Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is a globally increasing health epidemic. Lifestyle intervention is recommended as the main therapy for NAFLD. However, the optimal approach is still unclear. This study aimed to evaluate the effects of a comprehensive approach of intensive lifestyle intervention (ILI) concerning enhanced control of calorie-restricted diet (CRD), exercise, and personalized nutrition counseling on liver steatosis and extrahepatic metabolic status in Chinese overweight and obese patients with NAFLD.
Methods
This study was a multicenter randomized controlled trial (RCT) conducted across seven hospitals in China. It involved 226 participants with a body mass index (BMI) above 25. These participants were randomly assigned to two groups: the ILI group, which followed a low carbohydrate, high protein CRD combined with exercise and intensive counseling from a dietitian, and a control group, which adhered to a balanced CRD along with exercise and standard counseling. The main measure of the study was the change in the fat attenuation parameter (FAP) from the start of the study to week 12, analyzed within the per-protocol set. Secondary measures included changes in BMI, liver stiffness measurement (LSM), and the improvement of various metabolic indexes. Additionally, predetermined subgroup analyses of the FAP were conducted based on variables like gender, age, BMI, ethnicity, hyperlipidemia, and hypertension.
Results
A total of 167 participants completed the whole study. Compared to the control group, ILI participants achieved a significant reduction in FAP (LS mean difference, 16.07 [95% CI: 8.90–23.25] dB/m) and BMI (LS mean difference, 1.46 [95% CI: 1.09–1.82] kg/m2) but not in LSM improvement (LS mean difference, 0.20 [95% CI: -0.19–0.59] kPa). The ILI also substantially improved other secondary outcomes (including ALT, AST, GGT, body fat mass, muscle mass and skeletal muscle mass, triglyceride, fasting blood glucose, fasting insulin, HbA1c, HOMA-IR, HOMA-β, blood pressure, and homocysteine). Further subgroup analyses showed that ILI, rather than control intervention, led to more significant FAP reduction, especially in patients with concurrent hypertension (p < 0.001).
Conclusion
In this RCT, a 12-week intensive lifestyle intervention program led to significant improvements in liver steatosis and other metabolic indicators in overweight and obese Chinese patients suffering from nonalcoholic fatty liver disease. Further research is required to confirm the long-term advantages and practicality of this approach.
Trial registration
This clinical trial was registered on ClinicalTrials.gov (registration number: NCT03972631) in June 2019.
Similar content being viewed by others
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a global health problem that affects approximately one in four people worldwide [1]. NAFLD has become increasingly prevalent in China due to economic development and dramatic lifestyle alterations; it affects an estimated 240 million people, almost one-fifth of the global population with NAFLD [2,3,4]. The disease poses a tremendous public health burden, as NAFLD is intricately linked to obesity, diabetes, and other metabolic disorders. NAFLD can also lead to cirrhosis and hepatic carcinoma and increase the risk of cardiovascular disease.
Most guidelines and consensus recommend weight loss through lifestyle intervention as the first-line treatment for patients with NAFLD who are overweight and obese [5,6,7,8,9]. However, the ideal diet and physical activity (PA) regimen remains uncertain because previous studies have varied in their outcome measures, the diversity of NAFLD phenotypes, and the lengths of follow-up periods.
A low-calorie diet combined with moderate-intensity PA for an extended period is the current standard lifestyle intervention for NAFLD [9]. This approach has been reported to improve NAFLD and reduce hepatic fat [10, 11]. Recent findings have suggested that a low-carbohydrate and high-protein diet may have a superior effect on NAFLD than a low-fat diet, even with the same calorie restriction [12, 13]. Therefore, it merits investigation to determine whether a low-carbohydrate, high-protein diet is more beneficial than the traditional balanced diet for the Chinese population with NAFLD.
Previous studies indicate that lifestyle intervention for weight loss is not very effective in reality, with fewer than half of participants were able to achieve their preset weight loss goals [14]. This low success rate is influenced by various factors, such as a lack of motivation to adopt a new lifestyle and difficulties in maintaining long-term adherence through self-monitoring [15]. Some studies have suggested that an intensive lifestyle intervention (ILI), incorporating enhanced modification of diet and exercise, frequent counseling with health professionals, and application of novel monitoring techniques, have been identified as promising therapies to achieve successful weight loss and the related therapeutic goals [16,17,18,19]. This comprehensive approach has been proven to result in significant weight reduction and reduce the risk of liver fibrosis, type 2 diabetes, and other metabolic diseases in adults with NAFLD with obesity or glucose abnormalities [16, 20,21,22]. However, most studies have focused on European and American populations, which differ from Asian populations in terms of race, culture, lifestyle, and socioeconomic factors. Additionally, the BMI reference indices for diagnosing obesity and overweight in China differ from those in the West, raising questions about the applicability of the ILI model to Chinese patients with NAFLD.
Currently, no high-quality evidence has elucidated the effect of intensive lifestyle interventions on Chinese patients with NAFLD. A recent multicenter study (ChiCTR1800017463) demonstrated that ILI was effective for both weight management and NAFLD improvement in Chinese adults with obesity [19]. However, the study used the nonalcoholic fatty liver disease score (NFS). This serological formula is less efficient and precise than FibroTouch, FibroScan, or magnetic resonance elastography to evaluate liver steatosis and fibrosis. Therefore, we designed a 12-week multicenter randomized controlled trial (RCT) to examine the effect of a comprehensive ILI approach on overweight and obese patients with NAFLD in the Chinese population. We hypothesized that our comprehensive ILI approach, consisting of a calorie-restricted diet (CRD) with low-carbohydrate and high-protein, exercise, and frequent dietitian-led counseling, could be superior to conventional intervention in improving hepatic steatosis, fibrosis, and other metabolic parameters in overweight and obese patients with NAFLD.
