustive data from the mandatory Belgian health insurance. People were considered as having a specific pseudopathology if they had received prescriptions for more than 90 defined daily doses (DDD) of drugs belonging to specific anatomical therapeutic chemicals (ATC) categories (WHO Collaborating Centre for Drug Statistics Methodology) in the 12 months preceding death. Since DDD are defined for adults, we only considered subjects older than 20 years (Table S2). From IMA databases, we also obtained information on hospitalization days (cumulative total above 120 days in the year preceding death) and employment of people (yes/no) at the end of the calendar year preceding death.
Individual (pseudonymized) data were linked using the Belgian national register number, which allows to identify all the Belgian residents.
Finally, we obtained the population density of the census tract of residence from Statbel and we defined an indicator of built-up area calculated as the percentage of non-vegetated surface for a 1-km buffer around the residence (MODIS/Terra Vegetation Continuous Fields, 250 m spatial resolution) [20].
Statistical analyses
A time-stratified case-crossover design was used to assess the association between mortality and each air pollutant, separately. This design was proposed by Maclure et al. to assess the effect of a transient exposure on acute health outcomes [21]. This design has the advantage of controlling for variables which do not vary on a short time (sex, age or socioeconomic status for instance). In such a design, a case day is defined by the date of death and control days are defined in a short period before or after the case days. In a time-stratified approach, control days are selected from the same day of the week, month and year as the case day [22], controlling for seasonality and time trends.
Association between air pollutants and mortality
We followed a two-stage approach: first using conditional logistic regressions, we assessed the association between air pollutants and mortality in the nine agglomerations. To determine an appropriate lag time between exposure and the outcome for each pollutant, we compared a variety of single and cumulated lag days, up to 15 days, using the distributed lag linear models (DLM) proposed by Gasparrini et al. [23]. The lag which yielded the minimal summed Akaike Information Criterion (AIC) over the nine agglomerations was selected for the analyses [23]. To control for potential confounding, we adjusted in the conditional logistic regressions for daily mean temperature and relative humidity with 0–3 days moving averages using natural cubic splines with 3 degrees of freedom (df).
In a second step, a random-effect meta-analysis [15] was performed to pool the agglomeration-specific estimates and describe the global association between each air pollutant and mortality. Cochran’s Q test and the I-squared statistics were used to examine the between agglomeration heterogeneity.
Odds ratios resulting from the logistic regressions were converted into percentage changes for ease of interpretation.
Additionally, using the model specification aforementioned, we introduced air pollutants with a natural cubic spline function with 3 df (using distributed lag non-linear models [23]) to visualize and detect possible departure from linearity of the air pollutants-mortality relationships.
The packages survival, dlnm and mvmeta of the R software (R Foundation for Statistical Computing, Vienna, Austria) were used to perform the analyses.
Subgroups analyses and effect modification
To detect potential effect modification of the association between air pollutants and all-cause mortality, stratified analyses were carried out for individual characteristics (sex, age, employment status, hospitalization days, pseudopathologies), environmental variables (population density, built-up area) and season of death (May–September vs October–April)).
Effect modification was evaluated using the Z-test and comparing Z to the standard normal distribution [24]:
β1 and β2 are the effect estimates in two subgroups, SE(β1) and SE(β2) their respective standard errors.
Sensitivity analyses
To examine the robustness of our findings, we conducted several sensitivity analyses. First, we performed two-pollutant models by simultaneously introducing in the models pollutants that are not highly correlated (Pearson’s correlation coefficient < 0.8). Second, for each pollutant, instead of the lags minimizing the AICs, we performed analyses considering cumulated lags 1) 0 to 1 days and 2) 0 to 5 days. Finally, for meteorological variables (mean temperature and relative humidity), we 1) controlled 0–1 days moving averages instead of 0–3 days, 2) varied the df values of the natural cubic splines from 3 to 6.
