Abstract
Background
Several types of insecticides, treating technologies and materials are available for long-lasting insecticide-treated nets (LLINs). The variations may result in different efficacies against mosquitoes and correspondingly infection risks for the Plasmodium falciparum malaria parasite. This cross-sectional study investigated whether infection risk varied among children who slept under different LLIN brands in rural villages of western Kenya.
Methods
Children sleeping under various types of LLINs were tested for P. falciparum infection using a diagnostic polymerase chain reaction (PCR) assay. Data were collected for other potential factors associated with infection risk: sleeping location (with bed/without bed), number of persons sharing the same net, dwelling wall material, gap of eaves (open/close), proportional hole index, socio-economic status, and density of indoor resting anophelines. Bed-net efficacy against the Anopheles gambiae susceptible strain was estimated using the WHO cone test and the tunnel test. The residual insecticide content on nets was measured.
Results
Seven LLIN brands were identified, and deltamethrin-based DawaPlus® 2.0 was the most popular (48%) followed by permethrin-based Olyset® Net (28%). The former LLIN was distributed in the area about six months before the present study was conducted, and the latter net was distributed at least three years before. Of 254 children analysed, P. falciparum PCR-positive prevalence was 58% for DawaPlus® 2.0 users and 38% for Olyset® users. The multiple regression analysis revealed that the difference was statistically significant (adjusted OR: 0.67, 95% credible interval: 0.45–0.97), whereas the confounders were not statistically important. Among randomly selected net samples, all DawaPlus® 2.0 (n = 20) and 95% of Olyset® (n = 19) passed either the cone test or the tunnel test.
Conclusions
Olyset® was more effective in reducing infection risk compared with DawaPlus® 2.0. Although the data from the present study were too limited to explain the mechanism clearly, the results suggest that the characteristics of the former brand are more suitable for the conditions, such as vector species composition, of the study area.
Similar content being viewed by others
Background
Long-lasting insecticide-treated nets (LLINs) are effective in reducing malaria morbidity and mortality [1,2,3] and are widely accepted as an important tool to control malaria parasite infection [4]. As of 2019, the World Health Organization (WHO) listed 20 LLIN brands for procurement by international agencies and countries [5]. The pyrethroid insecticides used for these LLINs are deltamethrin, alpha-cypermethrin, and permethrin [5]. The insecticides act differently against anopheline mosquitoes; for instance, a laboratory study showed that fabric treated with deltamethrin has better killing effects than one with permethrin; however, the latter shows stronger repellent effects [6,7,8]. Although both types of pyrethroids reduce human contact with anophelines by killing and repelling, the question remains which mode of action or insecticide is better for reducing infection risk. To counter anophelines resistant to pyrethroids and dichlorodiphenyltrichloroethane (DDT), five LLIN brands in the list are treated with piperonyl butoxide (PBO) in addition to the pyrethroids. A randomized control trial showed that LLINs treated with PBO and permethrin are more effective in reducing Plasmodium falciparum parasite infection than nets with insecticide only [9].
The difference in insecticide treating technology and LLIN materials may also affect their performance. One treating technology is called incorporation technology; specifically, an insecticide is incorporated into polyethylene-based fibres of the net [10], such as the Olyset® Net (Sumitomo Chemical, Tokyo, Japan). The insecticide migrates from the inside of the fibres to the surface so that the amount of the active content is maintained for several years. Coating is a second technology, in which the polyester-based multifilaments are coated with insecticide using a resin-based polymer [11] that serves as a reservoir for replacement of insecticide lost from the surface. Polyethylene and polyester are the two major materials used for LLINs. The difference in treatment technology and netting material may alter the durability of nets and the availability of insecticides on the fibre surfaces and, consequently, affect infection risks [12, 13].
A meta-analysis showed that among three different insecticides the differences in effectiveness on infection risk were not statistically significant [3]. A large population-based cross-sectional study using data from 21 countries across sub-Saharan Africa also found little variability on infection of children by LLIN brands [14]. However, when data were examined separately for each surveyed population, the effects of LLINs varied among LLIN brands for some populations [14, 15]. Local environmental conditions likely vary across large geographical malarial areas and may influence the performance of LLINs. Local vector species compositions and their insecticide resistance status can also contribute to the variability of LLIN performance [16,17,18,19,20].
Since a variety of LLIN brands are available, and the environmental conditions of target areas vary, an LLIN brand that is effective for a certain area might be less effective elsewhere, and, therefore, the selection of an appropriate LLIN brand may become important. More comparative studies of various LLIN brands in real-field conditions are needed to produce information to select the most suitable LLIN brand for a target area. This study investigated whether P. falciparum parasite infection risk varies among children who slept under different LLIN brands, along with various conditions in rural villages in a malaria hyperendemic area of western Kenya.
Methods
Study area and target population
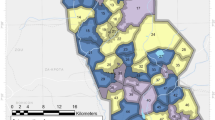
The study area was located on the western part of Gembe East Sub-location in Homabay County, Kenya (approximate area: 12 sq km; approximate midpoint: 0° 28′ 24.06″ S, 34° 19′ 16.82″ E) (Fig. 1). For scheduling and logistics, the area was divided into 12 sub-areas based on community centres, villages and political boundary. The rainfall pattern was binomial, with a long rainy season from March through May and a short rainy season from November to December. A typical household compound consists of multiple mud house structures with corrugated iron roofs that have open eaves [21,22,23]. Principal economic activities are small-scale fishing, farming and livestock [21,22,23].