Materials and methods
Study design and participant recruitment
This study was a two-arm, multicenter, randomized controlled trial registered on ClinicalTrials.gov (registration number: NCT03972631). Participants were recruited from health management centers and nutrition outpatients of seven Chinese hospitals (the First Affiliated Hospital of Zhejiang University, the Sichuan Provincial People’s Hospital, the Qilu Hospital of Shandong University, the Affiliated Hospital of Qingdao University, Xiangya Hospital of Central South University, the Beijing Hospital, and the First Affiliated Hospital of Kunming Medical University) between August 2019 and April 2021. The study protocol was approved by the Human Ethics and Research Ethics committees of the First Affiliated Hospital of Zhejiang University School of Medicine.
Eligible participants were adults aged 18 to 65 years who had a body mass index (BMI) between 25 and 35 kg/m2 and were clinically diagnosed with NAFLD by radiological assessment (ultrasound, computed tomography, or magnetic resonance imaging) [23]. The exclusion criteria are listed in detail in Supplementary Table 1. Before enrollment, all participants were required to sign an informed consent form. At enrollment, demographic data such as age, anthropometry, gender, ethnicity (Han or other), education, marital status, and comorbidities were obtained. Eligible participants were assigned to the ILI or control groups in a 1:1 ratio. This allocation was performed using a computer-generated random sequence stratified by center and gender. Details of the allocation were stored confidential in files on the lifestyle management platform operated by Zhejiang Nutriease Co., Ltd., Hangzhou.
Lifestyle intervention
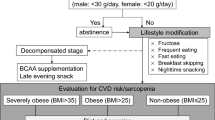
During the 12 weeks of the trial, participants in both groups were asked to follow a restricted-energy content (initial weight×25 kcal/kg×0.7). After randomization, participants in the control group were provided with a balanced CRD consisting of 45–55 E% carbohydrates, 20–30 E% fat, and 20–30 E% protein. The dietitian instructed the participants to follow a standard lifestyle intervention based on the Guidelines for the Prevention and Treatment of Nonalcoholic Fatty Liver Disease (2018, China) [24]. Participants in the ILI group were instructed to consume a low-carbohydrate, high-protein diet composed of 20–25% carbohydrate, 30–35% fat, and 40–45% protein per day. All participants were counseled to consume low glycemic index (GI) food as the primary source of carbohydrates, beans, and their products, white meat, and nuts as the main source of protein, and monounsaturated fatty acids as the main source of fat. The principle of ILI was similar to that of the control group, except for the recommendation to choose polyunsaturated fatty acids as the main source of fat. The participants of the ILI group received two nutrition bars (Zhejiang Nutriease Co Ltd, Hangzhou) weighing approximately 112 g per day to replace the staple food of lunch and dinner to help reduce carbohydrate intake while ensuring adequate protein intake. The composition of the bar is revealed in Supplementary Table 2.
Participants in the intervention group received a lifestyle intervention, which included detailed health education, specific diet modification, individualized physical exercise, mobile platform-assisted monitoring, and frequent counseling. The goal of the ILI group was to achieve a weight reduction of 10% of initial body weight. One-on-one health education was held by a dietitian who developed a personal health management plan for every participant based on their stage of obesity. Furthermore, periodic science articles on diet, exercise, and disease hazards were sent through the mobile app (NUTRIEASE 8.9.12, Notte, China) to improve participants’ nutritional knowledge and skills. Except for the three scheduled follow-ups mentioned in the control group (weeks 4, 8, and 12), participants in the ILI group had weekly counseling (lasting at least 15 min) by telephone or app message with a dietitian, who adjusted their diet and PA plans promptly and improved their adherence to the program. Regarding PA, all participants were encouraged to perform at least 150 min of moderate-intensity aerobic exercise per week and resistance exercise twice a week.
Nutrient and physical assessment
Participants were instructed to record food pictures and meal times 3 days (usually 2 weekdays and 1 weekend day) every four weeks and exercise activities using a mobile phone application (NUTRIEASE 8.9.12, Notte, China) at planned inspection visits. These logs were monitored by researchers and a dedicated dietitian, who conducted online supervision and provided feedback and recommendations using an online lifestyle management system. Dietitians estimated the daily intake of each participant based on the three-day food pictures and the nutrient content according to the nutrient content shown in the Chinese Food Composition Table [25]. Physical activity was assessed using the modified International Physical Activity Questionnaire (long-form) [26], which collected the type, intensity, frequency, and duration of exercise. The weighted metabolic equivalents of task (MET)-min per week (MET·min·wk–1) were calculated as duration×frequency per week×MET intensity and then summed across activity domains to produce a weighted estimate of total physical activity from all reported activities per week (MET·min·wk–1) [26].
Study outcomes
The primary outcome was the change in the fat attenuation parameter (FAP), a noninvasive indicator of liver fat content. Key secondary outcomes were the changes in body mass index (BMI) and liver stiffness measurement (LSM). FAP and LSM were measured with iLivTouch (Wuxi HISKY Medical Technologies Co., Ltd.) by an experienced physicist who was blinded to participants’ all clinical data and group assignment, according to the protocol by the manufacturer. The BMI was calculated as body weight in kilograms divided by the square of height in meters. Weight and height were measured after urination and defecation with fasting in the morning.
The other secondary outcomes included changes in systolic and diastolic blood pressure, body composition parameters (body fat mass, muscle mass and skeletal muscle mass), homocysteine, liver function tests (alanine aminotransferase [ALT], aspartate aminotransferase [AST], gamma-glutamyl transferase [GGT]), serum lipids (total cholesterol [TC], low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C] and triglycerides [TG]), glucose metabolism biomarkers (fasting blood glucose [FBG], fasting insulin [FINS], glycosylated hemoglobin A1c [HbA1c], Homeostasis Model Assessment of Insulin Resistance [HOMA-IR] and Homeostasis Model Assessment of Beta-cell function [HOMA-β]).
