Abstract
Background
Chronic diseases pose a serious threat to health and longevity worldwide. As chronic diseases require long periods of treatment and may become serious conditions, the ensuing financial burden is often worse than that for non-chronic diseases. In 2016, the Lao PDR implemented the National Health Insurance (NHI) system, which covers select provinces. However, data on health service accessibility and the financial burden on households, especially those with chronically ill members covered by the NHI, are scarce.
Methods
This study used a cross-sectional design. Data collection was conducted in Bolikhamxay province (population = 273,691), from January 15 to February 13, 2019. In total, 487 households, selected through stratified random sampling, were surveyed via questionnaire-based interviews. Healthcare service usage and financial burden were examined.
Results
A total of 370 households had at least one member with self-reported health issues within the last 3 months prior to the interview, while 170 had at least one member with a chronic condition. More than 75% of the households accessed a health facility when a member experienced health problems. The majority of households (43.2%) spent the maximum value covered by the NHI, but households in the second largest group (21.4%) spent 10 times the maximum value covered by the NHI. The prevalence of catastrophic health expenditure (i.e., health-related expenditure equivalent to > 20% of total income) was 25.9% (20% threshold) and 16.2% (40% threshold). Through logistic regression, we found that the major factors determining financial catastrophes owing to health problems were household members with chronic illness, hospitalization, household poverty status, household size (for both the 20 and 40% thresholds), visiting a private facility (20% threshold), and distance from the province to the referral hospital (40% threshold).
Conclusions
The NHI system has had a positive effect on households’ access to health facilities. However, catastrophic health expenditure remains high, especially among chronically ill patients. Facilities under the NHI system should be improved to provide more services, including care for chronic conditions.
Similar content being viewed by others
Background
Chronic diseases (e.g., major non-communicable diseases [NCDs] such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes) often lead to disabilities, while also posing a serious threat to health and longevity. Chronically ill patients have a higher risk of developing comorbid diseases, which worsen their health condition over time [1]. The burden of such diseases is more serious in low- and middle-income countries because of the myriad challenges in appropriate treatment, prevention, and early detection, compared with high-income countries [2, 3]. Several studies conducted in the Lao PDR have reported a high prevalence of morbidity and chronic diseases [4,5,6,7]. As chronic diseases must be treated over long periods, the ensuing financial burden is often worse than that for non-chronic diseases, which are commonly treated over short periods. Furthermore, in the advanced stages of chronic disease, more intensive and advanced treatments are needed to ensure patients’ survival. In such cases, higher treatment costs are common, which reduces health services accessibility for patients in the advanced stages of a disease. Further, even when patients finally receive treatment, they incur catastrophic health expenditure (CHE). Moreover, in most countries, the poorest people have the highest risk of developing chronic diseases and are the least able to cope with the financial consequences [8]. Thus, providing people with timely access to affordable healthcare is crucial. Nevertheless, reports show that 1.3 billion people worldwide are unable to access affordable and effective healthcare services [9].
Universal health coverage (UHC) is defined as a system in which all individuals and communities have access to health services without suffering financial hardship; this includes the full spectrum of essential and quality health services, ranging from health promotion to prevention, treatment, rehabilitation, and palliative care [10]. Many countries are working to implement UHC systems. In this context, financial protection plays a critical role [10,11,12,13]. Some studies posit that one of the barriers to healthcare access comprises financial burden—out-of-pocket (OOP) payments for treatment [14,15,16].
The government of the Lao PDR has attempted to address these issues and facilitate the implementation of UHC through the introduction of the National Health Insurance (NHI) system, which was launched in select provinces in 2016 [17, 18] and may soon be expanded to all provinces. Under the NHI, the payment system for health services has been simplified; healthcare visits require only a small, fixed co-payment at the facility level, regardless of the administered treatment (Table 1).
In implementing the NHI, the Lao PDR government aimed to ensure smooth access to healthcare and prevent CHE. Some studies have investigated the NHI’s impact in the Lao PDR [19, 20]; however, data on health service accessibility and CHE for households covered by the NHI are scarce, thereby highlighting another research gap—this is especially true of households with chronically ill patients. To bridge these gaps, in this study, we aimed to clarify citizens’ health-seeking behaviors, the prevalence of CHE, and the factors influencing CHE. To this end, we analyze households in Bolikhamxay province, including those with chronically ill patients. We chose this province because the NHI has been in operation here for more than 2 years. To help support the nationwide realization of NHI goals, we aimed to provide data to clarify potential pathways to more well-informed decision-making among managers and policymakers regarding the improvement of health insurance coverage and affordability.
