Abstract
Purpose
Whole grains have recently been promoted as beneficial to diabetes prevention. However, the evidence for the glycemic benefits of whole grains seems to conflict between the cohort studies and randomized control trials (RCTs). To fill the research gap, we conducted a meta-analysis to determine the effects of whole grains on diabetes prevention and to inform recommendations.
Methods
We searched PubMed, Clarivate Web of Science, and Cochrane Library until March 2024. We used the risk ratio (RR) of type 2 diabetes to represent the clinical outcomes for cohort studies, while the biomarkers, including fasting blood glucose and insulin, HbA1C, and HOMA-IR, were utilized to show outcomes for RCTs. Dose-response relationships between whole grain intakes and outcomes were tested with random effects meta-regression models and restricted cubic splines models. This study is registered with PROSPERO, CRD42021281639.
Results
Ten prospective cohort studies and 37 RCTs were included. Cohort studies suggested a 50 g/day whole grain intake reduced the risk of type 2 diabetes (RR = 0.761, 95% CI: 0.700 to 0.828, I2 = 72.39%, P < 0.001) and indicated a monotonic inverse relationship between whole grains and type 2 diabetes rate. In RCTs, whole grains significantly reduced fasting blood glucose (Mean difference (MD) = -0.103 mmol/L, 95% CI: -0.178 to -0.028; I2 = 72.99%, P < 0.01) and had modest effects on HbA1C (MD = -0.662 mmol/mol (-0.06%), 95% CI: -1.335 to 0.010; I2 = 64.55%, P = 0.05) and HOMA-IR (MD = -0.164, 95% CI: -0.342 to 0.013; I2 = 33.38%, P = 0.07). The intake of whole grains and FBG, HbA1C, and HOMA-IR were significantly dose-dependent. The restricted spline curves remained flat up to 150 g/day and decreased afterward. Subgroup analysis showed that interventions with multiple whole-grain types were more effective than those with a single type.
Conclusion
Our study findings suggest that a daily intake of more than 150 g of whole grain ingredients is recommended as a population approach for diabetes prevention.
Similar content being viewed by others
Introduction
Type 2 diabetes is a major global concern for human health and life expenditure. According to the International Diabetes Federation, an estimated 536.6 million people have been living with the rising burden of diabetes since 2021 [1]. Type 2 diabetes has several causes, among which unhealthy diets have been recognized as one of the most paramount contributors to the current global epidemic. In particular, individuals consuming carbohydrates of poor quality are linked to a higher risk of developing type 2 diabetes with the estimation that grains contribute approximately half of daily calorie intakes [2]. Thus, whole grains, often considered higher-quality sources of carbohydrates, have been highly promoted for their glycemic benefits [2, 3]. Defined by the HEALTHGRAIN Consortium, whole grains are intact, ground, cracked, or flaked grain kernels that contain all three anatomical components (endosperm, bran, and germ) in their original proportions [4]. To date, dietary strategies that focus on grain intake are still limited, especially for whole grains. While the current guidelines are only available to a general population and are irrespective of the risk level of individual health outcome [5,6,7,8,9,10], specific recommendations targeting type 2 diabetes prevention and management are urgently needed.
Shaping the population-level whole grain guidelines into a preventive recommendation for type 2 diabetes is a challenging goal that demands building an evidence base for observational studies and interventions. Previous reviews have evaluated evidence from prospective cohort studies and RCTs, proposing that the strength of the evidence from observational studies should support promoting whole grains for type 2 diabetes prevention [11,12,13,14]. However, the intervention effects in RCTs remain conflicting and not as pronounced as in cohort studies [15,16,17,18,19]. The variations in the doses and types of whole grains (mixed vs. single) and the health status of participants (healthy vs. metabolically abnormal) contribute to considerable variations in glycemic impacts. For example, consuming different types of whole grains might result in diverse metabolic outcomes because β-glucan in oats may barely slow the absorption of carbohydrates. At the same time, arabinoxylan rich in rye and wheat may increase the gut energy excretion [20]. Besides, the postulated dose-dependency of whole grains has rarely been investigated in RCTs to capture a sufficient dose on glycemic control, mostly due to ununified calculations of whole grain ingredients across products [13, 21]. Considering the contextual complexity of whole grain interventions, while numerous efforts have been made in intervention evaluations [22,23,24,25,26], the evidence to date would not be sufficient to reshape the dietary guidelines to reduce population type 2 diabetes risk. Thus, a combination of systematic and dose-dependent evaluations that elucidate the effectiveness and heterogeneity of RCTs would greatly help the continuing development of whole grain recommendations for type 2 diabetes.
Hence, this systematic review and meta-analysis aimed to evaluate the association between whole grain intake and incidence of type 2 diabetes in prospective cohort studies and then the effects of whole grains on the markers of glycemic control for RCTs. Subgroup analysis and dose-response curve would also be formulated to help illustrate the differences between cohort studies and RCTs and derive a quantitative recommendation for the daily consumption of whole grain ingredients to prevent type 2 diabetes.
Materials and methods
Protocol and data collection
We performed a systematic review and meta-analysis of prospective cohort studies that assessed the effects of whole grains on the occurrence of type 2 diabetes and RCTs that evaluated whole grain consumption on glycemic control. The protocol of the systematic review has been published on the PROSPERO register (http://www.crd.york.ac.uk/prospero/) under registration number CRD42021281639. PICO strategy (Supplementary Table 1) and detailed methods are presented in the electronic supplementary material (ESM) Methods. To summarize, we searched PubMed, Clarivate Web of Science, and Cochrane Library until March 2024. Eligible studies were those that examined the effect of whole grains on the risk of type 2 diabetes for prospective cohort studies or intermediate glycemic biomarkers for RCTs. The quality of the cohort studies was assessed using the well-established Newcastle-Ottawa Scale (NOS) tool [26], while the Cochrane Risk of Bias Assessment tool [27] was utilized to evaluate the quality of the RCTs (Supplementary Tables 2 and 3).
Data synthesis
Random-effects models were utilized to calculate the overall effect size using risk ratios (RRs) and hazard ratios (HRs) for assessing the occurrence of type 2 diabetes and mean differences for glycemic biomarkers. I2 statistic was used to assess between-study heterogeneity; a value over 50% indicated a significant level of heterogeneity. One-study-removed sensitivity analyses were obtained to determine whether removing any study could cause significant changes to the results. The possibility of a publication bias was examined by the visual inspection of funnel plots and the application of Begg’s test. For the dose-response analysis, all whole grain intakes were transformed into whole grain ingredients in g/day and tested with random effects meta-regression models and restricted cubic splines models [13, 14].
