Abstract
Background
Dispositional optimism is a psychological trait that has been associated with positive health outcomes such as reduced risk of cardiovascular diseases. However, there is little knowledge on the relationship between optimism and dietary intake in the population. The objective of this cross-sectional study was to assess whether optimism was associated with overall diet quality, food group consumption and snacking.
Methods
In 2016, 32,806 adult participants from the NutriNet-Santé study completed the Life-Orientation Test Revised (LOT-R) which assesses dispositional optimism. Overall diet quality (assessed by the mPNNS-Guideline Score) and consumption of 22 food groups were evaluated using at least three self-reported 24-h dietary records. Snacking behavior was evaluated by an ad-hoc question. Logistic and linear regressions were used to analyze the associations between optimism and these dietary behaviors, taking into account socio-demographic, lifestyle and depressive symptomatology characteristics.
Results
Optimism was associated with greater overall diet quality (β (95% CI) = 0.07 (0.004–0.11), P < 0.0001) and higher consumption of fruit and vegetables, seafood, whole grains, fats, dairy and meat substitutes, legumes, non-salted oleaginous fruits, and negatively associated with consumption of meat and poultry, dairy products, milk-based desserts, sugar and confectionery. In addition, optimism was associated with less snacking (OR (95% CI) = 0.89 (0.84, 0.95)). In contrast, optimism was associated with higher consumption of alcoholic beverage (β (95% CI) = 5.71 (2.54–8.88), P = 0.0004) and appetizers (OR (95% CI) = 1.09 (1.04, 1.14)). Finally, no association was observed between optimism and energy intake.
Conclusions
Optimism was associated with better overall diet quality and less snacking. It was also associated with consumption of healthy food groups as well as unhealthy food groups typically consumed in social eating occasions. These findings suggest that optimism could be taken into account in the promotion of a healthy eating behavior.
Similar content being viewed by others
Background
The impact of nutrition on chronic diseases, including obesity, cardiovascular diseases and cancer is utterly recognized [1,2,3,4]. Many factors influence eating behavior, including psychological ones [5]. So far, the literature has largely focused on negative psychological characteristics associated with eating behavior such as emotional eating [6, 7], cognitive restraint [8, 9] or impulsivity [10, 11]. However, more recently, research has started to focus on positive psychological traits that could have a beneficial impact on dietary behavior and nutritional status such as intuitive eating [12] or self esteem [13] . Positive characteristics generally allow the individual to easily overcome usual life stresses, perform successful work, and contribute to the social life of their community [14]. Therefore they may have positive consequences on physical health [14]. A perspective focused on building competency rather than on correcting weakness could present a major stride in health prevention [15].
One type of positive trait, called dispositional optimism is defined as the general expectation that good things, rather than bad things, will happen in the future [16]. It has been demonstrated in controlled randomized trials that optimism can be learned [17], leading to potential novel interventions to improve public health. Higher levels of dispositional optimism, assessed by validated quantitative scales, have been associated with better physical health, especially lower risk of cardiovascular diseases [18, 19], lower mortality [19, 20] and healthy aging [21]. These associations could be due to a more proactive approach to health promotion in optimistic people or better emotional responses to adversity [22]. Previous scientific literature has shown that dispositional optimism was associated with less smoking and more exercise [23]. Few studies investigated and observed an association between optimism and healthier diets. Optimism was associated with higher overall diet quality [24, 25] and greater consumption of specific healthy food groups such as fruit and vegetables [26, 27] or whole grains [28]. Although optimists are supposed to think that favorable outcomes are possible and act accordingly [29] some theorizing suggests that the positive thoughts associated with optimism might lead people to feel as if they do not need to engage in healthy behaviors [30]. Consistently, it has been observed in a cross-sectional study that dispositional optimism was associated with higher intake of alcoholic beverages [31].
Additional studies are needed since most of these studies on optimism and dietary intake have been based on specific populations such as women, older individuals or individuals with pathologies and did not consider psychological distress as potential confounders [23]. In addition, to our knowledge, no study has so far examined the association between optimism and snacking behavior. Snacking, an aspect of dietary behavior which can be defined as eating occasions apart from main meals has been associated with lower nutrient density and higher energy density compared to main meals [32], and with both healthy and unhealthy food choices [33]. In addition, greater eating frequency may contribute to an unbalanced diet that could consequently lead to overweight or obesity [34].
The aim of this study was to explore how optimism was associated with overall diet quality, energy and macronutrient intake, food group consumption and snacking behavior in a large sample of adults from the French general population, taking into account socio-demographic, lifestyle and depressive symptomatology characteristics.