Methods
Study design, area, and data collection method
Using a cross-sectional design, we investigated the health-seeking behaviors, prevalence of health problems, and related financial burden in households in Bolikhamxay province over the past 3 months. According to the latest data from this province, its total population is 273,691; it covers an area of 14,863 km2 (i.e., 5739 mi2), with a population density of 18/km2 [21]. It shares borders with Xiengkhouang Province to the northwest, Vietnam to the east, Khammouane Province to the south, and Thailand to the west. Bolikhamxay province consists of 7 districts (Pakxanh, Thaphabath, Pakkading, Borikhan, Viengthong, Xaychamphone, and Khamkeuth); it has 1 provincial hospital, 6 district hospitals, and 40 health centers [22].
Researchers working in the Lao Tropical and Public Health Institute were trained in interviewing procedures and conducted questionnaire-based interviews with the sampled households from January 15 to February 13, 2019. All interviews were conducted with the head of each household, who provided information about their family members, occasionally consulting with other family members about the same.
Sample size and household selection process
The sampling unit was a household, defined as a group of individuals living together, usually comprising parents and children, and sometimes including grandparents and uncles. To calculate the acceptable sample size for this study, we referred to a previous study on CHE conducted in Vietnam, a neighboring country with a similar political system, which showed a 17.4% CHE prevalence (20% threshold) in 2004 [23]. We also considered a margin of error of ±5, significance at the 99% confidence level, and Z = 2.57. The total number of households in Bolikhamxay province was 54,738—a number obtained by dividing the total population (273,691) [21] by the average number of members in a household (5) [21]. This yielded a sample size of 384 households. To address the possibility of withdrawal, approximately 25% more households were added to the sample, resulting in a final sample size of 480 households.
where the margin of error is ±5, significant at the 95% confidence level, Z = 1.96, the number of households in the province is 54,738, and the estimated proportion of households incurring CHE is 17.4%.
Using a stratified systematic method, the households were sampled as follows. First, we selected three districts, including the provincial capital district (Pakxan). The other two were chosen based on their distance (in km) from Pakxan; the first, Thaphabad, was 50 km away, while the second, Pakkading, was 70–100 km away. As there is only one medical facility at the provincial level in Pakxan, we classified districts into three categories (near, halfway, and far from the capital), assuming that distance from the capital would likely have a strong impact on healthcare access for patients who needed advanced medical intervention. Second, based on the National Statistical Office’s definition of rural areas, we divided the villages in each district into three groups (urban village, rural village with road, and rural village without road). From each group of villages, we randomly selected five villages in each district: one urban village, two rural villages with roads, and two rural villages without roads. We adopted this approach because we assumed that urbanization and the availability of roads would greatly affect general healthcare access within each district. Third, we randomly selected 32–33 households from each village, using the village registration book, with equal intervals on the lists. To ensure the minimum sample size acceptable for this study, upon not acquiring sufficient valid responses from the first group of selected households, we analyzed a novel batch of interviews with the next households on the list, and this procedure was repeated until we reached an acceptable number of valid responses from 32 households per village.
Definitions
Chronic disease
Prior research has posited that differences in the conceptualization of the term “chronic disease” occur largely due to the research data and the research field of lead authors [24]. As we wanted to focus our investigation on all diseases that involved relatively longer treatment periods (to analyze their possible financial burden), regardless of disease course, we chose to simplify the definition of chronic disease. In this study, a chronic disease refers to a disease that a patient has been diagnosed with for more than 3 months at the time of the survey [25]. In this study, we classified diseases into chronic and non-chronic, according to the duration of the condition. For example, if patients had an NCD but they were cured and stopped receiving treatment within the last 3 months, said disease was not categorized as chronic.
Catastrophic health expenditure (CHE)
This is defined as an event in which a household’s medical expenditure exceeds a certain threshold according to the household’s capacity to pay. In this study, to calculate CHE, we adopted the proportionality of income approach [26], where we considered the total monthly OOP spending as a proportion of monthly income, or the proportion of household OOP spending for healthcare greater than the CHE configured in pre-specified proportions. For this study, the data on total household income and total health expenditure per month were obtained from the questionnaire. The total health expenditure per month was calculated via the following procedure. First, in the questionnaire, we asked each household head about the health services their household used and the associated costs in the 3 months preceding the interview. Further, we explained that total health expenditure was defined as the average health expenditure per month, which comprises the sum of all expenses related to medicines, transportation to and from health facilities, consultation and treatment costs, laboratory tests and diagnostic fees, hospitalization fees, cost of visits to traditional healers, and other health-related expenditures during the last 3 months, which was then divided by three. Subsequently, CHE was calculated as the average health expenditure per month in the household divided by household’s total monthly income; the latter value was also obtained during the interview.