For RCTs, we did further subgroup analysis to detect probable sources of heterogeneity with a random effects model. Subgroup analyses included stratification for lengths of intervention (< 12 weeks or ≥ 12 weeks), types of study design (parallel or crossover), whole grain products variety (1–2 types or ≥ 5 types of whole grain products), types of whole grain (wheat, rice, mix or others), health status (generally healthy or unhealthy), baseline BMI, baseline age, baseline triglycerides and quality of studies (low risk, uncertain and high risk). Types of whole grain products refer to several major food categories containing whole grain ingredients, including bread (bread rolls, muffins, biscuits, etc.), cereal (ready-to-eat and hot cereal), grains (pasta, rice, etc.), grain-based desserts (cookies, cakes, pies, chips, etc.) and mixed dishes (pizza, salads, etc.). The “Generally healthy subgroup” included healthy individuals as well as overweight or obese people, and the “unhealthy subgroup” had studies on individuals with pre-diabetes, diabetes, metabolic syndrome, or at risk of metabolic disease (participants with at least one impaired glucose, lipid, or blood pressure). All analyses were conducted using R 4.0.2 software with “metafor” and “dosresmeta” packages. P values < 0.05 were considered statistically significant.
Results
Flow and characteristics of the included studies
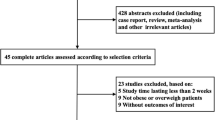
A flow chart of study identification was shown in Fig. 1. Ten prospective cohort studies with 473,019 adults [27,28,29,30,31,32,33,34] and 37 RCTs with 3136 participants [22,23,24, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] were included in the meta-analyses. Characteristics of the included studies were shown in Tables 1 and 2. For cohort studies, 6 studies were performed in the United States [27, 29, 33, 34], 2 in the Sweden Field [30, 32], 1 in the Finland Field [28], and 1 in the Denmark [32]. Follow-up years ranged from 6 to 40 years, and whole grain ingredient consumption ranged from 0.15 g/day to 151 g/day. There were 7 cohort studies classified as low risk of bias and 3 with moderate risk of bias (Supplemental Table 1).
Out of 37 RCTs, 14 studies were performed in Asia [22, 23, 38, 42, 46, 50, 55, 58, 61, 63, 65,66,67,68], 10 in the North America [24, 35,36,37, 41, 48, 49, 51, 56, 60], 12 in Europe [40, 43,44,45, 47, 52,53,54, 57, 59, 62, 64], and 1 in Australia [39]. Intervention duration was from 3 weeks to 2 years, and whole grain ingredient consumption ranged from 22.5 g/day to 207 g/day. Some RCTs had high-performance bias because they failed to implement blind intervention on subjects, and no other significant sources of bias were observed (Supplemental Table 2).
The association of whole grains and type 2 diabetes
Ten cohort studies were included in the analysis of whole grains and type 2 diabetes risk, in which 47,023 diabetic cases were reported among 473,019 participants. The summary RR for 50 g/day intake of whole grain ingredient was 0.761 (95% CI: 0.700 to 0.828, I2 = 72.39%, P < 0.001, Fig. 2). According to the Begg’s test (Kendall’s tau = -0.20, P = 0.48) and the visual inspection of the funnel plot (Supplemental Fig. 1), no evidence of publication bias was found. A sensitivity analysis revealed that the overall estimate did not depend on any single study.
Dose-response analyses indicated that the risk of type 2 diabetes was dose-dependent (β = -0.0052 (g/day)−1; 95% CI: -0.0067 to -0.0037). A nonlinear, inverse association (Pnon−linearity = 0.01) was observed between the whole grain ingredient intake and type 2 diabetes occurrence (Fig. 3), with a reduction in risk lower than 50 g/day and the association was attenuated for higher values. Given the limited number of cohort studies, the subgroup analysis was not performed.
The association of whole grains and fasting blood glucose
In total, 37 RCTs accounting for 3116 subjects reported FBG changes for the whole grain interventions. FBG after intervention was significantly lower compared with the control groups (MD = -0.103 mmol/L, 95% CI: -0.178 to -0.028; I2 = 72.99%, P < 0.01; Fig. 4). According to Begg’s test (Kendall’s tau = -0.12, P = 0.30) and the visual inspection of the funnel plot (Supplemental Fig. 2), no evidence of publication bias was found. A sensitivity analysis revealed that the overall estimate did not depend on any single study. Replacing the baseline to follow-up correlation with either 0.5 or 0.9, the relationship between FBG and the whole grain intervention did not change (MD = -0.091 mmol/L, 95% CI: -0.162 to-0.020; I2 = 61.37%, P < 0.01; MD = -0.124 mmol/L, 95% CI: -0.208 to-0.004; I2 = 88.02%, P < 0.01, respectively). Replacing studies with the most extended follow-up years or the latest data to shorter and earlier ones in studies based on the same group of participants, the relationship between FBG and the whole grain intervention did not change.
In subgroup analysis (Table 3), we found that whole grain product variety, whole grain types and health status contributed to the between-study heterogeneity. Significant reductions in FBG were observed in studies conducted with ≥ 5 whole grain products (MD = -0.101 mmol/L; 95% CI: -0.154 to -0.048; I2 = 19.41%, P < 0.001), those intervened with mixed whole grain (MD = -0.092 mmol/L; 95% CI: -0.148 to -0.035; I2 = 22.95%, P = 0.03), and those intervened with brown rice (MD = -0.305 mmol/L; 95% CI: -0.564 to -0.045; I2 = 86.66%, P = 0.02). We observed a marginally significant effect in studies conducted with 1–2 whole grain products (MD = -0.144 mmol/L; 95% CI: -0.287 to -0.001; I2 = 80.60%, P = 0.048), but no significant effect was observed in studies conducted with wheat (MD = 0.019 mmol/L; 95% CI: -0.130 to 0.168; I2 = 68.27%, P = 0.80) and other whole grain types (MD = -0.164 mmol/L; 95% CI: -0.434 to 0.106; I2 = 59.92%, P = 0.23). We also observed significant reductions in FBG in studies with low risk (MD = -0.153 mmol/L; 95% CI: -0.254 to -0.053; I2 = 77.37%, P < 0.01), compared to those with uncertain (MD = -0.091 mmol/L; 95% CI: -0.189 to 0.007; I2 = 24.51%, P = 0.07) and high risk (MD = -0.082 mmol/L; 95% CI: -0.059 to 0.223; I2 = 37.73%, P = 0.12). Furthermore, linear regression indicated that the FBG improvement was dose-dependent (β=-0.0011 mmol/L*(g/day)−1; 95% CI: -0.0021 to -0.0001, P = 0.04). We found a significant non-linear association between whole grain and FBG (Fig. 5a; Pnon−linearity = 0.04), and greater reduction was demonstrated at doses more than 150 g/day.
