Abstract
Background
Intravenous daratumumab (DARA IV) has been increasingly used in the treatment of amyloid light-chain (AL) amyloidosis. However, the outcomes for patients administered with DARA IV have not been aggregated. The objective of this systematic review and meta-analysis was to investigate the efficacy and safety of DARA IV for AL amyloidosis.
Methods
We searched Medline, EMBASE, Cochrane Library and Web of Science up to 17 June 2021. Response rates and survival rates, and the corresponding 95% confidence intervals (CIs) were pooled and calculated using a fixed-effects model.
Results
Thirty studies (5 cohort studies and 25 single-arm studies) with 997 patients were included. In patients receiving DARA IV-based treatments, very good partial response or better response rate, complete response rate, very good partial response rate, partial response rate and overall response rate were 66% (95% CI, 62–69%), 30% (95% CI, 23–36%), 40% (95% CI, 33–46%), 17% (95% CI, 14–21%), and 77% (95% CI, 73–80%), respectively. Cardiac and renal responses were 41% (95% CI, 34–49%) and 43% (95% CI, 32–54%), respectively. 58% (95% CI, 49–66%) of patients achieved PFS one year or longer. 2.5% (range, 1–10.0%) of patients experienced grade 3 or 4 adverse events, of which the most common adverse event was lymphocytopenia (range, 13.6–25.0%).
Conclusion
This study supports the efficacy and safety of DARA IV for the treatment of patients with AL amyloidosis.
Similar content being viewed by others
Introduction
Immunoglobulin light chain (AL) amyloidosis is characterized by a clonal population of bone marrow plasma cells that produces a κ or λ type monoclonal light protein chain as either an intact molecule or a fragment. This insoluble protein deposits in tissues and interferes with organ function [1]. Treatment of systemic AL amyloidosis relies primarily on multiple myeloma regimens by suppressing the secretion of amyloid-forming monoclonal free light chains (FLCs) by underlying plasma cell clone [2]. Autologous stem cell transplantation (ASCT) is the preferred regimen for patients with transplant-eligible AL Amyloidosis. Previous studies revealed that the median overall survival (OS) of patients with AL amyloidosis who received ASCT was 10 years, although most patients were not eligible for this therapy [3, 4]. For patients who are ineligible for ASCT, therapeutic regimens derived from multiple myeloma treatments are usually used for AL Amyloidosis, such as bortezomib-cyclophosphamide-dexamethasone (CyBorD) [5, 6]. Moreover, it has been shown that the hematological complete remission (CR) rates of newly diagnosed patients receiving CyBorD regimen were 23–47% and the prognosis of stage IIIB patients were still poor [7]. CR rates of lenalidomide-based therapies for newly diagnosed patients were only 14–23% [8, 9]. Although the survival could be improved by the aforementioned therapeutic regimens in some patients with AL Amyloidosis [10], some patients are still unable to benefit from these treatments, particularly those with an advanced cardiac disease [11]. Therefore, new therapies are in need for the treatments of AL amyloidosis patients.
Daratumumab is the first-in-class antibody-based therapy targeting the glycoprotein CD38, which is overly expressed on the surface of abnormal plasma cells [12, 13]. It has been reported that a higher CD38 expression is associated with adverse survival in AL amyloidosis [14]. Plasma cell death can be induced by daratumumab through various mechanisms, including complement-dependent cytotoxicity, antibody-dependent cell-mediated cytotoxicity, antibody-dependent cellular phagocytosis, and direct cellular apoptosis [13]. The combination of subcutaneous daratumumab with bortezomib, cyclophosphamide, and dexamethasone has been demonstrated to be effective and safe for patients with AL amyloidosis in the Andromeda study [15]. However, previously published original studies on intravenous daratumumab (DARA IV)-based regimens are hampered by the difference of study populations and relatively small sample sizes [16, 17] and there has been a lack of systematic assessment and synthesis of the efficacy and safety of DARA IV-based in AL amyloidosis. Therefore, this study used meta-analysis to synthesize the efficacy and safety of DARA IV-based therapies in the treatment of patients with AL Amyloidosis to provide reference for the selection of treatment in clinical settings.
Materials and methods
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA 2020) extension statement [18]. The protocol for this systematic review was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) with an identification number “INPLASY202160054”.
Data sources and literature searches
Systematic literature searches were conducted in Medline, EMBASE, Cochrane Library and Web of Science with the search terms relating to DARA IV and amyloidosis. Searches were performed from the database inception to June 17, 2021 and were restricted to full papers using human subjects and published in English. All document types were included in the screening phase. A detailed search strategy is available in the Additional file 1: Methods S1. To supplement the electronic searches, reference lists of included studies was checked for relevant studies to identify additional published or unpublished materials (grey literature).
Study selection
Two reviewers independently screened studies by viewing the titles and abstracts. All potentially relevant citations were requested and inspected in detail using the full-text version. Disagreements were resolved by discussion, with assistance from a third party if necessary. A PRISMA flow diagram was constructed to show the full study selection process. The following inclusion and exclusion criteria were used to select studies at title and abstracts stage as well as full-text screening stage: eligible study design includes interventional and noninterventional studies investigating the efficacy and safety of DARA IV-based therapy for the treatment of patients with AL amyloidosis. For patients with AL amyloidosis, there was no limitation on age, gender, ethnicity, prior lines of therapy, Mayo stage, or comorbidity. The administration of daratumumab was limited to intravenous use. The following studies were excluded: studies not reported in English, studies without outcome data, and case reports.