Our literature review showed a lack of consensus regarding the thresholds indicating CHE; specifically, we observed thresholds varying from 5 to 40% of total household income [26,27,28,29,30,31]. While there is no consensus regarding the CHE threshold, in this study, we employ the threshold proposed by Xu et al., who define health expenditure as catastrophic if a household’s financial contributions to health equal and/or exceed 40% of non-food expenditure or capacity to spend [29]. However, Rashidian et al. contend that the appropriate cut-off points for the proportion of OOP health expenses to total expenditure and the proportion of health expenditure to ability to pay is 20% [30]. Considering these two previous studies, we set a healthcare expenditure of 20% of the total household income as the threshold for CHE and an expenditure of 40% as the threshold for serious CHE.
Questionnaire structure and independent variables
The questionnaire was developed by drawing on a number of studies on CHE, healthcare utilization, and chronic disease, as well as previous household surveys [26, 31,32,33,34,35,36,37]; the relevant items were adapted to the Lao PDR’s context. We divided the questions into seven sections: a) household composition and demographic characteristics (total monthly income, educational level of the household head, and distance between the household and the nearest medical facility); b) self-reported health problems of household members in the last 3 months (including a variety of health issues ranging from mild to severe, including injuries); c) health-seeking behavior (comprising self-medication and healthcare services—including medical consultations—availed by household members during the preceding 3 months); and e) health services availed and associated costs in the 3 months preceding the interview. Total health expenditure was determined as the sum of all spending on medicines, transportation to and from health facilities, consultation and treatment costs, laboratory tests and diagnostic fees, hospitalization fees, cost of visits to traditional healers, and other health-related expenditures during the last 3 months—converted to 4 weeks, following a previous study [26]. To finalize the questionnaire, a pilot study was carried out with 100 households in Khammouane province (which borders the south of Bolikhamxay Province) to evaluate the accuracy, rigor, and communicability of the questionnaire.
Following previous studies, households were categorized into four groups, in descending order of income, as richest, rich, poor, and poorest. The education level of the head of the household was categorized as under or above primary education. Household size was defined as the number of individuals in a household (< 5 people or ≥ 5 people). Place of residence was defined as the distance from the nearest health facility treating patients with non-severe illnesses (< 5 km or ≥ 5 km) and the provincial-level referral facility treating patients with more severe illnesses (< 10 km or ≥ 10 km). The type of facility visited was defined as public or private. The type of illness suffered was defined as chronic or non-chronic.
Data analysis
SPSS™ version 25 (IBM Corp., Armonk, NY, USA) software was used for statistical analysis. A descriptive analysis was undertaken to understand household background, occurrence and type of health problems, health-seeking behavior (for households and individuals, separately), and household OOP payments. Chi-square statistics were used to compare non-chronically and chronically ill patients’ demographic variables and the different types of facilities used when incurring CHE. Mann-Whitney t-tests were used to compare OOP expenses between the different types of facilities. A logistic regression (logit) model was used to predict the probability of CHE. Based on the literature, we first assumed that the type of illness and treatment episodes had an impact on households with CHE. We expected that chronic illness, hospitalization, treatment in a private facility, and treatment in a provincial-level referral hospital would be associated with high healthcare expenditure.
The second group of variables comprised household characteristics, which included household size, educational level of the head of household, and distance from the nearest health facility as well as the nearest provincial-level referral hospital. We also included households’ economic status [37,38,39]. All these variables were entered into the logit model, using the forward stepwise entry function in SPSS; if the probability of a variable’s score statistic was < 0.05, it was included; conversely, it was removed if the probability was > 0.1. The stepwise entry-removal of the various explanatory variables allowed the identification of those that had a statistically significant influence on the probability of determining CHE. The following variables were included in the model as categorical variables: a) households that incurred expenditure for treating chronic illness and hospitalization (20 and 40% threshold), b) households in which at least one member visited a private facility (20% threshold), c) income groups (20 and 40% thresholds), d) household distance from the nearest provincial-level referral hospital (40% threshold), and e) household size (20 and 40% threshold). The probability of CHE was calculated using the logit model [40], and the model’s goodness-of-fit was assessed via the Hosmer-Lemeshow test [41].
Results
Household demographics and disease prevalence in households
All 487 households in Bolikhamxay province agreed to participate in the interviews (Fig. 1).
The results showed that 28.7% of households had an income < 1,000,000 LAK (62.2 USD)/month. Conversely, the richest households, with an income > 3,500,000 LAK (217.7 USD)/month, accounted for 22.4% of all households. Further, 56.9% of the households had ≤ four members, while 49.7% had a primary education level. Moreover, 73.9% had a distance < 5 km from the nearest medical facility, while 80.5% of the households had a distance ≥10 km from the top referral hospital in the province (Table 2).
Disease prevalence and health-seeking behaviors in households
Of the 487 households, 370 (76.0%) had at least one member with a health problem in the past 3 months. Among these, 170 (45.9%) had at least one member with a chronic condition, 79.2% used some kind of medical facility in the past 3 months, 55.4% used a public facility, 20.3% used a private facility, and 8.6% visited a foreign medical facility. Further, 31.6% had experienced hospitalization and 13.8% visited a provincial top referral hospital (Table 3).