Results
Between 2010 and 2015, 307,859 natural deaths were registered in the study area of which 307,490 geocoding of the address were possible. People geocoded with less precision (extrapolation of the street number) or people living < 200 m from a tunnel exit were excluded from the analyses (N = 2,736). The latter showed unrealistically high values of exposure. The population hence includes 304,754 people and IMA information was available for 300,492 of them. Deaths from cardiovascular and respiratory causes represented 29.7% and 11.2% of cases, respectively (Table 1).
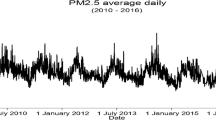
The average daily concentrations for PM2.5, PM10, O3, NO2 and BC were 15.3 µg/m3 (sd: 11.9), 22.2 µg/m3 (sd: 13.4), 39.3 µg/m3 (sd: 19.4), 25.8 µg/m3 (sd: 13.2) and 1.6 µg/m3 (sd: 1.1) respectively. There were no large differences in concentrations between agglomerations (< 10 µg/m3) except for one agglomeration (Antwerp) showing higher levels of NO2 concentrations (Table S3). Pollutant concentrations were similar in subgroups of populations stratified by individual characteristics and pseudopathologies (Table S4). There were, however, higher levels of PM2.5, PM10, NO2 and BC and lower levels of O3 concentrations in densely populated and highly built up areas as well as during the cold season (Table S4).
The pooled associations between air pollutants and mortality for PM, NO2 and BC showed no between agglomeration heterogeneity (I-squared range: 0.01%-18.2%, Cochran Q-test p-values range: 0.18–0.77) and moderate heterogeneity for O3 (I-squared: 48.9%, Cochran Q-test p-value: 0.001) (Table S5). We did not observe strong departure from linearity when modeling air pollutants-mortality curves with natural cubic spline functions (Fig. 1, Figure S1-S5) and thus modeled air pollutants as linear variables in further analyses. For PM, O3 and NO2, no obvious thresholds were observed, indicating positive linear associations. For BC, an increase in risk appeared at high concentrations (> 4 µg/m3) but the curve showed high uncertainties for these levels of concentrations. The minimum AICs were obtained for single lag days, at lag 0 for O3 and at lag 7 for the four other pollutants. The respective percentage changes for all-causes mortality associated with 10 μg/m3 increase in pollutants were 0.6% (95% CI: 0.2%, 1.0%) for PM2.5, 0.4% (0.1%, 0.8%) for PM10, 0.5% (-0.2%, 1.1%) for O3, 1.0% (0.3%, 1.7%) for NO2 and 7.1% (-0.1%, 14.8%) for BC (Table 1). We also observed percentage increases for increases in all pollutants concentrations for all-cardiovascular, all-respiratory as well as other natural mortality. Regarding more specific subgroups (IHD, cerebrovascular and COPD mortality), we found a significant increase of 1.6% (95% CI: 0.5%, 2.8%) in IHD mortality for an increase in O3 concentration (Table 1).
Stratified analyses did not show effect modification of the association between most of the individual characteristics (sex, age, employment and hospitalization days) and air pollutants (p > 0.05) (Fig. 2). Regarding preexisting conditions, there was, however, a significantly lower risk of death in people with diabetes for O3 (p = 0.02). We also observed a significant effect modification for thyroid affections and BC (p = 0.049) as well as suggestion of effect modification (p between 0.05 and 0.20 [25]) for PM2.5, PM10, and NO2. In addition, there was a suggestion of a higher risk of death in people with thrombosis or CVD for an increase in PM2.5 concentrations. Finally, there was a suggestion of effect modification for asthma and O3. It can be noted that people with asthma were at higher risk for all pollutants and that this group represents few people (Table S4). Concerning the environmental variables, a higher risk was suggested when NO2 increased for people living in highly built-up areas. There was also a suggestion of a higher risk during the cold season (October–April) when PM10, NO2 and BC increased.