Outcomes
The primary outcome was a very good partial response or better response (≥ VGPR) rate, defined as CR or VGPR. The secondary outcomes including CR was defined as normalization of the difference between involved and uninvolved free light chain (dFLC) levels and ratio, negative serum and urine immunofixation, or as defined in the original studies; VGPR was defined as a reduction in dFLC to < 40 mg/L, or as defined in the original studies; Partial response rate (PR) was defined as a greater than 50% reduction in the dFLC, or as defined in the original studies; Overall response rate (ORR) was defined as the sum rate of patients with CR, VGPR, and PR; Time to hematologic response or best hematologic response; Cardiac response rate was defined as an N-terminal pro-brain natriuretic peptide (NT-proBNP) response (> 30% and > 300 ng/L decrease in patients with a baseline NT-proBNP > 650 ng/L) or New York Heart Association (NYHA) class response (> 2 class decrease in subjects with baseline NYHA class 3 or 4), or as defined in the original studies; Renal response rate was defined as ≥ 30% decrease in proteinuria or drop in proteinuria below 0.5 g/24 h in the absence of renal progression, or as defined in the original studies; Progression-free survival (PFS) and OS, both were defined as in the original studies of 1 year or more than 1 year; Rates of ≥ 5% grade 3 or 4 adverse events (AEs); Rates of infusion-related reactions (IRRs).
When studies reported the same hematologic response, organ response or survival of different timepoints, we chose the clinical endpoints with longest observational time.
Data extraction
Data from each study was extracted independently by two reviewers using a standardized data extraction form, and disagreements were resolved by discussion or by referral to a third reviewer if necessary. If multiple publications were reported based on the same study population, we extracted all data from companion studies and removed duplicated data. A PICOS (Population, Intervention, Comparison, Outcome, Study design) structure was used to formulate the data extraction as follows: (1) General study characteristics: the first author’s name, the published year, country, study center (single/multiple); (2) Characteristics of participants: the number, gender and age of patients, diagnostic criteria, diagnostic results, inclusion/exclusion criteria, prior lines of therapies, Mayo stage, organ involvement, dFLC, and epidermal growth factor receptor (eGFR); (3) Interventions: treatment frequency, dosage, and treatment duration; (4) Outcomes: types of outcomes, definitions, and measurement timepoints; (5) Results: all relevant dichotomous results; (6) Study designs: randomized control trials (RCTs), non-randomized studies of interventions (NRSIs), single-arm studies, and case series.
Quality assessment
This single-arm meta-analysis was to pool data derived from single-arm study or the Dara-based treatment arm of randomized controlled trials and cohort studies. Therefore, we chose “Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group” that developed by the National Heart, Lung, and Blood Institute (NHLBI) and adapted for the purpose of our study (Additional file 1: Table S1) [19]. Two independent reviewers evaluated the quality of studies. The two reviewers resolved disagreements by discussion and if required, a third reviewer arbitrated.
Data synthesis and analysis
For data expressed as median and interquartile range (IQR)/range, we narratively described the data. Fixed-effects meta-analysis was performed to synthesize data using the R package “meta” (R software version 4.0.2) [20]. For dichotomous variables, we calculated risk ratios (RRs) with 95% confidence intervals (CIs). When no event was observed, we added a fixed value (typically 0.5) to the event number of intervention group. Where heterogeneity was significant (P ≤ 0.1 and I2 ≥ 50%), and the sources of heterogeneity were identified, we conducted a subgroup analysis to pool the data. When the source of heterogeneity was not identified by subgroup analysis, we used a random-effects model to pool the result. We performed a subgroup analysis on the primary outcome according to the type of regimen (daratumumab ± dexamethasone versus triple regimens), line of therapy (newly diagnosed versus relapsed/refractory), Mayo stage (I versus II versus III), and primary versus secondary patients. We did a sensitivity analysis, the Freeman-Tukey double arcsine transformation analysis was performed to deal 0 event, using stata package “metaprop” (Stata software version 15.0) [21]. We also did a sensitivity analysis, random-effects meta-analysis was performed when heterogeneity was not significant (P > 0.1 and I2 < 50%).
Results
Results of study selection
Figure 1 shows the flow diagram displaying the literature search results. The initial search retrieved a total of 496 articles, including 476 articles from databases, and 20 articles from conferences. After deduplication, 315 unique articles remained. We excluded 221 articles by screening the titles and abstracts. 48 articles were further excluded in a full-text review, leaving 46 eligible publications from 30 study populations, including 5 cohort studies and 25 single-arm studies [2, 16, 17, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64].
Characteristics of included studies and participants
A total of 30 studies with 997 participants were included in this review (for details of included studies, see Additional file 1: Table S2). The data of these studies were contributed by ten countries, namely the US (n = 15), Italy (n = 3), Germany (n = 2), Israel (n = 2), France (n = 2), Switzerland (n = 1), Austria (n = 1), Spain (n = 1), the UK (n = 1) and Greece (n = 1). There was one international collaborative study (France and Italy).
