Abstract
Background
International evidence suggests patients receiving cardiac interventions experience differential outcomes by their insurance status. We investigated outcomes of in-hospital care according to insurance status among patients admitted in public hospitals with acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI).
Methods
We conducted a cohort study within the Australian universal health care system with supplemental private insurance. Using linked hospital and mortality data, we included patients aged 18 + years admitted to New South Wales public hospitals with AMI and undergoing their first PCI from 2017–2020. We measured hospital-acquired complications (HACs), length of stay (LOS) and in-hospital mortality among propensity score-matched private and publicly funded patients. Matching was based on socio-demographic, clinical, admission and hospital-related factors.
Results
Of 18,237 inpatients, 30.0% were privately funded. In the propensity-matched cohort (n = 10,630), private patients had lower rates of in-hospital mortality than public patients (odds ratio: 0.59, 95% CI: 0.45–0.77; approximately 11 deaths avoided per 1,000 people undergoing PCI procedures). Mortality differences were mostly driven by STEMI patients and those from major cities. There were no significant differences in rates of HACs or average LOS in private, compared to public, patients.
Conclusion
Our findings suggest patients undergoing PCI in Australian public hospitals with private health insurance experience lower in-hospital mortality compared with their publicly insured counterparts, but in-hospital complications are not related to patient health insurance status. Our findings are likely due to unmeasured confounding of broader patient selection, socioeconomic differences and pathways of care (e.g. access to emergency and ambulatory care; delays in treatment) that should be investigated to improve equity in health outcomes.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality and disability worldwide [1]. In Australia, over 590,000 hospital admissions are for CVD each year, with acute myocardial infarction (AMI) contributing to more than 10% of CVD hospitalisations and over 17% of CVD deaths [2]. Reducing major in-hospital cardiovascular outcomes and deaths is a focus of the Australian national health strategy [3]. A large proportion of CVD hospitalisations and deaths are avoidable through timely detection and increased access to effective preventative and treatment, including access to coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI). PCI is the preferred therapy for symptomatic patients presenting with AMI and is the dominant revascularisation procedure in Australia and internationally [2, 4,5,6].
Despite advances in treatment and outcomes, socioeconomic inequities in access to and outcomes following cardiac care remain [2, 7,8,9,10,11]. In countries with highly privatised health systems, AMI inpatients with health insurance, compared with uninsured patients, have higher rates of revascularisation [12] and better outcomes such as shorter length of stay [12] and 30%-40% lower rates of in-hospital mortality [12,13,14], even after adjusting for patient demographic, socioeconomic and clinical characteristics. These differences likely reflect disparities in patient access to surveillance, preventive and hospital care, as well as physician preferences and incentives in performing procedures based on patient insurance status [7, 10, 15].
Evidence of socioeconomic disparities in CVD hospital care are also emerging from countries with universal health systems [7, 10, 16, 17]. In Australia, private health insurance supplements publicly funded universal health care; with almost half of Australians having private health insurance. Private insurance is associated with higher socioeconomic and better health status [18]. Privately insured patients experience shorter waiting times for elective surgery, can choose their treating physician and access private hospitals [19, 20]. As such, privately insured patients have greater access to cardiac interventions, including angiography, angioplasty, stenting, CABG and catheter ablation at the time of presentation [11, 21, 22].
The majority of emergency care in Australia, however, occurs within public hospitals, which account for over 80% of emergency AMI hospitalisations [11]. Patients in public hospitals with private health insurance can elect to be treated as a private or public patient [19]. In recent years, the number of privately funded public hospital admissions has increased, [23] raising concerns about the equity of care provided [24]. However, there is limited evidence on disparities in care outcomes between public and private CVD patients treated in Australian public hospitals [21, 25].
We investigated if private health insurance is associated with better in-hospital outcomes of care among patients in Australian public hospitals admitted with AMI undergoing PCI, the most common revascularisation procedure. Specifically, we measured hospital acquired complications (HACs), hospital length of stay (LOS) and in-hospital mortality among people undergoing their first-observed PCI.
Methods
Setting and dataset
New South Wales (NSW) is Australia’s most populous state, with a population of approximately 8 million people. We used de-identified, linked data from the NSW Admitted Patient Data Collection (APDC), NSW Emergency Department Data Collection (EDDC) and the Registry of Births, Deaths and Marriages (RBDM) Death Registrations data. The APDC is a census of all inpatient separations (discharges, transfers, and deaths) from public and private hospitals, public psychiatric hospitals, multi-purpose services, and private day procedure centres. The APDC contains data relating to patient demographics (e.g. age, sex, area of residence); admission characteristics (e.g. funding source, emergency/elective status, admission and separation date); patient diagnoses (condition onset flag; diagnoses coded according to the International Classification of Diseases 10th Revision Australian Modification [ICD-10-AM]); and procedures (coded according to the Australian Classification of Health Interventions [ACHI]). The EDDC data records characteristics of presentations to the emergency departments of public hospitals (e.g. visit type, mode of arrival, triage category). The RBDM Death Registrations data contain the date of death.