Individual disease prevalence and health-seeking behaviors among non-chronically ill and chronically ill patients
The 487 surveyed households had 2692 members. Among these, 375 (13.9%) members reportedly experienced non-chronic illnesses in the past 3 months, while 198 (7.4%) were chronically ill. Approximately 41.9% of non-chronic and 40.9% of chronically ill patients were male. Further, chronically ill patients were older than non-chronically ill patients, and the difference was statistically significant (medium [25–75%]; 56 [46–62], 33 [8–54]; p < 0.0001) (Table 4).
The percentage of non-chronically ill patients (40.0%) who visited health centers for treatment was higher than that of chronically ill patients (10.6%), and the difference was statistically significant (p < 0.001). The percentage of chronically ill patients (34.8%) who visited the provincial top referral hospital for treatment was higher than that of non-chronically ill patients (7.7%), and the difference was statistically significant (p < 0.0001). The percentage of chronically ill patients (18.7%) who visited private facilities for treatment was higher than that of non-chronically ill patients (14.4%), but the difference was not statistically significant (p = 0.19) (Table 4).
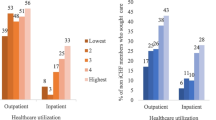
Health facility access by income group
Even in the lowest-income group, more than 85% of the households visited healthcare facilities (Table 5).
Distribution of total monthly household health expenditure and monthly health cost/monthly income (%)
Households with at least one member with any self-reported health problem had a medium OOP health expenditure of 100,000 LAK (6.22 USD; interquartile range, 25,000 LAK [1.6 USD] to 423,750 LAK [26.4 USD]) per month. The majority of households (43.2%) spent less than 30,000 LAK (1.9 USD) per month on healthcare, which is the maximum value covered by the NHI. The distribution of the other expenditure values was polarized; in the second largest group, households spent more than 300,000 LAK (18.7 USD) per month on healthcare, which is 10 times the maximum value covered by the NHI (21.4%; Fig. 2). The OOP health expenditure of households that used only public facilities for treatment (60,000 LAK [3.8 USD]; interquartile range: 20,000 LAK [1.2 USD] to 250,000 LAK [15.6 USD]) and other alternatives (e.g., private facilities or self-medication; 160,000 LAK [10.0 USD]; interquartile range: 50,000 LAK [3.1 USD] to 762,500 LAK [47.42 USD]) was statistically different (p < 0.0001; Table 6).
In total, 96 (25.9%) households met the 20% threshold for CHE, while 60 (16.2%) met the 40% threshold. Households that incurred CHE and used only public facilities for treatment differed statistically (p < 0.0001) from households that used private facilities (Table 6, Fig. 3).
Factors influencing catastrophic health expenditure
The logistic regression analysis revealed a wide range of determinants associated with an increased risk of CHE (Tables 6 and 7). It revealed that the odds of incurring CHE were 3.720 (95% CI, 2.051–6.704, p < 0.0001; 20% threshold) and 4.354 (95% CI, 2.138–8.866, p < 0.0001; 40% threshold) for households with chronically ill members and 2.355 (95% CI, 1.390–4.620, p < 0.0001; 20% threshold) and 3.367 (95% CI, 1.702–6.663, p < 0.0001; 40% threshold) times higher for households with hospitalized members, respectively. The poorest households were 4.002 (95% CI, 1.821–-8.792, p = 0.0001; 20% threshold) and 3.361 times (95% CI, 1.273–8.872, p = 0.014; 40% threshold) more likely to incur CHE when compared with the richest ones. Thus, as household monthly income decreased, the probability of incurring CHE increased. Finally, the odds of incurring CHE were 2.466 (95% CI, 1.310–4.640, p = 0.005) times higher for households that underwent treatment in private facilities (20% threshold) and 4.587 (95% CI, 1.690–13.558) times higher for households more than 10 km away from the provincial hospital (40% threshold). Households with fewer than five members were 2.127 (95% CI, 1.182–3.829, p = 0.012; 20% threshold) and 2.669 (95% CI, 1.321–5.344, p = 0.006; 40% threshold) times more likely to incur CHE (Tables 7 and 8).
Discussion
Our study clarified the health-seeking behaviors (especially vis-à-vis chronic diseases) and related financial burdens of households in Bolikhamxay province, one of the provinces in the Lao PDR fully covered by the current NHI system. Regarding the positive aspects of the NHI, most households with non-chronically ill (69.9%) and chronically ill (78.8%) patients reported that they visited a health facility for treatment. This study did not clarify whether this trend is a direct effect of the NHI because we did not analyze data from the period preceding the NHI’s implementation. Nevertheless, our findings highlight that in Bolikhamxay province, where the NHI has been implemented, more than 75% of the households in lower-income groups visited a health facility when one of the members had an illness; however, there were some gaps between income groups. Our findings are consistent with two previous studies conducted in a different province [19, 20], which found that the NHI has had positive effects on healthcare accessibility.
