Abstract
Background
MYCN gene amplification is related to risk stratification. Therefore it is important to identify accurately the level of the MYCN gene as early as possible in neuroblastoma (NB); however, for patients with bone marrow (BM) metastasis who need chemotherapy before surgery, timely detection of the MYCN gene is not possible due to the unavailability of primary tumors.
Methods
MYCN gene status was evaluated in 81 BM metastases of NB by interphase fluorescence in situ hybridization (FISH) analysis of BM cells. The clinicobiological characteristics and prognostic impact of MYCN amplification in NB metastatic to BM were analyzed.
Results
MYCN amplification was found in 16% of patients with metastases, and the results were consistent with the primary tumors detected by pathological tissue FISH. MYCN amplification was associated with age, lactate dehydrogenase (LDH) levels and prognosis (P = 0.038, P < 0.001, P = 0.026). Clinical outcome was poorer in patients with MYCN amplification than in those without amplification (3-year EFS 28.8 ± 13.1 vs. 69.7 ± 5.7%, P = 0.005; 3-year OS 41.5 ± 14.7 vs. 76.7 ± 5.5%, P = 0.005).
Conclusions
MYCN amplification predicts a poor outcome in NB metastatic to BM, and interphase FISH of bone marrow cells provides a timely direct and valid method to evaluate the MYCN gene status.
Similar content being viewed by others
Background
Neuroblastoma (NB),derived from the postganglionic sympathetic nervous system, is the most common extracranial malignancy in children [1]. It represents 8–10% of pediatric tumors and accounts for >10% of all pediatric cancer mortality [2]. Early NB often is clinically unrecognized [3]. The primary tumor usually occurs in the abdomen (60%), but more than 50% of children with neuroblastoma present with metastasis at diagnosis, and bone marrow (BM) is the most common site of metastasis (70.5%) [4]. In recent years, substantial progress has been made in the treatment effect of NB combinations of chemotherapy, radiotherapy, surgical resection and hematopoietic stem cell transplantation; however the 5-year overall survival (OS) is still less than 50% in high-risk NB [5, 6].
The MYCN gene codes for an oncogenic transcription factor and belongs to the MYC family of genes [7]. Amplification of the MYCN gene was observed in approximately 20% of all NB, and is considered to be a molecular marker to identify high-risk patients [8]. Because MYCN gene amplification is related to risk stratification, it is therefore important to identify accurately the level of MYCN gene amplification as early as possible in order to avoid either under- or over-treating patients [9–11]. At present, it is imperative to detect MYCN gene amplification in many established NB treatment protocols by fluorescence in situ hybridization (FISH) [12]. The samples are usually tissue from primary tumors; however, for those patients who need chemotherapy prior to surgery, timely identification of the level of MYCN gene is not possible because of the limited nature of tumor biopsies. BM is the most common site of metastasis, and there are no reports on the status of the MYCN gene in BM cells in patients with NB metastatic to BM.
The aim of our study was to clarify the clinical value of interphase FISH technique in detecting MYCN amplification of BM cells and evaluate the biological characteristics and prognostic impact of MYCN status in NB metastatic to BM.
Methods
Patients and treatment
A total of 81 pediatric patients aged 5–103 months (median 39 months) with newly diagnosed NB with BM metastasis at the Haematology Oncology Centre of Beijing Children’s Hospital, Capital Medical University, between January 2012 and August 2014 were enrolled in this research. The criterion for patient inclusion was ≥20% NB cells in diagnostic BM samples. BM samples of all patients were collected at diagnosis. Cells were cultured in RPMI-1640 medium supplemented with 20% fetal bovine serum. After 24 h in culture, the cells were treated with 0.075 mol/LKCl for 30 min, and then were fixed twice in a 3:1 mixture of methanol:acetic acid. Then the cells were stored in the above fixative solution at 4 °C.
The BCH-NB-2007 protocol [13] was used in all patients. All patients were followed until June 2016, with a median follow-up time of 28.2 months (range 0.5–54 months). This research and the BCH-NB-2007 protocol were approved by the Beijing Children’s Hospital Institutional Ethics Committee. Informed consent was obtained from the parents or guardians of each patient according to the Declaration of Helsinki.
Morphologic analysis and diagnostic biomarkers detection
Microscopic examinations of BM aspirates and biopsies were performed to determine the presence of NB cells. The presence of NB cells was determined by 2 independent laboratory pathologists, expert in this area. Serum tumour markers such as lactate dehydrogenase (LDH) and neuron specific enolase (NSE) levels were detected at the time of diagnosis in all patients. Urinary homovanillic acid (HVA) and vanillylmandelic acid (VMA) are typically measured in urine for the diagnosis and monitoring of NB.