Percentage changes for all-causes mortality associated with air pollutants increase by subgroups of population BC: black carbon; CVD: cardiovascular diseases; COPD: chronic obstructive pulmonary diseases Red: significant effect modification (p<0.05); Dashed red: suggestion of effect modification (p between 0.05 and 0.20) [25]. P-values for effect modification were assessed by Z-tests, which examined the statistical significance of the effect differences between different subgroups; for variables containing more than two categories, p was calculated by comparing the estimate of the specified category with the first category [26] Percentage changes were assessed on different lag days: lag 0 for O3, lag 7 for PM2.5, PM10, NO2 and BC
Two-pollutants models were run for all pairs of pollutants except for the PM2.5 and PM10 pair, and the NO2 and BC pair because Pearson’s correlation coefficients were higher than 0.8 (Table S6). Adjustment for O3 did not change the results and O3 estimates were not modified by adjustment for the other pollutants (Table 2). We observed a decrease in PM2.5 estimate after adjustment for NO2 but not after adjustment for BC. There was also a decrease in PM10 estimates with adjustment for NO2 and to a lesser extent for BC. NO2 and BC estimates were attenuated when models were adjusted for PM2.5 and to a lesser degree for PM10.
Results were robust to changes in the lags specification when using cumulated lags from 0 to 5 days, but for shorter lags of 0 to 1 days, percentage changes became non-significant for all the pollutants. Results were also robust to changes in the meteorological variables specification: increasing the number of df from 3 to 6 in natural cubic splines as well as considering 0–1 days moving averages gave similar estimates, although the percentage increase for BC became significant when changing the definition of the moving average (Table S7).
Discussion
In this study, we found evidence for increases in all-cause, cardiovascular and respiratory mortality with increases in PM2.5, PM10, NO2, O3 and BC concentrations, although the increases were significant for all-cause mortality and PM2.5, PM10, NO2 only. There was also evidence for a significant increase in IHD mortality with an increase in O3 concentration. We did not find effect modification of the association between mortality and any of the air pollutants by individual characteristics (sex, age, employment, hospitalization days). However, this study suggested differences in risks for people with chronic preexisting conditions (thrombosis, cardiovascular diseases, asthma, diabetes and thyroid affections). Finally, our results also suggest effect modification by levels of built-up area (for NO2) and season of death.
In our investigation of effect modification of the air pollution-related mortality association by pseudopathologies, there was suggestion for a higher vulnerability to PM2.5 in people with thrombosis and cardiovascular diseases. People with thyroid affections seemed to be more vulnerable to PM, NO2 and BC. These findings are in line with other studies reporting a higher vulnerability to PM10 in people with pre-existing conditions such as myocardial infarction and congestive heart failure [13], hypertension and chronic obstructive pulmonary disease [27], pneumonia, stroke and heart failure [28]. Some cardiovascular conditions (i.e., ischemic heart disease, pulmonary circulation impairment, heart conduction disorders, heart failure) were also associated with a greater vulnerability to NO2 [29]. A recent meta-analysis reported an increased risk of death from heart failure associated with short-term exposure to PM and NO2 as well as sulphur dioxide and carbon monoxide, but not O3 [30]. Our investigation also suggested a higher vulnerability to O3 in people with asthma. Interestingly, the risk was also higher for the four other pollutants even far from significance. Asthma has often been found to enhance vulnerability to air pollution [31]. The small number of people having asthma in our study, these people representing only 1.5% of our population, can explain the large uncertainties in the effect estimates and the absence of significant effect modification. In this study, we also reported lower risks of death in people with diabetes for increased levels of O3, which differ from the findings of Stafoggia et al. 2010 in a study conducted in 10 Italian cities [32]. Another study reported positive associations between type 2 diabetes mortality and PM and NO2 but O3 was not investigated [33]. Diabetes has actually been more often reported to increase vulnerability to PM-related mortality [13, 14, 27, 28].
