Abstract
Background
Disease-related malnutrition is associated with adverse outcomes such as increased rates of morbidity and mortality, prolonged hospital stay, and extra costs of health care. This study was conducted to assess nutritional status among patients and to determine the risk factors for malnutrition in Iran university f.
Methods
Persian Nutritional Survey In Hospitals (PNSI) was a cross-sectional study that conducted in 20 university hospitals across Iran. All the patients with age range of 18 to 65 years, who were admitted or discharged, were assessed by subjective global assessment (SGA).
Results
In total, 2109 patients were evaluated for malnutrition. Mean values of age and body mass index were 44.68 ± 14.65 years and 25.44 ± 6.25 kg/m2, respectively. Malnutrition (SGA-B & C) was identified in 23.92% of the patients, 26.23 and 21% of whom were among the admitted and discharged patients, respectively. The highest prevalence of malnutrition was in burns (77.70%) and heart surgery (57.84%) patients. Multivariate analysis presented male gender (OR = 1.02, P < 0.00), malignant disease (OR = 1.40, P < 0.00), length of hospital stay (OR = 1.20, P < 0.00), and polypharmacy (OR = 1.06, P < 0.00) as independent risk factors for malnutrition. Malnutrition was not associated with age (P = 0.10).
Conclusion
This study provides an overall and comprehensive illustration of hospital malnutrition in Iran university hospitals, finding that one out of four patients were malnourished; thus, appropriate consideration and measures should be taken to this issue.
Similar content being viewed by others
Background
Disease-related malnutrition is associated with adverse outcomes such as increased rates of morbidity and mortality, prolonged hospital stay, impaired wound healing, high readmission rate, and increased costs for health care [1,2,3,4].
Malnutrition development is associated with insufficient dietary intake or malabsorption, increased nutritional needs, complications of the underlying disease, or a combination of these factors [5]. There is evidence that showed other factors are associated with malnutrition and affect its prevalence such as higher age [6, 7], weight loss [6], polypharmacy [8], educational level, health care system, and economic situation of the country where the study was performed [6, 9].
Studies performed in the United States indicate that approximately 32.7% of hospital patients are either malnourished or at nutritional risk [10], they also indicated that 11–45% of patients in England hospitals and home care suffer from malnutrition [9].
There are different reports of malnutrition prevalence in Iran, Hosseini reported 5.7% of patients on admission and 11% of discharged patients had malnutrition based on body mass index (BMI) ≤18.5 kg/m2 [11]. The prevalence of malnutrition among the cancer patients was reported as 53.1%, out of which 29.1% had moderate and 24% had severe malnutrition based on PG-SGA [12]. Forty-three percent of hemodialysis patients were moderately malnourished by SGA [13]. Another study reported that 23% of admitted patients had mild to moderate malnutrition and 6% had severe malnutrition based on SGA [14]. A recent study reported malnutrition rate of 32.62% by Nutrition Risk in Critically ill (NUTRIC) score (included of 1321) in ICU patients of Iran hospitals [15].
Proper nutritional status can play a notably important role in lowering the incidence of the malnutrition-disease defective cycle. Despite the importance of disease-related malnutrition and the great economic costs of this condition imposes on health systems, there is no comprehensive data on disease-related malnutrition and related risk factors in Iran hospitals. Therefore, this study aimed to assess nutritional status among patients in Iran hospitals and to determine different risk factors for malnutrition in hospitalized patients.
Methods
Persian Nutritional Survey In Hospitals (PNSI) is a multicenter, cross-sectional study conducted in 20 public hospitals which were selected based on a random stratified-cluster method. The sample size was estimated as 2100 patients, based on the relevant formula [16], and data of the study by Norouzy et al. (P = 0.32, Z = 95%, d = 0.02) [17]. Informed consent was obtained from all the patients recruited in this study. This study was approved by the Ethics Committee of Mashhad University of Medical Sciences (number 920923). Two educational sessions were held for investigators and a written instruction about data collection was provided.