Nonlinear dose-response relationships between whole grain ingredients and mean differences in glycemic and insulin biomarkers in adults. (a) Fasting blood glucose (FBG). (b) Fasting blood insulin (FBI). (c) Glycated hemoglobin (HbA1C). (d) Homeostatic model assessment for insulin resistance (HOMA-IR)
The association of whole grains and fasting blood insulin
In total, 25 RCTs accounting for 2142 subjects reported fasting blood insulin for the whole grain interventions. There was no significant reduction in fasting blood insulin after the whole grain intervention (MD = -1.324 pmol/L, 95% CI: -3.611 to 0.963; I2 = 0% P = 0.26; Supplemental Fig. 3). No evidence of publication bias was found (Supplemental Fig. 4). A sensitivity analysis revealed that the overall estimate did not depend on any single study. Linear regression showed a negative but insignificant relationship between whole grain ingredient intake and FBI changes (β = -0.041 pmol/L*(g/day)−1; 95% CI: -0.097 to 0.015, P = 0.14). When the restricted spline model was implicated (Fig. 5b; Pnon-linearity =0.12), we observed an inverted U-shaped curve.
The effects of whole grains on glycated hemoglobin
In total, 13 RCTs accounting for 1043 subjects reported HbA1C for the whole grain interventions. Pooling these effect sizes (Supplemental Fig. 5), we found a modest effect of whole grain consumption on HbA1C (MD = -0.662 mmol/mol (-0.06%), 95% CI: -1.335 to 0.010; I2 = 64.55%, P = 0.053). According to Begg’s test (Kendall’s tau = -0.44, P = 0.04) and the funnel plot (Supplemental Fig. 6), no evidence of publication bias was found. A sensitivity analysis revealed the influence of a study by Kristensen et al. [59], with the results demonstrating some beneficial effects of whole grain on HbA1C (MD = -0.820 mmol/mol (-0.08%), 95% CI: -1.585 to -0.051; I2 = 62.92%, P = 0.04). It was worth noting that in that study, a non-compliance of 60% was reported.
In subgroup analysis (Table 3), study design, intervention duration and health status contributed to the between-study heterogeneity. We observed a significant effect of whole grain on HbA1C in the studies with crossover design (MD = -1.889 mmol/mol (-0.17%); 95% CI: -3.519 to -0.259; I2 = 72.61%, P = 0.02), those conducted in unhealthy participants (MD = -1.339 mmol/mol (-0.12%); 95% CI: -2.598 to -0.080; I2 = 71.58%, P = 0.04) and those with duration < 12 w (MD = -2.018 mmol/mol (-0.18%); 95% CI: -3.683 to -0.353; I2 = 71.56%, P = 0.02). We did not observe any significant effect in the studies with parallel design (MD = 0.053 mmol/mol (0.01%); 95% CI: -0.322 to 0.428; I2 = 0%, P = 0.78), those conducted in generally healthy participants (MD = 0.041 mmol/mol (0.004%); 95% CI: -0.369 to 0.452; I2 = 0%, P = 0.83) and those with duration ≥ 12 w (MD = 0.055 mmol/mol (0.01%); 95% CI: -0.319 to 0.428; I2 = 0%, P = 0.78). Linear regression indicated that the HbA1C improvement was dose-dependent (β = -0.027 mmol/mol*(g/day)−1; 95% CI: -0.051 to -0.003, P = 0.02). We discovered a significant non-linear association between whole grain and HbA1C, (Fig. 5c; Pnon−linearity = 0.04), and greater reduction was observed at doses more than 120 g/day.
The association of whole grains and HOMA-IR
In total, 15 RCTs accounting for 1254 subjects reported HOMA-IR for whole grain intervention. Pooling these effect sizes (Supplemental Fig. 7), we observed a modest effect of whole grain consumption on HOMA-IR (MD = -0.164, 95% CI: -0.342 to 0.013; I2 = 33.38%, P = 0.07). According to Begg’s test (Kendall’s tau = -0.20, P = 0.32) and the funnel plot (Supplemental Fig. 8), no evidence of publication bias was found. A sensitivity analysis revealed the influence of a study by Xue et al. [67], with the results demonstrating some beneficial effects of whole grain on HOMA-IR (MD = -0.203, 95% CI: -0.373 to -0.032; I2 = 23.24%, P = 0.02). However, in that study, poor compliance in the whole grain group was reported by the assessment of plasma alkylresorcinol.
In subgroup analysis (Table 3), we found that whole grain product variety could contribute to the between-study heterogeneity. We observed a significant effect on HOMA-IR in studies conducted with ≥ 5 whole grain products (MD = -0.229; 95% CI: -0.440 to -0.019; I2 = 0%, P = 0.03) while we did not observe any significant effect in studies that conducted with 1–2 whole grain products (MD = -0.120; 95% CI: -0.413 to 0.174; I2 = 54.72%, P = 0.42). Linear regression indicated that the HOMA-IR improvement was dose-dependent (β = -0.0049 (g/day)−1; 95% CI: -0.171 to -0.031, P = 0.01). We observed a significant non-linear relationship between whole grain consumption and HOMA-IR (Fig. 5d; Pnon-linearity < 0.001), with a greater reduction observed at doses exceeding 150 g/day.
Discussion
Summary of findings
Our systematic meta-analyses demonstrated the probable benefits of whole grain consumption for glycemic control. The summary from prospective cohort studies indicated that a 50 g/day intake of whole grain ingredients would protect against type 2 diabetes with a 25% reduction in the relative risks. Such findings were partially supported by RCTs, which indicated that an all-around improvement of glycemic markers could be obtained by an intake of 150 g/day of whole grain ingredients. Specifically, whole grain intake could improve fasting blood glucose, with modest effects on glycated hemoglobin and insulin resistance. However, there was no significant difference in fasting blood insulin. Furthermore, a combination of whole grains should be encouraged because participants who intervened with various whole grain products achieved greater glycemic control in RCTs.
Comparisons with the existing literature
Evaluating evidence for nutritional guidance across multiple study designs might be challenging. The impacts of such evaluations should be collected at a system level from prospective cohort studies of clinical endpoints and controlled trials of intermediate pathways [69]. Previous prospective cohort studies provided assessments of whole grain consumption over the long term (from 6 to 40 years) in a large number of participants (n = 473,019), providing sufficient time for the etiologies of diet-related chronic disease. However, these cohort studies were carried out on participants from limited regions of the world, namely America and the Nordics, who mainly consumed whole grain wheat with narrow intake ranges. Furthermore, the cohort studies on whole grains were particularly susceptible to confounding. Whole grain intake was associated with a healthy lifestyle, such as low BMI, frequent participation in sports, and moderate alcohol intake [70, 71]. Moreover, the lack of recognition of whole grain ingredients in foods might bring a bias in self-reporting whole grain intake in dietary assessments [72]. On the contrary, RCTs were preferable to minimize confounding effects and were more generalizable. For example, this analysis included 37 RCTs conducted in 14 countries, and only 11 of 37 were on American and Nordics. In particular, 14 RCTs were conducted on Asians with high rice consumption. However, RCTs were challenging to detect notable effects in a short duration (mainly 3 to 16 weeks) among a relatively small number of participants (n = 3116). With increased intervention durations, more significant improvements in glycemic control could be observed. Nevertheless, in our study, prospective cohort studies showed a reduction in the incidence of type 2 diabetes, while RCTs demonstrated various improvements in glycemic biomarkers.