The study dataset included all patients who had any procedure recorded within this time period. Data linkage was performed by the NSW Centre for Health Record Linkage (CHeReL) as part of its Master Linkage Key.
Study population
We included people aged 18 years or older who had a primary diagnosis of AMI and underwent first-observed (index) PCI procedure between 1st January 2017 to 31st December 2020 (See Supplementary Box 1 for codes and definitions). Where patients had multiple records for an admission (e.g. transfer between facilities; change from acute to sub-acute care) we treated these as a continuation of the same admission.
We excluded patients with a PCI procedure in the prior five years, as well as patients with a hybrid revascularisation (i.e. receiving both PCI and CABG) in their index admission, given these patients may differ from those eligible for PCI alone [26]. We also excluded patients with inconsistent records suggesting possible data linkage errors (e.g. APDC records after the date of death).
We defined patients as being privately insured if any of the episodes of care within an admission were billed as a private patient (exposure group), or as publicly insured if all episodes of care were billed as a public patient (comparison group). We excluded patients insured via other schemes (i.e. veterans, workers compensation) on the index admission.
Patient, admission and hospital characteristics
We measured factors potentially related to patients’ use of private health insurance and outcomes of care, including their demographics, clinical characteristics, characteristics of the index admission, and the hospital of admission and procedure. Patient demographics included age, sex, as well as Index of Relative Socioeconomic Disadvantage (IRSD) and remoteness of the area of the patient’s area (Statistical Area 2) of residence [27, 28]. Clinical characteristics of the index admission included the type of AMI (ST-elevated myocardial infarction [STEMI], non–ST-elevated myocardial infarction [NSTEMI], or unspecified) and type of PCI procedure (multi-vessel; multi-stent).
We measured patient morbidities within the index admissions or in the 12 months prior, including the Charlson Comorbidity score [29] and individual diagnoses (e.g. hypertension, diabetes, renal disease). We measured history of smoking using diagnoses within the index admission and the five years prior [30]. We also measured history of CABG, prior admissions for AMI or stroke, and number of hospital admissions and emergency department (ED) presentations prior to the index admission. Admission characteristics included the emergency status on admission and the mode of arrival for those admitted via the ED. Further details on the definition of variables are in Supplementary Table 1.
We identified the peer group of the hospital of admission, categorised as major, large, district or other hospitals (See supplementary Table 2). We measured hospital volume of procedures, using a data-driven approach to calculate quartiles of annual number of PCIs performed within each hospital. Volume was measured for the hospital performing the PCI procedure, noting that some private patients may have been transferred to a private facility for the PCI during their public hospital stay.
Propensity-matched cohort
To control for potential confounding by differences at the index admission, we used propensity scores to match private and publicly funded patients with similar demographic and clinical characteristics, as well as peer group of the hospital of admission and volume of procedures of the hospital undertaking the PCI. We used multivariate logistic regression to estimate the propensity score, using the variables described in Table 1). We matched patients using the 1:1 nearest neighbour without replacement (i.e. private and public patients are paired only once) and allowing the selection of a match within 0.2 propensity score standard deviation. We assessed adequate balance of the baseline covariates using standardised mean differences with a threshold of 10% [31].
In-hospital outcomes
For each patient in our matched cohort, we estimated the prevalence of HACs, the total hospital length of stay (LOS), and all-cause in-hospital mortality. We measured HACs as the occurrence of any hospital-acquired complications within the admission, as per the indicators developed by the Australian Commission on Safety and Quality in Health Care [32]. The HAC indicator includes various types of complications, such as cardiovascular complications, healthcare associated infections, surgical complications requiring an unplanned return to theatre, respiratory complications, and delirium. We calculated total hospital LOS as the difference between the admission end and start dates (including transfers and type change separations). For same-day admissions, we assigned LOS of one day. We identified in-hospital mortality if either the mode of separation for any episode of care within the admission was death, or if the patient had a death date registered in the RBDM Death Registrations between the admission start and end date.
Statistical analysis
We conducted a descriptive analysis of patient characteristics according to insurance status in both non-matched and propensity-matched cohorts. We presented categorical variables as proportions and quantitative variables by the mean or median values and respective standard deviation (SD) or Interquartile range (IQR). All other statistical analysis were performed in our propensity-matched cohort, only.