In December 2017, the population of the area was estimated to be 3769 through a household survey; the initial target population was children 15 years old and younger. Of 2006 children registered, 1094 were excluded because the ceilings of their sleeping houses were screened with a LLIN material in a previous project, which may affect the risk of infection [24]. The number of remaining children was 912.
Informed consent
Prior to the survey, the field workers visited households that consisted of at least one eligible child and explained the details of the survey, including the goals, risks and benefits. Once written consent was obtained from household heads or caretakers of the children, they were informed of the dates and time of the survey. At the time of visit, geographical coordinates of house structures where the children slept were recorded using a handheld global positioning system (GPS) (Garmin, Olathe, KS, USA).
Field data collection
Because the data on P. falciparum parasite infection of children were provided from the field evaluation study for developing a rapid diagnostic device [25], this study followed the schedule of the evaluation study. Accordingly, the cross-sectional survey was conducted separately for 6 of the 12 sub-areas in December 2017 and for the remaining sub-areas in February 2018.
The field workers visited the households between 05:00 and 06:30, and directly observed bed net use and sleeping locations of the target children, because these variables may affect infection risk [21, 23, 26,27,28,29]. Sleeping location was categorized as ‘with bed’ or ‘without bed’. Cases of sleeping on the floor, sofa or mattress without a bed frame were considered as ‘without bed’. The field workers also recorded the number of persons sharing the same net with each target child. The children were divided to two groups based on the number of persons sharing a net, ‘children sharing with none or one person’ and ‘those sharing with two or more persons’. This is based on the WHO recommendation of ‘one net for every two persons’, and the protective effect of LLIN that is expected if the recommendation is followed [30].
Immediately after the direct observation, indoor-resting female anophelines were sampled in the rooms where children slept, using the pyrethrum spray catch method [31]. The area (sq m) of each room was estimated, measuring with a tape measure, and the density of female anophelines was calculated as the number of anophelines divided by the area of sleeping room. All mosquitoes were collected before the local government started the indoor residual spray programme prior to the long rainy season of 2018.
Since modern house structures may reduce the infection risk, the field workers recorded wall materials (mud/others) and the presence/absence of eave openings [29, 32]. Cement, brick and iron walls were included in ‘others’ for wall material, because those houses were uncommon in this study area. In addition, household heads were asked if they possessed various consumer goods, materials of household construction, toilet/water access, and livestock, for constructing a socio-economic status (SES) index using multiple correspondence analysis [33,34,35].
During the household survey, a finger-prick blood was sampled from children after their axillary temperature was measured. The blood sample was tested for P. falciparum infection with a rapid diagnostic test (RDT)(Paracheck® Pf-Rapid Test Malaria Device, ver.3, Orchid Biomedical Systems, Verna, Goa, India). A part of the blood sample was used for measuring haemoglobin concentration with a portable haemoglobin photometer (HemoCue AB, Angelholm, Sweden). Artemether-lumefantrine was given to each child following diagnosis by a clinician and the guideline issued by WHO [36]. Children with haemoglobin concentration below 11.0 g/dL were given iron supplementation. In the laboratory, the blood samples were examined to detect P. falciparum using a diagnostic polymerase chain reaction (PCR) assay [37].
At the end of the survey, the bed nets that the children used were collected and new nets provided. Brand names of the bed nets were identified, and the proportional hole index (PHI) was estimated for each net following the WHO guideline [38]. PHI of the roof and side was calculated separately because more mosquitoes enter the net from the roof holes compared to the side holes [39, 40].
Data were collected on paper forms. Data entry was performed by two persons and independently verified. When discrepancies or missing data were found, the field workers revisited the households to confirm the data.
Insecticidal activity of LLIN
Following the WHO guideline for the bioassay test and chemical analysis [41], 5 pieces of nettings (4 pieces from side panels and one piece from the roof panel, 25 cm × 25 cm) were cut from each of 20 randomly selected nets for each LLIN brand. In the laboratory the biological efficacy of the nets was evaluated in the WHO cone bioassay test using the susceptible Anopheles gambiae s.s. Kisumu strain. Batches of five, non-blood-fed, 2–5-days-old females were exposed to each piece of netting in WHO cones for 3 min, and then the mosquitoes were held for 24 h with a sugar solution. A total of 100 females were exposed to each netting (5 mosquitoes × 5 cones × 4 pieces). Knockdown rate and mortality rate were observed at 60 min and 24 h after exposure, respectively. The WHO tunnel test using the An. gambiae Kisumu strain was conducted for netting that did not pass the cone test to determine the blood-feeding inhibition rate and 24-h mortality. Residual insecticide content of Olyset® and DawaPlus® 2.0 was analysed based on the CIPAC method 331/LN/M and 333/LN/(M)/3, respectively.
Power calculation
A study in the Democratic Republic of Congo had 32% of P. falciparum PCR-positive prevalence (pfPR) for children under 5 years of age who slept under deltamethrin-based nets, while the pfPR was 42% for those slept under permethrin-based nets [15]. With a Type I error of 5% and a sample size of 254, the power to detect the difference between deltamethrin-users and permethrin-users was 64%. Since the epidemiological data of the children were provided from the diagnostic device field evaluation study [42], the present study proceeded despite the relatively low detection power.