However, the results of previous meta-analyses and ours did not always corroborate. For example, Li et al. indicated significant effects of whole grains on FBG, FBI, HbA1C, and HOMA-IR. At the same time, Marventano et al. observed no significant results in those measures [18, 19]. One of the possible reasons for such controversial results could be that Li et al. included 8 studies with multiple arms conducted in the same population and were analyzed in meta-analysis as separate studies, which could bring a high risk of unit-of-analysis error. Furthermore, Marventano et al. excluded some crucial sources of whole grains (e.g., brown rice) in their meta-analysis. Moreover, these two meta-analyses both included studies with crossover design but reported the outcomes in two distinct phases.
What the study adds to the existing literature
In our meta-analysis, given prominence by the guidance of the Cochrane Handbook [73], we selected the publications with the longest follow-up years or the latest data from the publications based on the same group of participants and created single pair-wise comparisons combined with multiple arms in studies, and excluded studies with crossover design which reported the outcomes by two distinct phases [74, 75]. Also, we did not include pseudo-grain (e.g. buckwheat, Quinoa, amaranth) because people rarely eat whole grain products made by pseudo-cereal grains [72]. We hope these methodological developments could greatly help the current study, further supporting our findings that whole grain intake could significantly improve fasting blood glucose and insulin sensitivity.
Another concern for evaluating evidence from both cohort studies and interventions was the heterogeneity in the meta-analysis, which existed in both types of studies on whole grains. While this heterogeneity could not be adequately assessed for the cohorts as there were too few cohort studies, subgroup analyses of the RCTs identified potential sources of heterogeneity. A significant reduction in FBG and HOMA-IR was found in the studies with various whole grain products while whole grain products only had a borderline significant effect on FBG. In our study, participants provided with ≥ 5 whole grain products were characterized to have a diet of various whole grain products, in which participants consumed whole grain products (e.g., bread, breakfast cereal, pasta, rice, couscous, bars, snacks, et al.) in an ad libitum manner or according to menus. It was reported that whole grains could reduce hunger and increase fullness compared to refined grains, which brought a high risk of non-compliance in whole grain intervention studies [76]. Increases in whole grain choices could probably improve compliance. Moreover, the diversity in nutrient compositions of each whole grain would also lead to differential effects on glycemic control. In our study, mixed whole grains significantly reduced FBG. As for single whole grain, brown rice, rather than whole grain wheat, had a significant effect on FBG, while insufficient evidence was available for the effects of oats, barley and rye. Wheat and rye primarily contain non-viscous and poorly fermentable fibers, while oats and barley are rich in β-glucan, which is viscous and fermentable [76]. There was apparent evidence from RCTs that β-glucan could reduce glycemic and insulinemic responses by slowing the digestion of carbohydrates and promoting the growth of probiotics, while the observations from non-viscous fibers were not as apparent [77, 78]. Besides, numerous studies have demonstrated that the phenolic compounds vary among the husks of wheat, barley, oats and rice [79]. Brown rice and barley are rich in hydroxybenzoic acids, while wheat and oats are rich in hydroxycinnamic acids [80]. Also, brown rice is a good source of γ-oryzanol, phytosterols, and aminobutyric acid [81]. These bioactive compounds might help hamper oxidative stress, reduce subclinical inflammation, and inhibit α-amylase and α-glucosidase activities [11, 82]. Thus, such diversities in nutrient combinations among whole grains could synergistically impact the study outcomes. It was further argued that similar dietary advice on whole grains should be applied for both the prevention and management of type 2 diabetes [69]. Our results from the subgroup analyses of RCTs partially supported this claim. We found that participants with or at risk of metabolic diseases achieved better results on FBG and HbA1C compared with generally healthy participants. We also included factors such as baseline age and levels of triglycerides in subgroup analysis. However, the results revealed that those factors were not the primary sources of heterogeneity. All in all, our analyses of RCTs, compliant with the prospective cohort studies, suggested that the effectiveness of whole grains might vary by different types and that consuming multiple whole grain products might exert mutually reinforcing benefits on glycemic control.
Implications of our findings for policymakers
Despite the clear indications from evidence-based analyses that whole grains could improve glycemic responses in some form, dietary guidelines targeting individual consumption are lacking to help stem the emerging pandemic of type 2 diabetes. The current statements aiming at promoting whole grain consumption, such as “choosing whole grain varieties whenever you can” from the Eat Well guide from the UK government [7] and “make at least half of grains whole grains” from dietary guidelines for Americans (DGA) [6], are commonly generic and vague, and only a limited number of countries and organizations proposed quantitative recommendations ranged 45–232 g/day [9]. For instance, the EAT-Lancet Commission on Healthy Diets from Sustainable Food Systems recommended 232 g/day of whole grains to maintain energy intake. DGA recommended 48 g/day of whole grains to substitute half of daily grains [6, 8]. Indeed, the previous data might be insufficient to make separate estimations on the effects of doses, nutrition components, and processing methods. As far as we know, the dose-response meta-analyses on reducing type 2 diabetes risk focused mainly on observational studies [12, 13] but not on RCTs, representing a greater variety of intervention doses and populations. The lack of globally recognized methods of ingredient calculations in whole grain products has also made comparisons between studies challenging [72]. With the latest boom of whole grain studies and improved methodology, we should come closer to the ultimate answer: how much whole grains should be consumed to reduce type 2 diabetes risks. In this study, we conducted dose-response meta-analyses on both cohort studies and RCTs and quantified the intakes by whole grain ingredients rather than whole products. It was conservatively estimated that whole grain products contained, on average, 51% of whole grain ingredients because most countries claimed that whole grain products should contain 50 ∼ 100% whole grain ingredients. Our results from cohort studies suggested that any increase in whole grain intakes would benefit the prevention of type 2 diabetes. However, the evidence from RCTs indicated that the preventive efficacy of whole grain ingredients on glycemic control could only be obtained at doses > 150 g/day. Moreover, dose-response analysis indicated restricted generalization and residual confounding in cohort studies. Therefore, from our perspective, a feasible recommendation in type 2 diabetes prevention could be the dose ranges where cohort studies and RCTs aligned. To our knowledge, few studies reported adverse effects of high whole grain intakes on health outcomes. Collectively, advice on consuming > 150 g/day whole grain ingredients could be a low-risk public health strategy for general populations, which would be affordable and wide-reaching for country-specific cultural diets.