The characteristics of patients included in this study are summarized in Table 1. Of 888 patients, over half (62.7%) were male; of 736 patients, the ages ranged from 34 to 91 years. Of 441 patients, 87.8% patients were λ isotype and 12.2% were κ isotype. Of patients that reported the status of disease, most of them were at the relapsed or refractory stage (489/517). Mayo 2004 cardiac staging was available for 303 patients: 16.2% were stage I, 40.6% were stage II, and 43.2% were stage III. Mayo 2012 cardiac staging was available for 109 patients: 12.8% were stage I, 33.0% were stage II, 30.3% were stage III, and 23.9% were stage IV. The most commonly involved organs included the heart (74.3%), kidney (60.5%) and liver (8.2%).
Treatments
Of 997 patients with identified therapies, 665 (n = 665/977, 66.7%) received a daratumumab mono or combined with dexamethasone regimen (Dara ± dex), Daratumumab + Bortezomib + Dexamethasone (DVd) in 108 (10.8%), Daratumumab + Lenalidomide + Dexamethasone (DRd) in 71 (7.1%) and Daratumumab + Cyclophosphamide + Dexamethasone (DCd) in 4 (0.4%) (Table 2). The median of the treatment duration ranged from 4 to 31 cycles.
Quality assessment of included studies
All 30 studies clearly stated research questions or objectives, of which 27 studies clearly prespecified and described eligibility/selection criteria for the study population. The participants lost to follow-up were less than 20% in 26 studies, while in the other four studies more than 20% of participants were lost to follow-up. Eighteen studies prespecified and clearly defined measures of outcomes. Only one study described the evaluable sample size, while in the other studies, the authors were uncertain whether sample sizes were sufficient. None of the 30 studies reported blinding of the participants. Details of the quality assessment of included studies are shown in Additional file 1: Table S1.
Hematologic response and organ response
In 26 studies that reported a robust hematologic response (Fig. 2), 536 of 769 patients (66%; 95% CI, 62–69%; I2 = 41%) achieved a ≥ VGPR after treatment with daratumumab-based regimens. The overall response rate was 77% (95% CI, 73–80%), with a CR was achieved in 30% of patients (95% CI, 23–36%), a VGPR was achieved in 40% (95% CI, 33–46%), a PR was achieved in 17% (95% CI, 14–21%). In 15 studies with 397 patients, the median time to a first hematologic response ranged from 7 to 78 days, and in 11 studies with 253 patients, the median time to the best hematologic response ranged from 30 to 336 days (Additional file 1: Tables S3, S4). Cardiac and renal responses occurred in 41% (95% CI, 34–49%) and 43% (95% CI, 32–54%) of patients, respectively (Table 3). Forest plots are presented in Additional file 1: Fig. S1-S6.
Very good partial response or better rate
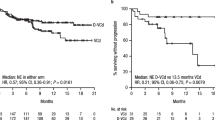
Figure 3 shows the pooled ≥ VGPR rate by categories of treatments, Mayo 2004 stage, newly diagnosis or relapsed/refractory and primary or secondary AL amyloidosis. Subgroup analyses revealed improvement in the ≥ VGPR rate following treatment with triple regimens. In three studies, 64 of 89 patients treated with a daratumumab-based triple regimens achieved ≥ VGPR (71%; 95% CI, 60–80%; I2 = 35%), whereas 251 of 387 patients in 16 studies treated with daratumumab mono or combined with dexamethasone (Dara ± dex) achieved ≥ VGPR (63%; 95% CI, 58–68%; I2 = 39%) (Fig. 3, Additional file 1: Fig. S7). It also showed that similar ≥ VGPR rates across different Mayo stages (Fig. 3, Additional file 1: Fig. S8-S9,) and patients with primary or secondary AL amyloidosis (Fig. 3, Additional file 1: Fig. S10), whereas a higher ≥ VGPR rates were observed in newly diagnosed patients than in patients with relapsed/refractory disease (84% vs. 67%, respectively) (Fig. 3, Additional file 1: Fig. S11). Notably, interpretation of subgroup analysis result should made with caution because of the small and imbalance sample sizes in each group.
Meta-analysis with a random effects model showed heterogeneity in the rate of VGPR, CR and renal response and the source of heterogeneity could not be identified when investigated by predefined subgroup factors. Line of therapy of newly diagnosed or relapsed/refractory may be one of the sources of heterogeneity in cardiac response rate. Subgroup analysis of the cardiac response in the newly diagnosed group showed ten of the 18 (55%; 95% CI, 32–76%; I2 = 12%) patients had a cardiac response, while in the relapsed or refractory group, 77 of 200 (39%; 95% CI, 32–46%; I2 = 36%) patients had a cardiac response. However, due to the small sample size of the subgroup, the results must be interpreted with caution.
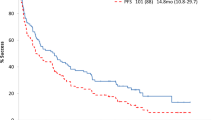
Progression-free survival and overall survival
Three studies [2, 48, 64] reported a PFS rate of 1 year or longer. Seventy-three of 126 (58%; 95% CI, 49–66%; I2 = 46%) patients reached PFS after 1 year or longer (Additional file 1: Fig. S12). Of 11 studies reporting OS, 411 of 534 (76%; 95% CI, 72–80%; I2 = 31%) patients survived after 1 year or longer (Additional file 1: Fig. S13). The causes of death were disease progression, infection, sepsis, immunomodulatory agent–related rejection of the transplanted heart and cardiac complication [2, 31, 54, 58, 64].