In each hospital, the investigators referred to included clinical wards and assessed newly admitted or discharged patients on a specified date consecutively. The inclusion criteria comprised of admitted or discharged patients within the age of 18 to 65 years with Iranian nationality, also we excluded duplicated patients. Patients undergoing surgery on the data collection day, outpatients, patients with trauma or eating disorders, and patients admitted to maternity, obstetric, pediatric, orthopedic, and emergency departments or intensive care units (ICUs) were excluded from the study. The study was conducted from 24th to 28th November 2015. STROBE checklist of study is available as supplementary material 1.
Data collection
Patient characteristics, i.e., gender, date of birth (age), underlying disease, the main affected organ, comorbidity, the number of different prescriptions per day, and history of ICU stay and surgery were recorded. The length of hospital stay was calculated for discharged patients from the date of admission and date of the survey. Body weight was measured by standard Seca scale (Seca 620, Germany) in light clothes to the nearest 1 kg. Body height was assessed by Seca portable stadiometer (Seca 213, Germany) to the nearest 1 cm. Mid-arm circumference (MAC) was measured in mid-acromion and olecranon process interval at the non-dominant relaxed arm with a non-stretchable tape measure to the nearest 0.1 cm.
Nutritional status
The nutritional status of patients was assessed by subjective global assessment (SGA) and anthropometric measures (BMI and MAC) for all the admitted and discharged patients included in the study [18].
SGA is a valid and reliable tool for assessing nutritional status in hospitalized patients [19, 20]. Among the recommended screening tools, SGA enjoys the highest diagnostic accuracy for acute care patients. Baker et al. [19] and Detsky et al. [20] demonstrated that the use of SGA for evaluating patients yields reliable results with inter-observer reliability of 80%. SGA is comprised of two components: medical history and physical sign. In the medical history part, the severity and pattern of weight loss, dietary intake, gastrointestinal symptoms, and functional capacity are evaluated. In the physical signs part, loss of subcutaneous fat, muscle mass, and presence of edema and ascites were assessed. According to this tool, patients are classified as well-nourished (SGA-A), moderately malnourished (SGA-B), and severely malnourished (SGA-C) [14].
Body mass index (BMI; weight/height2) is most commonly used for assessing nutritional status. BMI was calculated as weight (kg) divided by squared height (m2) [21]. If BMI was less than 18.5, between 18.5 and 25, and higher than 25, the patient was considered as malnourished, normal, and overweight or obese, respectively.
Statistical analysis
Quantitative variables with normal distribution were expressed as mean, standard deviation, and range. Quantitative variables with non-normal distribution were reported as median and range. Stratified variables were reported as frequency and percentage. Analysis of nominal qualitative data was performed by non-parametric tests such as the Chi-squared test. Mann-Whitney test was used for ordinal qualitative variables; for quantitative variables with normal distribution, t-test was run. Odds ratios (OR) were reported with 95% confidence interval. To identify independent risk factors logistic regression was used. A P-value less than 0.05 was considered statistically significant.
Results
Patient characteristics
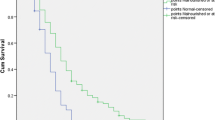
Participant flow chart is presented in Fig. 1, 2324 patients were assessed for eligibility, finally data of 2109 patients were analyzed. Patients from 100 medical wards of 20 hospitals were assessed in this study. The mean age of the participants was 44.68 ± 14 years of whom 50% (n = 1055) were male and 50% (n = 1054) were female. Demographics of the study population are shown in Table 1. Moreover, the mean values for weight, height, and BMI were 68.18 ± 16.53 kg, 164.43 ± 9.75 cm, and 25.44 ± 6.25 kg/m2, respectively. In 8.72% (n = 183) of the patients, BMI was less than 18.50 kg/m2.
Nutritional status
The nutritional data of the patients are presented in Table 2. The overall prevalence of malnutrition was 23.92% (n = 479 cases), which is determined by combining the SGA-B (moderate malnutrition, 17.33%) and –C (severe malnutrition, 6.59%) also 76.07% (n = 1523) of patients were identified as SGA-A (with normal nutritional status).