Our study suggested a higher risk of death associated with NO2 in highly built-up areas in comparison to less built-up areas. NO2 being a highly traffic-related pollutant, traffic load and street canyon effects can explain higher concentrations of NO2 in urban areas and an increase in the risk of death. By reducing NO2 levels, higher levels of greenness in less built-up areas might also explain these findings [34]. Besides, there was no suggestion of higher risks in highly built-up areas for other pollutants nor in densely populated areas, suggesting that people living in rural areas are also subject to the adverse effects of air pollution. Finally, our study suggested higher effects of PM, NO2 and BC pollutants on mortality during the cold season. Such findings have been observed elsewhere [35, 36] but on the contrary, higher risks during the warm season were also observed in other studies [5, 37, 38]. In this study, we reported higher concentrations of PM, NO2 and BC during the cold season compared to the warm season. Seasonal variations in pollutants levels, different according to the location, could explain the discrepancy between results.
Using objective measures of exposure provided by modeled concentrations of air pollutants, we observed increases in mortality risks with levels of air pollution but as reported by Kangas et al. for the Brussels-Capital Region (Belgium), an increase in mortality has also been linked to increased subjective measures of air pollution (consisting in self-reported perceived air quality) [39].
In two-pollutants models, although all associations remained positive with adjustment for other pollutants, we observed some attenuated associations: adjustment for NO2 decreased the PM-mortality association and the BC–mortality association decreased after adjusting for PM. These findings are in line with other studies showing lower effects of PM with adjustment for NO2 [40,41,42] and slightly BC estimates when adjusting for PM [3]. Nevertheless, our study supports the need for additional studies aimed at better differentiating the effects of individual pollutants on mortality from the associations due to pollutants acting as proxies of others.
This study has several strengths and limitations. First, we obtained individual data for more than half of the population of Belgium. Then, we used the most accurate exposure assessment by linking high-resolution models to the exact geographical coordinates of the address of residence to estimate their exposure to air pollution. In this way, the chance of missing local phenomena (i.e. very small areas recording high values of pollutants concentrations) was reduced. The possibility of exposure misclassification was thus reduced in this study by using geographic point coordinates rather than administrative unit polygons [43]. However, exposure was assessed at the address of residence at the time of death because the exact address of the place of death, often in the hospital, was not available. Exposure to air pollution in the few days preceding death can differ in both places. In this study, we performed stratified analyses with variables going from basic individual characteristics (age, sex) to environmental variables and pre-existing chronic health conditions, which were scarcely investigated in air pollution studies. It is however difficult to determine the chronic disease status of individuals based on medication data because the type and volume of medication is not always specific enough to distinguish between chronic diseases. Additionally, we cannot exclude that a proportion of the population with chronic diseases did not take the prescribed medications but also that some people who took the medication used to define a chronic disease used this medication for other reasons. More generally, a clear definition of chronic health conditions is missing for many chronic diseases so that clearly defining groups of chronic diseases remains difficult [44]. However, Berete et al. showed that the pseudopathology definitions used in this study correctly identify people suffering from several important diseases (cardiovascular diseases, diabetes, thyroid disorders) [45].
Conclusions
This study provided evidence for an increased risk of death associated with air pollution concentrations in Belgium. By identifying more vulnerable populations, the study also contributed to the identification of specific population groups with a higher risk of adverse health effects of air pollution. These findings can help to better define targeted health policies and prevention initiatives to reduce the health impact of air pollution.
Availability of data and materials
The data result from the linkage of administrative databases and has been collected in the framework of the HEASP project (Belgian Statistical Office—approval n°2018/014 from the 19th of June, 2018 and Sectoral Committee on Social Security and Health—approval n°18/080 from the 5th of June, 2018). Restrictions apply to the availability of these data, and so are not publicly available.
Abbreviations
- AIC:
-
Akaike Information Criterion
- BC:
-
Black carbon
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary diseases
- CVD:
-
Cardiovascular diseases
- DLM:
-
Distributed lag linear models
- IHD:
-
Ischemic heart disease
- IMA:
-
InterMutualistic Agency
- NO2 :
-
Nitrogen dioxide
- O3 :
-
Ozone
- PM2.5 :
-
Particulate matter with aerodynamic diameters less or equal than 2.5 μm
- PM10 :
-
Particulate matter with aerodynamic diameters less or equal than 10 μm
- RR:
-
Relative risk
References
Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A. Short-term exposure to particulate matter (PM10 and PM2. 5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environ Int. 2020;142:105876.