Ethical consideration
This study was approved by the Ethics Committees of the Kenya Medical Research Institute (SSC No. 3168), and the Ethics Committees of the National Institute of Advanced Industrial Science and Technology (No. 2017-156).
Data analyses
Association of 10 covariates with bed net brands was assessed using the Chi-square test for binary and categorical variables, and the Wilcoxon rank-sum test or t-test for continuous variables [29]. The covariates were number of persons sharing a net, age, gender, sleeping location, PHI of the roof, PHI of the sides, SES, density of female anophelines in the room, material of wall, and eave gap. Simple logistic regression examined the impacts of bed net type and the 10 variables on pfPR of children.
A multiple logistic regression model of parasitaemia examined bed net type and the 10 confounding factors. Generalized variance inflation factor (GVIF) was used to assess collinearity among the covariates [43]. Since the survey was conducted on multiple dates during the two separate periods, the dates were considered as a random effect. When multiple target children shared the same net and sleeping room, those nets and rooms were also considered as potential random effects. Further sub-area was included as a potential random effect. Model selection based on the deviance information criteria (DIC) was used for testing whether each random effect was necessary. The variogram was used to assess the presence of spatial dependency in the residual for each analysis. DIC was also used to assess whether the spatial model was better than the non-spatial model. The spatial component was included in the Bayesian model using integrated nested Laplace approximation (R-INLA) with 95% credible intervals [44].
The residual active insecticide content was compared between net brands using a generalized liner mixed model (GLMM) with 95% confidence intervals. The original LLIN from which 5 sub-sample nettings were obtained was considered as a random factor in the model. Knockdown rate and mortality rate were examined using Chi-square test. R (version 3.5.2) was used for all data analyses [45].
Results
Target children and LLINs
Of 912 target children, 729 were available at the time of the survey, and 546 slept under a LLIN. The number of LLINs used was 307, and 7 different LLIN brands were identified. DawaPlus® 2.0 (Tana Netting, Dubai, UAE) was the most popular (48%) followed by Olyset® (28%). The rest were Yorkool® LN (4%; Tianjin Yorkool International Trading, Tianjin, China), DuraNet® (4%; Shobikaa Impex, Tamilnadu, India), PermaNet® 2.0 (2%; Vestergaard, Lausanne, Switzerland), Olyset®Plus (1%; Sumitomo Chemical, Tokyo, Japan), Netprotect®(0.3%; Bestnet A/S, Kolding, Denmark), and unidentified nets (12%). Because DawaPlus® 2.0 and Olyset® comprised 76% of all the LLINs, the following analyses focused on these two brands. The Ministry of Health of Kenya distributed DawaPlus® 2.0 through health facilities in the study area in June and July, 2017, and Nagasaki University distributed Olyset® in September and October 2014.
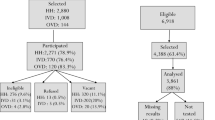
In December 2017, 356 children were directly observed for their sleeping conditions and tested for P. falciparum parasite infection (Fig. 2). Of these children, 139 were dropped because they did not use bed nets, or slept under nets other than Olyset® or DawaPlus® 2.0. Of 217 children remaining, 27 children shared the same room with other persons who did not use bed nets or slept under other types of nets, and 48 children shared the same room where at least one adult slept; the exclusion would minimize the influence of presence of a non-net user, other net types and adults. Adults may occupy a large space inside a net, and children might be squeezed towards the net, which may increase the risk of touching it or extending their limbs outside of it. On the other hand, parents tend to lay their small child (particularly a child under 2 years old) between their bodies in the net, which may provide protection. After removing 4 children without complete data, 138 children remained. In the same manner, 355 were dropped from 471 children who were available for the survey, and 116 children remained for the survey in February 2018. In total, a dataset of 254 children was used for the analyses.
Background information
The mean child age was 8.4 (SD = 3.5) years old, and the difference was not statistically significant between DawaPlus® 2.0 users and Olyset® users (Table 1). The differences in gender ratio and sleeping location were also not statistically significant between the two groups. The PHI on the side of Olyset® was significantly greater than that of DawaPlus® 2.0 while the difference in PHI on the roof was not significant. The proportion of children sharing the same net with two or more persons was significantly higher for DawaPlus® 2.0 users. The proportions of mud wall and open eaves were significantly higher for the rooms where DawaPlus® 2.0 users slept, and the SES of DawaPlus® 2.0 users was significantly lower. A total of 1365 anopheline mosquitoes were collected from 118 rooms where 254 target children slept. Although the mean density of anophelines in the rooms with Olyset® was almost half compared to those with DawaPlus® 2.0, the difference was not statistically significant.
Insecticidal activity
The mean residual insecticide content was 14.11 g/kg (SD = 3.31, n = 94) and 0.40 g/kg (SD = 0.29, n = 100) for Olyset® and DawaPlus® 2.0, respectively. When the contents were compared with the original contents (20.0 g/kg for Olyset®, and 2.66 g/kg for DawaPlus® 2.0), the residual rate was 70% and 15% for Olyset® and DawaPlus® 2.0, respectively. The residual rate was significantly higher for Olyset® (OR: 1.73, 95% confidence interval: 1.60–1.89, n = 194). Six Olyset® nettings were removed from the analysis because of measurement errors.