Weight loss in the last 3 months was reported by 37.31% (n = 799) of the respondents, of whom 217 subjects were well-nourished and 36 subjects were malnourished.
Approximately 3 and 0.50% of the patients had severe to moderate edema and ascites, respectively. A significant statistical association was found between BMI and SGA categories (P < 0.05). The highest prevalence of malnutrition was observed in burns department (77.70%), followed by cardiac Surgery (57.84%), and hematology departments (50.00%). The lowest number of patients with malnutrition was in the ophthalmology department (2.51%) (Table 3).
Analysis of factors which may have been associated with malnutrition shows male gender (OR = 1.023, 1.015-1.031 P < 0.001), malignant disease (OR = 1.409, 1.080-1.830 P < 0.001), number of medications (OR = 1.066, 1.030-1.104 P < 0.001) and length of hospital stay (OR = 1.206, 1.170-1.304 P < 0.001) were independent risk factors for malnutrition. Age and disease type were not associated with malnutrition (P > 0.05).
Discussion
This was the first multicenter study to determine the prevalence of malnutrition in patients of general hospitals in Iran. This study indicated that 23.92% of patients suffered from malnutrition. Independent factors associated with malnutrition were as follows: male gender, malignant disease, polypharmacy, and length of hospital stay.
The results of this study are comparable with reports on the prevalence of malnutrition in Europe and the USA, which shows the importance of identifying malnutrition in hospitals throughout the world. In the United States, Abby C. Sauer found that 33% of patients had malnutrition risk (MST score ≥ 2) [10]. In Europe, malnutrition prevalence was reported as 13% in patients [22].
The results of the present study are in line with those of a national study conducted in Germany using SGA that reported 28% of patients suffered from malnutrition. A study in European hospitals showed that the prevalence of malnutrition ranged between 10 and 50% depending on the studied region [12]. A study using SGA in Korea reported a 22% prevalence of malnutrition for hospitalized patients [23]. Evaluation of nutrition risks in Turkish hospitals demonstrated that 15% of patients were at nutrition risk on admission [22]. The prevalence of malnutrition diagnosed as determined by SGA in Australian hospitals was found to be 30% in patients [18].
There are various reports on the prevalence of malnutrition around the world globe, which might be due to features of the studied samples, the tool used to identify malnutrition, and the type of assessed centers. Moreover, it should be noted that the mean age of patients in this study (44.68 years) was less than other studies (63.93 years) performed in Australia and (52.21 years) Latin America, while age was shown to be an independent risk factor for malnutrition. Additionally, most patients in the present study did not have malignant diseases that could affect the prevalence of malnutrition.
The present study did not demonstrate any association between age and malnutrition that could be pertinent to the low mean age of the samples (44.68 years) [8]. In the study performed in Germany, which divided patients into two groups of aged under 65 and equal to or more than 65 years, malnutrition was not found to be associated with age in the group aged less than 65 years, while in those aged more than 65 years, age was identified as an independent risk factor for malnutrition [8]. In the present study, the prevalence of malnutrition in males was 5.20% higher than in females. This finding is in line with the findings of a study conducted in Argentina [24] and inconsistent with the results of a study by Aliabadi et al., while no difference was observed in the frequency between the two genders in another study [6]. The present findings suggest an association between malnutrition and malignant diseases. Lack of energy protein intake in cancer patients might be due to anorexia and other complications of chemotherapy, e.g., nausea, vomiting, changes in the sense of taste, xerostomia, and early satiety [13, 25]. The multivariate analysis reflected that malnutrition patients at discharge compared to those without malnutrition had a longer duration of hospital stay. Studies using various assessment tools have also shown length of hospitalization as an important risk factor for malnutrition [11, 21]. In this study, the number of administered medications was considered as an independent risk factor for malnutrition. This association was considered in several other studies [26]. The number of medications was closely related to malnutrition, which similar to benign and malignant diseases, however, it can be concluded that polypharmacy itself acts as a major contributing factor to malnutrition, especially given that a large number of drugs are known to decrease appetite or cause vomiting. Recent evidence confirms a synergistic negative effect of polypharmacy and malnutrition on outcomes of older adults [27].