Zhu X, Liu B, Guo C, Li Z, Cheng M, Zhu X, et al. Short and long-term association of exposure to ambient black carbon with all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ Pollut. 2023;1(324):121086.
Yang Y, Ruan Z, Wang X, Yang Y, Mason TG, Lin H, et al. Short-term and long-term exposures to fine particulate matter constituents and health: A systematic review and meta-analysis. Environ Pollut. 2019;1(247):874–82.
Wang M, Li H, Huang S, Qian Y, Steenland K, Xie Y, et al. Short-term exposure to nitrogen dioxide and mortality: A systematic review and meta-analysis. Environ Res. 2021;202:111766.
Liu C, Cai J, Chen R, Sera F, Guo Y, Tong S, et al. Coarse Particulate Air Pollution and Daily Mortality: A Global Study in 205 Cities. Am J Respir Crit Care Med. 2022 Jun 7; Available from: https://www.atsjournals.org/doi/pdf/https://doi.org/10.1164/rccm.202111-2657OC. [cited 2022 Jun 14].
Vicedo-Cabrera AM, Sera F, Liu C, Armstrong B, Milojevic A, Guo Y, et al. Short term association between ozone and mortality: global two stage time series study in 406 locations in 20 countries. BMJ. 2020 Feb 10;368. Available from: https://www.bmj.com/content/368/bmj.m108. [cited 2020 Nov 19].
Achilleos S, Kioumourtzoglou MA, Wu CD, Schwartz JD, Koutrakis P, Papatheodorou SI. Acute effects of fine particulate matter constituents on mortality: A systematic review and meta-regression analysis. Environ Int. 2017;109:89–100.
Eurostat 2011. Degree of urbanisation classification - 2011 revision. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php/Degree_of_urbanisation_classification_-_2011_revision#Degree_of_urbanisation_classification
Fierens F, Vanpoucke C, Trimpeneers E, Peeters O, Quidé S, de Vos T, et al. Annual report air quality in Belgium 2015. Belgian Interregional Environment Agency; 2015. Available from: https://www.irceline.be/en/documentation/publications/annual-reports/annual-report-2015/view
Fierens F, Vanpoucke C, Trimpeneers E, Dumoulin R, Maetz P, Hutsemékers V, et al. Rapport annuel 2021 de la qualité de l’air en Belgique. Belgian Interregional Environment Agency; 2021. Available from: https://www.irceline.be/fr/documentation/publications/annual-reports/rapport-annuel-2021/view
Abed Al Ahad M, Sullivan F, Demšar U, Melhem M, Kulu H. The effect of air-pollution and weather exposure on mortality and hospital admission and implications for further research: A systematic scoping review. PLoS One. 2020;15(10):e0241415.
Bell ML, Zanobetti A, Dominici F. Evidence on vulnerability and susceptibility to health risks associated with short-term exposure to particulate matter: a systematic review and meta-analysis. Am J Epidemiol. 2013;178(6):865–76.
Bateson TF, Schwartz J. Who is sensitive to the effects of particulate air pollution on mortality? A case-crossover analysis of effect modifiers. Epidemiology. 2004;15(2):143–9.
Alessandrini ER, Stafoggia M, Faustini A, Berti G, Canova C, De Togni A, et al. Association Between Short-Term Exposure to PM2.5 and PM10 and Mortality in Susceptible Subgroups: A Multisite Case-Crossover Analysis of Individual Effect Modifiers. Am J Epidemiol. 2016;
Gasparrini A, Armstrong B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med Res Methodol. 2013;9(13):1.