Methods
Population
This work was conducted as part of the NutriNet-Santé study, which is a large ongoing web-based prospective cohort launched in France in May 2009 (www.etude-nutrinet-sante.fr). The rationale, design and methods of the study have been fully described elsewhere [35]. Briefly, this study was designed to investigate the relationship between nutrition and health, as well as the determinants of dietary behaviors and nutritional status. It was implemented in a general population, including Internet-using adult volunteers aged 18 or older. At inclusion, participants have to complete several self-reported web-based questionnaires to assess their diet, physical activity, anthropometric measures, lifestyle characteristics, socioeconomic conditions and health status. Participants then complete this same set of questionnaires every year after inclusion. Another set of optional questionnaires related to determinants of eating behaviors, nutritional status, and specific health-related aspects are sent each month.
The NutriNet-Santé study was conducted according to guidelines laid down in the Declaration of Helsinki. All procedures were approved by the International Research Board of the French Institute for Health and Medical Research (IRB Inserm n° 0000388FWA00005831) and the Commission Nationale de l’Informatique et des Libertés (CNIL n° 908,450 and n° 909,216). Electronic informed consent was obtained from all participants. The study was registered at clinicaltrial.org (Clinical Trial no. NCT03335644).
Data collection
Dispositional optimism
Dispositional optimism was measured with the French version [36] of the Life Orientation Test revised (LOT-R) [16]. The LOT-R was administered between September and December 2016 to the NutriNet-Santé cohort. The questionnaire assesses dispositional optimism, which can be defined by a generalized expectation that good things will happen [37]. The LOT-R is a 6-item self-report questionnaire with three positively worded statements (e.g. ‘In uncertain times, I usually expect the best’) and three negatively worded statements (e.g. ‘If something can go wrong for me, it will’). Each item scored on a 5-point Likert scale ranging from 0 (strongly disagree) to 4 (strongly agree). After reversing the scoring for the negatively worded items, item scores were summed up and divided by the number of item leading to an overall optimism score ranging from 0 to 4 with higher scores representing greater optimism. We considered the LOT-R as an unidimensional scale following recommendations [38, 39]. In our population, the LOT-R displayed good internal consistency (Cronbach’s α = 0.84).
Assessment of food group consumption and diet quality
In the NutriNet-Santé study, all participants are invited to complete 24-h dietary records at baseline and every 6 months thereafter. The three self-administrated non-consecutive validated 24 h dietary records were randomly distributed between week and weekend days (2 weekdays and 1 weekend day). In the present study, we selected participants who completed at least three dietary records between the 2 years preceding and the 18 months following the completion of the LOT-R questionnaire, therefore between 2014 and 2018. The dietary record is completed by using an interactive interface allowing the selection of > 3300 food or beverage items and is designed for self-administration on the Internet [40]. Participants report all foods and beverages consumed at breakfast, lunch, dinner, and other eating occasions. They estimate the amounts eaten using standard measurements or using validated photographs [41]. Participants can choose among 7 portion sizes for most food products: 3 main portion sizes plus 2 intermediate and 2 extreme sizes. Nutrient intakes are estimated by using the published NutriNet-Santé food composition table [42]. Mean daily food intake (in grams per day) is weighted for the type of day of the week (weekday or weekend). Participants with unlikely estimates of energy intake were identified as under-reporters by using the method proposed by Black [43]. Briefly, basal metabolic rate was calculated according to age, gender, weight and height using Schofield’s equations [44]. Energy requirement was based on basal metabolic rate and physical activity level. The ratio between energy intake and estimated energy requirement was calculated and individuals with ratios below Goldberg cut-off were excluded [45]. The 24 h-record used in the NutriNet-Santé cohort has been validated versus blood and urinary biomarkers [46, 47], and versus an interview by a dietitian [40]. For the present study, we defined 22 food groups: fruits and vegetables, seafood (fish and shellfish), meat and poultry, processed meat, eggs, dairy products (e.g. milk, yogurts with less than 12% of added sugar), cheese, dairy and meat substitutes (e.g. soya-based products, vegetarian steaks), milk-based desserts (e.g. flan, cream desserts), starchy food, whole grains, legumes, fats (oil, butter, and margarine), sugary and fatty foods (e.g. cakes, chocolate, ice cream, pancakes), sugar and confectionery (e.g. honey, jelly, sugar, candy), fast food (e.g. pizzas, hamburgers, sandwiches, hot dogs), appetizers which included salted non oleaginous appetizers (e.g. crisps, salted biscuits) and salted oleaginous appetizers, non-salted oleaginous fruits (e.g. non-salted nuts, non-salted almonds), non-alcoholic beverages (including sweetened and light non-alcoholic beverages but excluding water) and alcoholic beverages.