We conducted a bivariate analysis by private health insurance status to calculate average HACs, hospital length of stay, and in-hospital mortality rates. We estimated the average LOS as the sum of the LOS of all patients divided by the total number of patients. We excluded patients with outlying LOS from these analyses, using a threshold based on LOS distribution [Outlier bound = 75th centile + 10 * (75th—25th centile)] [33].
To assess the association between private health insurance status and outcomes, we calculated odds ratios (ORs) for in-hospital mortality and HACs using Wald tests to test statistical differences between groups. We reported the reduced risk of in-hospital death using the formula: PR private – PR public patients, where PR is the Prevalence Ratio of in-hospital mortality in each group. We estimated average LOS differences using ordinary least squares regression with gauss family given the coefficient from this model is directly interpreted as differences in average LOS between groups. We used public patients as the referent group. We used cluster-robust standard errors in these analyses to account for the matched nature of the sample [31].
We performed cohort selection and data manipulation using SAS V.9.4 (SAS Institute Inc., Cary, NC, USA). We used "MatchIt" and “Cobalt” packages to conduct propensity score matching, diagnostics and estimate treatment effects, as well as conducted the remaining statistical analysis using R V.4.1.1 (R Core Team 2021, Vienna, Austria). For all statistical analyses, we considered the level of significance of 0.05 using two-sided tests.
Post-hoc analyses
We conducted a series of mutually exclusive post-hoc analyses to assess the robustness of our mortality findings. First, we accounted for differing propensity to be transferred between hospitals (e.g. for day procedure in a private facility), which may impact access to services and delays in decision-making processes between public and private patients [33]. We excluded patients transferred to other hospitals (public or private) for their PCI procedure, identified if the hospital performing the procedure differed from the hospital of admission.
Second, as there may be further socioeconomic differences between patients who do and do not hold private health insurance than those measured in our study, we investigated reported insurance status during the hospital admission (noting not all patients with health insurance will report so during the admission). To assess the potential further confounding effects by socioeconomic status, we: (i) restricted to patients recorded as holding private health insurance within the hospital admission, and (ii) restricted to patients where reported insurance status was in agreement with their billing status.
Third, we varied our mortality definition to account for differences in follow-up time and discharge protocols between public and privately treated patients (e.g. to private rehabilitation facilities). We (i) restricted the assessment window to 30 days following the PCI episode and (ii) increased the assessment window to include both in-hospital mortality and 30 days following discharge.
Fourth, we stratified our analyses by AMI type (STEMI or NSTEMI/ non-specified AMI), given differences in severity of the admission and that these patients may have different pathways of care, and by remoteness, given there are differences in access to care across areas.
Finally, we estimated the impact of unmeasured confounding in our analysis using the E-value [34]. This measure indicates the minimum strength of association that an unmeasured confounder would need to have to fully explain away the observed association.
Results
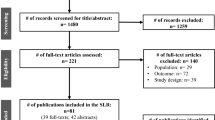
We identified 18,237 patients admitted to New South Wales public hospitals with AMI and undergoing PCI meeting our eligibility criteria, of which 5,486 (30.1%) were private patients. A total of 5,315 private patients were propensity-score matched to a public patient, leading to 10,630 patients for analysis (Fig. 1).
A summary of the index admission characteristics for the unmatched and matched cohorts is shown in Table 1. Prior to matching, private patients were more likely to be male, slightly older, a slightly higher proportion of NSTEMI patients, and a higher proportion having multi-vessel or multi-stent PCI than public patients. Private patients also had better health at the index admission than public patients, with a lower prevalence of several morbidities (e.g., heart failure, peripheral vascular disease, diabetes, chronic pulmonary disease, cardiogenic shock), a lower comorbidity score, a lower proportion being current smokers and lower proportion of multiple ED presentations. Private patients had higher socioeconomic status and were living more often in major cities than public patients, were more likely to be admitted for urgent care, arrive in the ED using emergency services, be admitted at larger hospitals and receive PCI procedures more often at hospitals with intermediate levels of annual procedures (Table 1).
After matching, socio-demographic, clinical, admission or hospital-related characteristics at the index admission were balanced between private and public patients, evidenced by standardised mean differences below 10% in the distribution of their characteristics (Supplementary Fig. 1).