Furthermore, this study examined the key financial burdens for households under the current NHI scheme. We observed that 25.9 and 16.2% of the households with at least one member with any self-reported health problem incurred CHE (20%) and serious CHE (40%) per month, respectively. Households with at least one member who was chronically ill or needed hospitalization were more likely to incur CHE. OOP health expenditure for chronic and severe diseases was a considerable burden on households, especially poorer ones; thus, the design of future CHE prevention interventions must take these factors into account [42,43,44,45]. Our findings indicate that the financial burden of households under the NHI remains high, especially for those with members who have chronic and/or severe diseases. Moreover, our analysis of household demographics showed that even among households covered by the NHI, OOP health expenditure is greatly polarized between small payments (i.e., within the value covered by the NHI) and very large payments (i.e., which greatly exceed the value covered by the NHI).
We offer the following reasons for these results. First, there are many households that prefer or may be forced to visit private facilities, as our findings showed that households with members who used private facilities were more likely to incur CHE, compared with those who used only public facilities. Our findings are consistent with those of previous studies which showed that people in the Lao PDR preferred to utilize private health services as their first choice regardless of their socioeconomic status, whereas the utilization of public services was low; additionally, high-income households preferred private clinics and receiving treatment abroad [46,47,48]. Another study found that many people from the Lao PDR sometimes used the health services from certain provinces in Thailand, where most health workers speak Isan Thai (a dialect of the Lao language) as their native tongue [48].
We hypothesize that this may have been because the members had diseases that were difficult to treat or could only be treated in private facilities; alternatively, people may still prefer private facilities even if they are costlier and not covered by the NHI. Therefore, to avoid CHE in Lao households covered by the NHI, managers must ensure that effective treatment for chronic and complex diseases can be provided at facilities covered by the NHI. To achieve this, it is necessary to increase the population’s willingness to visit public facilities, mainly by improving service quality and insurance coverage in public hospitals.
Our results also showed that many households incurred CHE even in public hospitals. This may be due to additional, indirect costs related to visiting health facilities, such as transportation costs, which are not covered by the NHI co-payment scheme. Previous research has also pointed out the existence of additional expenditures for patients visiting public health facilities, including those related to medications or supplies not available in public health facilities or not covered by the NHI [48]. Thus, to prevent CHE among households covered by the NHI, it is necessary to expand the scope of NHI coverage, especially for chronically ill patients (mainly those with NCDs), who require more complex and often prolonged treatments.
Among chronically ill patients in our sample, most visited the provincial, top referral hospital; however, there is only one such hospital in Bolikhamxay province. This denotes that travelling to the hospital entails a high cost (both time and money) for some households [49, 50]. Coupled with the abovementioned CHE rate, this becomes a critical concern for managers. To implement a UHC system, primary care must be emphasized [51]. However, this emphasis on primary care may lead some patients to suffer from complex and/or life-threatening problems if they are not referred to higher level facilities; this is especially true of aging societies such as that of the Lao PDR [52, 53]. These patients require advanced treatment, which often entails high costs that may lead to CHE. Hence, managers should place additional focus on methods for providing NHI patients with advanced care while considering the reality of their financial situation and the constraints of the NHI.
The results of this study, which underscore the differences in medical expenditure across various groups, also highlight the importance of supporting high medical expenditures. For example, in the Japanese NHI, there is a fixed percentage (10–30%) for co-payments for treatment as well as a limit for total co-payments per month, called the “ceiling amount” [54]. We advocate for a similar financial system for the NHI in the Lao PDR, which may help prevent CHE in households with chronically ill members.
To implement UHC, it is important to enhance the coverage of healthcare systems, as well as citizens’ financial protection. In the Lao PDR, the NHI was initially introduced with the aim of covering the entire population of select provinces, as well as to provide financial protection through a fixed payment system. However, it did not necessarily consider the enhancement of service provision; thus, we believe that the NHI’s potential preventive effect on CHE has been limited.
Even in poor households, it is common for people to seek better medical services when they become ill. Our findings underpin that CHE is more likely to occur in households with lower incomes. Similarly, global studies have highlighted the importance of ensuring a reasonable distribution of health services across different community-based and socioeconomic strata, especially for patients with chronic diseases [49]. Accordingly, our discussion suggests that the NHI requires additional improvements regarding health facility placement; patients must be able to access reasonably located healthcare facilities that deliver quality services. This should also be valid for facilities aimed at treating chronically ill patients, which often require long-term and frequent care delivery. To realize UHC in the Lao PDR, the government must adopt a comprehensive approach to the NHI that better reflects the current situation.
