Abstract
Background
The associations between maternal exposure to ambient PM2.5 during pregnancy and the risk of premature rupture of membranes (PROM) and preterm premature rupture of membranes (PPROM) are controversial. And no relevant study has been conducted in Asia. This study aimed to determine the association between maternal exposure to ambient PM2.5 during pregnancy and the risk of (P)PROM.
Methods
A cohort study including all singleton births in a hospital located in Central China from January 2015 through December 2017 was conducted. Multivariable logistic regression models, stratified analysis, generalized additive model, and two-piece-wise linear regression were conducted to evaluate how exposure to ambient PM2.5 during pregnancy is associated with the risks of PROM and PPROM.
Results
A total of 4364 participants were included in the final analysis, where 11.71 and 2.34% of births were complicated by PROM and PPROM, respectively. The level of PM2.5 exhibited a degree of seasonal variation, and its median concentrations were 63.7, 59.3, 55.8, and 61.8 μg/m3 for the first trimester, second trimester, third trimester, and the whole duration of pregnancy, respectively. After adjustment for potential confounders, PROM was positively associated with PM2.5 exposure (per 10 μg/m3) [Odds Ratio (OR) = 1.14, 95% Confidence Interval (CI), 1.02–1.26 for the first trimester; OR = 1.09, 95% CI, 1.00–1.18 for the second trimester; OR = 1.13, 95% CI, 1.03–1.24 for the third trimester; OR = 1.35, 95% CI, 1.12–1.63 for the whole pregnancy]. PPROM had positive relationship with PM2.5 exposure (per 10 μg/m3) (OR = 1.17, 95% CI, 0.94–1.45 for first trimester; OR = 1.11, 95% CI, 0.92–1.33 for second trimester; OR = 1.19, 95% CI, 0.99–1.44 for third trimester; OR = 1.53, 95% CI, 1.03–2.27 for the whole pregnancy) Positive trends between the acute exposure window (mean concentration of PM2.5 in the last week and day of pregnancy) and risks of PROM and PPROM were also observed.
Conclusions
Exposure to ambient PM2.5 during pregnancy was associated with the risk of PROM and PPROM.
Similar content being viewed by others
Introduction
The membranes surrounding the amniotic cavity normally rupture at the beginning of labor or during labor. Premature rupture of membranes (PROM) is defined as rupture of membranes (ROM) that occurs more than 1 h before the onset of labor [1]. If rupture occurs before 37 weeks, it is considered preterm PROM (PPROM). PROM, especially PPROM, has been linked with a number of adverse outcomes, including preterm birth, chorioamnionitis, endomyometritis, pelvic abscess, bacteremia, postpartum hemorrhage [2, 3], umbilical cord prolapses, umbilical cord compression, retained placenta, fetal distress [4, 5], and early onset neonatal infection [6]. These outcomes are often associated with increased maternal complications, neonatal mortality [7,8,9], and even adverse long-term outcomes [10].
Despite the high incidence and harmful consequences, the etiology of (P)PROM remains unclear to some degree. Recently, Pereira et al. found that exposure to airborne particulate matter with an aerodynamic diameter of 0.25 μm or less (PM2.5) during the second trimester of pregnancy had an effect on PROM risk in Western Australia [11]. But Dadvand et al. demonstrated that the increased risk of PPROM was associated with PM2.5 absorbance but not with PM2.5 exposure itself [12]. Consequently, the relationship between PM2.5 exposure and (P)PROM is controversial. Meanwhile, to our knowledge, these previous similar studies were all conducted in Caucasian whose environmental status is higher than the national average. No available epidemiological study has discussed the link between PM2.5 and the risks of (P)PROM in China, a country with a considerably high level of PM2.5.
In the present study, we aimed to investigate the association if any between exposure to ambient PM2.5 during pregnancy and the incidence of PROM and PPROM in Wuhan, Central China.