In-hospital outcomes in the propensity-matched cohorts
Hospital Acquired Complications: The occurrence of at least one HAC within the admission was relatively common (n = 802, 7.5%). The five most common HACs were cardiac complications (n = 251, 2.4%), healthcare associated infection (n = 240, 2.3%), surgical complications (n = 190, 1.8%), delirium (n = 116, 1.1%) and respiratory complications (n = 112, 1.1%). There were no clinical meaningful differences between private compared to public patients in rates of HACs during the admission (OR: 0.97, 95%CI: 0.84, 1.12) (Tables 2. and 3).
Length of stay: After excluding 74 outliers (n = 44 private, n = 30 public patients), the average LOS was 5.2 (± 4.4) days [Median 4.0 (IQR 3.0–6.0) days]. Private patients had a similar average LOS than public patients (mean difference = -0.11, 95%CI -0.28, 0.05, p-value = 0.182) (Table 2.). There were no differences among groups after further adjusting the average LOS for the presence of HACs (Mean difference = -0.10, 95%CI -0.25, 0.06, p-value = 0.239).
In-hospital mortality: Overall, rates of in-hospital mortality was low (n = 229, 2.2%). However, private patients were less likely to die in-hospital than public patients (OR: 0.59, 95% CI: 0.45, 0.77) (Table 2.). This corresponded to a reduction of approximately 11 deaths per 1,000 people among private compared to public patients undergoing PCI procedures for AMI in public hospitals.
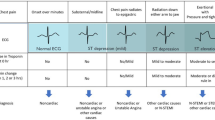
Post-hoc analysis of in-hospital mortality
Our post-hoc analyses all found results comparable with our primary analysis, with lower rates of mortality in private compared to public patients in all analyses using alternate cohorts and definitions (Fig. 2). When stratified by type of AMI (Fig. 2), significant differences in mortality outcomes were observed in STEMI patients only, with no significant difference in the subgroup of people with NSTEMI or non-specified AMI. When stratified by remoteness (Fig. 2), we observed significant differences in mortality outcomes only in major cities; however, we had small number of events in inner, outer, remote and very remote areas.
Finally, we estimated that the observed OR of 0.59, 95% CI: 0.45, 0.77 obtained in the primary analysis could be explained away by unmeasured confounders associated with both private health insurance and in-hospital mortality by an OR of 2.78 (95%CI 1.00, 3.87), adjusted for the currently measured covariates.
Discussion
In this study of public hospital inpatients in Australia’s most populous state, we found privately insured AMI patients undergoing their first-observed PCI were approximately 40% less likely to die in hospital than publicly funded patients with similar health, socio-demographic, and hospital characteristics, representing a reduction of approximately 11 deaths/1,000 people undergoing PCI procedures for AMI in public hospitals. This difference was driven mostly by STEMI patients and those residing in major cities. However, we did not observe any difference between public and privately funded patients in rates of hospital acquired complications or length of stay. These seemingly contradictory findings suggest that private health insurance status may not be impacting in-hospital complications for AMI patients within Australia’s universal healthcare system but may still be associated with mortality outcomes, particularly among STEMI inpatients. This disparity likely reflects either further unmeasured differences between the types of public and privately funded patients who receive PCI, or potential differences in access to, and timing of, emergency services and treatment.
The profile of our study population [35,36,37] and our relatively low rates of in-hospital mortality [36,37,38], complications [36, 37], and average length of stay [6, 37] are broadly consistent with those from PCI populations reported in Australian jurisdictional or nationwide registries. Our findings by funding status are also largely consistent with international studies [12, 13]. For example, a US study of STEMI patients found a 35% difference in rates of in-hospital mortality, and no difference in average LOS, between privately insured and Medicaid patients [13]. However, there are few studies from Australia or other countries with universal health care arrangements with which we can directly compare disparities by health insurance status.
There may be multiple explanations for the disparity in mortality observed in our study. While we adjusted for a range of socio-demographic and health characteristics in our propensity scores, there may be further residual confounding in the types of private and publicly funded public hospital patients who receive PCI. For example, there may be differences in clinical presentation which could not be reliably measured using administrative data, such as salvage PCI, lesion characteristics, cardiogenic shock and cardiac arrest at presentation. Some of these characteristics reflect clinically unstable patients and are among the strongest predictors of in-hospital mortality, [12, 39] although it is not clear if there would be a differential prevalence relating to health insurance status. Similarly, the fact that disparities in mortality were seen in STEMI, and not NSTEMI patients, suggest these potential differences exist among the more severe AMI patients. The in-hospital mortality rate in our private STEMI PCI patients were much lower than the national average (4.6%), [38] suggesting these may be a healthier subset of PCI patients.