The knockdown rate after 60 min was 98 and 99% for Olyset® and DawaPlus® 2.0, respectively, and the difference was not statistically significant (OR = 0.98, \(\chi\) 2 = 0.18, P = 0.668, df = 1). The 24-h mortality was 52 and 92% for Olyset® and DawaPlus® 2.0, respectively, a statistically significant difference (OR: 0.56, \(\chi\) 2 = 129.81, P < 0.001, df = 1). The tunnel test was conducted for two Olyset® and one DawaPlus® 2.0 that did not pass the cone test. While one Olyset® did not pass the tunnel test, the others passed the test. In total, 18 of 19 Olyset® (95%) and all DawaPlus® 2.0 passed either the cone test or the tunnel test. Data from one Olyset® was removed because of measurement errors.
Plasmodium falciparum infection
The pfPR was 58% for DawaPlus® 2.0 users and 38% for Olyset® users (Fig. 1). The simple logistic regression analysis showed that the 95% credible interval did not contain 0 for the net brands (Additional file 3: Fig. S3 and Table 2). The 95% credible intervals for the other variables contain 0. All analyses included the spatial component because of presence of spatial dependency (Additional file 1: Fig. S1).
The multiple logistic regression analysis confirmed the results from the simple regression analysis (Table 2). When Olyset® was used, the risk of infection became lower, and the 95% credible interval did not contain 0 (Additional file 4: Fig. S4). The GVIFs for the all covariates were less than 2 so they were included in the analysis. Among the potential random factors, date of survey and bed net were dropped from all analyses after model selection using deviance information criteria (DIC). Sub-area and sleeping room remained as random effects. All analyses considered spatial dependency, because the spatial models had slightly better sample variograms (Additional file 2: Fig. S2).
Discussion
This study demonstrated that the pfPR of children differed between users of Olyset® and DawaPlus® 2.0. The odds ratio indicated that use of Olyset® for a child reduced by 33% the likelihood of being infected (Table 2). The study also found differences in some variables between two groups (Table 1). The households of Olyset® users had significantly higher SES, and a decrease of infection risk is often associated with an increase of SES [46]. Households with low income cannot easily afford extra protection such as insecticide spray and drugs. Moreover, parents of households with high SES tend to have a better health knowledge, which may also lower the risk [47, 48]. It is plausible that households with high SES have better house construction, with glass or screened windows and closed eaves to prevent mosquitoes from entering [49]. While most of the houses in the study area were constructed with a mud wall and corrugated iron roofs that have open eaves, the higher proportion of the rooms with Olyset® had closed eaves and non-mud walls, such as concrete. Although the difference was not statistically significant, the density of anophelines in the rooms of Olyset® users was nearly 50% less than in those of DawaPlus® 2.0 users, suggesting that Olyset® users might have lower infection risks because of higher SES (Additional file 3: Fig. S3, Additional file 4: Fig. S4).
In addition to freely distributed LLINs, households with higher SES might be able to buy extra nets. Although the WHO guideline suggests ‘one net for every two people’ to achieve universal coverage, the goal has not been reached in several areas [50], where one net is often shared by more than two persons. The number of people sharing a net is significantly higher among DawaPlus® 2.0 users compared to Olyset® users. A recent study confirmed that the risk increases with an increase in the number of people sharing one LLIN, because the condition may increase the chance of their body being exposed outside the net [30].
As Olyset® in the study area had been used by residents longer than DawaPlus® 2.0, the condition of the former net was worse. The PHI on the sides of Olyset® was significantly higher. Although the difference was not statistically significant, the Olyset® also had a higher PHI on the roof. As mosquitoes may enter through holes, the infection risk is expected to be higher for children sleeping under the old nets. However, the results from the present study did not agree with this notion. Even though the effects of all these confounding factors, including spatial dependency, were controlled in the multiple regression model, the difference in pfPR between Olyset® users and DawaPlus® 2.0 users still remained.
The difference in pfPR of children sleeping under these LLIN brands may be explained by the differences between the insecticides. Permethrin is incorporated in the fibres of Olyset® while DawaPlus® 2.0 is treated with deltamethrin on the filament surface. A laboratory experiment showed that An. gambiae reduced landing attempts on Olyset® and increased frequencies of flight after the first contact with the net, while landing attempts on the net treated with deltamethrin were sustained longer [7, 51]. A possible effect of disengagement behaviour associated with permethrin is loss of the ability to sense host cues, which is also known in other insects, such as Glossina austeni [52]. Because of the greater repellent effect of permethrin, Olyset® may reduce the number of anophelines by decreasing the attraction cues of the room [53, 54]. The lower density of anophelines associated with Olyset® found in the present study agrees with this notion although the lower density cannot be explained by the data from the spray catch method only.
The disengagement associated with permethrin suggests decreased interactions between mosquitoes and humans [7, 55]. This deterrence effect should be beneficial for children sleeping with bed nets having holes [54, 56], and multiple children sharing one net [30]. Mosquitoes exposed to permethrin will not seek a blood meal even under these conditions because of a loss of the ability to sense host cues. Similarly, the deterrence will be beneficial for persons who are not under an LLIN [56, 57]. Further, this effect may reduce early-hour biting activity in the room or even outdoor biting activity near a house with an Olyset® [8]. Although loss of the response to host cues may be restored within 24 h [7], as long as a mosquito repeatedly visits the net with permethrin, the effect can be sustained. Permethrin is continuously provided to the surface of the fibre from the inside via osmotic pressure [10]. The present study confirmed that Olyset® used for at least three years had sustained the efficacy.