This study has some limitations. First, we analyzed data on households’ finances (i.e., health expenditure and income) by interviewing the household heads; however, this method may have affected data precision. Second, self-reported diagnoses were included for citizens who did not visit a health facility; however, the estimates (prevalence) were not weighted to obtain province-representative evidence and a longitudinal design was not adopted to assess the difference between the pre- and post-NHI periods.
Nevertheless, to the best of our knowledge, this is the first study to investigate the health-seeking behaviors and financial burdens of households covered by the NHI in the Lao PDR, including those with chronically ill patients. Most previous studies on the NHI in the Lao PDR focused on patients who visited healthcare facilities; consequently, their data did not consider patients who did not visit or could not access such facilities. Therefore, we deemed it necessary to examine the situation of people who did not or could not visit healthcare facilities; this allowed us to assess the effectiveness of interventions aimed at realizing UHC, such as the NHI in the Lao PDR. This is because the main purpose of the NHI is to improve the general population’s access to health facilities while ensuring they do not incur major financial burdens related to healthcare.
Conclusion
Our results provide a clear picture of the current status of the general population in provinces covered by the NHI, particularly regarding access to health services and households’ financial burden, especially for those with chronically ill members. We hope that this evidence provides a valuable theoretical framework for managers and policymakers to conduct well-informed decision-making to facilitate the realization of UHC in the Lao PDR.
Availability of data and materials
The data supporting the conclusions of this article are available from the corresponding author upon reasonable request.
Change history
23 February 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12939-023-01827-4
Abbreviations
- NCDs:
-
Non-communicable diseases
- NHI:
-
National Health Insurance
- UHC:
-
Universal health coverage
- CHE:
-
Catastrophic health expenditure
- OOP:
-
Out-of-pocket
References
Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009;373(9680):2004–6. https://doi.org/10.1016/S0140-6736(09)61074-6.
Yach D, Kellogg M, Voute J. Chronic diseases: an increasing challenge in developing countries. Trans R Soc Trop Med Hyg. 2005;99(5):321–4. https://doi.org/10.1016/j.trstmh.2005.02.001.
Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–38. https://doi.org/10.1016/S0140-6736(07)61696-1.
Pengpid S, Vonglokham M, Kounnavong S, Sychareun V, Peltzer K. The prevalence, awareness, treatment, and control of hypertension among adults: the first cross-sectional national population-based survey in Laos. Vasc Health Risk Manag. 2019;15:27–33. https://doi.org/10.2147/VHRM.S199178.
Vonglokham M, Kounnavong S, Sychareun V, Pengpid S, Peltzer K. Prevalence and social and health determinants of pre-diabetes and diabetes among adults in Laos: a cross-sectional national population-based survey, 2013. Trop Med Int Health. 2019;24(1):65–72. https://doi.org/10.1111/tmi.13164.
Louangpradith V, Phoummalaysith B, Kariya T, Saw YM, Yamamoto E, Hamajima N. Disease frequency among inpatients at a tertiary general hospital in Lao PDR. Nagoya J Med Sci. 2020;82:113–21. https://doi.org/10.18999/nagjms.82.1.113.
Are C, Meyer B, Stack A, Ahmad H, Smith L, Qian B, et al. Global trends in the burden of liver cancer. J Surg Oncol. 2017;115(5):591–602. https://doi.org/10.1002/jso.24518.
Suhrcke M, Nugent RA, Stuckler D, Rocco L. Chronic disease: an economic perspective. London: The Oxford Health Alliance; 2006.
International Labour Organization. Social health protect: an ILO strategy towards universal access to health care. 2008. https://www.ilo.org/wcmsp5/groups/public/-ed_protect/-soc_sec/documents/publication/wcms_secsoc_5956.pdf. Accessed 1 Feb 2021.
World Health Organization. Universal health coverage (UHC). 2021. https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc). Accessed 1 Feb 2021.
World Health Organization. Systems financing–the path to universal coverage. 2010. https://www.who.int/whr/2010/whr10_en.pdf. Accessed 1 Feb 2021.
Kutzin J. Anything goes on the path to universal health coverage? No Bull World Health Organ. 2012;90(11):867–8. https://doi.org/10.2471/BLT.12.113654.
Behera M, Behera D. A critical analysis of the term “universal health coverage” under post-2015 sustainable development goals. Ann Trop Med Public Health. 2015;8:155–8.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19(2):69–79. https://doi.org/10.1093/heapol/czh009.
Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur RM. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–71. https://doi.org/10.1196/annals.1425.011.
Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18.