FISH analysis of bone marrow cells
The FISH technique was applied using a DNA probe LSI N-MYC (2p24)/CEP2 (2p11.1-q11.1) Dual Color Probe (Vysis) to count the number of MYCN copies in relation to the number of chromosomes 2. FISH was performed in a dual-color procedure following the manufacturers’ instructions. BM cells fixed in methanol-acetic acid solution were dropped onto cleaned glass slides. The slides were denatured in 70% formamide/2× standard saline citrate (SSC) at 73 °C for 5 min, then dehydrated through an ethanol series of 70, 85 and 100% for 2 min, each. The probe mixture contained 7 μl hybridization buffer, 1 μl probe and 2 μl double-distilled water. The mixture was denatured for 5 min at 73 °C, and then applied on the slide. Hybridization was performed overnight at 37 °C under sealed coverslips. The slide was washed immediately in 0.4 × SSC/0.3%NP-40 (PH7.5) at 73 °C for 1 min, followed by 2 × SSC/0.1%NP-40 (PH7.0) at room temperature for 1 min. The nuclei were counterstained with 10 μl DAPI, and 400 cells were counted on one slide. Fluorescence images were taken with a Leica DM6000B microscope.
In accordance with the recommendations of the European Neuroblastoma Quality Assessment group [14], amplification was defined as a >fourfold increase of MYCN signals in relation to the number of chromosome 2. In addition, a 1.5- to 4-fold 2p24 copy number in relation to the copy number of chromosome 2 is defined as 2p24 gain, which could reflect either gain of 2p or gain of the MYCN gene. Additionally, the status of 1p36 and 11q were determined with DNA probes from Kreatech [ON1q21/SRD(1p36)] and Vysis [LSI MLL Dual Color, Break Apart Rearrangement Probe] respectively.
Statistical analysis
June 30, 2016 was chosen as the reference date for the end of data collection for purposes of statistical analysis. Comparisons between study groups with or without MYCN amplification and associations between patient pretreatment characteristics were evaluated by nonparametric tests. Event-free survival (EFS) was defined from the date of diagnosis to the date of the first event (for example, relapse or death), or the last contact with patients in continuous CR. Overall survival (OS) was defined as the time from the diagnostic date through the date of death (from any cause), or the last contact with patients in continuous CR. EFS and OS distribution with or without MYCN amplification was estimated with the Kaplan–Meier survival analysis. All tests were two-sided with a P < 0.05 considered statistically significant. SPSS 16.0 software was used for all statistical analyses.
Results
Clinical and laboratory characteristics of patients with BM metastases of NB
The criteria for diagnosis and staging adhered to the international neuroblastoma staging system (INSS). We divided these patients into four groups according to age (<12, 12–18, 18–24, >24 months). Among the 81 cases of NB metastatic to BM, there were significantly more males (63%) than females (37%) with a ratio 1.7:1.
All 81 patients had stage 4 disease. Patients were stratified into 3 risk groups (low-risk, LR; intermediate-risk, IR; high-risk, HR). MYCN amplification was seen in 13 patients (16.0%). Twenty-six patients (31.1%) had very high serum LDH levels (≥1500 IU/L), and 71 patients (87.7%) had very high serum NSE levels (≥100 UG/L).The median follow-up time was 21.4 months (range 0.5–44.0). Twenty-seven patients (33.3%) suffered relapse or died during the follow-up period. The main clinical characteristics of the 81 patients are shown in Table 1.
MYCN-status and other genetic markers of bone marrow cells by interphase FISH
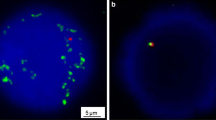
We investigated the MYCN status in all patients and amplification was seen in 13 cases (16.0%; Fig. 1). The signal copy numbers of MYCN gene were >15 copies, and the positive cells accounted for more than 80% in every case. An additional six cases (7%) displayed MYCN-gain with the signal copy numbers between 2 and 9 copies. Loss of heterozygosity (LOH) of 1p36 and 11q deletion were also analyzed in the MYCN-amplified cases by interphase FISH. Eight patients (61.5%) presented MYCN amplification and 1pLOH simultaneously; however, no 11q deletion was detected in the MYCN-amplified NB. The clinical characteristics and FISH results of 13cases are presented in Table 2.
