Abstract
Backgrounds & Aims
The nutritional evaluation of pancreatic cancer (PC) patients lacks a gold standard or scientific consensus, we aimed to summarize and systematically evaluate the prognostic value of nutritional screening and assessment tools used for PC patients.
Methods
Relevant studies were retrieved from major databases (PubMed, Embase, Web of Science, Cochrane Library) and searched from January 2010 to December 2023. We performed meta-analyses with STATA 14.0 when three or more studies used the same tool.
Results
This analysis included 27 articles involving 6,060 PC patients. According to a meta-analysis of these studies, poor nutritional status evaluated using five nutritional screening tools Prognostic Nutritional Index (PNI), Geriatric Nutritional Risk Index (GNRI), Controlling Nutritional Status Score (CONUT), Nutrition Risk Screening (NRS2002) and Glasgow Prognostic Score (GPS) was associated with all-cause mortality in PC patients. But Modified Glasgow Prognostic Score (mGPS) did not. Of all tools analyzed, CONUT had the maximum HR for mortality (HR = 1.978, 95%CI 1.345–2.907, P = 0.001).
Conclusion
All-cause mortality in PC patients was predicted by poor nutritional status. CONUT may be the best nutritional assessment tool for PC patients. The clinical application value of Short Form Mini Nutritional Assessment (MNA-SF), Generated Subjective Global Assessment (SGA) and Patient-generated Subjective Global Assessment (PG-SGA) in PC patients need to be confirmed. In order to improve patients’ nutritional status and promote their recovery, nutritional screening tools can be used.
Registration
This systematic review was registered at the International Prospective Register of Systematic Reviews (PROSPERO) (number CRD42022376715).
Similar content being viewed by others
Introduction
Pancreatic cancer (PC), a group of malignant tumors mainly originating from pancreatic duct- epithelium and acinus cells, is one of the most common malignant tumors in the digestive system [1]. The global prevalence of pancreatic cancer is about 2.6% [2]. Over the past 25 years, the global burden of pancreatic cancer has doubled and now ranks in the top 10 of all cancers in more than 130 countries [3]. With the progression of pancreatic cancer, malnutrition has become the most common and difficult problem for pancreatic cancer patients [4]. On the one hand, pancreatic cancer patients lead to tumor cachexia due to abnormal pancreatic secretion function and increased tumor metabolism. On the other hand, the anatomical changes caused by digestive tract reconstruction after tumor resection often lead to patients’ decreased appetite and difficulty in eating, and thus malnutrition [5]. Yu K [6]investigated 687 tumor patients, and the highest nutritional risk was pancreatic cancer (81.8%). Nutritional status affects the incidence of postoperative complications, length of hospital stay, and long-term prognosis of cancer patients [7,8,9,10]. Malnutrition has been proven to be an independent risk factor for prognosis in patients with pancreatic cancer [11]. Therefore, nutritional risk screening and nutritional support should be conducted before pancreatic cancer resection, and early identification and intervention of malnourished patients can indeed reduce postoperative complications, thus shortening hospital stay and reducing hospital costs [11].
Despite the nutritional abnormalities, most patients did not receive nutritional advice before undergoing chemotherapy despite their nutritional deficiencies [12, 13]. It is of significant importance for patients to obtain nutritional advice from all members of their medical team, in case a dietitian is unavailable. European Society for Clinical Nutrition and Metabolism recommends that cancer patients should undergo long-term repeated nutritional screening to identify patients at risk of malnutrition [14]. Therefore, the application of nutritional screening and assessment tools to assess preoperative nutritional status of pancreatic cancer patients, early detection of malnutrition risk and appropriate interventions can improve clinical outcomes [15].
Research and clinical experience continue to provide us with new tools for nutritional screening and assessment, providing us with more options for evaluating the prognosis of pancreatic cancer [16,17,18]. The prevalence of malnutrition in PC differed greatly from previous studies. As a result, many nutritional assessment or screening tools are employed [19]. The prevalence of malnutrition in PC patients differed from 9.1% (by CONUT) to 39.7% (by PNI) in the same cohort [20]. . In PC patients, this makes tracking prevalence and comparing the effects of different nutrition management interventions challenging. Thus, this study aims to provide a reference for the selection and evaluation of nutritional evaluation tools based on the prognostic value.