Blood pressure was recorded as the average of two measures while participants were in a seated position after at least 10 min of rest. Body composition was measured while standing on an automated hand-to-foot bioelectric impendence device named the Inbody 770 analyzer (In Body Co., South Korea) with bare feet and light clothing. All subjects strictly followed the instrument’s voice instructions under the supervision of the researchers. Blood samples were collected in the morning after fasting overnight. The Cobas c702 module (Roche Ltd) was used to determine FBG, liver function test, serum lipids, and homocysteine. FINS was assessed using Abbott i2000. HbA1c was detected using Tosoh’s HLC-723G8 automated glycohemoglobin analyzer. HOMA-IR was calculated from fasting plasma glucose and insulin concentrations using the formula: FBG (mmol/L)×FINS (Mu/mL)/22.5 [27, 28]. The HOMA-β was calculated using the formula: 20×FINS (Mu/mL)/[FBG (mmol/L)-3.5] [29]. All outcomes were collected at baseline and 12 weeks after the intervention started, except for BMI, which was additionally measured at 4 and 8 weeks during the intervention.
Statistical analysis
All analyses were conducted with SPSS version 25.0 (IBM, Armonk, NY, USA) and GraphPad Prism 8.0 (GraphPad Software Inc., San Diego, CA, USA). The primary outcome was the change in FPA between the two groups. The proposed standard deviation (SD) of reduction in FAP was 38 dB/m, according to a preliminary study [30]. Based on differences in treatment effect between groups and a significance level of 0.05, we estimated that an enrollment target of 214 participants (107 per group) would provide the trial with more than 80% statistical power to detect a significant difference of 15 dB/m in FAP between the two interventions. After accounting for an anticipated 20% dropout rate, a total of 257 participants were computed.
The per-protocol analysis set was used to perform all efficacy analyses. No additional imputation methods were applied since the missing data was scarce. Descriptive data were reported as mean ± SD or median (25th, 75th percentile), depending on whether the normal distribution assumptions were met, and categorical data are described with proportions. Differences in the trial outcomes between the two groups were evaluated with the use of the \({\chi }^{2}\) test or Fisher’s test for the categorical variables and the t-test or Mann–Whitney U test for the continuous variables. The Shapiro‒Wilk test was used to assess the normality of continuous data. An analysis of covariance (ANCOVA) was performed for primary and secondary outcomes, with treatment as a factor and the baseline value as the continuous covariate. When the assumptions for the ANCOVA were not met, nonparametric ANCOVA was used. Rate difference was calculated with Newcombe method.
The primary outcome was conducted for prespecified subgroup analyses by gender (male vs. female), age category (< 35 vs. ≥ 35 y), BMI category (< 28 vs. ≥ 28 kg/m2), ethnicity (Han vs. others), hyperlipidemia (yes vs. no) and hypertension (yes vs. no). We used an interaction term between treatment status and subgroup to assess effect modification by subgroup status.
Grouping differences of the trial outcomes were presented as least-squares (LS) means with 95% confidence intervals (CI). Statistical tests were two-tailed and considered significant when p < 0.05 for the primary outcome. To control for type I errors, two key secondary outcomes with Bonferroni correction. The threshold for statistical significance was p < 0.025. The p-value of other secondary outcomes and subgroup analyses were not adjusted for multiple testing and should be interpreted as exploratory.
Results
Study flow and characteristics of the participants at baseline
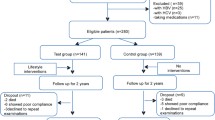
The recruitment process included 254 pre-screenings (Fig. 1). Twenty-eight individuals were excluded because of failure to meet the inclusion criteria (n = 6), unwillingness to participate (n = 19), and other reasons (n = 3). A total of 226 participants were included in the initial study and randomly assigned to the control group (n = 115) and the ILI group (n = 111). Due to the restrictions imposed by the COVID-19 epidemic, recruitment and follow-up became more difficult than expected. Finally, a total of 169 studies were completed (per protocol analysis), and statistical power was secured to evaluate primary and secondary outcomes. Most participants were male (62.7%) and of Han nationality (91.7%), with a mean age of 36.7 (30.8 ~ 41.6) years. The mean BMI was 29.2 (27.1~31.2) kg/m2.
The baseline characteristics of the 79 participants in the ILI group and 90 participants in the control group were well-balanced. No significant difference was found in gender, age, anthropometry (e.g., weight, height, and BMI), ethnicity, or marital status between the two groups (Table 1).
Effect on the liver outcome
After 12 weeks of lifestyle intervention, both groups showed a significant decrease in FAP. The mean FAP level in the control group at week 12 was 284.39 ± 27.31 dB/m, while in the ILI group, it dropped to 267.24 ± 25.56 dB/m (Table 2). The reduction in FAP levels was significantly more significant in the ILI group than in the control group (32.39 ± 28.84 vs. 17.05 ± 20.69 dB/m, p < 0.001). The covariance model also confirmed that ILI was more effective than the standard intervention in reducing the FAP level (LS mean difference: 16.07 [95% CI: 8.90–23.25] dB/m, p < 0.001), which implied that the ILI was superior to the standard intervention in reducing FAP levels in NAFLD (Fig. 2).
LSM was significantly decreased by 1.17 ± 1.93 kPa in the ILI group and 0.72 ± 1.78 kPa in the control group (p < 0.001, Fig. 3a). There were no significant differences between the two groups in improving liver fibrosis (LS mean difference: 0.20 [95% CI: -0.19-0.59] kPa, p = 0.317).