Strengths and weaknesses
The present study had several strengths. Arguably, the most important one was the parallel evaluations of whole grains in both prospective cohort studies and RCTs. The former approach involved the examination of the effects on type 2 diabetes, and the latter accessed the biomarkers of type 2 diabetes as outcomes. Although the dose-response effects of whole grains differed between the type 2 diabetes incidences and measures of glycemic control, aggregated data from RCTs and cohort studies could provide a solid evidence base for updating whole grain recommendations. Secondly, all the cohort studies included had a prospective design, reducing the risks of recall and selection bias. Thirdly, whole grains were proven effective in lowering fasting blood glucose and HbA1C in the studies with crossover design, which met the gold standard for randomized controlled trials. However, several limitations should also be acknowledged. Firstly, we extrapolated the whole grain ingredients by the assumption that whole grain foods contained 51% of whole grain ingredients on average. It would slightly underestimate the amount of whole grains, probably leading to underestimating the recommended whole grain intake. Future applications of a standardized methodology to calculate whole grain intake are needed. Secondly, the subgroup analyses were less reliable in the subgroups with smaller numbers of RCTs. Thirdly, testing the publication bias for limited cohort studies might be hard. In addition, treating glycemic control as the secondary outcome, as well as the small sample sizes of RCTs, might also contribute to the heterogeneity of this meta-analysis.
Conclusion
This study suggests a significant beneficial effect of whole grain consumption on glycemic control and reducing type 2 diabetes risks. Consuming more than 150 g of whole grain ingredients daily would be highly recommended to prevent type 2 diabetes in general populations. This information provides a more comprehensive evidence base for the revision of dietary recommendations on whole grains and contributes to improving public health strategies targeting type 2 diabetes prevention and management.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- FBG:
-
fasting blood glucose
- FBI:
-
fasting blood insulin
- MD:
-
mean difference
- MetS:
-
metabolic syndrome
- TG:
-
triglycerides
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119.
Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434–45. https://doi.org/10.1016/S0140-6736(18)31809-9.
Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 2018;361:k2234. https://doi.org/10.1136/bmj.k2234.
van der Kamp JW, Poutanen K, Seal CJ, Richardson DP. The HEALTHGRAIN definition of ‘whole grain’. Food Nutr Res. 2014;58. https://doi.org/10.3402/fnr.v58.22100.
Health Canada. (2012) Summary of Health Canada’s assessment of a health claim about whole grains and coronary heart disease. https://www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/assessments/assessment-health-claim-about-whole-grains-coronary-heart-disease.html. Accessed 1 June 2022.
U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2022) 2020–2025 Dietary Guidelines for Americans. https://www.dietaryguidelines.gov. Accessed 1 Jan. 2024.
Public Health England. (2016) The Eatwell Guide. https://www.gov.uk/government/publications/the-eatwell-guide. Accessed 1 June 2022.
Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood A, Jonell M, Clark M, Gordon LJ, Fanzo J, Hawkes C, Zurayk R, Rivera JA, De Vries W, Majele Sibanda L, Afshin A, Chaudhary A, Herrero M, Agustina R, Branca F, Lartey A, Fan S, Crona B, Fox E, Bignet V, Troell M, Lindahl T, Singh S, Cornell SE, Srinath Reddy K, Narain S, Nishtar S, Murray CJL. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–92. https://doi.org/10.1016/S0140-6736(18)31788-4.
Miller KB. Review of whole grain and dietary fiber recommendations and intake levels in different countries. Nutr Rev. 2020;78(Supplement1):29–36. https://doi.org/10.1093/nutrit/nuz052.
Health Canada. (2020) Canada’s Food Guide: choose healthy menu options. https://food-guide.canada.ca/en/healthy-eating-recommendations/limit-highly-processed-foods/choosing-healthy-menu-options/. Accessed 1 Jan. 2024.
Della Pepa G, Vetrani C, Vitale M, Riccardi G. Wholegrain intake and risk of type 2 diabetes: evidence from epidemiological and intervention studies. Nutrients. 2018;10(9):1288. https://doi.org/10.3390/nu10091288.
Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol. 2013;28(11):845–58. https://doi.org/10.1007/s10654-013-9852-5.
Chanson-Rolle A, Meynier A, Aubin F, Lappi J, Poutanen K, Vinoy S, Braesco V. Systematic review and meta-analysis of human studies to support a quantitative recommendation for whole grain intake in relation to type 2 diabetes. PLoS ONE. 2015;10(6):e0131377. https://doi.org/10.1371/journal.pone.0131377.
Sun Q, Spiegelman D, van Dam RM, Holmes MD, Malik VS, Willett WC, Hu FB. White rice, brown rice, and risk of type 2 diabetes in US men and women. Arch Intern Med. 2010;170(11):961–9. https://doi.org/10.1001/archinternmed.2010.109.
Kazemzadeh M, Safavi SM, Nematollahi S, Nourieh Z. Effect of brown rice consumption on inflammatory marker and cardiovascular risk factors among overweight and obese non-menopausal female adults. Int J Prev Med. 2014;5(4):478.
Kim M, Song G, Kang M, Yoo HJ, Jeong TS, Lee SH, Lee JH. Replacing carbohydrate with protein and fat in prediabetes or type-2 diabetes: Greater effect on metabolites in PBMC than plasma. Nutr Metab. 2016;13(1):3. https://doi.org/10.1186/s12986-016-0063-4.
Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr. 2012;142(7):1304–13. https://doi.org/10.3945/jn.111.155325.
Marventano S, Vetrani C, Vitale M, Godos J, Riccardi G, Grosso G. Whole grain intake and Glycaemic Control in healthy subjects: a systematic review and Meta-analysis of Randomized controlled trials. Nutrients. 2017;9(7):769. https://doi.org/10.3390/nu9070769.
Li S, Zong A, An R, Wang H, Liu L, Liu J, Guo X, Xu Z, Wang J, Li D, Du F, Xu T. Effects of whole grain intake on glycemic traits: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2021;1–20. https://doi.org/10.1080/10408398.2021.2001429.
Frølich W, Åman P, Tetens I. Whole grain foods and health–a scandinavian perspective. Food Nutr Res. 2013;57(1):18503. https://doi.org/10.3402/fnr.v57i0.18503.
Ghanbari-Gohari F, Mousavi SM, Esmaillzadeh A. Consumption of whole grains and risk of type 2 diabetes: a comprehensive systematic review and dose–response meta-analysis of prospective cohort studies. Food Sci Nutr. 2022;10(6):1950–60. https://doi.org/10.1002/fsn3.2811.
Malik VS, Sudha V, Wedick NM, Ramyabai M, Vijayalakshmi P, Lakshmipriya N, Gayathri R, Kokila A, Jones C, Hong B, Li R, Krishnaswamy K, Anjana RM, Spiegelman D, Willett WC, Hu FB, Mohan V. Substituting brown rice for white rice on diabetes risk factors in India: a randomised controlled trial. Br J Nutr. 2019;121(12):1389–97. https://doi.org/10.1017/S000711451900076X.
Nakayama T, Nagai Y, Uehara Y, Nakamura Y, Ishii S, Kato H, Tanaka Y. Eating glutinous brown rice twice a day for 8 weeks improves glycemic control in Japanese patients with diabetes mellitus. Nutr Diabetes. 2017;7(5):e273–273. https://doi.org/10.1038/nutd.2017.26.