The overall diet quality was assessed using the modified French National Nutrition and Health Program Guideline Score (mPNNS-GS). This score is an a priori nutritional overall diet quality score reflecting adherence to the French nutritional recommendations [48]. The mPNNS-GS is based on the PNNS-GS score [48], but accounts for dietary component only, excluding the physical activity component [49]. The score includes 12 components: eight refer to food serving recommendations (fruits and vegetables; starchy foods; whole grains; dairy products; meat, eggs and fish; seafood; vegetable fat; water vs soda) and four refer to moderation of intake (added fat; salt; sweets; and alcohol). Points are deducted for overconsumption of salt, of added sugars from sweetened foods and when energy intake exceeds the energy requirement (as assessed by physical activity level and basal metabolic rate calculated using Schofield equations [44]) by more than 5%. The score has a maximum of 13.5 points, with a higher score indicating better overall diet quality.
Assessment of snacking
A meal pattern questionnaire was administered between April and October 2014 where snacking, defined as eating food between meals, was assessed. Participants were asked “How often do you usually snack in the daytime?” Responses were rated on a 7-point scale from “never” to “6 times or more per day, each day” and further classified into 4 frequency categories: never, < once a week, ≥ once a week (and < once a day) and ≥ once a day. A binary variable was also computed with participants who never snacked against the others.
Covariates
At baseline and once per year, self-administered questionnaires are used to collect data on socio-demographic, economic characteristics, and anthropometric characteristics [50]. The data closest to the date of completion of the LOT-R were used. Potential confounders of the association between optimism and dietary intake were selected based on data of the literature. They were as follow: age (years), gender, education level (primary, secondary, undergraduate, and postgraduate), occupational status (unemployed, student, self-employed and farmer, employee and manual worker, intermediate profession, managerial staff and intellectual profession, retired), and monthly income per household unit (< 1200; 1200-1799; 1800-2299; 2300-2699; 2700-3699; ≥ 3700 euros per household unit and “unwilling to answer”), smoking status (never smoker, former smoker, and current smoker), level of physical activity, BMI, and depressive symptomatology. More precisely, monthly household income was provided and estimated per consumption unit according to household composition. The number of people in the household was converted into number of consumption units (CU) according to the OECD (Organization for Economic Cooperation and Development) equivalence scale: one CU is attributed for the first adult in the household, 0.5 for other persons aged 14 or older, and 0.3 for children under 14 [51]. Physical activity was assessed using the short form of the French version of the International Physical Activity Questionnaire (IPAQ) [52]. Energy expenditure expressed in Metabolic Equivalent of Task (MET-minutes/week) was estimated and three levels of physical activity were constituted (low (< 30 min/day), moderate (30-60 min/day), and high (≥ 60 min/day)). BMI (kg/m2) was calculated based on self-reported weight and height [53, 54]. Participants were classified as underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30) and obesity (BMI ≥ 30) [55]. Depressive symptomatology was assessed with the French version of the CES-D (Center for Epidemiology Studies Depression scale) [56, 57] between November 2017 and May 2018. It is a 20-item questionnaire rated on a 4-point scale with higher scores indicating higher depressive symptomatology. Participants were classified according to their level of depressive symptomatology (no vs yes) using the cutoff of 16 commonly used [56]. The CES-D had an excellent internal consistency (Cronbach’s α = 0.91) in our sample [56].
Statistical analysis
To compare included with excluded participants, we used Student t-test, and Pearson’s chi-square test. Individual characteristics, overall diet quality, energy and macronutrient intake, food group consumption and snacking behavior were described as means and standard deviation (SD), median and interquartiles (IQRs) or percentages across the various categories. To describe the relationships between optimism and participants’ characteristics, Pearson correlations for continuous variables and general linear models for categorical variables were used. To estimate the association between optimism (independent variable), overall diet quality (dependent variable), energy and macronutrient intake (dependent variable), and food group consumption (dependent variable), we used multivariable regression analyses. Multivariable linear regressions analyses were used for dependent variables with a normal distribution. In the case of variables without a normal distribution (i.e. processed meat, eggs, dairy products and meat substitutes, milk-based desserts, legumes, fast food, appetizers, non salted oleaginous fruits), two levels were defined: no intake vs intake and binary logistic regressions were used. Finally, to measure the association between optimism and snacking, we used binary (no vs yes) and multinomial logistic regressions (4 frequency categories: never, < once a week, ≥ once a week (and < once a day) and ≥ once a day). For logistic regressions, the strength of the association was estimated by calculating adjusted odds ratios (ORs) and 95% confidence intervals (95% CI). Two models were tested. A first model was adjusted for age and gender. A second model was additionally adjusted for education level, occupational status, monthly income per household unit, energy intake (except when energy was the outcome), smoking status, physical activity, BMI and depressive symptomatology. Analyses were not stratified by gender since the interactions between optimism and gender were non-significant for most food groups. Missing data regarding confounders were handled using multiple imputations (mice method) by fully conditional specification (5 imputed datasets). All tests were 2-sided and statistical significance was set at 5%. Statistical analyses were performed using SAS software (SAS Institute Inc., version 9.4).