Liver enzymes, including ALT, AST, and GGT, were all significantly reduced in both groups after 12 weeks of intervention (p < 0.05, Table 2). The reduction of ALT, AST and GGT in the ILI group was more significant than that in the control group (LS mean differenceALT: 4.06 [95% CI: 1.12–7.01]U/L, pALT=0.007; LS mean differenceAST:2.20 [95% CI: 0.21–4.22]U/L, pAST=0.030 and LS mean differenceGGT: 7.82 [95% CI, 5.17–10.47]U/L, pGGT<0.001).
Change in FAP level from baseline to TP12. The change in FAP level was 32.69 dB/m in the intervention group and 17.05 dB/m in the control group. The covariance model showed that the intervention group was significantly better than the control group in reducing the FAP level (LS mean difference: 16.07 [95% CI: 8.90–23.25] dB/m, p < 0.001)
Change in LSM and BMI from baseline to TP12. (a) Change in LSM from baseline to TP12. The ILI group had a more significant decrease in LSM than the control group (1.17 ± 1.93 kPa vs. 0.72 ± 1.78 kPa, respectively). The covariance model showed no significant difference between the two groups in reducing the LSM level (LS mean difference: 0.20 [95% CI: -0.19-0.59] kPa, p = 0.317). (b) Change in BMI from baseline to TP12. The ILI group had a more significant decrease in BMI than the control group (2.68 ± 1.12 kg/m2 vs. 1.21 ± 1.34 kg/m2, respectively). The covariance model showed that the ILI group was significantly better than the control group in reducing the BMI level (LS mean difference: 1.46 [95% CI, -1.09-1.82] kg/m2, p < 0.001)
Effect on anthropometry and body composition
As indicated in Fig. 3b, the ILI group had a significantly higher reduction in BMI than the control group (2.68 vs. 1.21 kg/m2, LS mean difference 1.46 [95% CI: -1.09-1.82] kg/m2, p < 0.001). The proportion of participants who achieved the goal of BMI reduction (≥ 10%) was 40.5% (32/79) in the ILI group and 10.1% (9/89) in the control group (difference of change: 30.4% [95% CI: 16.6 – 43.1%], p < 0.001). Body composition analysis also revealed that both groups experienced a reduction in body fat mass and muscle mass after 12 weeks of intervention (p < 0.05). However, only the ILI group had a reduction in skeletal muscle mass (p < 0.05).
Effect on lipid metabolism and insulin resistance
TG decreased in both groups but to a significantly larger extent in the ILI group than in the control group (LS mean difference: 0.27 [95% CI: 0.11–0.42] mmol/L, p = 0.001). The two groups showed no significant difference in TC, LDL-C, and HDL-C. However, in the control group, TC improved significantly after 12 weeks of intervention (p < 0.05). Fasting insulin, HbA1c, HOMA-IR, and HOMA-β were all decreased in both groups, and the reductions were significantly more significant in the ILI group than in the control group (p < 0.05). However, no significant change was found between groups in lowering the FBG (LS mean difference: 0.09 [95% CI: -0.05-0.20] mmol/L, p = 0.209). Fasting blood glucose decreased significantly from baseline to week 12 in the ILI group (p < 0.05), while the control group did not have a significant change.
Effect on cardiovascular risk factors
The effects of ILI on blood pressure and homocysteine are displayed in Table 2. Compared to the control group, the decrease in SBP and DBP was significantly higher in the ILI group (LS mean difference SBP: 3.41 [95% CI: 0.81–6.00] mmHg, pSBP =0.011 and LS mean difference DBP: 2.83 [95% CI: 0.77–4.90] mmHg, pDBP =0.008). After 12 weeks of treatment, SBP and DBP in the ILI group were significantly lower than the baseline values (p < 0.05). In contrast, the control group only significantly improved SBP (p < 0.05).
Homocysteine (Hcy) is recognized as a potential predictor of subclinical atherosclerosis and correlates with cardiovascular disease prevalence [31]. ILI was more effective than the conventional intervention in lowering Hcy levels (LS mean difference: 0.98 [95% CI: 0.29–1.66] µmol/L, p = 0.006]. Furthermore, only the ILI group had a significant decrease in Hcy levels from baseline (10.00 ± 3.06 vs. 11.85 ± 4.77 µmol/L, p < 0.05).
Assessment of dietary intake and physical activity
At baseline, there were no significant differences in total energy intake, dietary intake, or physical activity (Table 3). At the end of the study, both groups significantly reduced total energy and carbohydrate intake. However, members of the ILI group significantly increased protein and fiber intake (Table 3). Fat intake remained unchanged between baseline and week 12 in both groups. An increase in energy from protein and fat was also observed at week 12, with a significant difference between the two groups. At 12 weeks, physical activity improved significantly within the ILI group (98.4 ± 8.1vs. 69.3 ± 80.3 MET-h/week, p < 0.05) but did not differ between the two groups or within the control group.
Subgroup analysis
We performed a prespecified subgroup analysis to examine whether demographic factors influenced the effect of the intervention on FAP (Fig. 4). We stratified the participants by gender (male/female), age (< 35/ ≥35 y), BMI (< 28/ ≥28 kg/m2), ethnicity (Han Chinese/others), hyperlipidemia (yes/no), and hypertension (yes/no). The results showed that there was no significant treatment heterogeneity in FAP reduction between the two intervention groups by age, gender, ethnicity, and hyperlipidemia, except hypertension (p-value for interaction < 0.001). However, within the ILI group, the participants who were male (LS mean difference: 16.55 [95% CI: 7.97–21.12] dB/m), had BMI ≥ 28 kg/m2 (LS mean difference: 22.01 [95% CI: 13.39–30.62] dB/m) or belonged to Han Chinese (LS mean difference: 16.95 [95% CI: 9.68–77.15] dB/m) had a more significant decrease in FAP than their counterparts.