It is known that mosquito disengagement from Olyset® reduces lethality [7, 51]. The low 24-h mortality of Olyset® found in the bioassay of the present study is also likely due to disengagement, but it is not due to net age because enough insecticide content was maintained on the surface. It has been suggested that the poor killing effect delays the development of resistance against the insecticide [16, 54, 56]. Three main vector species in western Kenya have developed resistance to pyrethroid insecticides; namely, An. gambiae sensu stricto (s.s.), Anopheles arabiensis and Anopheles funestus s.s. Specifically, An. gambiae s.s. has developed resistance associated with a point mutation (knockdown resistance mutation: kdr) in the voltage-gated sodium channel (L1014S), and the other two species have developed metabolic resistance related to one or more detoxification enzymes, such as cytochrome P450s [16, 17, 58]. Although the field-collected adults of the three species from the present study area show strong resistance to both deltamethrin and permethrin in the susceptibility test using the WHO tube test, permethrin still shows a strong repellent effect against An. arabiensis and An. funestus s.s.[8]. On the other hand, permethrin has a less repellent effect against An. gambiae with kdr [6, 8]. As An. arabiensis and An. funestus dominate the present study area after the disappearance of An. gambiae [59], the Olyset® might have become more effective. In contrast, studies in Democratic Republic of Congo as well as Benin demonstrated that use of deltamethrin-based LLINs is associated with lower pfPR than use of permethrin-based LLINs [14, 15]. This conflicting result may be due to great abundance of An. gambiae or Anopheles coluzzi with kdr in these countries [60,61,62,63]. Although the present study excluded the potential effects of other LLIN brands in the same room, the study in Democratic Republic of Congo apparently did not exclude them because of a large-scale cross-sectional study.
This study collected data on the types and locations of LLINs. Although residents were not asked where they preferred to hang what kinds of nets, there were some important commonalities. Olyset® were more common around beds, where nets were hung in a semi-permanent fashion. DawaPlus® 2.0 were more common in community living areas, where nets must be hung, taken down and stored to make the space available for other activities during the daytime [26]. The Olyset® fabric is hard and difficult to fold to a compact size for storage possibly making it a preferred type of net in sleeping areas. The DawaPlus® 2.0, on the other hand, are softer and easier to fold on a routine basis which could explain why residents prefer to use it in living rooms and gathering spaces. This practice can explain not only the positive association of Olyset® users with sleeping in a bed, but also their negative association with pfPR. Unremoved Olyset® may strengthen the deterrence effects increasing the chance of mosquito contact with it even though no one is under the net, because human odour remaining on bedding would be still strong enough to attract mosquitoes to the net. Especially, the deterrence effects may reduce mosquito bites of residents outside of the nets in the early morning and evening. The early-hour biting is characteristic of An. arabiensis and An. funestus in this study area [64]. Moreover, simply using a net in the bed may provide more protective effects compared to sleeping on the floor, because the net spreads well with the bed frame, and its bottom end is tucked in firmly under the mattress [23].
Limitations
Data from the present study were insufficient for explaining the lower pfPR associated with Olyset® use. Data collection was limited to the low transmission season to match the schedule of the previous study. Since vector abundance and species composition may vary seasonally, the effects of LLINs might change during the high transmission season. As some residents alter their sleeping locations and bed nets, a cross-sectional study will have some limitations. In particular, the factors associated with bed net use might affect the results because the skewed sample size of Olyset® users was less than half of DawaPlus® 2.0 users. More studies under different locations and conditions are needed to confirm the repellent effects of LLINs with permethrin on P. falciparum parasite infection in the field.
Conclusions
The present study showed the possibility that P. falciparum parasite infection varies depending on the LLIN brand used. The results from the present study suggest that a selection of LLIN brand requires more care to maximize their effectiveness. The selection will be based on the environmental condition of each target village or geographical area. In particular, vector species composition and their insecticide resistant status should be considered for the selection.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DDT:
-
Dichlorodiphenyltrichloroethane
- DIC:
-
Deviance information criteria
- GLMM:
-
Generalized liner mixed model
- GPS:
-
Global positioning system
- GVIF:
-
Generalized variance inflation factor
- IRS:
-
Indoor residual
- kdr :
-
Knockdown resistance mutation
- LLIN:
-
Long-lasting insecticide-treated net
- PBO:
-
Piperonyl butoxide
- PCR:
-
Polymerase chain reaction
- pfPR:
-
P. falciparum PCR-positive prevalence
- PHI:
-
Proportional hole index
- SES:
-
Socioeconomic status
- RDT:
-
Rapid diagnostic test
- R-INLA:
-
Integrated Nested Laplace Approximation
- WHO:
-
World Health Organization
References
Eisele TP, Larsen D, Steketee RW. Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. Int J Epidemiol. 2010;39:i88–101.
Pryce J, Richardson M, Lengeler C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst Rev. 2018;11:CD00363.
Yang G-G, Kim D, Pham A, Paul CJ. A meta-regression analysis of the effectiveness of mosquito nets for malaria control: the value of long-lasting insecticide nets. Int J Environ Res Public Health. 2018;15:546.
WHO. Implications of insecticide resistance for malaria vector control. Geneva: World Health Organization; 2016 [updated 13 January 2020]. https://www.who.int/malaria/publications/atoz/insecticide-resistance-implications/en/. Accessed 13 Jan 2020.