Strength and limitation
The current study was the first national survey of hospital malnutrition and associated factors in Iran public hospitals which used a valid and reliable tool for nutritional assessment malnutrition, however, there were some limitations such as didn’t assess of malnutrition trend during hospitalization, because of the cross-sectional design of the study, another limitation was assessment by different investigators in hospitals. In further studies status of nutritional care and management of patients can be assessed, also effect of interventional measures in decline and management of problem could be evaluated.
The data of this study provide an overall and comprehensive illustration of the nutritional status of patients and identify groups at higher risk for malnutrition in Iranian university hospitals. Control and management of this problem need a structural approach that should contain all these aspects: 1- administration of a universal assessment to screening patients for nutritional risk to identify patients with or at risk of malnutrition, 2- handle multidisciplinary supportive nutrition care to provide appropriate nutritional therapy, 3- take measures to promote continuity of care after discharge from acute care hospitals. Notable, improve knowledge and consciousness of clinician’s team to consider malnutrition as a specific disease entity that concludes significant patient and economic outcomes and requires active management.
Conclusion
This study revealed that almost 24% of patients in public hospitals suffer from malnutrition. Male gender, malignancy, polypharmacy, and length of hospital stay were identified as independent risk factors for malnutrition. While the present study cannot determine to what extent and how malnutrition affects the outcomes, there is evidence showing effects on outcome and health costs, in this regard screening and nutrition interventions can improve the results.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. There is no public access to the databases.
Abbreviations
- ICU:
-
Intensive care units
- ICU:
-
Mid-arm circumference
- BMI:
-
Body mass index
- SGA:
-
Subjective global assessment
References
Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8(2):514–27.
Badosa EL, Tahull MB, Casas NV, Sangrador GE, Méndez CF, Meseguer IH, et al. Hospital malnutrition screening at admission: malnutrition increases mortality and length of stay. Nutr Hosp. 2017;34(4):907–13.
Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27:5e15.4.
Cardenas D, Bermúdez C, Pérez A, Diaz G, Cortes LY, Contreras CP, et al. Nutritional risk is associated with an increase of in-hospital mortality and a reduction of being discharged home: results of the 2009–2015 nutritionDay survey. Clin Nutr ESPEN. 2020;38:138–45.
Saunders J, Smith T, Stroud M. Malnutrition and undernutrition. Medicine. 2011;39(1):45–50.
Fragas RF, Oliveira MC. Risk factors associated with malnutrition in hospitalized patients. Rev Nutr. 2016;29:329–36.7.
Veramendi-Espinoza LE, Zafra-Tanaka JH, Salazar-Saavedra O, Basilio-Flores JE, Millones-Sánchez E, Pérez-Casquino GA, et al. Prevalence and associated factors of hospital malnutrition in a general hospital; Peru, 2012. Nutr Hosp. 2013;28(4):1236–43.
Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563–72.
Edington J, Boorman J, Durrant ER, et al. Prevalence of malnutrition on admission to four hospitals in England. The malnutrition prevalence group. Clin Nutr. 2000;19:191–5.
Sauer AC, Goates S, Malone A, Mogensen KM, Gewirtz G, Sulz I, et al. Prevalence of malnutrition risk and the impact of nutrition risk on hospital outcomes: results from nutritionDay in the US. J Parenter Enter Nutr. 2019;43(7):918–26.
Hosseini S, Amirkalali B, Nayebi N, Heshmat R, Larijani B. Nutrition status of patients during hospitalization, Tehran, Iran. Nutr Clin Pract. 2006;21(5):518–21.
Khoshnevis N, Ahmadizar F, Alizadeh M, Akbari ME. Nutritional assessment of cancer patients in Tehran, Iran. Asian Pac J Cancer Prev. 2012;13(4):1621–6.