Adverse events
During 12 weeks of intervention, the most common adverse events were gastrointestinal symptoms, such as constipation (two participants in the ILI group and one in the control group) and diarrhea (two participants in the ILI group). Four participants had upper respiratory tract infections (three in the ILI group and one in the control group). Four participants suffered joint sprains during exercise (two in the ILI group and two in the control group). In the ILI group, there were also reports of fatigue, pneumonia, lymphadenitis, and serum creatinine (one each). In the control group, there were also reports of knee pain, depression, and a car accident (one, two, and one, respectively). The other adverse events unrelated to the interventions are presented in Supplementary Table 3.
Discussion
In this multicenter randomized controlled trial, both lifestyle intervention strategies significantly decreased FAP, LSM, and liver enzymes in patients with NAFLD. However, our comprehensive ILI approach produced more substantial reductions in FAP and liver enzymes compared to the traditional interventions described in the current guidelines. Furthermore, the ILI approach markedly improved extrahepatic parameters, including BMI, body composition, blood pressure, homocysteine levels, triglycerides, and insulin resistance. These findings indicate that our ILI method is more effective in managing weight and improving metabolic health in overweight or obese NAFLD patients in China.
In our study, specific diet modifications played an essential role in the intensive lifestyle intervention. We found that a CRD with low carbohydrate and high protein, compared with the balanced diet with the same energy limitation used in the conventional intervention, was more effective in NAFLD management. A calorie reduction of 500 to 1000 kcal per day in a CRD regimen, as recommended by most guidelines, can improve intra- and extrahepatic metabolism by decreasing insulin resistance, improving liver inflammation, and altering gut microbiota [23]. Notably, the total calorie reduction and the optimal composition of macronutrients (carbohydrate, fat, and protein) in a diet design contributed to the metabolic outcomes. Specifically, low-carbohydrate diets have shown remarkable therapeutic efficacy in metabolic regulation and thus have been increasingly applied in treating obesity, NAFLD, and other metabolism-related diseases. Based on the advantages of low-carbohydrate diets in increasing energy expenditure and decreasing body weight observed in many preclinical studies [32], a low-carbohydrate diet has been validated to be more effective in reducing the intrahepatic fat content than a simple hypocaloric diet [33, 34]. The underlying mechanisms involved reduced hepatic de novo lipogenesis (DNL) by restricting glucose or fructose intake, which led to decreased synthesis of fatty acids and accumulation of intra-liver fat [35]. Another underlying mechanism was the improved insulin resistance by low carbohydrate diets, which enhanced lipolysis and reduced fatty acids delivered to the liver [36]. In the context of calorie restrcition, low-carbondydrate diets also have been regarded to have stronger impact on NAFLD outcomes in comparison with fat intake control [12, 34], which helps to explain the scenarios in our study that increasing fat intake in the low-carbonhydrate settings in the ILI group did not alter the final results, especially serum lipid level.
Low-carbohydrate and high-protein diets have been shown to reduce liver fat, improve glucose homeostasis, and promote weight loss in patients with metabolic syndrome and NAFLD [12]. Compared to normal or low-protein diets, high-protein diets significantly reduced liver fat content in several studies [13, 37, 38], as confirmed by our study. Further studies also suggested that high-protein diets could prevent and reverse hepatic steatosis development, regardless of dietary carbohydrate, fat, or overall caloric intake [39, 40]. High-protein diets have additional benefits for NAFLD outcomes. However, excessive protein intake can also increase serum creatine levels, as observed in one participant during the study period, indicating that renal function should be monitored in susceptible individuals.
We also found that intensive counseling enhanced the efficacy of ILI in NAFLD treatment. However, it is challenging to motivate individuals to adopt and maintain an intervened lifestyle [41], as they may face barriers such as limited food choice, exercise-induced pain and fatigue, unhealthy food cravings, and delayed benefits. Previous studies have disclosed that frequent professional counseling on medical nutrition therapy improves the outcomes of simple diet and exercise interventions [20, 42,43,44,45,46]. Therefore, we applied this strategy in our ILI approach, where the dietitians used a motivational interview with a four-step protocol (engaging, focusing, evoking, and planning) to facilitate behavioral change [41]. Notably, our intensive counseling consisted of weekly one-to-one communication supported by a smartphone app that allowed dietitians to provide timely feedback on patients’ diets and physical activity based on detailed records uploaded from mobile devices [18]. These strategies reinforced the self-monitoring behavior that led to sustained weight loss. Furthermore, as a positive result acquired in a short time, rapid weight loss in a short time could act as an incentive to increase adherence to the intervention.
Our findings also demonstrated that weight loss was a key factor in NAFLD resolution. In our study, ILIs reduced BMI by 9%, twice as much as the control group (approximately 4%). This indicated that ILIs successfully achieved the weight control goal (defined as a 7–10% reduction in initial weight) [5]. Previous clinical trials have shown that 5% weight loss after lifestyle changes improved steatosis reversion [22], normalized liver enzymes [47], and reduced the risk of diabetes and other metabolic disorders [48]. However, our results demonstrated that even a 4% BMI reduction in the control group improved multiple liver parameters, suggesting that any degree of weight control would eventually benefit NAFLD treatment. Moreover, our analyses revealed a more significant reduction in FAP and transaminase levels in the ILI group than in the control group, indicating that the beneficial effects on clinical and histological outcomes were closely associated with the degree of BMI reduction in a dose-dependent manner.