World Health Organization. Lao Ministry of Health moves forward with National Health Insurance. 2019. https://www.who.int/laos/news/detail/01-09-2019-lao-ministry-of-health-moves-forward-with-national-health-insurance. Accessed 30 Jun 2021.
National Health Insurance Bureau. Lao People’s Democratic Republic. Peace, independence, democracy, unity, prosperity: national health insurance funds implementation guideline, vol. No 0264: NHIB; 2016.
Nagpal S, Masaki E, Pambudi ES, Jacobs B. Financial protection and equity of access to health services with the free maternal and child health initiative in Lao PDR. Health Policy Plan. 2019;34(Supplement_1):i14–25. https://doi.org/10.1093/heapol/czz077.
The World Bank. Out-of-pocket spending and health service utilization in Lao P.D.R.: evidence from the Lao expenditure and consumption surveys (policy note). Lao PDR: World Bank; 2010.
Lao Statistics Bureau, Ministry of Planning and Investment. Results of population and housing census 2015. https://lao.unfpa.org/sites/default/files/pub-pdf/PHC-ENG-FNAL-WEB_0.pdf. Accessed 30 Jun 2021.
Japan International Cooperation Agency. Data collection survey on health sector in Lao People’s Democratic Republic: final report 2016. https://openjicareport.jica.go.jp/pdf/12252698_01.pdf. Accessed 1 Apr 2021.
Van Minh H, Phuong NTK, Saksena P, James CD, Xu K. Financial burden of household out-of-pocket health expenditure in Viet Nam: findings from the National Living Standard Survey 2002–2010. Soc Sci Med. 2013;96:258–63. https://doi.org/10.1016/j.socscimed.2012.11.028.
Bernell S, Howard SW. Use your words carefully: what is a chronic disease? Front Public Health. 2016;4:159. https://doi.org/10.3389/fpubh.2016.00159.
MedicineNet. Definition of chronic disease. 2016. http://www.medicinenet.com/script/main/art.asp?articlekey=33490. Accessed 11 Aug 2021.
Buigut S, Ettarh R, Amendah DD. Catastrophic health expenditure and its determinants in Kenya slum communities. Int J Equity Health. 2015;14:46. https://doi.org/10.1186/s12939-015-0168-9.
Wyszewianski L. Financially catastrophic and high-cost cases: definitions, distinctions, and their implications for policy formulation. Inquiry. 1986;23(4):382–94.
Berki SE. A look at catastrophic medical expenses and the poor. Health Aff (Millwood). 1986;5:138–45. https://doi.org/10.1377/hlthaff.5.4.138.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7. https://doi.org/10.1016/S0140-6736(03)13861-5.
Rashidian A, Akbari Sari A, Hoseini SM, Soofi M, Ameri H. Comparison of the thresholds of households’ exposure to catastrophic health expenditure in Iran and Brazil, and selection of the most appropriate threshold. Iranian J Pub Health. 2018;47(12):1945–52.
Aregbeshola BS, Khan SM. Determinants of catastrophic health expenditure in Nigeria. Eur J Health Econ. 2018;19:521–32.
Brinda EM, Andrés RA, Enemark U. Correlates of out-of-pocket and catastrophic health expenditures in Tanzania: results from a national household survey. BMC Int Health Hum Rights. 2014;14:5. https://doi.org/10.1186/1472-698X-14-5.
Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek M, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Pol Plan. 2012;27:613–23. https://doi.org/10.1093/heapol/czs001.
Comprehensive Survey of Living Conditions. 2016. https://www.mhlw.go.jp/english/database/db-hss/cslc.html. Accessed 20 Sept 2022.
Health measures in the 1997 Redesigned National Health Interview Survey (NHIS) 2015. https://www.cdc.gov/nchs/nhis/nhis_redesign.htm. Accessed 20 Sept 2022.
WHO Study of Global Ageing and Adult Health (SAGE). https://www.who.int/data/data-collection-tools/study-on-global-ageing-and-adult-health#:~:text=WHO%20Study%20on%20global%20AGEing,Russian%20Federation%20and%20South%20Africa. Accessed 20 Sept 2022.
Su TT, Kouyaté B, Flessa S. Catastrophic household expenditure for health care in a low-income society: a study from Nouna District, Burkina Faso. Bull WHO. 2006;84(1):21–7. https://doi.org/10.2471/BLT.05.023739.
Wter HR, Anderson GF, Mays J. Measuring financial protection in health in the United States. Health Policy. 2004;69:339–49. https://doi.org/10.1016/j.healthpol.2004.01.003.
Gotsadze G, Zoidze A, Rukhadze N. Household catastrophic health expenditure: evidence from Georgia and its policy implications. BMC Health Serv Res. 2009;9:69. https://doi.org/10.1186/1472-6963-9-69.
Greene W. Econometric analysis. New Jersey: Prentice Hall International Inc.; 1997.