Results
Characteristics of the sample
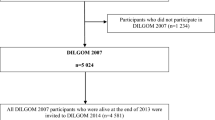
A total of 32,806 participants of NutriNet-Santé study completed the optional LOT-R questionnaire from the 159,351 subjects who received it. A total of 78 participants were excluded because they presented an acquiescence bias (agreeing to all questions without consideration of reversed items). From the 32,728 remaining participants 19,335 had completed at least 3 valid 24-h dietary records (excluding under-reporters), 17,849 had available data to calculate the mPNNS-GS and 28,948 had completed the snacking behavior assessment (see Additional file 1: Figure S1). Therefore, each analysis was carried on a different subsample to make better use of available data. Compared with excluded participants (those who completed the LOT-R but less than three 24-h dietary records), included participants had a higher level of optimism (LOT-R) (2.54 ± 0.64 vs 2.48 ± 0.66), were older (56.1 ± 13.8-year-old vs 53.2 ± 14.0), had a higher proportion of men (27.5% vs 24.5%) and of individuals with university education (69.9% vs 65.4) (all P < 0.0001).
Table 1 describes individual characteristics of participants and the association with optimism. On average, optimism was higher in men, in individuals with a higher level of education, in self-employed or farmer, in managerial staff or intellectual professions and in individuals with higher monthly household income. In addition, optimism was higher in individuals with a normal range BMI or overweight, in individuals with higher physical activity level, in smokers (former or current) and in individuals with no depressive symptomatology. No association with age was observed. Table 2 shows the descriptive characteristics of overall diet quality, energy, macronutrient intake, food group consumption and snacking. Around three quarters of the participants declared snacking practices, among which a majority snacked more than once a week (and less than once a day).
Association between optimism, diet quality, and intakes of energy, macronutrients and food groups
Tables 3 and 4 present the association between optimism and dietary intake. A higher score of optimism was associated with a greater overall diet quality (mPNNS-GS), higher intake of lipids (% of energy) and lower intake of carbohydrates and proteins (% of energy). No association with energy (nor energy without alcohol) was observed. Regarding food groups, participants with higher optimism reported higher consumption of fruits and vegetables, seafood, whole grains, fats, dairy and meat substitutes, legumes, appetizers (including salted non oleaginous appetizers and salted oleaginous appetizers), non-salted oleaginous fruits and alcoholic beverage. They also had lower intakes of meat and poultry, dairy products, milk-based desserts and sugar and confectionery.
Association between optimism and snacking behavior
Table 5 shows the association between optimism and snacking behavior. Optimism was inversely associated with overall snacking. More specifically, the association between optimism and snacking was observed for individuals who snacked at least once a week.
Discussion
To our knowledge, this study is the first to assess the association between optimism and eating behavior using 24 h records and taking socio-demographic, lifestyle and depressive symptomatology characteristics into account in a very large population-based sample of adults. Our findings suggest that dispositional optimism was associated with a higher overall diet quality. Optimism was positively associated with consumption of fruits and vegetables, seafood, whole grains, fats, dairy and meat substitutes, legumes, and non-salted oleaginous fruits, and negatively associated with consumption of meat and poultry, dairy products, milk-based desserts and sugar and confectionery. However, optimism was positively associated with alcoholic beverages and appetizers. Optimism was associated with lower snacking and snacking frequency. Finally, no association with energy was found.
Optimism, diet quality, and intakes of energy, macronutrients and food groups
We found that dispositional optimism was associated with an overall greater diet quality supporting previous data showing a positive association between optimism and alternative healthy eating index (AHEI) in postmenopausal women [24] and with a healthy diet metric of the ideal cardiovascular health based on the AHA guidelines in adults [25]. Our data indicated no association between optimism and energy, while optimism was associated with higher intake of lipids, and lower intake of proteins and carbohydrates. To our knowledge, no other study has investigated the association between optimism, energy and macronutrient intake. These results suggest that optimism could have an impact on diet quality but not on the overall energy intake. Our data showed that optimism was mainly associated with greater intake of healthy food groups including fruits and vegetables, seafood, whole grains, legumes, non-salted oleaginous fruits and lower intake of unhealthy food including milk-based desserts and sugar and confectionery. In agreement, previous data showed that higher optimism was associated with greater intake of fruits and vegetables [26, 27], and whole grains [28]. Healthier choices in optimistic individuals may be due to a more proactive approach to health promotion [22]. Optimistic individuals have been shown more likely to adopt healthier behaviors including less smoking and more exercise [23]. Optimists also show a better profile of emotional responses to adversity (less distress, more positive emotions) due to more effective coping reactions, which can lead to healthier choices [22]. Our results showing an association between optimism and dietary intake are important since it has been demonstrated in randomized trials that optimism can be learned [17], leading to potential novel interventions to improve public health. However, the reverse has also been suggested; that is, individuals who engage in healthier dietary behaviors may also as a consequence be more optimistic [58, 59].