Van Hecke E, Halleux JM, Decroly JM, Mérenne-Schoumaker B. Enquête socio-économique 2001 - Monographies. Noyaux d’habitat et régions urbaines dans une Belgique urbanisée. SPF Economie, P.M.E., Classes moyennes et Energie; 2009 p. 201. Available from: https://statbel.fgov.be/sites/default/files/Over_Statbel_FR/Enquete%20SocEco%202001%20-%20Monographie%209%20Noyaux%20d%E2%80%99habitat%20et%20R%C3%A9gions%20urbaines.pdf
Demoury C, De Troeyer K, Berete F, Aerts R, Van Schaeybroeck B, Van der Heyden J, et al. Association between temperature and natural mortality in Belgium: Effect modification by individual characteristics and residential environment. Sci Total Environ. 2022;851(Pt 2):158336.
Lefebvre W, Degrawe B, Beckx C, Vanhulsel M, Kochan B, Bellemans T, et al. Presentation and evaluation of an integrated model chain to respond to traffic- and health-related policy questions. Environ Model Softw. 2013;1(40):160–70.
Delvaux C, Ingels R, Vrábeĺ V, Journée M, Bertrand C. Quality control and homogenization of the Belgian historical temperature data. Int J Climatol. 2019;39(1):157–71.
DiMiceli C, Carroll M, Sohlberg R, Kim DH, Kelly M, Townshend J. MOD44B MODIS/Terra Vegetation Continuous Fields Yearly L3 Global 250m SIN Grid V006. NASA EOSDIS Land Processes DAAC; 2015. Available from: https://lpdaac.usgs.gov/products/mod44bv006/. [cited 2021 Sep 2].
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144–53.
Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology. 2001;12(2):186–92.
Gasparrini A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med. 2014;33(5):881–99.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219.
Faustini A, Stafoggia M, Berti G, Bisanti L, Chiusolo M, Cernigliaro A, et al. The relationship between ambient particulate matter and respiratory mortality: a multi-city study in Italy. Eur Respir J. 2011;38(3):538–47.
Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41:514–20.
Forastiere F, Stafoggia M, Berti G, Bisanti L, Cernigliaro A, Chiusolo M, et al. Particulate matter and daily mortality: a case-crossover analysis of individual effect modifiers. Epidemiology. 2008;19(4):571–80.
Zeka A, Zanobetti A, Schwartz J. Individual-Level Modifiers of the Effects of Particulate Matter on Daily Mortality. Am J Epidemiol. 2006;163(9):849–59.
Chiusolo M, Cadum E, Stafoggia M, Galassi C, Berti G, Faustini A, et al. Short-Term Effects of Nitrogen Dioxide on Mortality and Susceptibility Factors in 10 Italian Cities: The EpiAir Study. Environ Health Perspect. 2011;119(9):1233–8.
Jia Y, Lin Z, He Z, Li C, Zhang Y, Wang J, et al. Effect of Air Pollution on Heart Failure: Systematic Review and Meta-Analysis. Environ Health Perspect. 2023;131(7):76001.
Makri A, Stilianakis NI. Vulnerability to air pollution health effects. Int J Hyg Environ Health. 2008;211(3):326–36.
Stafoggia M, Forastiere F, Faustini A, Biggeri A, Bisanti L, Cadum E, et al. Susceptibility factors to ozone-related mortality: a population-based case-crossover analysis. Am J Respir Crit Care Med. 2010;182(3):376–84.
Wu C, Yan Y, Chen X, Gong J, Guo Y, Zhao Y, et al. Short-term exposure to ambient air pollution and type 2 diabetes mortality: A population-based time series study. Environ Pollut. 2021;15(289):117886.
Song J, Wang Y, Zhang Q, Qin W, Pan R, Yi W, et al. Premature mortality attributable to NO2 exposure in cities and the role of built environment: A global analysis. Sci Total Environ. 2023;25(866):161395.
Du P, Du H, Lu K, He MZ, Feng D, He M, et al. Traffic-related PM2.5 and its specific constituents on circulatory mortality: A nationwide modelling study in China. Environ Int. 2022;170:107652.
Mo S, Hu J, Yu C, Bao J, Shi Z, Zhou P, et al. Short-term effects of fine particulate matter constituents on myocardial infarction death. J Environ Sci. 2023;1(133):60–9.