Adverse events
Fifteen studies reported IRRs. Of the included 276 patients, 87 experienced grade 1 or 2 IRRs (33%; 95% CI, 21–47%; I2 = 76%) with a median rate of 33.3% (range, 11.1–70.0%) (Additional file 1: Fig. S14), 10 of 432 patients (3%; 95% CI, 2–6%; I2 = 0) experienced grade 3 or 4 IRRs with a median rate of 2.5% (range, 1.0–10.0%) (Additional file 1: Fig. S15).
Nine studies reported grade 3 or 4 adverse events. The most common (≥ 5%) grade 3 or 4 adverse events reported in more than one study were lymphocytopenia, heart failure, infection complications, pneumonia, fatigue, atrial fibrillation, neutropenia, and diarrhea. (Table 4) Other adverse events reported were presented in Additional file 1: Table S5.
Sensitivity analysis
The CR was achieved in 29% of patients (95% CI, 22–36%), a VGPR was achieved in 39% (95% CI, 32–46%), a PR was achieved in 14% (95% CI, 9–19%) (Additional file 1: Fig. S16–S18). Renal responses occurred in 41% (95% CI, 30–53%) (Additional file 1: Fig. S19). 10 of 432 patients (1%; 95% CI, 0–2%; I2 = 16.64%) experienced grade 3 or 4 IRRs (Additional file 1: Fig. S20). The results using Freeman-Tukey double arcsine transformation were similar to the results found. The results of the random-effects model were similar to those of the fixed-effects model, as shown in Additional file 1: Table S6.
Discussion
This systematic review and meta-analysis of 30 studies evaluated the efficacy and safety of DARA IV-based therapies for the treatment of patients with AL amyloidosis. First, the results showed 66% of patients achieved ≥ VGPR. Subgroup analysis showed a slightly increased ≥ VGPR rate in patients treated with daratumumab-based triple regimens than mono or combined with only dexamethasone (71% vs. 63%). We also observed ≥ VGPR rates were similar for patients with primary or secondary AL amyloidosis (65% vs. 64%). Furthermore, rates of ≥ VGPR were higher in patients with newly diagnosed AL amyloidosis (84%) than in those with relapsed/refractory disease (67%). However, findings from the subgroup analysis should be interpreted with caution as additional studies are needed for confirmation [65].
In this study, the CR, VGPR and PR rates were 30%, 40% and 17%, respectively. In a prospective study including 915 patients with AL amyloidosis treated with bortezomib-based therapies, the CR rate was only 25%, and the cardiac and renal response rates were 32.5% and 15.4%, respectively [66]. A retrospective analysis of 25 patients with relapsed and refractory AL amyloidosis treated with DARA IV reported a hematologic response rate of 76%, with 36% of patients achieving CR and 24% achieving a very good partial response (VGPR) [38]. Moreover, 77% of patients achieved an overall response, 41% of patients with cardiac involvement exhibited a cardiac response, and 43% of patients with renal involvement showed a renal response.
This study revealed that 58% and 76% of patients reached one-year or longer PFS and OS, respectively, even though most included patients had relapsed/refractory AL amyloidosis. It is important to note that due to limited studies, only four studies in this review reported 1 year or longer progression-free survival rates with no more than 2 years follow-up. For comparison, in a study assessing the efficacy and safety of lenalidomide, melphalan and dexamethasone in AL amyloidosis patients with high rates of advanced cardiac involvement, the one-year survival rate was 58% [67]. This study suggested that treatment with DARA IV may improve survival for patients with AL amyloidosis.
Most of the IRRs were grade 1 or 2. 33% of patients experienced grade 1 or 2 IRRs and 3% of patients experienced grade 3 or 4 IRRs. The most common grade 3 or 4 adverse events reported were lymphocytopenia, heart failure, infection complications, pneumonia, fatigue, atrial fibrillation, neutropenia, and diarrhea. However, caution should be exercised when interpreting the results, as cardiac-related complications due to amyloid deposition are expected in AL amyloidosis and limitations of the meta-analysis. Besides, there were no new adverse events related to daratumumab. Overall, DARA IV therapy had an acceptable safety profile for patients with AL amyloidosis.
This study has several strengths. First, this study had good quality control. We conducted this study strictly according to the Cochrane and PRISMA standard. An information specialist performed the literature search. When necessary, a hand search was used to identify the reference lists of systematic reviews and conference abstracts. The screening and data extraction processes were performed independently by two reviewers and checked by a third independent assessor, ensuring the accuracy of the data. Second, to our knowledge, this study is the first comprehensive and the most current meta-analysis evaluating the efficacy and safety of DARA IV for the treatment of patients with AL amyloidosis. Third, we conducted subgroup analyses to reduce heterogeneity as much as possible.
There are nonetheless several limitations. Due to the language limitation, literature not in English and Chinese were excluded. All included studies were single arm studies or cohort studies, blinding and sample size calculation methods were not reported for most studies, which may either overestimate or underestimate the efficacy of DARA IV.