Method
Search strategy and selection criteria
Studies were retrieved from major databases (PubMed, Embase, Web of Science, Cochrane Library) and searched from the earliest available date until October. This systematic review was registered at the International Prospective Register of Systematic Reviews (PROSPERO) (number CRD42022376715). Inclusion criteria were as follows: Inclusion criteria were as follows: (1) P (patients): The participants were patients with PC (≥ 18 years old); (2) I (intervention—exposure): patients with malnutrition risk as determined by ESPEN 2017 recommended tools; (3) C (control): patients with a normal nutritional status as determined by ESPEN 2017 recommended tools [14]; and (4) O (outcomes): studies that reported all-cause mortality. A cut-off value to divide patients into malnutrition and normal nutrition groups was identified for (2) and (3). The hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for (4) were either directly reported by the studies or could be calculated using the data provided. The exclusion criteria included: (1) Research proposals, guidelines, conference abstracts, reviews; (2) Studies not published in English or Chinese; (3) Full text not available. The following search terms were used: “Pancreatic Neoplasms“[MeSH Terms] AND (“prognos*“[Title/Abstract] OR “predict*“[Title/Abstract] OR “mortality“[Title/Abstract] OR “survival“[Title/Abstract]) AND (“malnutri*“[Title/Abstract] OR “nutri*“[Title/Abstract] OR “undernutri*“[Title/Abstract]). Search database from search date January 2010 to December 2023. Additionally, reference lists of the cited articles were manually searched to identify additional relevant articles.
Screening of the articles
Using the database returned articles’ titles and abstracts, two investigators (Yu & Li) independently searched the database. To determine if studies met the inclusion criteria, the full text of the studies was read. The inclusion discrepancies between the other two investigators were confirmed by a third investigator (Liu).
Quality assessment of the articles
Cohort studies were evaluated using the modified Newcastle-Ottawa Scale (NOS) [21], in which 1 to 3, 4 to 6, and 7 to 9 scores were considered low, medium, and high quality, respectively. Studies with a final score above 6 were considered high quality.
Data extraction
Full texts of the screened articles were carefully reviewed and data were extracted: surname of the first author, publication year, study design (retrospective or prospective), country, disease stage, sample size, mean/median age or age range, categorical or continuous analysis of nutritional status score, most fully adjusted risk estimate, follow-up duration, determination method and cut-off value of nutrition evaluation tool, therapeutic method. Each study’s hazard ratio (HR) and 95% Confidence Interval (CI) were directly extracted from the multivariate analysis.
Statistical analysis
The meta-analysis was conducted using STATA 14.0. We acquired hazard ratios with 95% confidence intervals for each study, and then plotted the pooled results. Statistical analyses were performed if three or more studies used the same nutrition screening or assessment tool. Heterogeneity was explored using I2 statistics and Cochran’s Q test. The determination of significant high heterogeneity in studies was based on the criteria of I2 ≥ 50% or P<0.10 of the Cochran Q test, after which a random-effects model was employed [22]. Conversely, studies exhibiting I2<50% and P>0.10 were analyzed using a fixed-effects model. Heterogeneity among studies was considered minor if I2<25%, moderate if I2 values ranged between 25% and 50%, and large if I2 values exceeded 50%. Statistical significance was established at a P value less than 0.05.
Results
Literature search
In total, 2189 references were identified, including 148 in PubMed, 10 in Embase, 2031 in Web of Science, and 1 in Cochrane Library. According to the manual analysis of these studies, 27 articles were included in the analysis. Meta-analysis was performed by 26 articles and qualitative analysis was performed by 2 articles. One article provided qualitative and quantitative analysis. Because multiple tools used in this article. The search and selection process is illustrated in Fig. 1.
Study characteristics
The features of the 27 studies were outlined in Table 1. There were a total of 6,060 PC patients from either China, Japan, US, Korea, Norway, Italy, Turkey, Germany. A score of 6 to 9 was assigned to the study quality by NOS.
In the 27 articles, 9 types of nutritional screening tools ( NRS2002 [32,33,34, 43], PNI [19, 20, 23,24,25,26,27,28,29, 31, 38, 44,45,46,47], GPS [19, 20, 23, 27, 31, 35, 41], mGPS [19, 24, 30, 31], CONUT [19, 20, 24, 35,36,37,38], MUST [43], MNA-SF [43], NRI [43] and GNRI [19, 39, 40]), 3 types of nutritional assessment tools(SGA [43], PG-SGA [42], MNA [43]) were reported in Table 2. The most used tool was PNI (N = 16), followed by CONUT(N = 7) and GPS(N = 7).