It is well known that a patients’ journey, from the onset of symptoms to the procedure, influences revascularisation outcomes, such as delays in first-medical contact and systems delays after presentation [4]. Patient care-seeking behaviours are associated with treatment delays, such as contacting primary health care providers (e.g., GPs) and not using emergency medical transport [40, 41]. In Australia, less than 15% of patients with AMI arrive in the emergency department within one hour of symptoms [40] (the optimal time window for reperfusion therapy), and the median time from symptoms to door is approximately 2.2 hours [40, 41]. Despite Australia having one of the shortest prehospital delays [41], ambulance services are not publicly funded—and uninsured people are potentially less likely to call for an ambulance while experiencing symptoms to avoid out-of-pockets costs for these services [40, 42, 43]. The relationship between private health insurance with other types of delay (e.g., time to electrocardiogram and diagnosis) is not well documented and worth exploring in future research. Those discrepancies may be particularly relevant for more severe forms of myocardial infarction (i.e., STEMI), as observed in our study. There may also be differences in the care provided during the hospital admission, such as the experience of the surgeon, the assessment of urgency of admission [44], use of fibrinolytic and other adjuvant therapy, and the type of intervention provided (e.g., bare metal or drug-eluting stenting), which we were unable to assess [13, 43].
Private health insurance is intrinsically tied to socioeconomic status, and there may be further demographic characteristics which we were not able to be identify (e.g. health literacy). Indeed, public patients in our study tended to be younger, more likely to be smokers, from lower socioeconomic areas, and with higher morbidities at presentation, suggesting a higher prevalence of marginalised populations with features that drive higher mortality. While our findings were consistent when restricting only to patients who reported holding private health insurance, it is still plausible there may be differences in the types of publicly and privately funded patients receiving a PCI. A recent US study found substantial differences in 30-day mortality between Medicare and Medicare Advantage patients admitted for AMI in 2009 had disappeared by 2018. These findings were unable to be explained, but hypothesised to reflect unmeasured changes in patients selected and enrolled in Medicare Advantage over time, as well as possible changes in coding practices [45]. We know that the clinical and demographic profile of patients receiving PCI has been changing in Australia over time, [6] and that there has also been differential uptake of elective PCIs in areas of high socioeconomic status [46]. Whether there are substantial differences in patient selection, clinical characteristics or hospital coding between private and public PCI patients in Australia is yet to be understood.
A key feature of Australian private health insurance is that it can increase or fast track access to ambulatory and specialist services [47], and it’s possible that the difference in mortality relates to service use prior to hospitalisation. Prior studies have reported differential access to cardiac services by socioeconomic factors (e.g. education) or insurance status [4]. Those disparities include increased use of angiography [15] presenting directly to PCI-capable hospitals and reduced time to reperfusion [43]. Other studies assessing disparities by indigenous status also highlighted that lack of private health insurance contributed to lower access to angiography and revascularisation procedures, [48, 49] including a lower probability of being transferred to metropolitan hospitals for angiography [50]. Finally, we acknowledge disparities by insurance status may occur in cardiovascular post-discharge care and events [9, 10, 16, 17, 43] and further studies should also investigate potential disparities post-discharge.
The limitations of administrative data are well known. Our study used one of the most comprehensive sets of patient socio-demographic and clinical characteristics in studies exploring disparities in mortality by insurance status, [7, 10, 12,13,14] but there are further unmeasured confounders not captured in administrative data, as acknowledged above. While few studies have identified the cause of disparities between patient outcomes by insurance status, the strength of association of such a confounder would need to be large (OR = 2.78), suggesting multiple factors may be at play. Further studies linking registry-based data and electronic health records with administrative data could help overcoming this limitation. Finally, Australia’s funding arrangements for hospital care are unique [23], and our findings may not be generalisable to other universal health systems. Furthermore, the use of a propensity matched study means our analysis is restricted to a particular subset of public and privately funded PCI patients, and may not be a representative sample. However, the fact we found similar disparities in outcomes of cardiovascular care to those reported in other health systems suggests there are commonalities in the patient experience. This Australian experience can inform the debate for countries considering expansion of universal health care with supplementary private health insurance [20].
Conclusion
Privately insured patients admitted for AMI in Australian public hospitals and undergoing their first-observed PCI had lower in-hospital mortality rates than comparable publicly funded patients, and similar rates of in-hospital complications and average LOS. These results suggest in-hospital care is not the main contributor to inequities in mortality by insurance status, and other broader socioeconomic factors relating to patient selection, pathways of care and risk of mortality should be explored. Further studies including more granular information on patient, clinical and care pathways, and in countries with different structures of health systems and access to care, are required to understand and to improve equity in PCI health outcomes.