In contrast, our findings also showed that higher optimism was associated with some unhealthy dietary items, i.e. appetizers (both oleaginous and non-oleaginous) and alcoholic beverages. In agreement, previous data showed higher intake of alcohol in elderly with higher optimism [31]. However, no association between optimism and median alcohol intake was observed in another study [27]. The large majority of meals in France is shared with others [60]. Appetizers and alcoholic beverages are typically eaten during social eating occasions and in particular in France during the so called “apéritif”. The apéritif is a moment of conviviality shared by people before the main meal and often consisting of raw vegetables, crisps, salted nuts, processed meat, cheese and quiches/pizzas [61, 62] as well as alcoholic and sweetened non-alcoholic drinks [62]. Studies have shown that optimists have greater social connections than pessimists [22, 63, 64] suggesting that they are more likely to share their meals with other people and therefore to include an apéritif in their meal.
Optimism and snacking behavior
Our results showed that more optimistic individuals were less likely to snack and to snack often compared with less optimistic individuals. To our knowledge, there is no data available assessing the association between optimism and snacking behavior. Snacking has been associated with depressive symptomatology [65], perceived stress [66] and coping strategies [67]. We can hypothesize that the better coping strategies observed in more optimistic individuals [29] lead to lower psychological distress [68, 69], which can in turn decrease snacking through lower emotional eating. Indeed, emotional eating has been associated with both stress [70, 71] and snacking [7].
Strengths and limitations
The main strength of this study was the use of at least three 24-h dietary records that allowed us to have a good representation of the participants’ usual diet. As previously shown, usual intake of population can be estimated based on at least two recalls [72]. Another important strength is the large sample size, which provided a high statistical power. The use of the Internet for data collection permitted access to a heterogeneous sample of volunteers. In addition, important socio-demographic and economic confounding factors have been taken into account. However we cannot exclude the possibility of residual confounding due to other individual or environmental factors. The Web-based version of the LOT-R questionnaire minimized missing data by using automatic controls and alerts to users. The LOT-R was validated in French and demonstrated good psychometric properties [36]. The main limitation of our study is its transversal conception which does not allow us to conclude on the causal relationship of the association. An inverse causality between dispositional optimism and dietary intake is likely to exist, as previously suggested [58, 59]. In our analysis, depressive symptom was assessed from a questionnaire collected in between 2017 and 2018 while optimism were collected in 2016. So there could be a problem of temporality. Caution is also needed when generalizing our results since the NutriNet-Santé study is a long-term nutrition-focused cohort and participants are recruited on a voluntary basis. Consequently, our subjects are likely to have high health awareness and a higher interest in nutrition compared to the French population. However, a low magnitude of differences in food intakes (apart from fruits and vegetables) was observed between the NutriNet-Santé study and a representative sample of the French population [73]. In regards to snacking measure, the nutritional quality of the snacks was not assessed in the present study, although previous data of the NutriNet-Santé cohort suggested a lower nutrient density and higher energy density of snacks compared with main meals [32]. Finally, optimism trait is regarded as a stable personality characteristic over extended periods [29]. However, it relies on the subject’s self-perception and understanding of the questionnaire.
Conclusions
Our findings showed that dispositional optimism was associated with a higher overall diet quality, and less snacking practices. It was also associated with consumption of specific unhealthy foods and alcohol beverages. Our results therefore suggest that optimists tend to have a healthier diet overall but with larger intakes of food and beverages typically consumed at social eating occasions. Replication of these findings, particularly by longitudinal and experimental studies are needed. Since optimism can be enhanced, programs targeting optimism may provide effective strategies for helping influencing dietary behaviors toward better food choices.
Availability of data and materials
Data of this study are protected under the protection of health data regulation set by the ‘Commission Nationale de l’Informatique et des Libertés (CNIL). The data are available upon request to Nathalie Pecollo (n.pecollo@eren.smbh.univ-paris13.fr) for review by the steering committee of the NutriNet-Santé study.
Abbreviations
- CES-D:
-
Center for Epidemiologic Studies Depression scale
- CNIL:
-
Commission Nationale de l’Informatique et des Libertés
- CU:
-
Consumption Unit
- IRB:
-
Institute for Health and Medical Research
- LOT-R:
-
Life Orientation Test Revised
- mPNNS-GS:
-
modified Programme National Nutrition Santé - Guideline Score
- OECD:
-
Organization for Economic Cooperation and Development
References
James S, Abate D, Abate K. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Lond Engl. 2019;393:1958–72.
World Health Organization. Diet, nutrition and the prevention of chronic diseases. Geneva: WHO; 2003. Report No.: 916
Stewart BW, Wild CP. World Cancer report. International Agency for Research on Cancer: Lyon; 2014.
Getz GS, Reardon CA. Nutrition and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2007;27:2499–506.
Stok FM, Hoffmann S, Volkert D, Boeing H, Ensenauer R, Stelmach-Mardas M, et al. The DONE framework: Creation, evaluation, and updating of an interdisciplinary, dynamic framework 2.0 of determinants of nutrition and eating. PLoS ONE. 2017;12 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5289713/. Cited 29 Jan 2019.