Representative FISH images of BM cells. a The status of MYCN amplification using a dual-color probe. Green signals represent the specific probe for MYCN and red signals stand for centromeric chromosome 2 probes. MYCN signals show more than 30 copies within the nuclei. b The status of 1pLOH using a dual-color probe. Green signals represent the copy numbers at 1q21 and red signals are the specific DNA probe of 1p36. Bars 5 μm
In this study, the primary tumors of 53 patients were also detected by pathological tissue FISH, and MYCN amplification was seen in 14 cases. Only one case had a different result, with the primary tumor sample showing MYCN amplification, but the BM cell sample showing normal signals. The remaining other 42 cases showed consistent results in the two different specimens.
Impact of MYCN amplification on prognosis of NB metastatic to BM
The 3-year EFS rate of the 81 patients was 60.8 ± 7.0%, with a median follow-up of 21.4 months. To evaluate the prognostic value of MYCN gene in NB metastatic to BM, we divided the whole cohort of 81 patients into MYCN-normal and MYCN-amplification groups (68 and 13 cases, respectively). During the follow-up period, more patients suffered from relapse or died in MYCN-amplification group (8/13, 61.5%) than in the MYCN-normal group (19/68, 27.9%). Clinical outcome was poorer in patients with MYCN gene amplification than in those without amplification (3-year EFS 28.8 ± 13.1 vs. 69.7 ± 5.7%, P = 0.005; 3-year OS 41.5 ± 14.7 vs. 76.7 ± 5.5%, P = 0.005; Fig. 2).
Relationship of MYCN status to clinicobiological characteristics of NB metastatic to BM
We next assessed the associations of MYCN status at diagnosis with the clinicobiological characteristics of the 81 cases of NB metastatic to BM. We divided these patients into two groups according to the levels of MYCN. We observed a significant association between MYCN amplification and age, LDH levels as well as prognosis (P = 0.038, P < 0.001, P = 0.026). No significant correlations between MYCN amplification and gender, treatment, NSE levels, or primary site were apparent; however, we found that all 13 cases of MYCN amplification occurred in patients in the high-risk (HR) treatment group, high serum NSE levels group, and in those whose primary site was mainly in the abdomen, although the difference was not statistically significant.
In this study, MYCN amplification was found in 16% of NB metastatic to BM and was found in different proportions of children of different ages. Children younger than 1 year had the best results with no amplification found. Children older than 2 years exhibited the highest prevalence of MYCN amplification (53.8%) compared with any other group. Among patients between 18 and 24 months of age, 30.8% had MYCN amplification as opposed to 15.4% of patients between 12 and 18 months of age (Table 3).
Discussion
Amplification of the MYCN proto-oncogene is a powerful prognostic indicator of advanced stages and rapid tumor progression [15]. In our clinical practice, some patients suffered from treatment failure mainly because of incorrect risk stratification [16]. For those patients who need chemotherapy before surgery, timely assessment of the level of MYCN gene expression may not be possible due to the lack of availability of primary tumors. In addition, the results of MYCN gene of primary tumors maybe inaccurate after toxic chemotherapy, leading to insufficient dosage and period of treatment. In this study, we found interphase FISH of BM cells was reliable in detecting MYCN gene status in BM metastases of NB. In our study, MYCN amplification was present in 16.0% of patients in whom the positive cells accounted for more than 80% of BM cells, which was close to the percentage reported by other groups [17, 18]. In addition, we obtained nearly consistent results in the two different specimens including BM cells and primary tumors. Interphase FISH analysis provides a direct and rapid method. Only a small number of tumor cells are required, compared with primary tumor biopsies, and FISH is more sensitive, counting the MYCN copy number in each single cell.
A total of 81 patients with BM metastasis were enrolled in this research. The median age was 39 months (range 5–103 months) with 91.4% of patients older than 18 months. In our study, there were significantly more males (63%) than females (37%), with a ratio of 1.7:1, which is higher than the proportion reported by other groups [19]. All patients had stage 4 disease, and 92.6% of cases belonged to the HR group. This is consistent with the International Neuroblastoma Risk Group (INRG) suggestion that an age-at-diagnosis cutoff of greater than 18 months is associated with higher risk disease [20]. We found abdomen to be the most common site (90.1%); thorax was the second (7.4%), and only one NB primary was located in the epidural area, and one in the sacroiliac region.
Patient age is a clinical variable with independent prognostic value in NB [21]. In this study, the prevalence of MYCN amplification displayed obvious association with age. The prevalence reached a peak of 53.8% in patients older than 2 years, was 30.8% for those between 18 and 24 months of age, and 15.4% in patients 12–18 months of age. No amplification was found in patients younger than 1 year. These results demonstrated that in NB metastases in BM, MYCN amplification is the age-dependent variation.