Availability of data and materials
This study used data from the New South Wales Admitted Patient Data Collection linked to the Registry of Births, Deaths and Marriages (RBDM) Death Registrations, and restrictions apply under the Health Records and Information Privacy Act 2002. Data not included in the article or uploaded as supplementary information are available upon reasonable request conditional to the permission of the data custodian and approval from the New South Wales Population and Health Services Research Ethics Committee.
Abbreviations
- ACHI:
-
Australian classification of health interventions
- AMI:
-
Acute myocardial infarction
- APDC:
-
Admitted patient data collection
- CABG:
-
Coronary artery bypass grafting
- CHeReL:
-
NSW Centre for health record linkage
- CVD:
-
Cardiovascular disease
- ED:
-
Emergency department
- EDDC:
-
Emergency department data collection
- HAC:
-
Hospital acquired complications
- ICD-10-AM:
-
International classification of diseases 10th revision Australian modification
- IQR:
-
Interquartile range
- IRSD:
-
Index of relative socioeconomic disadvantage
- LOS:
-
Length of stay
- NSTEMI:
-
Non–ST-elevated myocardial infarction
- NSW:
-
New South Wales
- PCI:
-
Percutaneous coronary intervention
- PR:
-
Prevalence ratio
- RBDM:
-
Registry of births, deaths and marriages death registrations data
- SD:
-
Standard deviation
- STEMI:
-
ST-elevated myocardial infarction
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Australian Institute of Health and Welfare. Heart, stroke and vascular disease—Australian facts [internet]. Canberra: AIHW; 2021 [cited 2021 Nov 1]. Available from: https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts.
Australian Commission on Safety and Quality in Health Care. National core, hospital-based outcome indicator specification 2019. Sydney: ACSQHC; 2019. p. 165. Report No. Version 3.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention: executive summary: a report of the american college of cardiology foundation/American heart association task force on practice guidelines and the society for cardiovascular angiography and interventions. Circulation. 2011;124(23):2574–609.
Agarwal M, Agrawal S, Garg L, Mohananey D, Garg A, Bhatia N, et al. National trends in the incidence, management, and outcomes of heart failure complications in patients hospitalized for st-segment elevation myocardial infarction. Mayo Clinic Proceedings: Innovations, Quality & Outcomes. 2017;1(1):26–36.
Shawon MSR, Falster MO, Hsu B, Yu J, Ooi SY, Jorm L. Trends and outcomes for percutaneous coronary intervention and coronary artery bypass graft surgery in new south wales from 2008 to 2019. Am J Cardiol. 2023;187:110–8.
Lin X, Cai M, Tao H, Liu E, Cheng Z, Xu C, et al. Insurance status, inhospital mortality and length of stay in hospitalised patients in Shanxi, China: a cross-sectional study. BMJ Open. 2017;7(7):e015884.
Casey SD, Mumma BE. Sex, race, and insurance status differences in hospital treatment and outcomes following out-of-hospital cardiac arrest. Resuscitation. 2018;126:125–9.
Ng DK, Brotman DJ, Lau B, Young JH. Insurance status, not race, is associated with mortality after an acute cardiovascular event in Maryland. J Gen Intern Med. 2012;27(10):1368–76.
Fujito H, Kitano D, Saito Y, Toyama K, Fukamachi D, Aizawa Y, et al. Association between the health insurance status and clinical outcomes among patients with acute heart failure in Japan. Heart Vessels. 2022;37(1):83–90. https://doi.org/10.1007/s00380-021-01895-y. Epub 2021 Jun 22.
Korda RJ, Clements MS, Kelman CW. Universal health care no guarantee of equity: comparison of socioeconomic inequalities in the receipt of coronary procedures in patients with acute myocardial infarction and angina. BMC Public Health. 2009;9:460.
Pancholy S, Patel G, Pancholy M, Nanavaty S, Coppola J, Kwan T, et al. Association Between Health Insurance Status and In-Hospital Outcomes After ST-Segment Elevation Myocardial Infarction. Am J Cardiol. 2017;120(7):1049–54.
Patel N, Gupta A, Doshi R, Kalra R, Bajaj NS, Arora G, et al. In-Hospital management and outcomes after St-segment-elevation myocardial infarction in Medicaid beneficiaries compared with privately insured individuals. Circ Cardiovasc Qual Outcomes. 2019;12(1):e004971.
Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452–9.
Hughes V, Paige E, Welsh J, Joshy G, Banks E, Korda RJ. Education-related variation in coronary procedure rates and the contribution of private health care in Australia: a prospective cohort study. Int J Equity Health. 2020;19(1):139.