Meta-analysis of the prognostic value of all-cause mortality in PC patients
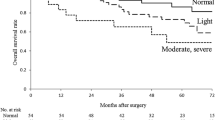
Based on results from fixed-effects and random-effects models, poor nutritional status as determined by CONUT(HR = 1.978, 95%CI 1.345–2.907, P = 0.001), GNRI(HR = 1.595, 95%CI 1.033–2.466, P = 0.036), GPS(HR = 1.464, 95%CI 1.299–1.650, P<0.001), NRS2002(HR = 1.248, 95%CI 1.155–1.348, P<0.001) and PNI(HR = 1.504, 95%CI 1.295–1.747, P<0.001) was associated with mortality due to all causes in PC patients. As a result, mGPS (HR = 1.793, 95%CI 0.883–3.643, P = 0.106) was unable to show that abnormal nutritional status in PC patients was a significant predictor of all-cause mortality. According to Table 3, CONUT had the highest mortality rate among these tools.
Subgroup analysis was conducted based on sample size, follow-up duration, cutoff value, treatment method, tumor stage and region for CONUT, GPS and PNI. In these three groups, there were no significant differences between the heterogeneity of each subgroup and the whole cohort based on the subgroup analysis. Ample size, follow-up duration, cutoff value, treatment method, and tumor stage and region are not related to heterogeneity of CONUT, GPS and PNI groups, as shown in Table 4.
Sensitivity analyses and publication bias
We performed a sensitivity analysis in CONUT, GPS, mGPS, NRS2002, and PNI groups to determine whether omitting any study would affect the pooled HR. To assess publication bias, we also conducted Begg’s funnel plot and Egger’s linear regression test. As P = 0.266 for Begg’s test and P = 0.041 for Egger’s test in CONUT groups, P = 0.089 for Begg’s test and P = 0.036 for Egger’s test in mGPS groups and P = 0.669 for Begg’s test and P = 0.026 for Egger’s test in PNI groups indicted slight publication bias. Then trim and fill analysis showed robust results. As P = 0.711 for Begg’s test and P = 0.356 for Egger’s test in GPS group and P = 0.089 for Begg’s test and P = 0.255 for Egger’s test in NRS2002 groups showed no significant publication bias.
Qualitative analysis of prognostic value in PC patients
The remaining 2 studies used PG-SGA, NRI, SGA, MUST, MNA and MNA-SF to evaluate PC patients’ nutritional status. Heckler reported that malnutrition assessed by NRI, MUST, MNA could not predict OS in 116 PC patients [43]. Nutritional screening tools MNA-SF and SGA and PG-SGA indicate that abnormal nutritional status is an important predictor of all-cause mortality in PC patients.
Discussion
In this systematic review, we summarized the prognostic value of different nutritional screening and assessment tools for PC patients, including NRS2002, PNI, GPS, mGPS, CONUT, MUST, MNA-SF, NRI, GNRI, SGA, PG-SGA and MNA. Our study demonstrated that these tools exclude mGPS, NRI, MUST and MNA could predict survival of patients with pancreatic cancer. And CONUT had the maximum prognostic potential for mortality in PC patients.
The CONUT scoring system comprises of lymphocyte count, serum albumin, and total cholesterol. Serum albumin is a frequently utilized indicator for evaluating nutritional status, and numerous studies have demonstrated that low serum albumin levels are an autonomous predictor of poor survival for diverse cancers [11, 48]. Furthermore, total lymphocyte count associated with human nutrition [49]. While the PNI also incorporates serum albumin and peripheral blood lymphocytes, the primary distinction from CONUT is the lack of a total cholesterol calculation. According to Kheirouri [50], the CONUT score has demonstrated greater precision than the PNI in prognosticating survival across diverse cancer types, rendering it a more desirable tool. The cellular membrane represents a crucial constituent, wherein cholesterol serves not only as a marker of caloric consumption [51, 52], but also as a contributor to tumorigenesis and immune-related signaling pathways [53, 54]. Investigations have revealed that diminished levels of cholesterol are linked to inferior survival outcomes, plausibly due to the involvement of cholesterol in numerous biochemical pathways that underlie immune responses and tumor development [55]. . Existing studies have fully demonstrated that CONUT score is more effective than other prognostic score [56, 57], this is consistent with the conclusion of this study.
The NRS2002 tool demonstrated superior predictive ability for mortality risk in patients with PC (HR = 1.248, 95%CI (1.155–1.348), P < 0.001), despite its subjective nature, which requires patients to report recent changes in weight and eating habits. European Society for Parenteral and Enteral Nutrition (ESPEN) recommends the use of NRS2002 for both cancer and surgical patients [58, 59]. . Due to its ease of use and lack of reliance on laboratory indices, NRS2002 is frequently employed as a preoperative nutritional screening tool for cancer patients in certain Chinese medical institutions [60, 61]. .