We found that amplification of the MYCN oncogene was significantly correlated with poor EFS and OS in our study, which is consistent with previous findings [22]. Serum markers, such as lactic dehydrogenase (LDH), and neuron-specific enolase (NSE) were recognized as prognostic markers especially in metastatic NB [23]. In this study, we found that 76.9% (10/13) of patients with MYCN-amplification had elevated serum LDH levels, in contrast to 23.1% (3/13) of those without MYCN amplification. This difference was statistically significant (P < 0.001); however, there was no significant association between MYCN amplification and NSE levels even though all patients with MYCN amplification had high serum NSE levels. This phenomenon might reflect the fact that LDH was a better clinical prognostic marker than NSE for patients with NB metastatic to BM.
1pLOH and loss of 11q occur in approximately 25–30% of primary NB, and are both associated with poor outcome [24]. Recent studies demonstrated that MYCN is a direct target of miR-34a, which maps to the 1p36 region, and 1pLOH results in loss of miR-34a, which may lead to amplification of MYCN gene [25]; however, the correlation of MYCN and 1pLOH remains controversial among different groups [26]. In our study, 61.5% of NB with MYCN-amplification had 1pLOH suggesting that a positive relationship maybe exist. No 11q deletion was detected in the MYCN-amplified NB in this study. This was consistent with the previous finding of an inverse relationship between MYCN amplification and 11q loss [27]. Because we did not detect the two markers in the absence of MYCN amplification, we can not make a statistical analysis.
Conclusions
To date, this is the largest study of Chinese pediatric patients with NB metastatic to BM treated in a single institution. Our focus was on long-term outcomes in patients with or without MYCN amplification detected by interphase FISH of bone marrow cells. Our study demonstrated an association of MYCN amplification with poor long-term prognosis in patients with NB metastatic to BM. In our study, interphase FISH of bone marrow cells provided a direct and valid method to assess MYCN amplification and 1pLOH.
Abbreviations
- NB:
-
neuroblastoma
- FISH:
-
fluorescence in situ hybridization
- LDH:
-
lactate dehydrogenase
- NSE:
-
neuron specific enolase
- EFS:
-
event-free survival
- OS:
-
overall survival
References
Davidoff AM. Neuroblastoma. Semin Pediatr Surg. 2012;21:2–14.
Hasan MK, Nafady A, Takatori A, Kishida S, Ohira M, Suenaga Y, Hossain S, Akter J, Ogura A, Nakamura Y, Kadomatsu K, Nakagawara A. ALK is a MYCN target gene and regulates cell migration and invasion in neuroblastoma. Sci Rep. 2013;3:3450.
Brodeur GM, Bagatell R. Mechanisms of neuroblastoma regression. Nat Rev Clin Oncol. 2014;11:704–13.
Morandi F, Corrias MV, Pistoia V. Evaluation of bone marrow as a metastatic site of human neuroblastoma. Ann NY Acad Sci. 2015;1335:23–31.
Domingo-Fernandez R, Watters K, Piskareva O, Stallings RL, Bray I. The role of genetic and epigenetic alterations in neuroblastoma disease pathogenesis. Pediatr Surg Int. 2013;29:101–19.
Chaturvedi NK, McGuire TR, Coulter DW, Shukla A, McIntyre EM, Sharp JG, Joshi SS. Improved therapy for neuroblastoma using a combination approach: superior efficacy with vismodegib and topotecan. Oncotarget. 2016;7:15215–29.
Beckers A, Peer GV, Carter DR, Mets E, Althoff K, Cheung BB, et al. MYCN-targeting miRNAs are predominantly downregulated during MYCN-driven neuroblastoma tumor formation. Oncotarget. 2015;6:5204–16.
Ambros PF, Ambros IM, Brodeur GM, et al. International consensus for neuroblastoma molecular diagnostics: report from the International Neuroblastoma Risk Group (INRG) Biology Committee. Br J Cancer. 2009;100:1471–82.
Iehara T, Hosoi H, Akazawa K, et al. MYCN gene amplification is a powerful prognostic factor even in infantile neuroblastoma detected by mass screening. Br J Cancer. 2006;94:1510–5.
Jeison M, Ash S, Halevy-Berko G, et al. 2p24 gain region harboring MYCN gene compared with MYCN amplified and nonamplified neuroblastoma: biological and clinical characteristics. Am J Pathol. 2010;176:2616–25.
Suita S, Tajiri T, Kaneko M, et al. Implications of MYCN amplification in patients with stage 4 neuroblastoma who undergo intensive chemotherapy. J Pediatr Surg. 2007;42:489–93.