In conclusion, results of this meta-analysis suggests that DARA IV-based therapies are effective in generating hematologic and organ responses in both newly diagnosed and relapsed/refractory patients with AL amyloidosis. The safety profile is consistent with that has been previously documented for DARA IV in this population.
Availability of data and materials
Not applicable.
Abbreviations
- DARA IV:
-
Intravenous daratumumab
- AL:
-
Amyloid light-chain
- FLCs:
-
Free light chains
- ASCT:
-
Autologous stem cell transplantation
- OS:
-
Overall survival
- CyBorD:
-
Bortezomib-Cyclophosphamide-Dexamethasone
- CR:
-
Complete remission
- DARA:
-
Daratumumab
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- INPLASY:
-
International Platform of Registered Systematic Review and Meta-analysis Protocols
- VGPR:
-
Very good partial response
- dFLC:
-
Difference between involved and uninvolved free light chain
- PR:
-
Partial response
- ORR:
-
Overall response
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- NYHA:
-
New York Heart Association
- PFS:
-
Progression-free survival
- AEs:
-
Adverse events
- IRRs:
-
Infusion-related reactions
- PICOS:
-
Population, Intervention, Comparison, Outcome, Study design
- eGFR:
-
Epidermal growth factor receptor
- RCTs:
-
Randomized control trials
- NRSIs:
-
Non-randomized studies of interventions
- NHLBI:
-
National Heart, Lung, and Blood Institute
- IQR:
-
Interquartile range
- RRs:
-
Risk ratios
- CIs:
-
Confidence intervals
References
Gertz MA. Immunoglobulin light chain amyloidosis: 2020 update on diagnosis, prognosis, and treatment. Am J Hematol. 2020;95(7):848–60.
Roussel M, Merlini G, Chevret S, Arnulf B, Stoppa AM, Perrot A, et al. A prospective phase 2 trial of daratumumab in patients with previously treated systemic light-chain amyloidosis. Blood. 2020;135(18):1531–40.
Palladini G, Milani P, Merlini G. Management of AL amyloidosis in 2020. Blood. 2020;136(23):2620–7.
Sidiqi MH, Aljama MA, Buadi FK, Warsame RM, Lacy MQ, Dispenzieri A, et al. Stem cell transplantation for light chain amyloidosis: decreased early mortality over time. J Clin Oncol. 2018;36(13):1323–9.
Group. CSLCAC, Center. NKDCMR, Diseases. NCMRCfH. Guidelines for the diagnosis and treatment of systemic light chain amyloidosis (revised in 2021). Chin Med J. 2021;101(22):1646–56.
Palladini GSS, Merlini G, et al. First glimpse on real-world efficacy outcomes for 2000 patients with systemic light chain amyloidosis in Europe: a retrospective observational multicenter study by the European myeloma network. Blood. 2020;136(Supplement 1):50–1.
Yu GY, Li J. Treatment progress of primary light⁃chain amyloidosis. J Leukemia Lymphoma. 2021;30(1):11–3.
Cibeira MT, Oriol A, Lahuerta JJ, Mateos MV, de la Rubia J, Hernandez MT, et al. A phase II trial of lenalidomide, dexamethasone and cyclophosphamide for newly diagnosed patients with systemic immunoglobulin light chain amyloidosis. Br J Haematol. 2015;170(6):804–13.
Moreau P, Jaccard A, Benboubker L, Royer B, Leleu X, Bridoux F, et al. Lenalidomide in combination with melphalan and dexamethasone in patients with newly diagnosed AL amyloidosis: a multicenter phase 1/2 dose-escalation study. Blood. 2010;116(23):4777–82.
Rysava R. AL amyloidosis: advances in diagnostics and treatment. Nephrol Dial Transplant. 2019;34(9):1460–6.
Sidiqi MH, Gertz MA. Daratumumab for the treatment of AL amyloidosis. Leuk Lymphoma. 2019;60(2):295–301.
Hashmi H, Husnain M, Khan A, Usmani SZ. CD38-directed therapies for management of multiple myeloma. Immunotargets Therapy. 2021;10:201–11.
Roccatello D, Fenoglio R, Sciascia S, Naretto C, Rossi D, Ferro M, et al. CD38 and anti-CD38 monoclonal antibodies in AL amyloidosis: targeting plasma cells and beyond. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21114129.
Seckinger A, Hillengass J, Emde M, Beck S, Kimmich C, Dittrich T, et al. CD38 as immunotherapeutic target in light chain amyloidosis and multiple myeloma-association with molecular entities, risk, survival, and mechanisms of upfront resistance. Front Immunol. 2018;9:1676.
Kastritis E, Palladini G, Minnema MC, Wechalekar AD, Jaccard A, Lee HC, et al. Daratumumab-based treatment for immunoglobulin light-chain amyloidosis. N Engl J Med. 2021;385(1):46–58.
Lecumberri R, Krsnik I, Askari E, Sirvent M, Gonzalez-Perez MS, Escalante F, et al. Treatment with daratumumab in patients with relapsed/refractory AL amyloidosis: a multicentric retrospective study and review of the literature. Amyloid. 2020;27(3):163–7.
Schwotzer R, Manz MG, Pederiva S, Waibel C, Caspar C, Lerch E, et al. Daratumumab for relapsed or refractory AL amyloidosis with high plasma cell burden. Hematol Oncol. 2019;37(5):595–600.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed). 2021;372: n71.