Hung CL, Chao TF, Su CH, Liao JN, Sung KT, Yeh HI, et al. Income level and outcomes in patients with heart failure with universal health coverage. Heart (British Cardiac Society). 2021;107(3):208–16.
Stirbu I, Looman C, Nijhof GJ, Reulings PG, Mackenbach JP. Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Community Health. 2012;66(12):1159–66.
Doiron D, Jones G, Savage E. Healthy, wealthy and insured? The role of self-assessed health in the demand for private health insurance. Health Econ. 2008;17(3):317–34.
Australian Institute of Health and Welfare. Private health insurance use in Australian hospitals, 2006–07 to 2015–16: Australian hospital statistics. Canberra: AIHW; 2017. 162p. Cat No HSE 196.
Landon BE, Larkin S, Elshaug AG. Challenges of a supplemental private option under national health insurance-observations from Australia. JAMA Intern Med. 2021;181(4):421–2.
Robertson IK, Richardson JR. Coronary angiography and coronary artery revascularisation rates in public and private hospital patients after acute myocardial infarction. Med J Aust. 2000;173(6):291–5.
Quiroz JC, Brieger D, Jorm LR, Sy RW, Falster MO, Gallego B. An Observational Study of Clinical and Health System Factors Associated With Catheter Ablation and Early Ablation Treatment for Atrial Fibrillation in Australia. Heart Lung Circ. 2022;31(9):1269–76. https://doi.org/10.1016/j.hlc.2022.04.049.
Ernst & Young. Private Patient Public Hospital Service Utilisation. [Internet] Sydney: Independent Hospital Pricing Authority; 2017. [Cited 2021 Mar 3]. Available from: https://www.ihacpa.gov.au/resources/private-patient-public-hospital-service-utilisation-2017.
De Oliveira Costa J, Pearson SA, Elshaug AG, Van Gool K, Jorm LR, Falster MO. Rates of Low-Value Service in Australian Public Hospitals and the Association with Patient Insurance Status. JAMA Netw Open. 2021;4(12):e2138543. https://doi.org/10.1001/jamanetworkopen.2021.38543.
Bradshaw PJ, Stobie P, Einarsdóttir K, Briffa TG, Hobbs MS. Using quality indicators to compare outcomes of permanent cardiac pacemaker implantation among publicly and privately funded patients. Intern Med J. 2015;45(8):813–20.
Green KD, Lynch DR Jr, Chen TP, Zhao D. Combining PCI and CABG: the role of hybrid revascularization. Curr Cardiol Rep. 2013;15(4):351.
Australian Bureau of Statistics. Socio-economic indexes for areas (SEIFA): Technical Paper. [Internet] Canberra: ABS; 2011. [cited 021 Mar 12]. Available from: https://www.abs.gov.au/statistics/detailed-methodology-information/concepts-sources-methods/socio-economic-indexes-areas-seifa-technical-paper.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94.
Havard A, Jorm LR, Lujic S. Risk adjustment for smoking identified through tobacco use diagnoses in hospital data: a validation study. PLoS ONE. 2014;9(4):e95029.
Austin PC. An Introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Australian Commission on Safety and Quality in Health Care. Australian Institute of Health and Welfare. Exploring Healthcare Variation in Australia: Analyses Resulting from an OECD Study. Sydney: ACSQHC; 2014. https://www.safetyandquality.gov.au/sites/default/files/migrated/Exploring-Healthcare-Variation-in-Australia-Analyses-Resulting-from-an-OECD-Study.pdf.
National Health Performance Authority. Hospital Performance: Length of stay in public hospitals in 2011–12. 2013.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268–74.
Eccleston D, Horrigan M, Rafter T, Holt G, Worthley SG, Sage P, et al. Improving guideline compliance in australia with a national percutaneous coronary intervention outcomes registry. Heart Lung Circ. 2017;26(12):1303–9.
Lee P, Brennan AL, Stub D, Dinh DT, Lefkovits J, Reid CM, et al. Estimating the economic impacts of percutaneous coronary intervention in Australia: a registry-based cost burden study. BMJ Open. 2021;11(12):e053305.
Yeoh J, Yudi MB, Andrianopoulos N, Yan BP, Clark DJ, Duffy SJ, et al. Evolution of Australian Percutaneous Coronary Intervention (from the Melbourne Interventional Group [MIG] Registry). Am J Cardiol. 2017;120(1):47–54.
National Cardiac Registry Team. National Cardiac Registry Annual status Report 2021. School of Public Health and Preventive Medicine- Monash University; 2022 [cited 2023 Jan 12]. Available from: https://nationalcardiacregistry.org.au/annual-status-report/.