Elfhag K, Tholin S, Rasmussen F. Consumption of fruit, vegetables, sweets and soft drinks are associated with psychological dimensions of eating behaviour in parents and their 12-year-old children. Public Health Nutr. 2008;11:914–23.
Camilleri GM, Méjean C, Kesse-Guyot E, Andreeva VA, Bellisle F, Hercberg S, et al. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J Nutr. 2014;144:1264–73.
Johnson F, Pratt M, Wardle J. Dietary restraint and self-regulation in eating behavior. Int J Obes 2005. 2012;36:665–74.
de Lauzon B, Romon M, Deschamps V, Lafay L, Borys J-M, Karlsson J, et al. The three-factor eating questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134:2372–80.
Jasinska AJ, Yasuda M, Burant CF, Gregor N, Khatri S, Sweet M, et al. Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite. 2012;59:738–47.
Bénard M, Bellisle F, Kesse-Guyot E, Julia C, Andreeva VA, Etilé F, et al. Impulsivity is associated with food intake, snacking, and eating disorders in a general population. Am J Clin Nutr. 2019;109:117–26.
Van Dyke N, Drinkwater EJ. Relationships between intuitive eating and health indicators: literature review. Public Health Nutr. 2014;17:1757–66.
Abilés V, Rodríguez-Ruiz S, Abilés J, Mellado C, García A, Pérez de la Cruz A, et al. Psychological characteristics of morbidly obese candidates for bariatric surgery. Obes Surg. 2010;20:161–7.
Linley PA, Joseph S, Harrington S, Wood AM. Positive psychology: past, present, and (possible) future. J Posit Psychol. 2006;1:3–16.
Seligman ME, Csikszentmihalyi M. Positive psychology. An introduction. Am Psychol. 2000;55:5–14.
Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. 1994;67:1063–78.
Malouff JM, Schutte NS. Can psychological interventions increase optimism? A meta-analysis. J Posit Psychol. 2017;12:594–604.
Kim ES, Park N, Peterson C. Dispositional optimism protects older adults from stroke: the health and retirement study. Stroke. 2011;42:2855–9.
Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s health initiative. Circulation. 2009;120:656–62.
Kim ES, Hagan KA, Grodstein F, DeMeo DL, De Vivo I, Kubzansky LD. Optimism and cause-specific mortality: a prospective cohort study. Am J Epidemiol. 2017;185:21–9.
James P, Kim ES, Kubzansky LD, Zevon ES, Trudel-Fitzgerald C, Grodstein F. Optimism and healthy aging in women. Am J Prev Med. 2019;56:116–24.
Carver CS, Scheier MF. Dispositional Optimism. Trends Cogn Sci. 2014;18:293–9.
Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL, Kubzansky LD. Is optimism associated with healthier cardiovascular-related behavior? Meta-analyses of 3 health behaviors. Circ Res. 2018;122:1119–34.
Hingle MD, Wertheim BC, Tindle HA, Tinker L, Seguin RA, Rosal MC, et al. Optimism and diet quality in the Women’s health initiative. J Acad Nutr Diet. 2014;114:1036–45.
Serlachius A, Pulkki-Råback L, Elovainio M, Hintsanen M, Mikkilä V, Laitinen TT, et al. Is dispositional optimism or dispositional pessimism predictive of ideal cardiovascular health? The Young Finns Study. Psychol Health. 2015;30:1221–39.
Ronaldson A, Molloy GJ, Wikman A, Poole L, Kaski J-C, Steptoe A. Optimism and recovery after acute coronary syndrome: a clinical cohort study. Psychosom Med. 2015;77:311–8.
Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45:169–76.
Gacek M. Individual differences as predictors of dietary patterns among menopausal women with arterial hypertension. Prz Menopauzalny Menopause Rev. 2014;13:101–8.
Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30:879–89.
Weinstein ND. Optimistic biases about personal risks. Science. 1989;246:1232–3.
Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006;11:71–84.
Hassen WS, Castetbon K, Tichit C, Péneau S, Nechba A, Ducrot P, et al. Energy, nutrient and food content of snacks in French adults. Nutr J. 2018;17:33 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5828417/. Cited 31 Jul 2018.
Hartmann C, Siegrist M, van der Horst K. Snack frequency: associations with healthy and unhealthy food choices. Public Health Nutr. 2013;16:1487–96.
Murakami K, Livingstone MBE. Eating frequency is positively associated with overweight and central obesity in U.S. adults. J Nutr. 2015;145:2715–24.
Hercberg S, Castetbon K, Czernichow S, Malon A, Mejean C, Kesse E, et al. The Nutrinet-Santé study: a web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health. 2010;10:242.