Patients and methods
Study population
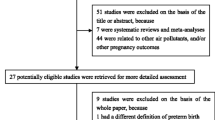
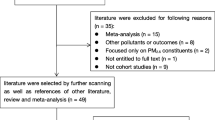
We conducted a population-based study using hospital database in the First People’s Hospital of Jiangxia District in Wuhan, which is a major hospital in the Jiangxia District. We constructed a study cohort that included all singleton births from January 2015 to December 2017. A flow chart (Fig. 1) of the exclusion criteria was provided. Exclusion criteria for participants were as follows: (a) PROM or PPROM cases related to injury, cervix issues, and bleeding during pregnancy; (b) individuals with ages outside the range of 18–35 years old; (c) test tube babies; (d) former or current smokers; (e) congenital uterine malformations; (f) residence in areas further than 40 km from the PM2.5 monitoring station of Donghu New Technology Development Zone; and (g) missing gestational age or delivery data. The final analyses included 4364 singleton live births.
The study protocol was approved by the Medical Ethics Committee of the First People’s Hospital of Jiangxia District and complied with the Declaration of Helsinki. We verbally informed the participants that the data will be used anonymously for a medical study. No informed consent was required, because the study was observational, and the data were anonymized.
Measurement of variables
In China, pregnant women are advised to start systematic antenatal examination and hospital record at the end of the first trimester (i.e., week 12). The hospital records contain a wide range of clinical data on pregnancy and delivery, together with demographic characteristics, underlying diseases, and previous medical histories. ROM diagnosis was performed using the following: pooling test, which is the collection of fluid in the vaginal fornix or fluid leaking from the cervical opening (during coughing or valsalva maneuver); and Nitrazine test, which uses fluid collected from the posterior fornix of the vagina with an alkaline pH. The first and second trimesters were defined as weeks 1–12 and 13–27, respectively. The third trimester was defined as commencing at week 28 and ending at week 40 or at birth, whichever was earlier.
Exposure assignment
Daily (24-h average) PM2.5 measurements were obtained from the Ministry of Ecological Environment of the People’s Republic of China (Donghu New Technology Development Zone site, 114.3894 °E, 30.4822 °N). This site is the nearest monitoring station in the First People’s Hospital of Jiangxia District (approximately 13 km) and the only monitor operational for PM2.5 measurements throughout the study period. We excluded puerperae residing outside 40 km of the vicinity of the site. This choice of threshold distance is same with that used in the study conducted by Pereira in 2014 [11], and is shorter than that used for sensitivity analysis in the study of Di in 2017 [13]. For each subject, we computed the average concentration of PM2.5 for the whole pregnancy, each trimester, the last week, and last day of pregnancy. Temperature exposures were generated by using the same procedure described for PM2.5 exposure.
Statistical analyses
The quarterly incidence rates of PROM and PPROM were calculated and compared with the temporal trend of PM2.5 (Fig. 2). The summary statistics of the characteristics of all patients were expressed as frequencies (proportions) for categorical variables and as means ± SD or median (interquartile range) for continuous variables (Table 1). We also conducted a univariate analysis to evaluate the association between the characteristics and (P)PROM (Additional file 1: Table S1).
Logistic regression models were used to evaluate the relationships of the concentration of PM2.5 (per 10 μg/m3) in each trimester and in the whole pregnancy (as continuous variables) to the risks of PROM and PPROM with and without adjustment for confounding variables (year of birth, season of conception, maternal age, parity, maternal anemia, preeclampsia, gestational diabetes, history of obstetrical-gynecological pathology, and/or mean concentration of PM2.5 in the other two trimesters). We calculated the hazard odd ratios (ORs) and 95% confidence intervals (CIs) (Table 2). We then applied generalized additive models to estimate the above-mentioned relationships with adjustment for potential confounders (Figs. 3 and 4; Additional file 1: Figures S1–S6).