In 2005, Bouillanne [62] established the GNRI as an objective and simple nutritional screening tool determined by serum albumin, height, and body weight. In elderly long-term care patients, it has been shown to be a useful tool in predicting mortality [63, 64]. Nurses only need to measure the patient’s weight and height, and take blood samples in a few minutes, which is less of a burden for older patients. Especially for some patients with cognitive, hearing and visual impairment, as well as some uncooperative patients, objective data can be used to better to evaluate the nutritional status of patients. According to Grinstead, monitoring nutritional status using weight and albumin to promote increased survival is vital to promoting survival after initial diagnosis [65].
C-reactive protein (CRP) and serum albumin were used in the GPS, which was proposed by McMillan [66] in 2013. CRP elevation indicates systematic inflammation [67, 68]. And it reflects growth activity in tumors, because tumors can produce cytokines, which increase the inflammatory response [69]. In addition, this scoring system can distinguish between different stages of cachexia [70]. . According to Yamada [71], GPS outperformed other inflammation-based markers in predicting survival in PC patients. Based on GPS, mGPS was modified with more detailed criteria. In a large patient cohort, Proctor [72] evidenced that the mGPS as the systemic inflammatory response, is a powerful prognostic factor compared with other biochemical parameters. Whereas, this study found no significant difference in mGPS’s predictive value in predicting the prognosis of PC patients (P = 0.106), which may be due to the limited literature included and the differences in treatment methods of study subjects affecting the results. More researches were needed in the future to verify mGPS’s prognostic effect of PC patients.
Our meta-analysis suggested that low PNI were associated with poor OS in patients with PC. And high CONUT, GPS, NRS2002 were correlated with worse OS in PC patients. Subgroup analysis based on sample size、follow-up duration、cutoff value、treatment method、tumor stage and country region also confirmed that PNI, CONUT, GPS, NRS2002 functioned as prognostic indicators for PC. The remaining studies used PG-SGA, NRI, SGA, MUST, MNA and MNA-SF to evaluate PC patients’ nutritional status. According to our qualitative studies, malnutrition assessed by NRI, MUST, and MNA could not predict all-cause mortality in PC patients. Other findings in PC patients indicated that abnormal nutritional status was an important determinant of survival. Nevertheless, nutritional status is not always a good predictor of all-cause mortality in PC patients [15]. Researchers found that different nutritional tools were significantly different in their predictive value for all-cause mortality in nine studies that used two or more nutritional tools simultaneously [19, 20, 23, 24, 27, 31, 35, 38, 43]. . Therefore, nutritional screening and assessment tools should be chosen based on the characteristics of PC patients and clinical settings.
To our knowledge, this study is the first attempt to evaluate the effect of nutritional screening and assessment tools on survival from pancreatic cancer. However, due to insufficient studies on nutritional assessment tools, only nutritional screening tools were meta-analyzed, and nutritional assessment tools were descriptive. And the current study has several potential limitations. First, we did not include ongoing studies and limited our search to English language publications. In addition, credible conclusion about the predictive value of these nutritional screening and assessment tools established on more studies was necessary because of the small sample size of the current meta-analysis. Second, the Newcastle-Ottawa Scale require judgment (i.e. subjective) and could differ across people. Third, this Meta-analysis indicated large heterogeneity in the predictive value of these tools. However, subgroup analysis failed to fully explain the cause of heterogeneity. Cancer stage、follow-up years and treatments were important confounding factors for OS, and not all the studies provide the information. Finally, most included studies were from China or Japan. A comprehensive and thorough investigation of the subject may be enhanced by gathering information from western countries.
Conclusion
We found that poor nutritional status evaluated through GNRI, PNI, CONUT, NRS2002, and GPS significantly predicted mortality from all causes in PC patients. A nutritional screening tool with the highest predictive value was CONUT. Nutritional screening and assessment tools should be selected according to the purpose, the characteristics of the patient, and the clinical setting. To provide more tools for PC patients to predict their prognosis, large-scale studies are needed to prove the clinical application value of SGA, PG-SGA, and MNA-SF.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Yang Q, Zhang J, Zhu Y. Potential roles of the gut microbiota in pancreatic carcinogenesis and therapeutics. Front Cell Infect Microbiol. 2022;12:872019.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Cabasag CJ, Ferlay J, Laversanne M, Vignat J, Weber A, Soerjomataram I, Bray F. Pancreatic cancer: an increasing global public health concern. Gut. 2022;71(8):1686–7.
Pezzilli R, Caccialanza R, Capurso G, Brunetti O, Milella M, Falconi M. Pancreatic enzyme replacement therapy in pancreatic Cancer. Cancers 2020, 12(2).