Trottier C, Mageau G, Trudel P, Halliwell WR. Validation de la version canadienne-française du life orientation test-revised. [validation of the Canadian-French version of life orientation test-revised.]. Can J Behav Sci Rev Can Sci Comport. 2008;40:238–43.
Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 1985;4:219–47.
Segerstrom SC, Evans DR, Eisenlohr-Moul TA. Optimism and pessimism dimensions in the life orientation test-revised: method and meaning. J Res Personal. 2011;45:126–9.
Ryff CD, Singer B. What to do about positive and negative items in studies of psychological well-being and ill-being? Psychother Psychosom. 2007;76:61–2.
Touvier M, Kesse-Guyot E, Méjean C, Pollet C, Malon A, Castetbon K, et al. Comparison between an interactive web-based self-administered 24 h dietary record and an interview by a dietitian for large-scale epidemiological studies. Br J Nutr. 2011;105:1055–64.
Le Moullec N, Deheeger M, Preziosi P, Monteiro P, Valeix P, Rolland-Cachera MF, et al. Validation of the photo manual used for the collection of dietary data in the SU. VI. MAX. study. Cah Nutr Diet. 1996;31:158–64.
Nutrinet-Santé E. Table de composition des aliments de l’étude Nutrinet-Santé. Paris: Economica; 2013.
Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes. 2000;24:1119.
Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1984;39:5–41.
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr. 1991;45:569–81.
Lassale C, Castetbon K, Laporte F, Camilleri GM, Deschamps V, Vernay M, et al. Validation of a web-based, self-administered, non-consecutive-day dietary record tool against urinary biomarkers. Br J Nutr. 2015;113:953–62.
Lassale C, Castetbon K, Laporte F, Deschamps V, Vernay M, Camilleri GM, et al. Correlations between Fruit, Vegetables, Fish, Vitamins, and Fatty Acids Estimated by Web-Based Nonconsecutive Dietary Records and Respective Biomarkers of Nutritional Status. J Acad Nutr Diet. 2016;116:427–438.e5.
Estaquio C, Kesse-Guyot E, Deschamps V, Bertrais S, Dauchet L, Galan P, et al. Adherence to the French Programme National Nutrition Sante Guideline Score is associated with better nutrient intake and nutritional status. J Am Diet Assoc. 2009;109:1031–41.
Assmann KE, Andreeva VA, Camilleri GM, Verger EO, Jeandel C, Hercberg S, et al. Dietary scores at midlife and healthy ageing in a French prospective cohort. Br J Nutr. 2016;116:666–76.
Vergnaud A-C, Touvier M, Méjean C, Kesse-Guyot E, Pollet C, Malon A, et al. Agreement between web-based and paper versions of a socio-demographic questionnaire in the NutriNet-Santé study. Int J Public Health. 2011;56:407–17.
INSEE. INSEE (Institut national de la statistique et des études économiques) [National Institute of Statistics and Economic Studies]. Unités de consommation [consumption units]. Available from: http://www.insee.fr/en/methodes/default.asp?page=definitions/unite-consommation.htm. Accessed 23 Aug 2018.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Touvier M, Méjean C, Kesse-Guyot E, Pollet C, Malon A, Castetbon K, et al. Comparison between web-based and paper versions of a self-administered anthropometric questionnaire. Eur J Epidemiol. 2010;25:287–96.
Lassale C, Péneau S, Touvier M, Julia C, Galan P, Hercberg S, et al. Validity of web-based self-reported weight and height: results of the Nutrinet-Santé study. J Med Internet Res. 2013;15:e152.
World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: OMS; 2000. p. 252. Report No.: 894. Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Fuhrer R, Rouillon F. La version française de l’échelle CES-D (Center for Epidemiologic Studies-Depression Scale). Description et traduction de l’échelle d’autoévaluation. [the French version of the CES-D (Center for Epidemiologic Studies-Depression Scale).]. Psychiatr Psychobiol. 1989;4:163–6.
Kargakou A, Sachlas A, Lyrakos G, Zyga S, Tsironi M, Rojas Gil AP. Does health perception, dietary habits and lifestyle effect optimism? A quantitative and qualitative study. Adv Exp Med Biol. 2017;988:49–61.
Ruiz-Cabello P, Soriano-Maldonado A, Delgado-Fernandez M, Alvarez-Gallardo IC, Segura-Jimenez V, Estevez-Lopez F, et al. Association of Dietary Habits with Psychosocial Outcomes in Women with Fibromyalgia: The al-Ándalus Project. J Acad Nutr Diet. 2017;117:422–432.e1.
Ducrot P, Méjean C, Bellisle F, Allès B, Hercberg S, Péneau S. Adherence to the French eating model is inversely associated with overweight and obesity: results from a large sample of French adults. Br J Nutr. 2018;120:231–9.
CSA Research. CSA - Les Français et L’apéritif. csa.eu. 2018. Available from: https://www.csa.eu/fr/survey/les-français-et-l-aperitif. Cited 16 Aug 2018.