National Heart L, and Blood Institute. Quality assessment tool for before-after (pre-post) studies with no control group. Maryland: National Heart, Lung, and Blood Institute; [updated 2021 July; cited 2013]. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
Team. RC. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/. 2020.
Efthimiou O. Practical guide to the meta-analysis of rare events. Evid Based Ment Health. 2018;21(2):72–6.
Abeykoon JP, Zanwar S, Dispenzieri A, Gertz MA, Leung N, Kourelis T, et al. Daratumumab-based therapy in patients with heavily-pretreated AL amyloidosis. Leukemia. 2019;33(2):531–6.
Chung A, Kaufman GP, Sidana S, Eckhert E, Schrier S, Arai S, et al. Long-term outcomes and organ responses with daratumumab therapy in previously treated patients with al amyloidosis. Blood. 2019;134(Supplement1):1828.
Chung A, Kaufman GP, Sidana S, Eckhert E, Schrier SL, Lafayette RA, et al. Organ responses with daratumumab therapy in previously treated AL amyloidosis. Blood Adv. 2020;4(3):458–66.
Cohen O, Brodermann MH, Blakeney IJ, Mahmood S, Sachchithanantham S, Ravichandran S, et al. The UK experience of daratumumab monotherapy in relapsed systemic AL amyloidosis. Br J Haematol. 2020;189:116–7.
Cohen OC, Brodermann MH, Blakeney IJ, Mahmood S, Sachchithanantham S, Ravichandran S, et al. Rapid response to single agent daratumumab is associated with improved progression-free survival in relapsed/refractory AL amyloidosis. Amyloid Int J Exp Clin Investig. 2020;27(3):200–5.
Dima D, Hu X, Dower J, Comenzo RL, Varga C. Pattern of use and efficacy of daratumumab-based therapy in patients with AL amyloidosis: a single institution experience. Blood. 2020;136(Supplement 1):44–5.
Fazio F, Basset M, Milani P, Foli A, Nuvolone M, Foà R, et al. Treatment with daratumumab in patients with multiple myeloma associated AL amyloidosis. Blood. 2019;134(Supplement1):1860.
Godara A, Siddiqui NS, Lee L, Toskic D, Fogaren T, Varga C, et al. Combined use of two monoclonal antibodies in patients with systemic AL amyloidosis and cardiac involvement. J Clin Oncol. 2019;37(15):8009.
Godara A, Siddiqui NS, Lee LX, Toskic D, Fogaren T, Varga C, et al. Dual monoclonal antibody therapy in patients with systemic AL amyloidosis and cardiac involvement. Clin Lymphoma Myeloma Leuk. 2020;20(3):184–9.
Gounot R, Le Bras F, Dupuis J, Oghina S, Bodez D, Roulin L, et al. Daratumumab is safe and induces a rapid hematological response in light-chain amyloidosis with severe cardiac impairment. Leuk Lymphoma. 2020;62(4):979–83.
Gounot R, Lemonnier F, Dupuis J, Oghina S, Bodez D, Ladaique A, et al. Daratumumab is well tolerated and induces a rapid hematological response in non IG-M light chain amyloidosis with severe cardiac impairment. EHA Learning Center. On Saturday, June 15, 2019 from 17:30–19:00.
Jaccard A, Arnulf B, Stoppa AM, Karlin L, Perrot A, Macro M, et al. A prospective phase II study of daratumumab in previously-treated systemic light-chain (AL) amyloidosis. HemaSphere. 2018;130(Supplement 1):508.
Jeryczynski G, Antlanger M, Duca F, Binder-Rodriguez C, Reiter T, Simonitsch-Klupp I, et al. First-line daratumumab shows high efficacy and tolerability even in advanced AL amyloidosis: the real-world experience. ESMO open. 2021;6(2): 100065.
Jeryczynski G, Eder A, Reitter EM, Krauth MT, Agis H. Firstline daratumumab shows high hematologic and organ response rates in advanced cardiac al amyloidosis—a retrospective case series. Blood. 2019;134(Supplement1):3123.
Kastritis E, Gavriatopoulou M, Kostopoulos IV, Dialoupi I, Roussou M, Kanellias N, et al. Consolidation with a short course of daratumumab can significantly improve complete response rates in patients with al amyloidosis or LCDD. EHA Learning Center. On Saturday, June 15, 2019 from 17:30–19:00.
Kaufman G, Witteles R, Wheeler M, Ulloa P, Lugtu M, Arai S, et al. Hematologic responses and cardiac organ improvement in patients with heavily pretreated cardiac immunoglobulin light chain (AL) amyloidosis receiving daratumumab. Blood. 2016;128(22):4525.
Kaufman GP, Schrier SL, Lafayette RA, Arai S, Witteles RM, Liedtke M. Daratumumab yields rapid and deep hematologic responses in patients with heavily pretreated AL amyloidosis. Blood. 2017;130(7):900–2.
Kennedy VE, Shah N, Wolf JL, Martin TG, Wong SWK. Front-line daratumumab in newly diagnosed AL amyloidosis patients. J Clin Oncol. 2020;38(15): e20569.
Khouri J, Bicky T, Reu FJ, Samaras CJ, Liu HD, Karam MA, et al. Daratumumab is safe and highly effective in al amyloidosis. Blood. 2017;130(Supplement 1):1819.