Smooth curves between the mean concentration of PM2.5 for each trimester and for the whole pregnancy and PROM*. *The orange line represents the association between the mean concentration of PM2.5 during the whole pregnancy and PROM, adjusted for year of birth, season of conception, maternal age, parity, maternal anemia, preeclampsia, gestational diabetes, and history of obstetrical-gynecological pathology (Model I); The purple line represents the association between the mean concentration of PM2.5 during the first trimester and PROM, adjusted for Model I plus mean concentration of PM2.5 in the second and third trimesters; The green line represents the association between the mean concentration of PM2.5 during the second trimester and PROM, adjusted for Model I plus mean concentration of PM2.5 in the first and third trimesters; The blue line represents the association between the mean concentration of PM2.5 during the third trimester and PROM, adjusted for Model I plus mean concentration of PM2.5 in the first and second trimesters
Smooth curves between the mean concentration of PM2.5 for each trimester and the whole pregnancy and PPROM*. *The orange line represents the association between the mean concentration of PM2.5 during the whole pregnancy and PPROM, adjusted for year of birth, season of conception, maternal age, parity, maternal anemia, preeclampsia, gestational diabetes, and history of obstetrical-gynecological pathology (Model I); The purple line represents the association between the mean concentration of PM2.5 during the first trimester and PPROM, adjusted for Model I plus mean concentration of PM2.5 in second and third trimesters; The green line represents the association between the mean concentration of PM2.5 during the second trimester and PPROM, adjusted for Model I plus mean concentration of PM2.5 in the first and third trimesters; The blue line represents the association between the mean concentration of PM2.5 during the third trimester and PPROM, adjusted for Model I plus mean concentration of PM2.5 in the first and second trimester
As part of a sensitivity analysis, we did stratified analysis. We conducted logistic regression models to evaluate the relationships of the concentration of PM2.5 (per 10 μg/m3) in the whole pregnancy to the risks of (P)PROM with adjustment for above-mentioned confounding variables in subgroups of age, parity, mode of delivery, season of conception, maternal anemia, preeclampsia, gestational diabetes and history of obstetrical-gynecological pathology (Additional file 1: Table S2).
The associations were further investigated using a two-piece-wise linear model. The turning point of PM2.5, where the relationship between incidence of PROM or PPROM and PM2.5 started to change and became eminent was determined using trial method, which was to move the trial turning point along the pre-defined interval and selected the one that provides the maximum model likelihood. For convenient clinical use, we designated the nearest half or whole number as the turning point (Table 3).
We also investigated the association between acute exposure windows (mean concentration of PM2.5 in the last week and day of pregnancy) and ROM. The results are presented in Table 4 and Additional file 1: Figures S7–S10. PM2.5 effect estimates were calculated per 10 μg/m3 increment and as quartiles.
The temporal trend of temperature and the associations betwS7een temperature and PM2.5 and (P)PROM were also presented in Additional file 1: Figures S11–S13 and Additional file 1: Table S3. Variance Inflation Factor test was conducted to evaluate the multicollinearity between the potential risk factors and independent variable in Additional file 1: Table S4. Temperature exposure was included in adjusted models to assess sensitivity of the observed odds ratios (Additional file 1: Tables S5-S7).
Data were analyzed using the statistical packages R (R Foundation; http://www.r-project.org; version 3.4.3) and EmpowerStats (www.empowerstats.com; X&Y Solutions Inc.).
Results
During the study period, 11.7% (511) and 2.3% (102) of births were complicated by PROM and PPROM, respectively. The median concentrations of PM2.5 were 63.7, 59.3, 55.8, and 61.8 μg/m3 for the first trimester, second trimester, third trimester, and the whole duration of pregnancy, respectively (Table 1). Degrees of seasonal variation were observed in the level of PM2.5 and in the incidence rates of PROM and PPROM. The latter exhibited decreasing tendencies that were not observed in the air quality data (Fig. 2).