Opinionway. Les Français et l’apéritif idéal. 2017. Available from: https://www.opinion-way.com/fr/sondage-d-opinion/sondages-publies/search-result.html?filter_search=ap%C3%A9ritif&layout=table&show_category=0. Cited 22 Aug 2018.
Srivastava S, McGonigal KM, Richards JM, Butler EA, Gross JJ. Optimism in close relationships: how seeing things in a positive light makes them so. J Pers Soc Psychol. 2006;91:143–53.
Brissette I, Scheier MF, Carver CS. The role of optimism in social network development, coping, and psychological adjustment during a life transition. J Pers Soc Psychol. 2002;82:102–11.
Elstgeest LEM, Visser M, Penninx BWJH, Colpo M, Bandinelli S, Brouwer IA. Bidirectional associations between food groups and depressive symptoms: longitudinal findings from the Invecchiare in chianti (InCHIANTI) study. Br J Nutr. 2019;121:439–50.
Wallis DJ, Hetherington MM. Emotions and eating. Self-reported and experimentally induced changes in food intake under stress. Appetite. 2009;52:355–62.
Fanelli Kuczmarski M, Cotugna N, Pohlig RT, Beydoun MA, Adams EL, Evans MK, et al. Snacking and diet quality are associated with the coping strategies used by a socioeconomically diverse urban cohort of African-American and white adults. J Acad Nutr Diet. 2017;117:1355–65.
Giltay EJ, Zitman FG, Kromhout D. Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: the Zutphen elderly study. J Affect Disord. 2006;91:45–52.
Nes LS, Segerstrom SC. Dispositional optimism and coping: a meta-analytic review. Soc Psychol Rev. 2006;10:235–51.
Van Strien T, Herman CP, Anschutz DJ, Engels RCME, de Weerth C. Moderation of distress-induced eating by emotional eating scores. Appetite. 2012;58:277–84.
Oliver G, Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62:853–65.
Brussaard JH, Löwik MRH, Steingrímsdóttir L, Møller A, Kearney J, De Henauw S, et al. A European food consumption survey method--conclusions and recommendations. Eur J Clin Nutr. 2002;56(Suppl 2):S89–94.
Andreeva VA, Deschamps V, Salanave B, Castetbon K, Verdot C, Kesse-Guyot E, et al. Comparison of dietary intakes between a large online cohort study (etude NutriNet-Santé) and a nationally representative cross-sectional study (etude Nationale nutrition Santé) in France: addressing the issue of generalizability in E-epidemiology. Am J Epidemiol. 2016;184:660–9.
Acknowledgments
The authors thank Younes Esseddik, Thi Hong Van Duong, Frédéric Coffinieres, Régis Gatibelza, Maithyly Sivapalan and Paul Flanzy (computer scientists); Nathalie Arnault, Véronique Gourlet, Dr. Fabien Szabo, Julien Allegre and Laurent Bourhis (data-manager/biostatisticians); Cédric Agaesse and Anne-Elise Dussolier (dieticians) for their technical contribution to the NutriNet-Santé study and Nathalie Druesne-Pecollo (operational coordination). We thank all the volunteers of the NutriNet-Santé cohort.
Funding
The NutriNet-Santé Study is supported by the French Ministry of Health (DGS), the Santé Publique France agency, the French National Institute for Health and Medical Research (INSERM), the French National Institute for Agricultural Research (INRA), the National Conservatory for Arts and Crafts (CNAM), the Medical Research Foundation (FRM), and the University of Paris 13.
This research was part of the FOODPOL project, which was supported by the French National Institute for Agricultural Research (Institut National de la Recherche Agronomique) in the context of the 2013–2017 Metaprogramme “Diet impacts and determinants: Interactions and Transitions”.
Author information
Authors and Affiliations
Contributions
WA conducted the literature review and drafted the manuscript. WA, MR, and SP performed analyses. WA, MB, RS, EK-G, MR, MT, SH, CB and SP were involved in interpreting results and critically reviewed the manuscript. EK-G, MT, SH, and SP were responsible for developing the design and protocol of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NutriNet-Santé study is conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of the French Institute for Health and Medical Research (IRB Inserm no. 0000388FWA00005831) and by the National Commission on Informatics and Liberty (CNIL no. 908450 and no. 909216). Electronic informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Names for PubMed indexing: Ait-hadad, Bénard, Shankland, Kesse-Guyot, Robert, Touvier, Hercberg, Buscail, Péneau
Supplementary information
Additional file 1:
Figure S1. Participant flow chart from the NutriNet-Santé cohort study included in current analyses.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ait-hadad, W., Bénard, M., Shankland, R. et al. Optimism is associated with diet quality, food group consumption and snacking behavior in a general population. Nutr J 19, 6 (2020). https://doi.org/10.1186/s12937-020-0522-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-020-0522-7