Cooper DN, Kable ME, Marco ML, De Leon A, Rust B, Baker JE, Horn W, Burnett D, Keim NL. The effects of moderate whole grain consumption on fasting glucose and lipids, gastrointestinal symptoms, and microbiota. Nutrients. 2017;9(2):173. https://doi.org/10.3390/nu9020173.
Araki R, Ushio R, Fujie K, Ueyama Y, Suzuki H, Nakata Y, Hashimoto K. Effect of partially-abraded brown rice consumption on body weight and the indicators of glucose and lipid metabolism in pre-diabetic adults: a randomized controlled trial. Clin Nutr ESPEN. 2017;19:9–15. https://doi.org/10.1016/j.clnesp.2017.01.015.
Giacco R, Lappi J, Costabile G, Kolehmainen M, Schwab U, Landberg R, Uusitupa M, Poutanen K, Pacini G, Rivellese AA, Riccardi G, Mykkänen H. Effects of rye and whole wheat versus refined cereal foods on metabolic risk factors: a randomised controlled two-centre intervention study. Clin Nutr. 2013;32(6):941–9. https://doi.org/10.1016/j.clnu.2013.01.016.
Meyer KA, Kushi LH, Jacobs DR Jr, Slavin J, Sellers TA, Folsom AR. Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr. 2000;71(4):921–30. https://doi.org/10.1093/ajcn/71.4.921.
Montonen J, Knekt P, Järvinen R, Aromaa A, Reunanen A. Whole-grain and fiber intake and the incidence of type 2 diabetes. Am J Clin Nutr. 2003;77(3):622–9. https://doi.org/10.1093/ajcn/77.3.622.
van Dam RM, Hu FB, Rosenberg L, Krishnan S, Palmer JR. Dietary calcium and magnesium, major food sources, and risk of type 2 diabetes in US black women. Diabetes Care. 2006;29(10):2238–43. https://doi.org/10.2337/dc06-1014.
Ericson U, Sonestedt E, Gullberg B, Hellstrand S, Hindy G, Wirfält E, Orho-Melander M. High intakes of protein and processed meat associate with increased incidence of type 2 diabetes. Br J Nutr. 2013;109(6):1143–53. https://doi.org/10.1017/S0007114512003017.
Wirström T, Hilding A, Gu HF, Östenson C-G, Björklund A. Consumption of whole grain reduces risk of deteriorating glucose tolerance, including progression to prediabetes. Am J Clin Nutr. 2013;97(1):179–87. https://doi.org/10.3945/ajcn.112.045583.
Kyrø C, Tjønneland A, Overvad K, Olsen A, Landberg R. Higher whole-grain intake is associated with lower risk of type 2 diabetes among middle-aged men and women: the Danish Diet, Cancer, and Health Cohort. J Nutr. 2018;148(9):1434–44. https://doi.org/10.1093/jn/nxy112.
Hu Y, Ding M, Sampson L, Willett WC, Manson JE, Wang M, Rosner B, Hu FB, Sun Q. Intake of whole grain foods and risk of type 2 diabetes: results from three prospective cohort studies. BMJ (Clinical Res ed). 2020;370:m2206–2206. https://doi.org/10.1136/bmj.m2206.
Li J, Glenn AJ, Yang Q, Ding D, Zheng L, Bao W, Beasley J, LeBlanc E, Lo K, Manson JE, Philips L, Tinker L, Liu S. Dietary protein sources, mediating biomarkers, and incidence of type 2 diabetes: findings from the women’s Health Initiative and the UK Biobank. Diabetes Care. 2022;45(8):1742–53. https://doi.org/10.2337/dc22-0368.
Pick M, Hawrysh ZJ, Gee M, Toth E. Barley bread products improve glycemic control of type 2 subjects. Int J Food Sci Nutr. 1998;49(1):71–8. https://doi.org/10.3109/09637489809086406.
Pereira MA, Jacobs DR Jr., Pins JJ, Raatz SK, Gross MD, Slavin JL, Seaquist ER. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. Am J Clin Nutr. 2002;75(5):848–55. https://doi.org/10.1093/ajcn/75.5.848.
Pins JJ, Geleva D, Keenan JM, Frazel C, O’Connor PJ, Cherney LM. Do whole-grain oat cereals reduce the need for antihypertensive medications and improve blood pressure control? J Fam Pract. 2002;51(4):353–9.
Li J, Kaneko T, Qin LQ, Wang J, Wang Y. Effects of barley intake on glucose tolerance, lipid metabolism, and bowel function in women. Nutrition. 2003;19(11–12):926–9. https://doi.org/10.1016/s0899-9007(03)00182-5.
McIntosh GH, Noakes M, Royle PJ, Foster PR. Whole-grain rye and wheat foods and markers of bowel health in overweight middle-aged men. Am J Clin Nutr. 2003;77(4):967–74. https://doi.org/10.1093/ajcn/77.4.967.
Andersson A, Tengblad S, Karlstrom B, Kamal-Eldin A, Landberg R, Basu S, Aman P, Vessby B. Whole-grain foods do not affect insulin sensitivity or markers of lipid peroxidation and inflammation in healthy, moderately overweight subjects. J Nutr. 2007;137(6):1401–7. https://doi.org/10.1093/jn/137.6.1401.
Katcher HI, Legro RS, Kunselman AR, Gillies PJ, Demers LM, Bagshaw DM, Kris-Etherton PM. The effects of a whole grain-enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am J Clin Nutr. 2008;87(1):79–90. https://doi.org/10.1093/ajcn/87.1.79.
Kim JY, Kim JH, Lee DH, Kim SH, Lee SS. Meal replacement with mixed rice is more effective than white rice in weight control, while improving antioxidant enzyme activity in obese women. Nutr Res. 2008;28(2):66–71. https://doi.org/10.1016/j.nutres.2007.12.006.
Brownlee IA, Moore C, Chatfield M, Richardson DP, Ashby P, Kuznesof SA, Jebb SA, Seal CJ. Markers of cardiovascular risk are not changed by increased whole-grain intake: the WHOLEheart study, a randomised, controlled dietary intervention. Br J Nutr. 2010;104(1):125–34. https://doi.org/10.1017/s0007114510000644.
Giacco R, Clemente G, Cipriano D, Luongo D, Viscovo D, Patti L, Di Marino L, Giacco A, Naviglio D, Bianchi MA. Effects of the regular consumption of wholemeal wheat foods on cardiovascular risk factors in healthy people. Nutr Metab Cardiovasc Dis. 2010;20(3):186–94. https://doi.org/10.1016/j.numecd.2009.03.025.
Tighe P, Duthie G, Vaughan N, Brittenden J, Simpson WG, Duthie S, Mutch W, Wahle K, Horgan G, Thies F. Effect of increased consumption of whole-grain foods on blood pressure and other cardiovascular risk markers in healthy middle-aged persons: a randomized controlled trial. Am J Clin Nutr. 2010;92(4):733–40. https://doi.org/10.3945/ajcn.2010.29417.