The mean age of the puerperae was 26.7 years. PROM and PPROM case births exhibited higher proportion of vaginal delivery, conception in winter, firstborn and maternal preeclampsia compared with births of women without (P) PROM (Table 1).
Table 2 shows that when adjusted for year of birth, season of conception, maternal age, parity, maternal anemia, preeclampsia, gestational diabetes, and history of obstetrical-gynecological pathology (Model I), the mean PM2.5 values (per 10 μg/m3) during the whole pregnancy were positively associated with PROM risk (OR = 1.35, 95% CI, 1.12–1.63) and PPROM (OR = 1.53, 95% CI, 1.03–2.27). But the relationships between PM2.5 in each trimester and the risks of (P)PROM were not significant. Given that the level of PM2.5 exhibited a degree of seasonal variation, the effects during the two trimesters with relatively low PM2.5 level were still considerable and were not overshadowed by the trimester with the highest PM2.5 level. Therefore, we adjusted mean PM2.5 in the other two trimesters to estimate the independent relationships (Model II). In Model II, mean PM2.5 values (per 10 μg/m3) in every trimester were positively associated with PROM risk (OR = 1.14, 95% CI, 1.02–1.26 for first trimester; OR = 1.09, 95% CI, 1.00–1.18 for second trimester; OR = 1.13, 95% CI, 1.03–1.24 for third trimester). The relationships between mean PM2.5 values (per 10 μg/m3) in every trimester and PPROM still had positive trends (OR = 1.17, 95% CI, 0.94–1.45 for first trimester; OR = 1.11, 95% CI, 0.92–1.33 for second trimester; OR = 1.19, 95% CI, 0.99–1.44 for third trimester).
In the sensitivity analysis, we found the independent positive relationships between the concentration of PM2.5 in the whole pregnancy and (P)PROM were robust and consistent in different subgroups of age, parity, mode of delivery, season of conception, maternal anemia, preeclampsia, gestational diabetes and history of obstetrical-gynecological pathology (Additional file 1: Table S2).
Figures 3 and 4 show the nonlinear relationships of the concentration of PM2.5 in each trimester and in the whole pregnancy to PROM and PPROM by curve fitting (separate curves of different adjusted models are presented in Additional file 1: Figures S1–S6).
By two-piece-wise linear regression, in the present study we found the turning points of 46 and 63 μg/m3 for PROM and PPROM, respectively. For PROM, the adjusted OR was 1.43 (95% CI, 1.17–1.73) when PM2.5 ≥ 46 μg/m3 and 0.18 (95% CI, 0.03–1.34) when PM2.5 < 46 μg/m3. For PPROM, the adjusted OR values were 2.42 (95% CI, 1.31–4.46) and 1.15 (95% CI, 0.71–1.85) when PM2.5 ≥ 63 μg/m3 and PM2.5 < 63 μg/m3, respectively (Table 3).
Positive trends between the acute exposure window (mean concentration of PM2.5 in the last week and day of pregnancy) and the risks of PROM and PPROM were observed. As for PROM, OR = 1.01 (95% CI, 0.97–1.04) for last week of pregnancy and OR = 1.02 (95% CI, 1.00–1.05) for last day of pregnancy (per 10 μg/m3). As for PPROM, OR = 1.04 (95% CI, 0.96–1.12) for last week of pregnancy and OR = 1.04 (95% CI, 0.99–1.10) for Last day of pregnancy (per 10 μg/m3) (Table 4). The nonlinear relationships between acute exposure to PM2.5 and the risks of PROM and PPROM are presented in Additional file 1: Figures S7–S10.
Additional file 1: Figure S11 showed a degree of seasonal variation level of the temperature. Additional file 1: Table S3 showed that there is no significant relationship between temperature and (P)PROM. We found that there were severe multicollinearities (Variance Inflation Factor > 5) between temperature and PM2.5 during pregnancy (Additional file 1: Table S4). Sensitivity analysis to temperature adjustment showed that the ORs and turning points did not change considerably after adjustment for temperature exposures, while the 95% CIs got a little wider (Additional file 1: Tables S5-S7).