In addition to body weight, body fat distribution is another indicator of metabolic status in NAFLD, as hepatic fat content and its related metabolic parameters could decrease in NAFLD patients without noticeable changes in body weight change [49]. Therefore, analyzing body composition, especially body fat mass, is an important way to evaluate the effect of dietary intervention [50]. Our data showed a significant reduction in body fat mass in the ILI group, confirming the superior effect of ILIs on NAFLD-related metabolic disorders. Notably, ILIs also reduced muscle mass and skeletal muscle mass. This may be due to decreased muscle protein synthesis and increased muscle proteolysis caused by CRD during calorie restriction [51,52,53]. To prevent weight-induced muscle mass loss, resistance exercise training, and high protein intake should be applied [54,55,56].
Compared to conventional treatment, our comprehensive approach to ILI improves specific cardiovascular markers, such as homocysteine and systolic and diastolic blood pressure. This may be due to the low carbohydrate content, which has been proven to lower blood pressure and reduce estimated cardiovascular risk in the “Omni Heart Randomized Trial” [57]. Moreover, reducing BMI is crucial for patients with hypertension, as 1 kg of body weight loss leads to a 1 mmHg BP reduction, according to the latest guidelines for essential hypertension [58]. Interestingly, our further prespecified subgroup analysis showed that the effect of ILI on reducing intrahepatic fat was more pronounced in patients with prehypertension than in those without hypertension. There is some evidence that prehypertension is associated with the incidence and progression of NAFLD. A meta-analysis of 11 cohort studies in patients with NAFLD, confirmed by liver biopsies, showed that hypertension (HTN) at baseline almost doubled the risk of progression of fibrosis progression [59]. The activated renin-angiotensin system (RAS) in HTN may impair hepatic function by increasing oxidative stress, apoptosis, and inflammation [60]. Therefore, we speculated that the improvement in HTN could assist in inhibiting the synthesis of hepatic fat in patients with NAFLD by regulating the RAS pathway. However, the population with pre-HTN in our study was small. More studies are required to confirm this conclusion and clarify the underlying mechanism.
The strength of this article lies in one-on-one nutritional counseling coupled with a three-month follow-up, which can improve patient compliance. This mainly benefits the Chinese population, where nutritional counseling is not as common. Additionally, this study provides an analysis of dietary components, which are relatively rare among the Chinese population due to the diverse and complex nature of Chinese cuisine, making nutrient calculations challenging. We use standardized dietary software and nutritionist training to calculate the participants’ nutrient intake. However, there are some limitations in the present RCT. First, the dropout rate during follow-up was 26%, which could be impacted by unexpected quarantine policies during the COVID-19 pandemic and could potentially compromise the results of this study. Due to the pandemic-related loss of follow-up, we could not accurately perform the intention-to-treat analyses since the final status of the participants lost to follow-up was primarily unclear. Second, the duration of the intervention was only 12 weeks, during which the patients were closely monitored. Hence, the long-term benefits after the intervention period are uncertain, especially for those patients with NAFLD who returned to the normal diet after the trial. A further follow-up study should be performed to predict the long-term risk of steatosis recurrence after the intervention. Finally, our study lacks precise characterization of some variables, such as the intensity of physical activity, the intake amount of different types of unsaturated fatty acid, the histological assessment of steatosis, the unavailability of more established tools for subclinical atherosclerosis diagnosis (such as brachial-ankle pulse wave velocity in addition to the Hcy level alone), which all might introduce bias to the final results.
Conclusion
In conclusion, this 12-week multicenter randomized controlled trial demonstrated that ILIs, comprising a low-carbohydrate, high-protein calorie-restricted diet along with exercise, significantly enhanced liver steatosis and other metabolic parameters in overweight Chinese patients with NAFLD. Compared to standard interventions, the provision of diet and exercise therapy by registered dietitians at a high frequency appears to be more effective. Further research is needed to explore the long-term benefits and practicality of ILIs in real-world settings.
Data availability
The data presented in this study are available upon request from the corresponding author. The data are publicly unavailable because individual privacy may be compromised.
Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- ILI:
-
Intensive lifestyle intervention
- FAP:
-
Fat attenuation parameter
- BMI:
-
Body index mass
- CRD:
-
Calorie-restricted diet
- LSM:
-
Liver stiffness measurement
- PA:
-
Physical activity
- RCT:
-
Randomized controlled trial
- GI:
-
Glycemic index
- MET·min·wk–1 :
-
(MET)-minutes per week
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- GGT:
-
Gamma-glutamyl transferase
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- FBG:
-
Fasting blood glucose
- FINS:
-
Fasting insulin
- HbA1c:
-
Glycosylated hemoglobin A1c
- HOMA-IR:
-
Homeostasis Model Assessment of Insulin Resistance
- HOMA-β:
-
Homeostasis Model Assessment of Beta-cell Function
- SD:
-
Standard deviation
- LS:
-
Least-squares
- CIs:
-
Confidence intervals
- Hcy:
-
Homocysteine
- DNL:
-
De novo lipogenesis
- HTN:
-
Hypertension
- RAS:
-
Renin-angiotensin system
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Zhou J, Zhou F, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Epidemiological features of NAFLD from 1999 to 2018 in China. Hepatology. 2020;71:1851–64.
Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected Rapid increase in the Burden of NAFLD in China from 2008 to 2018: a systematic review and Meta-analysis. Hepatology. 2019;70:1119–33.
Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–98.
European Association for the Study of the L. European Association for the Study of D, European Association for the study of O: EASL-EASD-EASO Clinical Practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the study of Liver diseases. Hepatology. 2018;67:328–57.
Plauth M, Bernal W, Dasarathy S, Merli M, Plank LD, Schutz T, et al. ESPEN guideline on clinical nutrition in liver disease. Clin Nutr. 2019;38:485–521.
Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the study of the liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919.
Semmler G, Datz C, Reiberger T, Trauner M. Diet and exercise in NAFLD/NASH: beyond the obvious. Liver Int. 2021;41:2249–68.
Haufe S, Haas V, Utz W, Birkenfeld AL, Jeran S, Bohnke J, et al. Long-lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss. Diabetes Care. 2013;36:3786–92.
Elias MC, Parise ER, de Carvalho L, Szejnfeld D, Netto JP. Effect of 6-month nutritional intervention on non-alcoholic fatty liver disease. Nutrition. 2010;26:1094–9.
Worm N. Beyond Body Weight-Loss: dietary strategies targeting Intrahepatic Fat in NAFLD. Nutrients 2020, 12.
Xu C, Markova M, Seebeck N, Loft A, Hornemann S, Gantert T, et al. High-protein diet more effectively reduces hepatic fat than low-protein diet despite lower autophagy and FGF21 levels. Liver Int. 2020;40:2982–97.
Musso G, Cassader M, Rosina F, Gambino R. Impact of current treatments on liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of randomised trials. Diabetologia. 2012;55:885–904.
Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–84.
Arora C, Malhotra A, Ranjan P, Singh V, Singh N, Shalimar, et al. Effect of intensive weight-loss intervention on metabolic, ultrasound and anthropometric parameters among patients with obesity and non-alcoholic fatty liver disease: an RCT. Eur J Clin Nutr. 2022;76:1332–8.
Vamvakis A, Gkaliagkousi E, Lazaridis A, Grammatikopoulou MG, Triantafyllou A, Nikolaidou B et al. Impact of intensive lifestyle treatment (Diet Plus Exercise) on endothelial and vascular function, arterial stiffness and blood pressure in stage 1 hypertension: results of the HINTreat Randomized Controlled Trial. Nutrients 2020, 12.
Handelsman Y, Butler J, Bakris GL, DeFronzo RA, Fonarow GC, Green JB, et al. Early intervention and intensive management of patients with diabetes, cardiorenal, and metabolic diseases. J Diabetes Complications. 2023;37:108389.
Jiang W, Huang S, Ma S, Gong Y, Fu Z, Zhou L, et al. Effectiveness of companion-intensive multi-aspect weight management in Chinese adults with obesity: a 6-month multicenter randomized clinical trial. Nutr Metab (Lond). 2021;18:17.
Force USPST, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB et al. Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2018, 320:1163-71.
Bischoff M, Zimny S, Feiner S, Sauter J, Sydor S, Denk G, et al. Multidisciplinary lifestyle intervention is associated with improvements in liver damage and in surrogate scores of NAFLD and liver fibrosis in morbidly obese patients. Eur J Nutr. 2022;61:2725–35.
Lazo M, Solga SF, Horska A, Bonekamp S, Diehl AM, Brancati FL, et al. Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes Care. 2010;33:2156–63.
Alcoholic Liver Disease CSoHCMA, Fatty Liver Expert Committee CMDA. [Guidelines of prevention and treatment for nonalcoholic fatty liver disease: a 2018 update]. Zhonghua Gan Zang Bing Za Zhi. 2018;26:195–203.
Fan JG, Wei L, Zhuang H. National Workshop on fatty L, alcoholic liver disease CSoHCMA, fatty liver Disease Expert Committee CMDA: guidelines of prevention and treatment of nonalcoholic fatty liver disease (2018, China). J Dig Dis. 2019;20:163–73.
Yang YX. Chinese Food Ingredients Standard Edition. 6th ed. Beijing: Peking University Medical Press; 2018.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294:E15–26.
Meyer C, Pimenta W, Woerle HJ, Van Haeften T, Szoke E, Mitrakou A, et al. Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Care. 2006;29:1909–14.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Mao CS, Ning HB, He J, Yin H, Kang Y, Shang J. The value of FibroTouch fat attenuation parameter in patients with chronic hepatitis B complicated with nonalcoholic fatty liver disease. Chin J Infect Dis. 2015;33:339–42.
Popescu D, Rezus E, Badescu MC, Dima N, Seritean Isac PN, Dragoi IT et al. Cardiovascular Risk Assessment in Rheumatoid Arthritis: accelerated atherosclerosis, new biomarkers, and the effects of Biological Therapy. Life (Basel) 2023, 13.
Kennedy AR, Pissios P, Otu H, Roberson R, Xue B, Asakura K, et al. A high-fat, ketogenic diet induces a unique metabolic state in mice. Am J Physiol Endocrinol Metab. 2007;292:E1724–39.
Browning JD, Baker JA, Rogers T, Davis J, Satapati S, Burgess SC. Short-term weight loss and hepatic triglyceride reduction: evidence of a metabolic advantage with dietary carbohydrate restriction. Am J Clin Nutr. 2011;93:1048–52.
Kirk E, Reeds DN, Finck BN, Mayurranjan SM, Patterson BW, Klein S. Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Gastroenterology. 2009;136:1552–60.
Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–51.
Lomonaco R, Ortiz-Lopez C, Orsak B, Webb A, Hardies J, Darland C, et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:1389–97.
Markova M, Pivovarova O, Hornemann S, Sucher S, Frahnow T, Wegner K et al. Isocaloric diets high in animal or plant protein reduce Liver Fat and inflammation in individuals with type 2 diabetes. Gastroenterology 2017, 152:571 – 85 e8.
Kontogianni MD, Tileli N, Margariti A, Georgoulis M, Deutsch M, Tiniakos D, et al. Adherence to the Mediterranean diet is associated with the severity of non-alcoholic fatty liver disease. Clin Nutr. 2014;33:678–83.