Dorri AM, Koor BE, Nakhaie MR. Subjective global assessment in hemodialysis patients in an Iranian care hospital. J Adv Med Med Res. 2017;23(4):1–7.
Gholami SS, Ardekani TM, Karami K, Taheri A, Gholamnezhad M. Evaluation of malnutrition status in patients admitted to Shahid Rajaee Hospital in Gachsaran City in 2016. World Fam Med J Inc Middle East J Fam Med. 2017;99(5588):1–7.
Mishamandani ZJ, Norouzy A, Hashemian SM, Khoundabi B, Rezaeisadrabadi M, Safarian M, et al. Nutritional status of patients hospitalized in the intensive care unit: a comprehensive report from Iranian hospitals, 2018. J Crit Care. 2019;54:151–8.
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14.
Norouzy A, Hashemi P, Amiri A, Salehi M, Deldar K, Fakhar Y, et al. Adult malnutrition screening, prevalence in four Iranian hospitals: cross-sectional study. Mediterr J Nutr Metab. 2012;5(1):45–8.
Agarwal E, Ferguson M, Banks M, Bauer J, Capra S, Isenring E. Nutritional status and dietary intake of acute care patients: results from the nutrition care day survey 2010. Clin Nutr. 2012;31(1):41–7.
Baker JP, Detsky AS, Wesson DE, Wolman SL, Stewart S, Whitewell J, et al. Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med. 1982;306:969–72.
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson R, et al. What is subjective global assessment of nutritional status. JPEN J Parenter Enteral Nutr. 1987;11(1):8–13.
Raymond JL, Morrow K. Krause and Mahan’s food and the nutrition care process e-book. Amsterdam: Elsevier Health Sciences; 2020.
Ostrowska J, Sulz I, Tarantino S, Hiesmayr M, Szostak-Węgierek D. Hospital malnutrition, nutritional risk factors, and elements of nutritional care in Europe: comparison of polish results with all European countries participating in the nDay survey. Nutrients. 2021;13(1):263.
Kang MC, Kim JH, Ryu SW, Moon JY, Park JH, Park JK, et al. Prevalence of malnutrition in hospitalized patients: a multicenter cross-sectional study. J Korean Med Sci. 2018;33(2):e10.
Tangvik RJ, Tell GS, Guttormsen AB, Eisman JA, Henriksen A, Nilsen RM, et al. Nutritional risk profile in a university hospital population. Clin Nutr. 2015;34(4):705-11.
Correia MI, Perman MI, Waitzberg DL. Hospital malnutrition in Latin America: a systematic review. Clin Nutr. 2017;36(4):958–67.
Kose E, Wakabayashi H, Yasuno N. Polypharmacy and malnutrition management of elderly perioperative patients with cancer: a systematic review. Nutrients. 2021;13(6):1961.
Little MO. Updates in nutrition and polypharmacy. Curr Opin Clin Nutr Metab Care. 2018;21(1):4–9.
Acknowledgements
Not applicable.
Funding
Fund was obtained by Abdolreza Norouzy. This study was funded by Ministry of Medical and Health Education of Iran, Mashhad University of Medical Sciences, Kerman University of Medical Sciences, Kermanshah University of Medical Sciences, and Neyshabour University of Medical Sciences. The authors would like to thank officials of the included hospitals.
Author information
Authors and Affiliations
Contributions
All authors contributed to study design, SP, FSH, JK, A-AH, PT, YP, MA-N, MS, MH, and AN contributed to data collection, SP, FSH, AN, SE-H, OP analyzed data, SP and FSH provided manuscript. The manuscript has been revised and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences. Informed consent was obtained from each participate.
Consent for publication
As our manuscript does not include any individual data or sensitive personal information, therefore consent for publication is “Not Applicable” in this case.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
STROBE checklist for nutritional epidemiologic studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Poudineh, S., Shayesteh, F., Kermanchi, J. et al. A multi-centre survey on hospital malnutrition: result of PNSI study. Nutr J 20, 87 (2021). https://doi.org/10.1186/s12937-021-00741-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-021-00741-1