WHO. Prequalified Lists. Geneva: World Health Organization; 2019. https://www.who.int/pq-vector-control/prequalified-lists/en/. Accessed 13 Jan 2020.
Chandre F, Darriet F, Duchon S, Finot L, Manguin S, Carnevale P, et al. Modifications of pyrethroid effects associated with kdr mutation in Anopheles gambiae. Med Vet Entomol. 2000;14:81–8.
Siegert PY, Walker E, Miller JR. Differential behavioral responses of Anopheles gambiae (Diptera: Culicidae) modulate mortality caused by pyrethroid-treated bednets. J Econ Entomol. 2009;102:2061–71.
Kawada H, Ohashi K, Dida GO, Sonye G, Njenga SM, Mwandawiro C, et al. Insecticidal and repellent activities of pyrethroids to the three major pyrethroid-resistant malaria vectors in western Kenya. Parasit Vectors. 2014a;7:208.
Protopopoff N, Mosha JF, Lukole E, Charlwood JD, Wright A, Mwalimu CD, et al. Effectiveness of a long-lasting piperonyl butoxide-treated insecticidal net and indoor residual spray interventions, separately and together, against malaria transmitted by pyrethroid-resistant mosquitoes: a cluster, randomised controlled, two-by-two factorial design trial. Lancet. 2018;391:1577–88.
Ito T, Okuno T. Development of Olyset (R) net' as a Tool for Malaria Control. Sumitomo Kagaku Tokushugo(Sumitomo Chemical Review). 2006;4–11.
Kilian A, Byamukama W, Pigeon O, Atieli F, Duchon S, Phan C. Long-term field performance of a polyester-based long-lasting insecticidal mosquito net in rural Uganda. Malar J. 2008;7:49.
Graham K, Kayedi MH, Maxwell C, Kaur H, Rehman H, Malima R, et al. Multi-country field trials comparing wash-resistance of PermaNetTM and conventional insecticide-treated nets against anopheline and culicine mosquitoes. Med Vet Entomol. 2005;19:72–83.
Hakizimana E, Cyubahiro B, Rukundo A, Kabayiza A, Mutabazi A, Beach R, et al. Monitoring long-lasting insecticidal net (LLIN) durability to validate net serviceable life assumptions, in Rwanda. Malar J. 2014;13:344.
Janko MM, Churcher TS, Emch ME, Meshnick SR. Strengthening long-lasting insecticidal nets effectiveness monitoring using retrospective analysis of cross-sectional, population-based surveys across sub-Saharan Africa. Sci Rep. 2018;8:17110.
Levitz L, Janko M, Mwandagalirwa K, Thwai KL, Likwela JL, Tshefu AK, et al. Effect of individual and community-level bed net usage on malaria prevalence among under-fives in the Democratic Republic of Congo. Malar J. 2018;17:39.
Kawada H, Dida GO, Ohashi K, Komagata O, Kasai S, Tomita T, et al. Multimodal Pyrethroid Resistance in Malaria Vectors, Anopheles gambiae s.s., Anopheles arabiensis, and Anopheles funestus s.s. in Western Kenya. PLoS ONE. 2011;6:22574.
Kawada H, Futami K, Komagata O, Kasai S, Tomita T, Sonye G, et al. Distribution of a Knockdown Resistance Mutation (L1014S) in Anopheles gambiae s.s. and Anopheles arabiensis in Western and Southern Kenya. PLoS ONE. 2011;6:24323.
Churcher TS, Lissenden N, Griffin JT, Worrall E, Ranson H. The impact of pyrethroid resistance on the efficacy and effectiveness of bednets for malaria control in Africa. Elife. 2016;5:e16090.
Ondeto BM, Nyundo C, Kamau L, Muriu SM, Mwangangi JM, Njagi K, et al. Current status of insecticide resistance among malaria vectors in Kenya. Parasit Vectors. 2017;10:429.
Hancock PA, Wiebe A, Gleave KA, Bhatt S, Cameron E, Trett A, et al. Associated patterns of insecticide resistance in field populations of malaria vectors across Africa. Proc Natl Acad Sci USA. 2018;115:5938.
Iwashita H, Dida G, Futami K, Sonye G, Kaneko S, Horio M, et al. Sleeping arrangement and house structure affect bed net use in villages along Lake Victoria. Malar J. 2010;9:176.
Larson PS, Minakawa N, Dida GO, Njenga SM, Ionides EL, Wilson ML. Insecticide-treated net use before and after mass distribution in a fishing community along Lake Victoria, Kenya: successes and unavoidable pitfalls. Malar J. 2014;13:466.
Minakawa N, Kongere JO, Dida GO, Ikeda E, Hu J, Minagawa K, et al. Sleeping on the floor decreases insecticide treated bed net use and increases risk of malaria in children under 5 years of age in Mbita District. Kenya Parasitol. 2015;142:1516–22.
Kawada H, Dida GO, Ohashi K, Sonye G, Njenga SM, Mwandawiro C, et al. Preliminary evaluation of insecticide-impregnated ceiling nets with coarse mesh size as a barrier against the invasion of malaria vectors. Jpn J Infect Dis. 2012;65:243–6.