Khouri J, Kin A, Thapa B, Reu FJ, Bumma N, Samaras CJ, et al. Daratumumab proves safe and highly effective in AL amyloidosis. Br J Haematol. 2019;185(2):342–4.
Kimmich C, Schönland S, Ziehl R, Ho AD, Dittrich T, Müller-Tidow C, et al. Daratumumab monotherapy in thirty-two heavily pre-treated patients with advanced systemic light-chain amyloidosis. Blood. 2017;130(Supplement 1):1837.
Kimmich CR, Terzer T, Benner A, Dittrich T, Veelken K, Carpinteiro A, et al. Daratumumab for systemic AL amyloidosis: prognostic factors and adverse outcome with nephrotic-range albuminuria. Blood. 2020;135(18):1517–30.
Kimmich CR, Terzer T, Benner A, Hansen T, Carpinteiro A, Dittrich T, et al. Daratumumab, lenalidomide, and dexamethasone in systemic light-chain amyloidosis: high efficacy, relevant toxicity and main adverse effect of gain 1q21. Am J Hematol. 2021;96(7):253–7.
Kleman A, Leng S, Szabo A, Wu R, Chhabra S, Dhakal B, et al. Changes in cardiac biomarkers with daratumumab therapy in patients with light chain amyloidosis. Clin Lymphoma Myeloma Leuk. 2019;19(10):e321–2.
Lee LX, Ho K, Zhou P, Varga C, Fogaren T, Toskic D, et al. Daratumumab activity is agnostic to FC gamma receptor 3a (FCγr3a) 158 genotype in patients with primary refractory or relapsed systemic al amyloidosis. Blood. 2017;130(Supplement 1):3164.
Lee LX, Zhou P, Varga C, Fogaren T, Ho K, Ma X, et al. Daratumumab activity in relapsed or primary refractory systemic AL amyloidosis and Fc gamma receptor 3A V158F polymorphisms. Amyloid J Protein Folding Disord. 2019;26(2):101–2.
Lee SS, Rosko N, Patel BJ, Waldron M, Tomer J, Goldman R, et al. Rapid hematologic and organ responses with daratumumab, bortezomib and dexamethasone in patients with relapsed/refractory AL amyloidosis. Blood. 2018;132(Supplement 1):2009.
Milani P, Fazio F, Basset M, Berno T, Larocca A, Foli A, et al. High rate of profound clonal and renal responses with daratumumab treatment in heavily pre-treated patients with light chain (AL) amyloidosis and high bone marrow plasma cell infiltrate. Am J Hematol. 2020;95(8):900–5.
Milani P, Fazio F, Basset M, Berno T, Larocca A, Foli A, et al. Treatment with daratumumab in patients with multiple myeloma associated al amyloidosis. Blood. 2019;134(Supplement1):1860.
Ozga M, Zhao Q, Benson DM, Elder P, Williams N, Bumma N, et al. The effect of cytogenetic abnormalities on organ involvement and survival in patients with al amyloidosis. Blood. 2019;134(Supplement1):1833.
Pick M, Vainstein V, Goldschmidt N, Lavie D, Libster D, Gural A, et al. Daratumumab resistance is frequent in advanced-stage multiple myeloma patients irrespective of CD38 expression and is related to dismal prognosis. Eur J Haematol. 2018;100(5):494–501.
Ratermann K, Steinbach M, Caballero K, Cowley J, Nativi-Nicolau J, Kovacsovics T. Retrospective study of AL-amyloid patients with t(11;14) treated with daratumumab. Clin Lymphoma Myeloma Leuk. 2019;19(10): e328.
Riva M, Scapinello G, Ammirati L, Lessi F, Branca A, Zambello R, et al. Daratumumab in heavily pretreated, transplant ineligible, AL amyloidosis patients: a single centre experience. Haematologica. 2019;104:64–5.
Rosko N, Mo H, Rudoni J, Siebenaller C, Lee SS, Chakraborty R, et al. Rapid infusion daratumumab is safe in patients with AL amyloidosis. Blood. 2019;134(Supplement1):1838.
Roussel M, Arnulf B, Stoppa AM, Karlin L, Perrot A, Macro M, et al. A prospective phase II of daratumumab in previously treated systemic light-chain (AL) amyloidosis: updated results. Clin Lymphoma Myeloma Leuk. 2019;19(10):e40–1.
Roussel M, Stoppa AM, Perrot A, Karlin L, Arnulf B, Macro M, et al. A prospective phase ii of daratumumab in previously-treated systemic light-chain (AL) amyloidosis. Blood. 2017;130((Roussel M.) Hematology Department, IUCT-Oncopole, Toulouse, France).
Sanchorawala V, Sarosiek S, Schulman A, Mistark M, Migre ME, Cruz R, et al. Safety, tolerability, and response rates of daratumumab in relapsed AL amyloidosis: results of a phase 2 study. Blood. 2020;135(18):1541–7.
Sanchorawala V, Sarosiek S, Sloan JM, Brauneis D, Migre ME, Mistark M, et al. Safety, tolerability and response rates of daratumumab in patients with relapsed light chain (AL) amyloidosis: results of a phase II study. Blood. 2018;132.