Petzel MQB, Hoffman L. Nutrition implications for Long-Term survivors of pancreatic Cancer surgery. Nutr Clin Pract. 2017;32(5):588–98.
Yu K, Zhou XR, He SL. A multicentre study to implement nutritional risk screening and evaluate clinical outcome and quality of life in patients with cancer. Eur J Clin Nutr. 2013;67(7):732–7.
Lin J, Peng J, Qdaisat A, Li L, Chen G, Lu Z, Wu X, Gao Y, Zeng Z, Ding P, et al. Severe weight loss during preoperative chemoradiotherapy compromises survival outcome for patients with locally advanced rectal cancer. J Cancer Res Clin Oncol. 2016;142(12):2551–60.
Hill A, Kiss N, Hodgson B, Crowe TC, Walsh AD. Associations between nutritional status, weight loss, radiotherapy treatment toxicity and treatment outcomes in gastrointestinal cancer patients. Clin Nutr. 2011;30(1):92–8.
Planas M, Álvarez-Hernández J, León-Sanz M, Celaya-Pérez S, Araujo K, García de Lorenzo A. Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES® study. Supportive care in cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2016;24(1):429–35.
Kyle UG, Pirlich M, Lochs H, Schuetz T, Pichard C. Increased length of hospital stay in underweight and overweight patients at hospital admission: a controlled population study. Clin Nutr. 2005;24(1):133–42.
La Torre M, Ziparo V, Nigri G, Cavallini M, Balducci G, Ramacciato G. Malnutrition and pancreatic surgery: prevalence and outcomes. J Surg Oncol. 2013;107(7):702–8.
de van der Schueren MAE, Laviano A, Blanchard H, Jourdan M, Arends J, Baracos VE. Systematic review and meta-analysis of the evidence for oral nutritional intervention on nutritional and clinical outcomes during chemo(radio)therapy: current evidence and guidance for design of future trials. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2018;29(5):1141–53.
Roeland EJ, Bohlke K, Baracos VE, Bruera E, Del Fabbro E, Dixon S, Fallon M, Herrstedt J, Lau H, Platek M, et al. Management of Cancer Cachexia: ASCO Guideline. J Clin Oncology: Official J Am Soc Clin Oncol. 2020;38(21):2438–53.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, Compher C, Correia I, Higashiguchi T, Holst M, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64.
Castillo-Martínez L, Castro-Eguiluz D, Copca-Mendoza ET, Pérez-Camargo DA, Reyes-Torres CA, Ávila EA, López-Córdova G, Fuentes-Hernández MR, Cetina-Pérez L, Milke-García MDP. Nutritional Assessment Tools for the identification of Malnutrition and Nutritional Risk Associated with Cancer Treatment. Revista De Investigacion Clinica; organo del Hospital de Enfermedades de la Nutricion. 2018;70(3):121–5.
Cong K, Chunwei G. Exploration of three different nutritional scores in predicting postoperative complications after pancreaticoduodenectomy. Nutr Hosp. 2022;39(1):101–10.
Longhurst C. Nutrition advice crucial, say cancer patients. Nurs Standard (Royal Coll Nurs (Great Britain): 1987). 2016;31(1):10.
Vasiloglou MF, Fletcher J, Poulia KA. Challenges and perspectives in nutritional counselling and nursing: a narrative review. J Clin Med 2019, 8(9).
Itoh S, Tsujita E, Fukuzawa K, Sugimachi K, Iguchi T, Ninomiya M, Maeda T, Kajiyama K, Adachi E, Uchiyama H, et al. Prognostic significance of preoperative PNI and CA19-9 for pancreatic ductal adenocarcinoma: a multi-institutional retrospective study. Pancreatology. 2021;21(7):1356–63.
Terasaki F, Sugiura T, Okamura Y, Ito T, Yamamoto Y, Ashida R, Ohgi K, Uesaka K. The preoperative controlling nutritional status (CONUT) score is an independent prognostic marker for pancreatic ductal adenocarcinoma. Updates Surg. 2021;73(1):251–9.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
Abe T, Amano H, Kobayashi T, Hattori M, Hanada K, Nakahara M, Ohdan H, Noriyuki T. Efficacy of the physiobiological parameter-based grading system for predicting the long-term prognosis after curative surgery for resectable pancreatic cancer. Eur J Surg Oncology: J Eur Soc Surg Oncol Br Association Surg Oncol. 2021;47(3 Pt B):613–9.