Carugno M, Consonni D, Randi G, Catelan D, Grisotto L, Bertazzi PA, et al. Air pollution exposure, cause-specific deaths and hospitalizations in a highly polluted Italian region. Environ Res. 2016;147:415–24.
Guo Y, Ma Y, Zhang Y, Huang S, Wu Y, Yu S, et al. Time series analysis of ambient air pollution effects on daily mortality. Environ Sci Pollut Res. 2017;24(25):20261–72.
Kangas T, Gadeyne S, Lefebvre W, Vanpoucke C, Rodriguez-Loureiro L. Are air quality perception and PM2.5 exposure differently associated with cardiovascular and respiratory disease mortality in Brussels? Findings from a census-based study. Environ Res. 2023;219:115180.
Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N Engl J Med. 2019 Aug 21; Available from: https://www.nejm.org/doi/https://doi.org/10.1056/NEJMoa1817364. [cited 2020 Nov 19].
Michikawa T, Ueda K, Takami A, Sugata S, Yoshino A, Nitta H, et al. Japanese Nationwide Study on the Association Between Short-term Exposure to Particulate Matter and Mortality. J Epidemiol. 2019;29(12):471–7.
Tian F, Qi J, Wang L, Yin P, Qian ZM, Ruan Z, et al. Differentiating the effects of ambient fine and coarse particles on mortality from cardiopulmonary diseases: A nationwide multicity study. Environ Int. 2020;145:106096.
Beale L, Abellan JJ, Hodgson S, Jarup L. Methodologic issues and approaches to spatial epidemiology. Environ Health Perspect. 2008;116(8):1105–10.
Maertens de Noordhout Charline, Devos Carl, Adriaenssens Jef, Bouckaert Nicolas, Ricour Céline, Gerkens Sophie. Health system performance assessment: care for people living with chronic conditions. Brussels: Belgian Health Care Knowledge Centre (KCE); 2022. (KCE Reports). Report No.: 352.
Berete F, Demarest S, Charafeddine R, Bruyère O, Van der Heyden J. Comparing health insurance data and health interview survey data for ascertaining chronic disease prevalence in Belgium. Arch Public Health. 2020;78(1):120.
Acknowledgements
The authors thank the Belgian Statistical Office, the InterMutualistic Agency, the Royal Meteorological Institute of Belgium and the Belgian Interregional Environment Agency for providing data.
Funding
This research was funded by Sciensano, the Belgian institute for health.
Author information
Authors and Affiliations
Contributions
CD, RA, FB, JVH and EDC contributed to the conception of the study and interpretation of the data. CD led the data collection, analyzed the data and wrote the original draft. AP helped CD in the software analysis. CV and EDC contributed to the methodology. All authors substantively revised and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Summary statistics for population and mortality by agglomeration. Table S2. Algorithms defining the pseudopathologies. Table S3. Pollutants averaged (2010-2015) daily concentrations (µg/m3) by agglomeration. Table S4. Summary statistics for air pollutants by subgroups, 2010-2015. Table S5. I-square statistic and p-values for Cochran Q-test for heterogeneity. Table S6. Pearson correlations between pollutants. Table S7. Percentage changes and 95% confidence intervals associated with 10 μg/m3 increase in PM2.5, PM10, O3, NO2 and black carbon, 2010-2015 in sensitivity analyses. Figure S1. Agglomeration-specific and pooled PM2.5-mortality relationships. Figure S2. Agglomeration-specific and pooled PM10-mortality relationships. Figure S3. Agglomeration-specific and pooled O3-mortality relationships. Figure S4. Agglomeration-specific and pooled NO2 -mortality relationships. Figure S5. Agglomeration-specific and pooled black carbon-mortality relationships.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Demoury, C., Aerts, R., Berete, F. et al. Impact of short-term exposure to air pollution on natural mortality and vulnerable populations: a multi-city case-crossover analysis in Belgium. Environ Health 23, 11 (2024). https://doi.org/10.1186/s12940-024-01050-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-024-01050-w