Sanchorawala V, Sarosiek S, Sloan JM, Brauneis D, Migre ME, Mistark M, et al. Safety and tolerability of daratumumab in patients with relapsed light chain (AL) amyloidosis: preliminary results of a phase ii study. Blood. 2017. https://doi.org/10.1182/blood-2018-99-112991.
Shragai T, Gatt M, Lavie N, Vaxman I, Tadmor T, Rouvio O, et al. Daratumumab for relapsed AL amyloidosis—when cumulative real-world data precedes clinical trials: a multisite study and systematic literature review. Eur J Haematol. 2021;106(2):184–95.
Sidiqi MH, Al Saleh ASS, Vaxman I, Dispenzieri A, Buadi FK, Muchtar E, et al. Optimal therapy for relapsed al amyloidosis post autologous stem cell transplant. Blood. 2019. https://doi.org/10.1182/blood-2019-125453.
Van De Wyngaert Z, Carpentier B, Pascal L, Lionne P, Leduc I, Srour M, et al. Efficacy and safety of daratumumab in a frail real-life relapsed or refractory systemic light-chain amyloidosis population (AL): report on 15 cases from the North of France. Blood. 2018. https://doi.org/10.1182/blood-2018-99-116801.
Van de Wyngaert Z, Carpentier B, Pascal L, Lionne-Huyghe P, Leduc I, Srour M, et al. Daratumumab is effective in the relapsed or refractory systemic light-chain amyloidosis but associated with high infection burden in a frail real-life population. Br J Haematol. 2020;188(3):e24–7.
Liu B, Wang Y, Bai M, Sun S. A comparative study of cyclophosphamide, thalidomide and dexamethasone (CTD) versus bortezomib and dexamethasone (BDEX) in al amyloidosis: a real-word study in chinese patients. Nephrol Dial Transplant. 2020;35(SUPPL 3):574.
Manwani R, Cohen O, Sharpley F, Mahmood S, Sachchithanantham S, Foard D, et al. A prospective observational study of 915 patients with systemic AL amyloidosis treated with upfront bortezomib. Blood. 2019;134(25):2271–80.
Dinner S, Witteles W, Afghahi A, Witteles R, Arai S, Lafayette R, et al. Lenalidomide, melphalan and dexamethasone in a population of patients with immunoglobulin light chain amyloidosis with high rates of advanced cardiac involvement. Haematologica. 2013;98(10):1593–9.
Acknowledgements
We thank Dr. Margueritte White of Global Community Writer for the language editing. We appreciate Dr. Xin Gao for his supports in the statistical methods development. The collection and assembly of data and statistical expertise were provided by Ms. Yang Zhang and Ms. Yan Huo, from Systematic Review Solutions, Ltd.
Funding
This work was supported by Xi’an Janssen Pharmaceutical Ltd. The authors were responsible for all content and editorial decisions, and received no honoraria related to the development of this publication.
Author information
Authors and Affiliations
Contributions
Draft protocol, JL and BW; study selection, RZ and XW; data extraction, LX and BW; data analysis, CS and XW; writing-review and editing, CS and JL. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhang Renyi was a Janssen employee and works for an Overland ADCT biopharma.
Supplementary Information
Additional file 1: Methods S1.
Search strategy. Table S1. Study quality based on (Before-After (Pre-Post)) outlined by National Institutes of Health (NIH). Table S2. Characteristics of studies include in this review. Table S3. The median time to first hematologic response. Table S4. The median time to best hematologic response. Table S5. Other adverse events in included studies. Table S6. Results of the random effects model in sensitivity analysis. Fig. S1. Meta-analysis forest plot of overall response rate. Fig. S2. Meta-analysis forest plot of complete remission. Fig. S3. Meta-analysis forest plot of very good partial response. Fig. S4. Meta-analysis forest plot of partial response. Fig. S5. Meta-analysis forest plot of cardiac response. Fig. S6. Meta-analysis forest plot of renal response. Fig. S7. Meta-analysis forest plot of ≥ VGPR-intervention. Fig. S8. Meta-analysis forest plot of ≥ VGPR-Mayo 2004. Fig. S9. Meta-analysis forest plot of ≥ VGPR-Mayo 2004 IIIA/B. Fig. S10. Meta-analysis forest plot of ≥ VGPR-primary or secondary. Fig. S11. Meta-analysis forest plot of ≥ VGPR-line of therapy. Fig. S12. Meta-analysis forest plot of PFS-1 year or longer. Fig. S13. Meta-analysis forest plot of OS-1 year or longer. Fig. S14. Meta-analysis forest plot of Infusion related reaction-grade-1–2. Fig. S15. Meta-analysis forest plot of Infusion related reaction-grade-3–4. Fig. S16. Meta-analysis forest plot of complete remission. Fig. S17. Meta-analysis forest plot of very good partial response. Fig. S18. Meta-analysis forest plot of partial response. Fig. S19. Meta-analysis forest plot of Renal response. Fig. S20. Meta-analysis forest plot of Infusion related reaction-grade-3–4.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, C., Wang, X., Zhang, R. et al. Efficacy and safety of intravenous daratumumab-based treatments for AL amyloidosis: a systematic review and meta-analysis. Cancer Cell Int 22, 222 (2022). https://doi.org/10.1186/s12935-022-02635-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-022-02635-6