Asama H, Suzuki R, Takagi T, Sugimoto M, Konno N, Watanabe K, Nakamura J, Kikuchi H, Takasumi M, Sato Y, et al. Evaluation of inflammation-based markers for predicting the prognosis of unresectable pancreatic ductal adenocarcinoma treated with chemotherapy. Mol Clin Oncol. 2018;9(4):408–14.
Asaoka T, Miyamoto A, Maeda S, Tsujie M, Hama N, Yamamoto K, Miyake M, Haraguchi N, Nishikawa K, Hirao M, et al. Prognostic impact of preoperative NLR and CA19-9 in pancreatic cancer. Pancreatology. 2016;16(3):434–40.
Geng Y, Qi Q, Sun M, Chen H, Wang P, Chen Z. Prognostic nutritional index predicts survival and correlates with systemic inflammatory response in advanced pancreatic cancer. Eur J Surg Oncology: J Eur Soc Surg Oncol Br Association Surg Oncol. 2015;41(11):1508–14.
Kurahara H, Maemura K, Mataki Y, Sakoda M, Lino S, Hiwatashi K, Kawasaki Y, Arigami T, Ishigami S, Kijima Y, et al. Prognostication by inflammation-based score in patients with locally advanced pancreatic cancer treated with chemoradiotherapy. Pancreatology. 2015;15(6):688–93.
Lee SH, Chung MJ, Kim B, Lee HS, Lee HJ, Heo JY, Kim YJ, Park JY, Bang S, Park SW, et al. The significance of the Prognostic Nutritional Index for all stages of pancreatic Cancer. Nutr Cancer. 2017;69(3):512–9.
Onoe S, Yokoyama Y, Kokuryo T, Igami T, Mizuno T, Yamaguchi J, Watanabe N, Kawakatsu S, Ebata T. A presurgical prognostic stratification based on nutritional assessment and carbohydrate antigen 19 – 9 in pancreatic carcinoma: an approach with nonanatomic biomarkers. Surgery. 2021;169(6):1463–70.
Wang DS, Luo HY, Qiu MZ, Wang ZQ, Zhang DS, Wang FH, Li YH, Xu RH. Comparison of the prognostic values of various inflammation based factors in patients with pancreatic cancer. Med Oncol (Northwood Lond Engl). 2012;29(5):3092–100.
Abe T, Nakata K, Kibe S, Mori Y, Miyasaka Y, Ohuchida K, Ohtsuka T, Oda Y, Nakamura M. Prognostic Value of Preoperative Nutritional and Immunological Factors in patients with pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2018;25(13):3996–4003.
Park JS, Kim H-M, Jeung H-C, Kang SA. Association between early nutritional risk and overall survival in patients with advanced pancreatic cancer: a single-center retrospective study. Clin Nutr ESPEN. 2019;30:94–9.
Rivelsrud M, Paur I, Sygnestveit K, Nilsen RM, Tangvik RJ. Nutritional treatment is associated with longer survival in patients with pancreatic disease and concomitant risk of malnutrition. Clin Nutr. 2021;40(4):2128–37.
Trestini I, Paiella S, Sandini M, Sperduti I, Elio G, Pollini T, Melisi D, Auriemma A, Soldà C, Bonaiuto C, et al. Prognostic impact of Preoperative Nutritional risk in patients who undergo surgery for pancreatic adenocarcinoma. Ann Surg Oncol. 2020;27(13):5325–34.
Dang C, Wang M, Zhu F, Qin T, Qin R. Controlling nutritional status (CONUT) score-based nomogram to predict overall survival of patients with pancreatic cancer undergoing radical surgery. Asian J Surg. 2022;45(6):1237–45.
Kato Y, Yamada S, Suenaga M, Takami H, Niwa Y, Hayashi M, Iwata N, Kanda M, Tanaka C, Nakayama G, et al. Impact of the Controlling Nutritional Status score on the Prognosis after curative resection of pancreatic ductal adenocarcinoma. Pancreas. 2018;47(7):823–9.
Uemura S, Iwashita T, Ichikawa H, Iwasa Y, Mita N, Shiraki M, Shimizu M. Impact of Controlling nutritional status (CONUT) in patients with unresectable advanced pancreatic cancer receiving multi-agent chemotherapy: a single center, retrospective cohort study. Pancreatology. 2022;22(2):304–10.
Wang A, Sun B, Wang M, Shi H, Huang Z, He T, Li Q, Deng J, Fu W, Jiang Y. Predictive value of CONUT score combined with serum CA199 levels in postoperative survival of patients with pancreatic ductal adenocarcinoma: a retrospective study. PeerJ 2020, 2020(3).