Villamón E, Berbegall AP, Piqueras M, et al. Genetic instability and intratumoral heterogeneity in neuroblastoma with MYCN amplification plus 11q deletion. PLoS ONE. 2013;8:e53740.
Xiaoli M, Mei J, Dawei Z, et al. Clinical features and recent treatment effect analysis of 91 neuroblastoma patients with multidisciplinary treatment. J Appl Clin Pediatr. 2013;28:178–82.
Theissen J, Boensch M, Spitz R, et al. Heterogeneity of the MYCN oncogene in neuroblastoma. Clin Cancer Res. 2009;15(6):2085–90.
Lau DT, Flemming CL, Gherardi S, et al. MYCN amplification confers enhanced folate dependence and methotrexate sensitivity in neuroblastoma. Oncotarget. 2015;6:15510–23.
Huang M, Weiss WA. Neuroblastoma and MYCN. Cold Spring Harb Perspect Med. 2013;3:a014415.
Spitz R, Hero B, Skowron M, Ernestus K, Berthold F. MYCN-status in neuroblastoma:characteristics of tumours showing amplification, gain, and non-amplification. Eur J Cancer. 2004;40:2753–9.
George RE, London WB, Cohn SL, Maris JM, Kretschmar C, Diller L, Brodeur GM, Castleberry RP, Look AP. Hyperdiploidy plus nonamplified MYCN confers a favorable prognosis in children 12–18 months old with disseminated neuroblastoma: a pediatric oncology group study. Am Soc Clin Oncol. 2005;23:6466–73.
Park SH, Kim S, Park CJ, et al. Presence of differentiating neuroblasts in bone marrow is a favorable prognostic factor for bone marrow metastatic neuroblastoma at diagnosis. Ann Lab Med. 2013;33:89–96.
Moroz V, Machin D, Faldum A, et al. Changes over three decades in outcome and the prognostic influence of age-at-diagnosis in young patients with neuroblastoma: a report from the International Neuroblastoma Risk Group Project. Eur J Cancer. 2011;47:561–71.
Müller I, Larsson K, Frenzel A, et al. Targeting of the MYCN protein with small molecule c-MYC inhibitors. PLoS ONE. 2014;9:e97285.
Bagatell R, Beck-Popovic M, Zhang Y, Pearson ADJ, Matthay KK, Monclair T, Ambros PF, Cohn SL. Significance of MYCN amplification in international neuroblastoma staging system stage 1 and 2 neuroblastoma: a report from the International Neuroblastoma Risk Group Database. J Clin Oncol. 2009;27:365–70.
Gotoh T, Hosoi H, Iehara T, et al. Prediction of MYCN Amplification in neuroblastoma using serum DNA and real-time quantitative polymerase chain reaction. J Clin Oncol. 2005;23:5205–10.
Breen CJ, O’Meara A, McDermott M, et al. Coordinate deletion of chromosome 3p and 11q in neuroblastoma detected by comparative genomic hybridization. Cancer Genet Cytogenet. 2000;120:44–9.
Wei JS, Song YK, Durinck S, et al. The MYCN oncogene is a direct target of miR-34a. Oncogene. 2008;27:5204–13.
Agostini M, Knight RA. miR-34:f rom bench to bedside. Oncotarget. 2014;5:872–81.
Fischer M, Bauer T, Oberthür A, et al. Integrated genomic profiling identifies two distinct molecular subtypes with divergent outcome in neuroblastoma with loss of chromosome 11q. Oncogene. 2010;29:865–75.
Authors’ contributions
YZX and MXL designed the study. YZX performed the experiments, collected the data, and wrote the articles. HC and XTY helped to collect the samples. LXJ, ZQ, WXS, ZW and JM recruited the patients. GC and LSG participated in the statistical analysis. MXL reviewed the final manuscript and take primary responsibility for the article. All authors read and approved the final manuscript.
Acknowledgements
This work was supported in part by: Beijing Municipal Science and Technology Commission of the capital special funding (No. Z151100004015159), Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (No. ZY201404).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The authors support the data findings be deposited in publicly available repositories (where available and appropriate).
Ethics approval and consent to participate
This research was approved by the Beijing Children’s Hospital Institutional Ethics Committee. Informed consents were obtained from the parents or guardians of each patients according to the Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yue, ZX., Huang, C., Gao, C. et al. MYCN amplification predicts poor prognosis based on interphase fluorescence in situ hybridization analysis of bone marrow cells in bone marrow metastases of neuroblastoma. Cancer Cell Int 17, 43 (2017). https://doi.org/10.1186/s12935-017-0412-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-017-0412-z