Yatsushiro S, Yamamoto T, Yamamura S, Abe K, Obana E, Nogami T, et al. Application of a cell microarray chip system for accurate, highly sensitive, and rapid diagnosis for malaria in Uganda. Sci Rep. 2016;6:30136.
Baume CA, Reithinger R, Woldehanna S. Factors associated with use and non-use of mosquito nets owned in Oromia and Amhara Regional States Ethiopia. Malar J. 2009;8:264.
Noor AM, Kirui VC, Brooker SJ, Snow RW. The use of insecticide treated nets by age: implications for universal coverage in Africa. BMC Public Health. 2009;9:369.
Eisele TP, Miller JM, Moonga HB, Hamainza B, Hutchinson P, Keating J. Malaria infection and anemia prevalence in Zambia’s Luangwa District: an area of near-universal insecticide-treated mosquito net coverage. Am J Trop Med Hyg. 2011;84:152–7.
Minta AA, Landman KZ, Mwandama DA, Shah MP, Eng JLV, Sutcliffe JF, et al. The effect of holes in long-lasting insecticidal nets on malaria in Malawi: results from a case–control study. Malar J. 2017;16:394.
Tamari N, Minakawa N, Sonye GO, Awuor B, Kongere JO, Munga S, et al. Antimalarial bednet protection of children disappears when shared by three or more people in a high transmission setting of western Kenya. Parasitology. 2019;146:363–71.
Silver JB. Mosquito ecology field sampling methods. 3rd ed. edn. Dordrecht: Springer; 2008.
Tusting LS, Ippolito MM, Willey BA, Kleinschmidt I, Dorsey G, Gosling RD, et al. The evidence for improving housing to reduce malaria: a systematic review and meta-analysis. Malar J. 2015;14:209.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32.
Traissac P, Martin-Prevel Y. Alternatives to principal components analysis to derive asset-based indices to measure socio-economic position in low- and middle-income countries: the case for multiple correspondence analysis. Int J Epidemiol. 2012;41:1207–8.
Wanyua S, Ndemwa M, Goto K, Tanaka J, K’Opiyo J, Okumu S, et al. Profile: the Mbita health and demographic surveillance system. Int J Epidemiol. 2014;42:1678–85.
WHO. Guidelines for the treatment of malaria. Geneva: World Health Organization; 2015.
Johnston SP, Pieniazek NJ, Xayavong MV, Slemenda SB, Wilkins PP, da Silva AJ. PCR as a confirmatory technique for laboratory diagnosis of malaria. J Clin Microbiol. 2006;44:1087–9.
WHO. Guidelines for monitoring the durability of long-lasting insecticidal mosquito nets under operational conditions. Geneva: World Health Organization; 2011.
Lynd A, McCall PJ. Clustering of host-seeking activity of Anopheles gambiae mosquitoes at the top surface of a human-baited bed net. Malar J. 2013;12:267.
Sutcliffe JF, Yin S. Behavioural responses of females of two anopheline mosquito species to human-occupied, insecticide-treated and untreated bed nets. Malar J. 2014;13:294.
WHO. Guidelines for laboratory and field-testing of long-lasting insecticidal nets. Geneva: World Health Organization; 2013.
Yamamoto T, Hashimoto M, Nagatomi K, Nogami T, Sofue Y, Hayashi T, et al. Development of a quantitative, portable, and automated fluorescent blue-ray device-based malaria diagnostic equipment with an on-disc SiO2 nanofiber filter. Sci Rep. 2020;10:1–12.
Zuur AF, Ieno EN, Elphick CS. A protocol for data exploration to avoid common statistical problems. Methods Ecol Evol. 2010;1:3–14.
Zuur AF, Ieno EN, Saveliev AA. Beginner’s Guide to Spatial, Temporal and Spatial-Temporal Ecological Data Analysis with R-INLA. Newburgh: Highland Statistics; 2017.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018.
Degarege A, Fennie K, Degarege D, Chennupati S, Madhivanan P. Improving socioeconomic status may reduce the burden of malaria in sub Saharan Africa: A systematic review and meta-analysis. PLoS ONE. 2019;14:e0211205.
Dike N, Onwujekwe O, Ojukwu J, Ikeme A, Uzochukwu B, Shu E. Influence of education and knowledge on perceptions and practices to control malaria in Southeast Nigeria. Soc Sci Med. 2006;63:103–6.
Clouston SAP, Yukich J, Anglewicz P. Social inequalities in malaria knowledge, prevention and prevalence among children under 5 years old and women aged 15–49 in Madagascar. Malar J. 2015;14:499.
Mburu MM, Juurlink M, Spitzen J, Moraga P, Hiscox A, Mzilahowa T, et al. Impact of partially and fully closed eaves on house entry rates by mosquitoes. Parasit Vectors. 2018;11:383.
WHO. World malaria report 2019. Geneva: World Health Organization; 2019.
Hougard JM, Duchon S, Darriet F, Zaim M, Rogier C, Guillet P. Comparative performances, under laboratory conditions, of seven pyrethroid insecticides used for impregnation of mosquito nets. Bull World Health Organ. 2003;81:324–33.
Chadd EM, Brady J. sublethal insecticide effects on the probing responsiveness of tsetse flies and blowflies. Physiol Entomol. 1982;7:133–41.
Lindsay SW, Adiamah JH, Miller JE, Armstrong JR. Pyrethroid-treated bednet effects on mosquitoes of the Anopheles gambiae complex in The Gambia. Med Vet Entomol. 1991;5:477–83.