Discussion
In this population-based cohort study, our multilevel analysis provided preliminary evidence that exposure to PM2.5 during pregnancy was significantly associated with increased risks of PROM and PPROM in Wuhan, Central China. To our knowledge, this is the first study of the relationship between PM2.5 and (P)PROM in Asia and areas with relatively high air pollution.
Previous studies have also investigated the associations between PM2.5 and the risks of PROM and PPROM, but the results were controversial. In the study conducted in Barcelona between 2002 and 2013 (median PM2.5 was 19.8 μg/m3), Dadvand et al. demonstrated that the increased risk of PPROM was associated with PM2.5 absorbance but not with PM2.5 exposure itself [12]. In the study conducted in Western Australia from 1997 to 2007(median PM2.5 was 8.55 μg/m3), Pereira et al. found that PROM was only significantly associated with PM2.5 exposure in the second trimester but not in the first or third trimester or the whole pregnancy [11]. In a retrospective cohort study in America (median PM2.5 was 11.9 μg/m3), Maeve et al. identified associations during acute windows of elevated exposure to PM2.5 in the last 3 h before delivery, but no evidence exists on the association between whole-pregnancy exposure to PM2.5 and PROM or PPROM [14].
In the present study, given the more severe air pollution in China and the use of different statistical methods, we found significant association between PM2.5 exposure and the risks of PROM and PPROM. In our study, the values of PM2.5 were relatively high, and had almost no overlap with the previous studies (the median concentration of 61.8 μg/m3 vs 19.8 μg/m3, 8.55 μg/m3and 11.9 μg/m3). An analysis of PM2.5 levels in 22 countries by the World Health Organization found an association with preterm birth only in China—the country with the highest levels of PM2.5 [15], which may be similar to our situation. As for statistical analyses, compared with previous studies where the date was treated as a whole, we analyzed the data segmentally according to the turning points to obtain more accurate results. At the same time, adjusting the mean PM2.5 in the other two trimesters (Model II) can counteract the seasonal fluctuations in the PM2.5, which may have a huge impact on results. However, previous studies didn’t make such an attempt. These may partly explain the negative results of previous similar studies.
The association between PM2.5 and the risks of PROM and PPROM could be partially explained by oxidative stress mechanism. As a leading air pollutant, PM2.5 can lodge deep inside our lungs and enter the blood stream, causing respiratory, cardiovascular, cerebrovascular [16], and kidney diseases [17], as well as adverse pregnancy outcomes. A newly published study showed independent associations between exposure to PM2.5 and daily all-cause, cardiovascular, and respiratory mortality in more than 600 cities across the globe [18]. Studies have shown that maternal exposure to PM2.5 during the prenatal period was associated with abortion, preterm death and birth, low birth weight, intrauterine growth defects, placental DNA hypomethylation and mtDNA methylation [19,20,21,22,23,24]. Multiple studies indicated that PM2.5 can induce or increase oxidative stress and oxidative DNA damages in the human body [25, 26]. Growing evidence show that oxidative stress plays a role in the pathogenesis of reproduction [27]. Specifically, exposure to PM2.5 could induce the production of reactive oxygen species, which damage DNA [28], release destructive catalytic enzymes, and damage the collagen matrix. Collagen content damage in the chorioamniotic sac leads to tearing, which in turn causes PROM and PPROM [29,30,31]. Similarly, exposure to tobacco smoke [32] or disinfection by-products in drinking water [33] has been linked to PROM and PPROM by oxidative stress.