Funamizu N, Sakamoto A, Utsunomiya T, Uraoka M, Nagaoka T, Iwata M, Ito C, Tamura K, Sakamoto K, Ogawa K, et al. Geriatric nutritional risk index as a potential prognostic marker for patients with resectable pancreatic cancer: a single-center, retrospective cohort study. Sci Rep. 2022;12(1):13644.
Hu SP, Chen L, Lin CY, Lin WH, Fang FQ, Tu MY. The prognostic value of preoperative geriatric nutritional risk index in patients with pancreatic ductal adenocarcinoma. Cancer Manage Res. 2020;12:385–95.
Kokumai T, Aoki S, Mizuma M, Maeda S, Ohtsuka H, Nakagawa K, Morikawa T, Motoi F, Kamei T, Unno M. Prognostic value of an inflammation-based nutritional score for patients with initially unresectable pancreatic adenocarcinoma undergoing conversion surgery following chemo-/radiotherapy. Surg Today. 2021;51(10):1682–93.
Bicakli DH, Uslu R, Guney SC, Coker A. The Relationship between Nutritional Status, Performance Status, and Survival among Pancreatic Cancer patients. Nutr CANCER-AN Int J. 2020;72(2):202–8.
Heckler M, Klaiber U, Hüttner FJ, Haller S, Hank T, Nienhüser H, Knebel P, Diener MK, Hackert T, Büchler MW, et al. Prospective trial to evaluate the prognostic value of different nutritional assessment scores for survival in pancreatic ductal adenocarcinoma (NURIMAS pancreas SURVIVAL). J cachexia Sarcopenia Muscle. 2021;12(6):1940–7.
Nakagawa S, Yamashita Y-i, Umezaki N, Yamao T, Okabe H, Imai K, Nitta H, Hashimoto D, Chikamoto A, Baba H. Serum marker score based on Prognostic Nutrition Index, Carcinoembryonic Antigen, and Carbohydrate Antigen 19 – 9 is Associated with recurrence for patients undergoing surgery for pancreatic ductal adenocarcinoma. Pancreas. 2018;47(9):1130–4.
Shirakawa T, Makiyama A, Shimokawa M, Otsuka T, Shinohara Y, Koga F, Ueda Y, Nakazawa J, Otsu S, Komori A, et al. C-reactive protein/albumin ratio is the most significant inflammatory marker in unresectable pancreatic cancer treated with FOLFIRINOX or gemcitabine plus nab-paclitaxel. Sci Rep. 2023;13(1):8815.
Hayashi M, Kobayashi D, Takami H, Inokawa Y, Tanaka N, Kurimoto K, Nakanishi K, Umeda S, Shimizu D, Hattori N, et al. Albumin-globulin ratio indicates the survival outcome of pancreatic Cancer cases who underwent Preoperative Treatment and Curative Surgical Resection. Nutr Cancer. 2023;75(5):1330–9.
Ma LX, Wang Y, Espin-Garcia O, Allen MJ, Jang GH, Zhang A, Dodd A, Ramotar S, Hutchinson S, Tehfe M, et al. Systemic inflammatory prognostic scores in advanced pancreatic adenocarcinoma. Br J Cancer. 2023;128(10):1916–21.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69.
Rocha NP, Fortes RC. Total lymphocyte count and serum albumin as predictors of nutritional risk in surgical patients. Arquivos brasileiros de cirurgia digestiva: ABCD = Brazilian Archives of Digestive Surgery. 2015;28(3):193–6.
Kheirouri S, Alizadeh M. Prognostic potential of the Preoperative Controlling Nutritional Status (CONUT) score in Predicting Survival of patients with Cancer: a systematic review. Adv Nutr (Bethesda Md). 2021;12(1):234–50.
Kang R, Li P, Wang T, Li X, Wei Z, Zhang Z, Zhong L, Cao L, Heckman MG, Zhang YW, et al. Apolipoprotein E epsilon 2 allele and low serum cholesterol as risk factors for gastric cancer in a Chinese Han population. Sci Rep. 2016;6:19930.
Niendorf A, Nägele H, Gerding D, Meyer-Pannwitt U, Gebhardt A. Increased LDL receptor mRNA expression in colon cancer is correlated with a rise in plasma cholesterol levels after curative surgery. Int J Cancer. 1995;61(4):461–4.
Jacobs RJ, Voorneveld PW, Kodach LL, Hardwick JC. Cholesterol metabolism and colorectal cancers. Curr Opin Pharmacol. 2012;12(6):690–5.