Hosmer DW, Lemeshov S. Applied logistic regressions. New York: John Wiley & Sons Inc; 2000.
Choi J-W, Choi J-W, Kim J-H, Yoo K-B, Park E-C. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Serv Res. 2015;15:26. https://doi.org/10.1186/s12913-014-0675-1.
Wang Z, Li X, Chen M. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. 2015;14:8. https://doi.org/10.1186/s12939-015-0134-6.
Van Minh H. Tran BX assessing the household financial burden associated with the chronic non-communicable diseases in a rural district of Vietnam. Glob Health Action. 2012;5:1. https://doi.org/10.3402/gha.v5i0.18892.
Rezapour A, Vahedi S, Khiavi FF, Esmaeilzadeh F, Javan-Noughabi J, Rajabi A. Catastrophic health expenditure of chronic diseases: evidence from Hamadan, Iran. Int J Prev Med. 2017;8:99. https://doi.org/10.4103/ijpvm.IJPVM_104_17.
Paphassarang C, Philavong K, Boupha B, Blas E. Equity, privatization and cost recovery in urban health care: the case of Lao PDR. Health Policy Plan. 2002;17(1):72–84.
Powell-Jackson T, Lindelow M. Out-of-pocket spending and health service utilization in Lao P.D.R.: evidence from the Lao expenditure and consumption surveys (policy note). Vientiane: World Bank; 2010.
Knowles JC. Public expenditure in the Lao PDR health sector: background paper for 2006 PER. Manila: Governance, Finance and Trade Division, Mekong Department, Asian Development Bank; 2006.
Fuady A, Houweling TA, Mansyur M, Richardus JH. Catastrophic total costs in tuberculosis-affected households and their determinants since Indonesia’s implementation of universal health coverage. Infect Dis Poverty. 2018;7:3. https://doi.org/10.1186/s40249-017-0382-3.
Barter DM, Agboola SO, Murray MB, Bärnighausen T. Tuberculosis and poverty: the contribution of patient costs in sub-Saharan Africa – a systematic review. BMC Public Health. 2012;12:980. https://doi.org/10.1186/1471-2458-12-980.
Primary health care on the road to universal health coverage. 2019 Global monitoring report executive summary 2019. https://www.who.int/docs/default-source/documents/2019-uhc-report-executive-summary. Accessed 1 Jun 2021.
Phouminidr B. Policy of ageing in Lao People’s Democratic Republic. 2019. https://www.duke-nus.edu.sg/docs/librariesprovider3/education-docs/1)-policies-on-the-health-of-older-adults-(laos)-by-associate-prof-dr-bouathep-phoumindr.pdf?sfvrsn=e3afdd71_4. Accessed 30 Jun 2021.
World Health Organization. Ageing and health in the South-East Asia Region. 2020. https://www.who.int/southeastasia/health-topics/ageing. Accessed 1 Jun 2021.
Ministry of Health, Labour and Welfare, Japan. High-cost medical expense benefit (Eligibility certificate for ceiling-amount application). https://www.mhlw.go.jp/file/06-Seisakujouhou-10800000-Iseikyoku/0000056917.pdf. Accessed 1 Jun 2021.
Acknowledgments
We are grateful to Dr. Khouanchay Soundavong, Dr. Kethmany Chanthakouman, and the Lao TPHI team of data collectors for their assistance in survey arrangement and data collection.
Funding
This study was supported by the International Medical Research and Development Fund in National Center for Global Health and Medicine—Project number: 28–3. Title of Research Project: Research on the use of overseas centers for health policy research on universal health coverage and other issues.
Author information
Authors and Affiliations
Contributions
Tomoo Ito was involved in the study design, data analysis, and interpretation. All authors critiqued the report, commented on drafts of the manuscript, and approved the final report.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the National Center for Global Health and Medicine (NCGM-G-002144-01) and the National Ethics Committee for Health Research of the Lao Ministry of Health (No, 053/NECHR). Verbal informed consent (approved by the Ethical Committee) was obtained from each respondent and key participant prior to commencing their respective interviews. All documents were de-identified. Caregivers or mothers provided consent for children when they took part in the interviews. Privacy and confidentiality were assured for all respondents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: in Table 7 the odds ratio for ‘Household size > 5’ was incorrectly given as '2.127' but should have been '2.128', and in Table 8 the odds ratio for ‘Poorest: Under 1,000,000 LAK (62.2 USD)/month’ was incorrectly given as '3.369' but should have been '3.339'
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ito, T., Kounnavong, S. & Miyoshi, C. Financial burden and health-seeking behaviors related to chronic diseases under the National Health Insurance Scheme in Bolikhamxay Province, Lao PDR: a cross-sectional study. Int J Equity Health 21, 180 (2022). https://doi.org/10.1186/s12939-022-01788-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-022-01788-0