Mosha FW, Lyimo IN, Oxborough RM, Matowo J, Malima R, Feston E, et al. Comparative efficacies of permethrin-, deltamethrin-and α-cypermethrin-treated nets, against Anopheles arabiensis and Culex quinquefasciatus in northern Tanzania. Ann Trop Med Parasitol. 2008;102:367–76.
Miller JR, Siegert PY, Amimo FA, Walker ED. Designation of chemicals in terms of the locomotor responses they elicit from insects: an update of Dethier, et al. (1960). J Econ Entomol. 2009;102:2056–206.
Miller JE, Lindsay SW, Armstrong JR. Experimental hut trials of bednets impregnated with synthetic pyrethroid or organophosphate insecticide for mosquito control in The Gambia. Med Vet Entomol. 1991;5:465–76.
Spitzen J, Koelewijn T, Mukabana WR, Takken W. Effect of insecticide-treated bed nets on house-entry by malaria mosquitoes: the flight response recorded in a semi-field study in Kenya. Acta Trop. 2017;172:180–5.
Mathias DK, Ochomo E, Atieli F, Ombok M, Nabie Bayoh M, Olang G, et al. Spatial and temporal variation in the kdr allele L1014S in Anopheles gambiae ss and phenotypic variability in susceptibility to insecticides in Western Kenya. Malar J. 2011;10:10.
Futami K, Dida GO, Sonye GO, Lutiali PA, Mwania MS, Wagalla S, et al. Impacts of insecticide treated bed nets on Anopheles gambiae s.l. populations in Mbita district and Suba district Western Kenya. Parasit Vectors. 2014;7:63.
Bobanga T, Umesumbu SE, Mandoko AS, Nsibu CN, Dotson EB, Beach RF, et al. Presence of species within the Anopheles gambiae complex in the Democratic Republic of Congo. Trans R Soc Trop Med Hyg. 2016;110:373–5.
Wiebe A, Longbottom J, Gleave K, Shearer FM, Sinka ME, Massey NC, et al. Geographical distributions of African malaria vector sibling species and evidence for insecticide resistance. Malar J. 2017;16:85.
Lynd A, Oruni A, van’t Hof AE, Morgan JC, Naego LB, Pipini D, et al. Insecticide resistance in Anopheles gambiae from the northern Democratic Republic of Congo, with extreme knockdown resistance (kdr) mutation frequencies revealed by a new diagnostic assay. Malar J. 2018;17:412.
Fassinou AJYH, Koukpo CZ, Ossè RA, Agossa FR, Azondékon R, Sominahouin A, et al. Pesticides and the evolution of the genetic structure of Anopheles coluzzii populations in some localities in Benin (West Africa). Malar J. 2019;18:407.
Kawada H, Ohashi K, Dida GO, Sonye G, Njenga SM, Mwandawiro C, et al. Preventive effect of permethrin-impregnated long-lasting insecticidal nets on the blood feeding of three major pyrethroid-resistant malaria vectors in western Kenya. Parasit Vectors. 2014b;7:383.
Acknowledgements
We thank the participating children, their parents, local communities, and schools for supporting our study. We also thank Dr. Kazunori Ohashi and the staff members of Africa Technical Research Centre (Arusha, Tanzania) for the bioassays and chemical analysis; Dr. Hitoshi Kawada for critical comments; Ms Junko Sakemoto, Prof Yoshio Ichinose, Ms Yukie Saito, and Ms Shizuko Yagi for administrative support; Mr Peter A. Lutiali for mosquito identification; Mr Charles O. Gunga, Ms Lucy Oketch, Mr Fredrick O. Sonye and the local staff members for their dedication to the fieldwork. This study was conducted at the Kenya Research Center, Institute of Tropical Medicine, Nagasaki University, Japan. This paper is published with the permission of the Director of Kenya Medical Research Institute.
Funding
This study was partially supported by Global Health Innovative Technology Fund and conducted at the Joint Usage / Research Center for Tropical Disease, Institute of Tropical Medicine, Nagasaki University, Japan. This paper is published with the permission of the Director of Kenya Medical Research Institute.
Author information
Authors and Affiliations
Contributions
NT, NM, MH and MK conceived and designed the study. NT, NM, GOS, BA, JOK and SM organized the field work and collected data. NM and NT performed the data analyses. NT and NM wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Prior to the survey, individual written consent was obtained from all household heads or caretakers of the children. This study was approved by the Ethics Committees of the Kenya Medical Research Institute (SSC No.3168), and the Ethics Committees of the National Institute of Advanced Industrial Science and Technology (No. 2017–156).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information

Additional file 1: Fig. S1.
Variograms to examine spatial dependency in the simple regression model for each explanatory variable.

Additional file 2: Fig. S2.
Variograms to examine spatial dependency in the multiple regression model.
Additional file 3: Fig. S3.
The 95% credible intervals of each variable from non-spatial and spatial bivariate regression models.
Additional file 4: Fig. S4.
The 95% credible intervals of each variable from non-spatial and spatial multiple regression models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tamari, N., Minakawa, N., Sonye, G.O. et al. Protective effects of Olyset® Net on Plasmodium falciparum infection after three years of distribution in western Kenya. Malar J 19, 373 (2020). https://doi.org/10.1186/s12936-020-03444-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-020-03444-w