Garcia-Caraballo SC, Comhair TM, Verheyen F, Gaemers I, Schaap FG, Houten SM, et al. Prevention and reversal of hepatic steatosis with a high-protein diet in mice. Biochim Biophys Acta. 2013;1832:685–95.
Schwarz J, Tome D, Baars A, Hooiveld GJ, Muller M. Dietary protein affects gene expression and prevents lipid accumulation in the liver in mice. PLoS ONE. 2012;7:e47303.
Stonerock GL, Blumenthal JA. Role of counseling to promote adherence in healthy Lifestyle Medicine: strategies to improve Exercise Adherence and enhance physical activity. Prog Cardiovasc Dis. 2017;59:455–62.
Al-Shookri A, Khor GL, Chan YM, Loke SC, Al-Maskari M. Effectiveness of medical nutrition treatment delivered by dietitians on glycaemic outcomes and lipid profiles of Arab, Omani patients with type 2 diabetes. Diabet Med. 2012;29:236–44.
Dyson PA, Twenefour D, Breen C, Duncan A, Elvin E, Goff L, et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med. 2018;35:541–7.
Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, et al. Nutrition Therapy for adults with diabetes or Prediabetes: a Consensus Report. Diabetes Care. 2019;42:731–54.
Tsirou E, Grammatikopoulou MG, Theodoridis X, Gkiouras K, Petalidou A, Taousani E, et al. Guidelines for Medical Nutrition Therapy in Gestational Diabetes Mellitus: systematic review and critical Appraisal. J Acad Nutr Diet. 2019;119:1320–39.
Briggs Early K, Stanley K. Position of the Academy of Nutrition and Dietetics: the role of Medical Nutrition Therapy and registered Dietitian nutritionists in the Prevention and Treatment of Prediabetes and Type 2 diabetes. J Acad Nutr Diet. 2018;118:343–53.
Suzuki A, Lindor K, St Saver J, Lymp J, Mendes F, Muto A, et al. Effect of changes on body weight and lifestyle in nonalcoholic fatty liver disease. J Hepatol. 2005;43:1060–6.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines and the obesity society. J Am Coll Cardiol. 2014;63:2985–3023.
Mardinoglu A, Wu H, Bjornson E, Zhang C, Hakkarainen A, Rasanen SM, et al. An Integrated understanding of the Rapid Metabolic benefits of a carbohydrate-restricted Diet on hepatic steatosis in humans. Cell Metab. 2018;27:559–71. e5.
Hashimoto Y, Fukuda T, Oyabu C, Tanaka M, Asano M, Yamazaki M, et al. Impact of low-carbohydrate diet on body composition: meta-analysis of randomized controlled studies. Obes Rev. 2016;17:499–509.
Cava E, Yeat NC, Mittendorfer B. Preserving healthy muscle during weight loss. Adv Nutr. 2017;8:511–9.
Pasiakos SM, Cao JJ, Margolis LM, Sauter ER, Whigham LD, McClung JP, et al. Effects of high-protein diets on fat-free mass and muscle protein synthesis following weight loss: a randomized controlled trial. FASEB J. 2013;27:3837–47.
Villareal DT, Smith GI, Shah K, Mittendorfer B. Effect of weight loss on the rate of muscle protein synthesis during fasted and fed conditions in obese older adults. Obes (Silver Spring). 2012;20:1780–6.
Fyfe JJ, Hamilton DL, Daly RM. Minimal-dose resistance training for improving muscle Mass, Strength, and function: a narrative review of current evidence and practical considerations. Sports Med. 2022;52:463–79.
Verreijen AM, Engberink MF, Memelink RG, van der Plas SE, Visser M, Weijs PJ. Effect of a high protein diet and/or resistance exercise on the preservation of fat free mass during weight loss in overweight and obese older adults: a randomized controlled trial. Nutr J. 2017;16:10.
Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2012;96:1281–98.
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–64.
Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Beyond salt: lifestyle modifications and blood pressure. Eur Heart J. 2011;32:3081–7.
Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–54. e1-9; quiz e39-40.
Putnam K, Shoemaker R, Yiannikouris F, Cassis LA. The renin-angiotensin system: a target of and contributor to dyslipidemias, altered glucose homeostasis, and hypertension of the metabolic syndrome. Am J Physiol Heart Circ Physiol. 2012;302:H1219–30.
Acknowledgements
We would like to thank Dr. Liying Guan from Shandong Provincial Hospital and Dr. Dongai Yao from Zhongnan Hospital of Wuhan University for their attendance in patient enrollment.
Funding
This study was financially supported by China Health Promotion Foundation (No. CHPF2018-NAFLD).
Author information
Authors and Affiliations
Contributions
The authors’contributions were as follows: L.Z and Z.Q designed the research; J.P.P, L.Y.P, Z.Z.M, W.M, C.S.Y, W.Y, Z.C, Y.R, L.C.B, S.P, and T.C.H conducted the research and performed data collection; L.Z, W.X.M and Z.Q supervised the implementation; J.P.P, L.C.B and L.N performed the statistical analysis; L.Z and J.P.P wrote the manuscript draft; L.Z and Z.Q contributed to the critical revision of the manuscript. All the authors have read and approved the final manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present trial was approved by the Ethics Committee of First Affiliated Hospital, Zhejiang University School of Medicine (protocol code: 2018 Research Review No. 535 and date of approval: 3 May 2018). All participants completed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Z., Jin, P., Liu, Y. et al. A comprehensive approach to lifestyle intervention based on a calorie-restricted diet ameliorates liver fat in overweight/obese patients with NAFLD: a multicenter randomized controlled trial in China. Nutr J 23, 64 (2024). https://doi.org/10.1186/s12937-024-00968-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-00968-8