Castro-Dominguez YS, Wang Y, Minges KE, McNamara RL, Spertus JA, Dehmer GJ, et al. Predicting In-Hospital mortality in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol. 2021;78(3):216–29.
Coventry LL, Bremner AP, Williams TA, Celenza A. The effect of presenting symptoms and patient characteristics on prehospital delay in MI patients presenting to emergency department by ambulance: a cohort study. Heart Lung Circ. 2015;24(10):943–50.
Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, et al. prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]). Am J Cardiol. 2009;103(5):598–603.
National Heart Foundation of Australia. Submission to the Senate inquiry into out-of pocket costs in Australian healthcare. [Internet] Canberra: National Heart Foundation of Australia; 2014. [cited 2022 Jul 8]. Available from: https://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/Australian_healthcare/Submissions.
Biswas S, Andrianopoulos N, Duffy SJ, Lefkovits J, Brennan A, Walton A, et al. Impact of socioeconomic status on clinical outcomes in patients with St-segment-elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2019;12(1):e004979.
Shmueli A, Savage E. Private and public patients in public hospitals in Australia. Health policy (Amsterdam, Netherlands). 2014;115(2–3):189–95.
Landon BE, Anderson TS, Curto VE, Cram P, Fu C, Weinreb G, et al. Association of medicare advantage vs traditional Medicare with 30-day mortality among patients with acute myocardial infarction. JAMA. 2022;328(21):2126–35.
Trafalski S, Briffa T, Hung J, Moorin RE, Sanfilippo F, Preen DB, et al. Effect of private insurance incentive policy reforms on trends in coronary revascularisation procedures in the private and public health sectors in Western Australia: a cohort study. BMC Health Serv Res. 2013;13:280.
Pulok MH, van Gool K, Hall J. Horizontal inequity in the utilisation of healthcare services in Australia. Health policy (Amsterdam, Netherlands). 2020;124(11):1263–71.
Randall DA, Jorm LR, Lujic S, O’Loughlin AJ, Eades SJ, Leyland AH. Disparities in revascularization rates after acute myocardial infarction between aboriginal and non-aboriginal people in Australia. Circulation. 2013;127(7):811–9.
Lopez D, Katzenellenbogen JM, Sanfilippo FM, Woods JA, Hobbs MS, Knuiman MW, et al. Disparities experienced by Aboriginal compared to non-Aboriginal metropolitan Western Australians in receiving coronary angiography following acute ischaemic heart disease: the impact of age and comorbidities. International journal for equity in health. 2014;13(1):93.
Lopez D, Katzenellenbogen JM, Sanfilippo FM, Woods JA, Hobbs MS, Knuiman MW, et al. Transfers to metropolitan hospitals and coronary angiography for rural Aboriginal and non-Aboriginal patients with acute ischaemic heart disease in Western Australia. BMC Cardiovasc Disord. 2014;14:58.
Acknowledgements
We thank the NSW Ministry of Health for data provision, and the NSW Centre for Health Record Linkage (CHeReL) for conducting probabilistic linkage of records.
Funding
This research is supported by the National Health and Medical Research Council (NHMRC) Ideas Grant (ID: 1183273) and Project Grant (ID: 1162833). MOF is supported by a Future Leader Fellowship from the National Heart Foundation of Australia (ID: 105609), an Early Career Fellowship from the NHMRC (ID: 1139133) and the NHMRC Centre of Research Excellence in Medicines Intelligence (ID: 1196900). JOC is supported by the NHMRC Centre of Research Excellence in Medicines Intelligence (ID: 1196900).
Author information
Authors and Affiliations
Contributions
JOC and MOF conceived and designed the study. SAP, DB, LRJ, and KVG, contributed to the study design. MOF and LRJ acquired the data. JOC conducted the statistical analysis with support from MOF, SL, MSRS. JOC and MOF drafted the initial article. All authors contributed to the interpretation of results and critical revision of relevant content. All authors commented on drafts and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the NSW Population and Health Services Research Ethics Committee (Approval Number: 2019/ETH00436).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table S1. Detailed list of codes and definitions. Supplementary Table S2. Hospital peer groups. Supplementary Figure S1. Love plot of absolute standardised differences of baseline covariates between private and public patients before and after propensity score matching.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Oliveira Costa, J., Pearson, SA., Brieger, D. et al. In-hospital outcomes by insurance type among patients undergoing percutaneous coronary interventions for acute myocardial infarction in New South Wales public hospitals. Int J Equity Health 22, 226 (2023). https://doi.org/10.1186/s12939-023-02030-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-023-02030-1