The level of temperature variation with time, so the overlaps between temperature and season and PM2.5 may exist. Variance Inflation Factor test confirmed the multicollinearities between temperature and PM2.5 which may lead to overfitting. We also found no significant relationship between temperature and (P)PROM, therefore, in the main text we did not incorporate the temperature exposure into the adjustment model. Nevertheless, we conduct sensitivity analysis to temperature adjustment in the supplementary file. After adjustment for temperature, the results did not change considerably. The reason for the widen of the 95% CIs may be due to the inclusion of variables with severe multicollinearity, as well as the increased degree of model freedom due to the addition of adjustment variables. This is consistent with the sensitivity analysis of Pereira et al. [11] that temperature adjustment did not improve precision of the estimate between PM2.5 and PROM.
The present study has several strengths. First, the sample size was relatively large, which gave relatively good generalizability to the surrounding population. Second, we collected the past medical records of all births throughout the hospital to ensure unbiased choices. Third, given the different adjustments for mean PM2.5 in the other two trimesters in Model II, the result was notably disparate from that in Model I. As far as we know, this is the first study to adjust the independent variables in the other two trimesters. Our results can lead to more reliable research and may partly explain the negative results in previous studies. Fourth, we found the turning points of 46 and 63 μg/m3 for PROM and PPROM, respectively. This may not be accurate enough and require further confirmation in future studies for more sample sizes and different regions, but it can still provide a certain degree of reference for prenatal care, pollution control and further research. Fifth, previous studies can provide limited information for population in Asia or in areas with relatively high levels of air pollution, while our research partly filled this gap.
Several limitations should be noted in our study. First, some values were missing because data were based on fore-passed hospital records. Also, misclassification of (P)PROM may exist, since Nitrazine test for diagnosis of (P)PROM is a test with high sensitivity but poor specificity. But it is reasonable to consider the misclassification as independent and nondifferential, which would bias the observed association towards the null. Second, we used a single-ground-based PM2.5 monitor throughout the study period. Hence, the effect of exact street address and possible maternal residential mobility during pregnancy might have been overlooked. Nevertheless, the selection of a threshold distance of 40 km was reasonable, because PM2.5 can travel greater distances than PM10, whose exposure models are agree with estimates derived from the closest monitoring station [11, 34]. The same threshold distance was used in study of Pereira in 2014 [11]. Moreover, in a study of PM2.5 and mortality published in 2017, Di et al. found that estimates of risk based on ZIP-Code-specific assessments of exposure were slightly higher than those provided by the nearest data-monitoring site (within a distance of 50 km), these two measurement methods can get similar conclusions [13]. Therefore, it is plausible that such agreement would be better still for a threshold distance of 40 km in our study. Third, we used ambient pollutant levels as a surrogate for personal exposure, which might lead to some exposure biases. However, these should both result only in nondifferential exposure error and underestimates of pollutant mediated (P)PROM risks. Besides, we did not include some possible related factors (subclinical infections, etc.) in the analysis, however, the robustness of the sensitivity analysis results could give us more confidence in the associations we observed.
Conclusion
In this cohort study, we found that for the first time exposure to PM2.5 during pregnancy was significantly associated with the risk of PROM and PPROM in Wuhan, Central China. These findings could provide further evidence for the adverse impact of air pollution on pregnancy outcomes and could also benefit public health to a certain degree. Further mechanism and intervention studies (such as antioxidant and so on) should be performed.
Availability of data and materials
The datasets generated during the current study can be obtained from the corresponding authors upon reasonable request.
Abbreviations
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- PM2.5 :
-
Airborne particulate matter with an aerodynamic diameter of 0.25 μm or less
- PPROM:
-
Preterm premature rupture of membranes
- PROM:
-
Premature rupture of membranes
References
ACOG Practice Bulletin No. 188: Prelabor Rupture of Membranes. OBSTET GYNECOL. 2018 2018-01-01;131(1):e1-14.
Rouse DJ, Landon M, Leveno KJ, et al. The Maternal-Fetal Medicine Units cesarean registry: chorioamnionitis at term and its duration-relationship to outcomes. Am J Obstet Gynecol. 2004;191(1):211–6 2004-07-01.