Zhang G, Pan A, Zong G, Yu Z, Wu H, Chen X, Tang L, Feng Y, Zhou H, Chen X. Substituting white rice with brown rice for 16 weeks does not substantially affect metabolic risk factors in middle-aged Chinese men and women with diabetes or a high risk for diabetes. J Nutr. 2011;141(9):1685–90. https://doi.org/10.3945/jn.111.142224.
Kristensen M, Toubro S, Jensen MG, Ross AB, Riboldi G, Petronio M, Bügel S, Tetens I, Astrup A. Whole grain compared with refined wheat decreases the percentage of body fat following a 12-week, energy-restricted dietary intervention in postmenopausal women. J Nutr. 2012;142(4):710–6. https://doi.org/10.3945/jn.111.142315.
MacKay KA, Tucker AJ, Duncan AM, Graham TE, Robinson LE. Whole grain wheat sourdough bread does not affect plasminogen activator inhibitor-1 in adults with normal or impaired carbohydrate metabolism. Nutr Metab Cardiovasc Dis. 2012;22(9):704–11. https://doi.org/10.1016/j.numecd.2010.10.018.
Wang B, Medapalli R, Xu J, Cai W, Chen X, He JC, Uribarri J. Effects of brown rice diet on metabolic parameters and inflammatory markers in Chinese American with prediabetes. e-SPEN J. 2012;8(1):e15–20. https://doi.org/10.1016/j.clnme.2012.11.001.
Bui TN, Le Hop T, Nguyen DH, Tran QB, Nguyen TL, Le DT, Nguyen DVA, Vu AL, Aoto H, Okuhara Y, Ito Y, Yamamoto S, Kise M. Pre-germinated brown rice reduced both blood glucose concentration and body weight in Vietnamese women with impaired glucose tolerance. J Nutr Sci Vitaminol (Tokyo). 2014;60(3):183–7. https://doi.org/10.3177/jnsv.60.183.
Jackson KH, West SG, Vanden Heuvel JP, Jonnalagadda SS, Ross AB, Hill AM, Grieger JA, Lemieux SK, Kris-Etherton PM. Effects of whole and refined grains in a weight-loss diet on markers of metabolic syndrome in individuals with increased waist circumference: a randomized controlled-feeding trial. Am J Clin Nutr. 2014;100(2):577–86. https://doi.org/10.3945/ajcn.113.078048.
Vitaglione P, Mennella I, Ferracane R, Rivellese AA, Giacco R, Ercolini D, Gibbons SM, La Storia A, Gilbert JA, Jonnalagadda S. Whole-grain wheat consumption reduces inflammation in a randomized controlled trial on overweight and obese subjects with unhealthy dietary and lifestyle behaviors: role of polyphenols bound to cereal dietary fiber. Am J Clin Nutr. 2015;101(2):251–61. https://doi.org/10.3945/ajcn.114.088120.
Ampatzoglou A, Williams CL, Atwal KK, Maidens CM, Ross AB, Thielecke F, Jonnalagadda SS, Kennedy OB, Yaqoob P. Effects of increased wholegrain consumption on immune and inflammatory markers in healthy low habitual wholegrain consumers. Eur J Nutr. 2016;55(1):183–95. https://doi.org/10.1007/s00394-015-0836-y.
Connolly ML, Tzounis X, Tuohy KM, Lovegrove JA. Hypocholesterolemic and prebiotic effects of a whole-grain oat-based granola breakfast cereal in a cardio-metabolic at risk population. Front Microbiol. 2016;7(NOV). https://doi.org/10.3389/fmicb.2016.01675.
Geng SS, Zhu Y, Zhang JP, Cai YQ. Lowering effect of pre-germinated brown rice on dyslipidemia in Chinese patients. Int J Clin Exp Med. 2016;9(11):22317–23.
Kirwan JP, Malin SK, Scelsi AR, Kullman EL, Navaneethan SD, Pagadala MR, Haus JM, Filion J, Godin JP, Kochhar S, Ross AB. A whole-grain diet reduces cardiovascular risk factors in overweight and obese adults: a randomized controlled trial. J Nutr. 2016;146(11):2244–51. https://doi.org/10.3945/jn.116.230508.
Vetrani C, Costabile G, Luongo D, Naviglio D, Rivellese AA, Riccardi G, Giacco R. Effects of whole-grain cereal foods on plasma short chain fatty acid concentrations in individuals with the metabolic syndrome. Nutrition. 2016;32(2):217–21. https://doi.org/10.1016/j.nut.2015.08.006.
Kondo K, Morino K, Nishio Y, Ishikado A, Arima H, Nakao K, Nakagawa F, Nikami F, Sekine O, Nemoto K-i. Fiber-rich diet with brown rice improves endothelial function in type 2 diabetes mellitus: a randomized controlled trial. PLoS ONE. 2017;12(6):e0179869. https://doi.org/journal.pone.0179869.
Kristensen M, Pelletier X, Ross AB, Thielecke F. A high rate of non-compliance confounds the study of whole grains and weight maintenance in a randomised intervention trial—the case for greater use of dietary biomarkers in nutrition intervention studies. Nutrients. 2017;9(1):55. https://doi.org/10.3390/nu9010055.
Philip Karl J, Meydani M, Barnett JB, Vanegas SM, Goldin B, Kane A, Rasmussen H, Saltzman E, Vangay P, Knights D, Oliver Chen CY, Das SK, Jonnalagadda SS, Meydani SN, Roberts SB. Substituting whole grains for refined grains in a 6-wk randomized trial favorably affects energy-balance metrics in healthy men and postmenopausal women1-3. Am J Clin Nutr. 2017;105(3):589–99. https://doi.org/10.3945/ajcn.116.139683.
Kikuchi Y, Nozaki S, Makita M, Yokozuka S, Fukudome S-i, Yanagisawa T, Aoe S. Effects of whole grain wheat bread on visceral fat obesity in Japanese subjects: a randomized double-blind study. Plant Foods Hum Nutr. 2018;73(3):161–5. https://doi.org/10.1007/s11130-018-0666-1.
Hoevenaars FPM, Esser D, Schutte S, Priebe MG, Vonk RJ, Van Den Brink WJ, Van Der Kamp JW, Stroeve JHM, Afman LA, Wopereis S. Whole grain wheat consumption affects postprandial inflammatory response in a randomized controlled trial in overweight and obese adults with mild hypercholesterolemia in the Graandioos Study. J Nutr. 2019;149(12):2133–44. https://doi.org/10.1093/jn/nxz177.
Kuroda Y, Matsuzaki K, Wakatsuki H, Shido O, Harauma A, Moriguchi T, Sugimoto H, Yamaguchi S, Yoshino K, Hashimoto M. Influence of Ultra-high Hydrostatic Pressurizing Brown Rice on cognitive functions and Mental Health of Elderly Japanese individuals: a 2-Year randomized and controlled trial. J Nutr Sci Vitaminol (Tokyo). 2019;Supplement65. https://doi.org/10.3177/jnsv.65.S80.