Wang C, Li P, Xuan J, Zhu C, Liu J, Shan L, Du Q, Ren Y, Ye J. Cholesterol enhances colorectal Cancer progression via ROS elevation and MAPK signaling pathway activation. Cell Physiol Biochemistry: Int J Experimental Cell Physiol Biochem Pharmacol. 2017;42(2):729–42.
Strasak AM, Pfeiffer RM, Brant LJ, Rapp K, Hilbe W, Oberaigner W, Lang S, Borena W, Concin H, Diem G, et al. Time-dependent association of total serum cholesterol and cancer incidence in a cohort of 172,210 men and women: a prospective 19-year follow-up study. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2009;20(6):1113–20.
Zhang Y, Kong FF, Zhu ZQ, Shan HX. Controlling Nutritional Status (CONUT) score is a prognostic marker in III-IV NSCLC patients receiving first-line chemotherapy. BMC Cancer. 2023;23(1):225.
Xiao Q, Li X, Duan B, Li X, Liu S, Xu B, Shi S, Zhang J, Qin H, Duan X, et al. Clinical significance of controlling nutritional status score (CONUT) in evaluating outcome of postoperative patients with gastric cancer. Sci Rep. 2022;12(1):93.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, Laviano A, Ljungqvist O, Lobo DN, Martindale R, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017;36(3):623–50.
Qiu M, Zhou YX, Jin Y, Wang ZX, Wei XL, Han HY, Ye WF, Zhou ZW, Zhang DS, Wang FH, et al. Nutrition support can bring survival benefit to high nutrition risk gastric cancer patients who received chemotherapy. Supportive care in cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2015;23(7):1933–9.
Zhou X, Liu J, Zhang Q, Rao S, Wu X, Zhang J, Li J. Comparison of the suitability between NRS2002 and MUST as the First-Step Screening Tool for GLIM Criteria in hospitalized patients with GIST. Front Nutr. 2022;9:864024.
Huang S, Wang S, Xie Y, He X, Yi X, Zhang J, Deng Z, Yin L. Application of NRS2002 in Preoperative Nutritional Screening for Patients with Liver Cancer. Journal of oncology 2021, 2021:8943353.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–83.
Cereda E, Pedrolli C, Zagami A, Vanotti A, Piffer S, Faliva M, Rondanelli M, Caccialanza R. Nutritional risk, functional status and mortality in newly institutionalised elderly. Br J Nutr. 2013;110(10):1903–9.
Cereda E, Zagami A, Vanotti A, Piffer S, Pedrolli C. Geriatric nutritional risk index and overall-cause mortality prediction in institutionalised elderly: a 3-year survival analysis. Clin Nutr. 2008;27(5):717–23.
Grinstead C, George T, Han B, Yoon SL. Associations of Overall Survival with Geriatric Nutritional Risk Index in Patients with Advanced Pancreatic Cancer. Nutrients 2022, 14(18).
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–40.
Deme D, Telekes A. [Prognostic importance of plasma C-reactive protein (CRP) in oncology]. Orv Hetil. 2017;158(7):243–56.
Tuttle CSL, Thang LAN, Maier AB. Markers of inflammation and their association with muscle strength and mass: a systematic review and meta-analysis. Ageing Res Rev. 2020;64:101185.
Zhu M, Ma Z, Zhang X, Hang D, Yin R, Feng J, Xu L, Shen H. C-reactive protein and cancer risk: a pan-cancer study of prospective cohort and mendelian randomization analysis. BMC Med. 2022;20(1):301.
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003;89(6):1028–30.
Yamada S, Fujii T, Yabusaki N, Murotani K, Iwata N, Kanda M, Tanaka C, Nakayama G, Sugimoto H, Koike M, et al. Clinical implication of inflammation-based prognostic score in pancreatic Cancer: Glasgow Prognostic score is the most Reliable parameter. Med (Baltim). 2016;95(18):e3582.
Proctor MJ, Morrison DS, Talwar D, Balmer SM, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC. An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumour site: a Glasgow inflammation outcome study. Br J Cancer. 2011;104(4):726–34.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Mengxia Yu and Xiaoxuan Li designed the research and wrote paper. Linglong Liu analyzed data, performed statistical analysis and filtered articles. Tianying Yao, Jiarong Li and Wang Su filtered articles and extracted data. All authors have read and agreed to the published version of the manuscript. And all authors declare no conflict of interest.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, M., Li, X., Chen, M. et al. Prognostic potential of nutritional risk screening and assessment tools in predicting survival of patients with pancreatic neoplasms: a systematic review. Nutr J 23, 17 (2024). https://doi.org/10.1186/s12937-024-00920-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-00920-w