Mark SP, Croughan-Minihane MS, Kilpatrick SJ. Chorioamnionitis and uterine function. Obstet Gynecol. 2000;95(6 Pt 1):909–12 2000-06-01.
Merenstein GB, Weisman LE. Premature rupture of the membranes: neonatal consequences. Semin Perinatol. 1996;20(5):375–80 1996-10-01.
Major CA, de Veciana M, Lewis DF, Morgan MA. Preterm premature rupture of membranes and abruptio placentae: is there an association between these pregnancy complications? Am J Obstet Gynecol. 1995;172(2 Pt 1):672–6 1995-02-01.
Cohen-Wolkowiez M, Moran C, Benjamin DK, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28(12):1052–6 2009-12-01.
Duff P. Premature rupture of the membranes in term patients: induction of labor versus expectant management. Clin Obstet Gynecol. 1998;41(4):883–91 1998-12-01.
Yawn BP, Wollan P, McKeon K, Field CS. Temporal changes in rates and reasons for medical induction of term labor, 1980–1996. Am J Obstet Gynecol. 2001;184(4):611–9 2001-03-01.
Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol. 1999;180(3 Pt 1):628–33 1999-03-01.
Clark EA, Varner M. Impact of preterm PROM and its complications on long-term infant outcomes. Clin Obstet Gynecol. 2011;54(2):358–69 2011-06-01.
Pereira G, Bell ML, Belanger K, de Klerk N. Fine particulate matter and risk of preterm birth and pre-labor rupture of membranes in Perth, Western Australia 1997–2007: a longitudinal study. Environ Int. 2014;73:143–9.12.
Dadvand P, Basagaña X, Figueras F, et al. Air Pollution and Preterm Premature Rupture of Membranes: A Spatiotemporal Analysis. Am J Epidemiol. 2014;179(2):200–7 2014-01-15.
Di Q, Dominici F, Schwartz JD. Air Pollution and Mortality in the Medicare Population. N Engl J Med. 2017;377(15):1498–9 2017-10-12.
Wallace ME, Grantz KL, Liu D, Zhu Y, Kim SS, Mendola P. Exposure to Ambient Air Pollution and Premature Rupture of Membranes. Am J Epidemiol. 2016;183(12):1114–21 2016-06-15.
Fleischer NL, Merialdi M, van Donkelaar A, et al. Outdoor air pollution, preterm birth, and low birth weight: analysis of the world health organization global survey on maternal and perinatal health. Environ Health Perspect. 2014;122(4):425–30 2014-04-01.
Bonyadi Z, Ehrampoush MH, Ghaneian MT, Mokhtari M, Sadeghi A. Cardiovascular, respiratory, and total mortality attributed to PM2.5 in Mashhad, Iran. Environ Monit Assess. 2016;188(10):570.
Mehta AJ, Zanobetti A, Bind MA, et al. Long-Term Exposure to Ambient Fine Particulate Matter and Renal Function in Older Men: The Veterans Administration Normative Aging Study. Environ Health Perspect 2016;124(9):1353–60. 2016-09-01.
Liu C, Chen R, Sera F, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381(8):705–15.
Janssen BG, Saenen ND, Roels HA, et al. Fetal Thyroid Function, Birth Weight, and in Utero Exposure to Fine Particle Air Pollution: A Birth Cohort Study. Environ Health Perspect. 2017;125(4):699–705.20 2017-04-01.
Trasande L, Malecha P, Attina TM. Particulate Matter Exposure and Preterm Birth: Estimates of U.S. Attributable Burden and Economic Costs. Environ Health Perspect. 2016;124(12):1913–8 2016-12-01.
Sun X, Luo X, Zhao C, et al. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ Pollut. 2016;211:38–47.
Janssen BG, Godderis L, Pieters N, et al. Placental DNA hypomethylation in association with particulate air pollution in early life. Part Fibre Toxicol. 2013;10:22 2013-06-07.