Roager HM, Vogt JK, Kristensen M, Hansen LBS, Ibrügger S, Mærkedahl RB, Bahl MI, Lind MV, Nielsen RL, Frøkiær H. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut. 2019;68(1):83–93. https://doi.org/10.1136/gutjnl-2017-314786.
Mai TT, Trang TT, Hai TT. Effectiveness of germinated brown rice on metabolic syndrome: a randomized control trial in Vietnam. AIMS Public Health. 2020;7(1):33–43. https://doi.org/10.3934/publichealth.2020005.
Ren C, Hong B, Zheng X, Wang L, Zhang Y, Guan L, Yao X, Huang W, Zhou Y, Lu S. Improvement of germinated brown rice quality with autoclaving treatment. Food Sci Nutr. 2020;8(3):1709–17. https://doi.org/10.1002/fsn3.1459.
Xue K, Liu Y, Iversen KN, Mazidi M, Qu Z, Dong C, Jin T, Hallmans G, Aman P, Johansson A, He G, Landberg R. Impact of a Fermented High-Fiber Rye Diet on Helicobacter pylori and Cardio-metabolic risk factors: a Randomized Controlled Trial among Helicobacter pylori-positive Chinese adults. Front Nutr. 2021;7:608623. https://doi.org/10.3389/fnut.2020.608623.
Ding Q, Ren J, Zhou Y, Bai Z, Yan J, Na G, Shan Y. Whole grain germinated brown rice regulates intestinal immune homeostasis and gastrointestinal hormones in type 2 diabetic patients-a randomized control trial. Food Funct. 2022;13(15):8274–82. https://doi.org/10.1039/d2fo00477a.
Mozaffarian D, Forouhi NG. Dietary guidelines and health—is nutrition science up to the task? BMJ. 2018;360:k822. https://doi.org/10.1136/bmj.k822.
Kyrø C, Skeie G, Dragsted LO, Christensen J, Overvad K, Hallmans G, Johansson I, Lund E, Slimani N, Johnsen NF, Halkjær J, Tjønneland A, Olsen A. Intake of whole grains in Scandinavia is associated with healthy lifestyle, socio-economic and dietary factors. Public Health Nutr. 2011;14(10):1787–95. https://doi.org/10.1017/s1368980011000206.
Andersen JLM, Halkjær J, Rostgaard-Hansen AL, Martinussen N, Lund A-SQ, Kyrø C, Tjønneland A, Olsen A. Intake of whole grain and associations with lifestyle and demographics: a cross-sectional study based on the Danish Diet, Cancer and Health—Next generations cohort. Eur J Nutr. 2021;60(2):883–95. https://doi.org/10.1007/s00394-020-02289-y.
Mathews R, Chu Y. Global review of whole grain definitions and health claims. Nutr Rev. 2020;78(Supplement1):98–106. https://doi.org/10.1093/nutrit/nuz055.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. Wiley; 2019.
Rave K, Roggen K, Dellweg S, Heise T, tom Dieck H. Improvement of insulin resistance after diet with a whole-grain based dietary product: results of a randomized, controlled cross-over study in obese subjects with elevated fasting blood glucose. Br J Nutr. 2007;98(5):929–36. https://doi.org/10.1017/s0007114507749267.
Ross AB, Bruce SJ, Blondel-Lubrano A, Oguey-Araymon S, Beaumont M, Bourgeois A, Nielsen-Moennoz C, Vigo M, Fay LB, Kochhar S, Bibiloni R, Pittet AC, Emady-Azar S, Grathwohl D, Rezzi S. A whole-grain cereal-rich diet increases plasma betaine, and tends to decrease total and LDL-cholesterol compared with a refined-grain diet in healthy subjects. Br J Nutr. 2011;105(10):1492–502. https://doi.org/10.1017/s0007114510005209.
Sanders LM, Zhu Y, Wilcox ML, Koecher K, Maki KC. Effects of whole grain intake, compared with Refined Grain, on Appetite and Energy Intake: a systematic review and Meta-analysis. Adv Nutr. 2021;1177–95. https://doi.org/10.1093/advances/nmaa178.
Zurbau A, Noronha JC, Khan TA, Sievenpiper JL, Wolever TMS. The effect of oat β-glucan on postprandial blood glucose and insulin responses: a systematic review and meta-analysis. Eur J Clin Nutr. 2021;75(11):1540–54. https://doi.org/10.1038/s41430-021-00875-9.
Vuksan V, Jenkins AL, Rogovik AL, Fairgrieve CD, Jovanovski E, Leiter LA. Viscosity rather than quantity of dietary fibre predicts cholesterol-lowering effect in healthy individuals. Br J Nutr. 2011;106(9):1349–52. https://doi.org/10.1017/S0007114511001711.
Guo H, Wu H, Sajid A, Li Z. Whole grain cereals: the potential roles of functional components in human health. Crit Rev Food Sci Nutr. 2021;1–16. https://doi.org/10.1080/10408398.2021.1928596.
Khan J, Khan MZ, Ma Y, Meng Y, Mushtaq A, Shen Q, Xue Y. Overview of the composition of whole grains’ phenolic acids and Dietary Fibre and their effect on chronic non-communicable diseases. Int J Environ Res Public Health. 2022;19(5):3042. https://doi.org/10.3390/ijerph19053042.
Saleh ASM, Wang P, Wang N, Yang L, Xiao Z. Brown Rice Versus White Rice: nutritional quality, potential health benefits, development of Food products, and Preservation technologies. Compr Rev Food Sci Food Saf. 2019;18(4):1070–96. https://doi.org/10.1111/1541-4337.12449.
Gong L, Feng D, Wang T, Ren Y, Liu Y, Wang J. Inhibitors of α-amylase and α-glucosidase: potential linkage for whole cereal foods on prevention of hyperglycemia. Food Sci Nutr. 2020;8(12):6320–37. https://doi.org/10.1002/fsn3.1987.
Funding
This study was funded by the National Natural Science Foundation of China (81861138007) and the Shanghai Pujiang Program (21PJD005). The study sponsor/funder was not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; and did not impose any restrictions regarding the publication of the report.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows-TY, YL, KX and GH: Designed the research. TY and JZ: Conducted the research. TY and WL: Extracted the data. TY and JD: Analyzed the data. TY, JZ, JK and YL: Wrote the paper. YL and GH are responsible for the final content; All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The manuscript does not contain clinical studies or patient data.
Conflict of interest
Jianheng Zheng, Juntao Kan and Jun Du are employees of Nutrilite Health Institute, Shanghai, China. The conclusions and interpretations provided, based on the scientific data reviewed, are those of the authors and not of the employer and funding agencies of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ying, T., Zheng, J., Kan, J. et al. Effects of whole grains on glycemic control: a systematic review and dose-response meta-analysis of prospective cohort studies and randomized controlled trials. Nutr J 23, 47 (2024). https://doi.org/10.1186/s12937-024-00952-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-00952-2