Wang C, Yang J, Hao Z, et al. Suppression of progesterone synthesis in human trophoblast cells by fine particulate matter primarily derived from industry. Environ Pollut. 2017;231(Pt 1):1172–80 2017-12-01.
Janssen BG, Byun HM, Gyselaers W, Lefebvre W, Baccarelli AA, Nawrot TS. Placental mitochondrial methylation and exposure to airborne particulate matter in the early life environment: An ENVIRONAGE birth cohort study. Epigenetics. 2015;10(6):536–44 2015-01-20.
Kannan S, Misra DP, Dvonch JT, Krishnakumar A. Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential. Cien Saude Colet. 2007;12(6):1591–602 2007-11-01.
Wei Y, Han IK, Shao M, Hu M, Zhang OJ, Tang X. PM2.5 constituents and oxidative DNA damage in humans. Environ Sci Technol. 2009;43(13):4757–62 2009-07-01.
Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:28 2005-07-14.
Janssen BG, Munters E, Pieters N, et al. Placental mitochondrial DNA content and particulate air pollution during in utero life. Environ Health Perspect. 2012;120(9):1346–52 2012-09-01.
Woods JJ. Reactive oxygen species and preterm premature rupture of membranes-a review. Placenta. 2001;22(Suppl A):S38–44 2001-04-01.
Longini M, Perrone S, Vezzosi P, et al. Association between oxidative stress in pregnancy and preterm premature rupture of membranes. Clin Biochem. 2007;40(11):793–7 2007-07-01.
Wall PD, Pressman EK, Woods JJ. Preterm premature rupture of the membranes and antioxidants: the free radical connection. J Perinat Med. 2002;30(6):447–57 2002-01-20.
Menon R, Fortunato SJ, Yu J, et al. Cigarette smoke induces oxidative stress and apoptosis in normal term fetal membranes. Placenta. 2011;32(4):317–22 2011-04-01.
Joyce SJ, Cook A, Newnham J, Brenters M, Ferguson C, Weinstein P. Water Disinfection By-Products and Prelabor Rupture of Membranes. Am J Epidemiol. 2008;168(5):514–21 2008-07-02.
Sellier Y, Galineau J, Hulin A, et al. Health effects of ambient air pollution: do different methods for estimating exposure lead to different results? Environ Int. 2014;66:165–73 2014-05-01.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (Nos. 81370468 and 81671386). We thank all the participants who allowed their data to be used for this study. We acknowledge Dr. Chang-Zhong Chen (Microarray Core Facility, Dana-Farber Cancer Institute, Harvard Medical School, Boston) and Dr. Xinglin Chen (Department of Epidemiology and Biostatistics, Empower U, X&Y solutions Inc., Boston, USA) for their excellent technical assistance and critical review of this work.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81370468 and 81671386).
Author information
Authors and Affiliations
Contributions
CL and KW designed the study. KW, YT, HZ and XZ collected the data. KW, HZ and XZ performed the analytical work. KW, YT, and SS wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The collection of hospital database in the First People’s Hospital of Jiangxia District for this study was approved by the Medical Ethics Committee of the First People’s Hospital of Jiangxia District and complied with the Declaration of Helsinki. We verbally informed the participants that the data will be used anonymously for medical study. No informed consent was required because the study is observational and the data are anonymized.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Fig S1~Fig S10. Separate generalized additive models curves to estimate the relationships between the concentration of PM2.5 and the risk of PROM/PPROM. Table S1. Univariate analysis for association of the characteristics and the risk of (P)PROM. Table S2. Subgroup analysis. Figs S11–S13 and Tables S3-S7. Sensitivity analysis about temperature.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, K., Tian, Y., Zheng, H. et al. Maternal exposure to ambient fine particulate matter and risk of premature rupture of membranes in Wuhan, Central China: a cohort study. Environ Health 18, 96 (2019). https://doi.org/10.1186/s12940-019-0534-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-019-0534-y