Abstract
Background
Atrial fibrillation (AF) is acknowledged as a disease continuum. Despite catheter ablation being recommended as a primary therapy for AF, the high recurrence rates have tempered the initial enthusiasm. Insulin resistance (IR) has been established as an independent predictor for the onset of AF. However, the correlation between non-insulin-based IR indices and late AF recurrence in patients undergoing radiofrequency catheter ablation remains unknown.
Methods
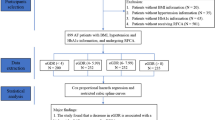
A retrospective cohort of 910 AF patients who underwent radiofrequency catheter ablation was included in the analysis. The primary endpoint was late AF recurrence during the follow-up period after a defined blank period. The relationship between non-insulin-based IR indices and the primary endpoint was assessed using multivariate Cox hazards regression models and restricted cubic splines (RCS). Additionally, the net reclassification improvement and integrated discrimination improvement index were calculated to further evaluate the additional predictive value of the four IR indices beyond established risk factors for the primary outcome.
Results
During a median follow-up period of 12.00 months, 189 patients (20.77%) experienced late AF recurrence, which was more prevalent among patients with higher levels of IR. The multivariate Cox hazards regression analysis revealed a significant association between these IR indices and late AF recurrence. Among the four indices, METS-IR provided the most significant incremental effect on the basic model for predicting late AF recurrence. Multivariable-adjusted RCS curves illustrated a nonlinear correlation between METS-IR and late AF recurrence. In subgroup analysis, METS-IR exhibited a significant correlation with late AF recurrence in patients with diabetes mellitus (HR: 1.697, 95% CI 1.397 − 2.063, P < 0.001).
Conclusion
All the four non-insulin-based IR indices were significantly associated with late AF recurrence in patients undergoing radiofrequency catheter ablation. Addressing IR could potentially serve as a viable strategy for reducing the late AF recurrence rate.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most prevalent sustained arrhythmia, and its incidence and prevalence are increasing globally, imposing a substantial burden on public health and healthcare costs [1]. AF is associated with an elevated risk of multiple adverse outcomes, including a 1.5- to 2-fold higher risk of death [2, 3], a 2.4-fold increase in the risk of stroke [3], a 1.5-fold risk of myocardial infarction [4], a 5-fold risk of heart failure [3], and a 1.5-fold raised risk of cognitive impairment or dementia [5]. Despite recent evidence supporting catheter ablation of AF as a Class 1 first-line therapy for rhythm control in appropriately selected patients [6], there is a recurrence rate of 30–40% after the procedure [7]. AF has been recognized as a disease continuum that requires a variety of strategies at the different stages, from prevention, lifestyle and risk factor modification, screening, and therapy [6]. Thus, early and optimized risk stratification to prevent recurrent AF is beneficial for patients undergoing catheter ablation.
Insulin resistance (IR), a pathological condition characterized by diminished response to insulin, is a significant precursor of diabetes mellitus (DM), hypertension, metabolic syndrome, and cardiometabolic risk [8]. Most cardiovascular risk factors have been shown to be associated with increased risk of new-onset AF and AF recurrence after catheter ablation [9, 10]. IR also has certain adverse effects on atrial electrical and structural remodeling processes, ultimately contributing to the development of AF [11, 12]. The hyperinsulinemic-euglycemic clamp has been recognized as the gold-standard method for assessing IR, its clinical use is limited by its complexity and time-consuming nature. Similarly, the homeostatic model assessment of insulin resistance (HOMA-IR), an IR index calculated using fasting insulin and fasting blood glucose (FBG), is also hindered by the need for serum insulin measurement, which may pose challenges in primary healthcare facilities, especially in developing countries, due to the high cost and lack of instrumentation [13]. Recently, several alternative measures of non-insulin-based IR indices including the TyG index, TG/HDL-C, METS-IR, and TyG-BMI index, have been established, offering greater convenience while remaining valid.
At present, the relationship between the recurrence rate after radiofrequency catheter ablation (RFCA) and non-insulin-based IR indices in AF patients has not been confirmed. Therefore, in this study, we aimed to explore the predictive value of non-insulin-based IR indices on AF recurrence in patients with varying glycemic statuses who have undergone RFCA.
Methods
Study population
This retrospective study enrolled 910 consecutive patients who underwent first-time RFCA for non-valvular AF between March 2017 and July 2023 at the Third People’s Hospital of Chengdu (Sichuan, China). The inclusion criteria were age ≥ 18 years and hospitalization for the first radiofrequency catheter ablation for non-valvular AF. The exclusion criteria were defined as follows: (1) severe cardiac valvular disease, such as severe aortic stenosis or aortic insufficiency, severe mitral valve stenosis, incomplete closure, and history of mitral valve replacement surgery; (2) previous left intra-atrial catheter ablation and left atrial surgery; (3) patients with significant liver impairment (i.e., three times the normal value); (4) malignant tumors with life expectancy of less than 1 year; (5) use of glucocorticoid drugs at baseline; and (6) patients with incomplete essential clinical data.
The study obtained approval from the Ethics Committee of the Third People’s Hospital of Chengdu and was conducted in compliance with the Helsinki Declaration. Written informed consent was obtained from all participants.
Date collection and definitions
Data on sociodemographic characteristics, medical history, smoking status, laboratory examination, and medical and procedural information of participants were collected from the electronic medical records. Previous medical history data included a history of hypertension, DM, dyslipidemia, coronary heart disease, heart failure, stroke, and chronic obstructive pulmonary disease.
Peripheral venous blood samples were collected after overnight fasting (> 8 h). Laboratory parameters, including hemoglobin, FBG, triglycerides, total cholesterol, low-density lipoprotein-C (LDL-C), high-density lipoprotein-C (HDL-C), serum creatinine, and brain natriuretic peptide (BNP), were measured by standard biochemical techniques in the Clinical Laboratory of the Third People’s Hospital of Chengdu. The left ventricular ejection fraction (LVEF) was determined by the two-dimensional modified Simpson’s method.
Patients exhibiting AF episodes lasting longer than 7 days were defined as having persistent AF, whereas individuals whose episodes terminated spontaneously within 7 days were classified as having paroxysmal AF [14]. A participant was categorized as having DM if they had a prior clinical diagnosis, were presently using medications for DM, or showed typical symptoms of DM with casual blood glucose ≥ 11.1 mmol/L, and/or FBG ≥ 7.0 mmol/L, and/or 2-h blood glucose ≥ 11.1 mmol/L in the 75-g oral glucose tolerance test [15]. The Body Mass Index (BMI) was calculated using the formula: weight / height2. TG/HDL-C was calculated using the formula: TG (mg/dL) ÷ HDL-C (mg/dL)[16]. Mets-IR was calculated using the formula: ln [(2 × FBG (mg/dL)) + TG (mg/dL)] × BMI (kg/m2)) ÷ (ln [HDL-C (mg/dL)]) [17]. The triglyceride–glucose index (TyG index) was calculated using the formula: ln [fasting TG (mg/dL) ×FBG (mg/dL)/2] [18]. TyG-BMI index was calculated using the formula: ln [fasting TG (mg/dL) × FBG (mg/dL)/2] × BMI (kg/m2) [19]. Estimated glomerular filtration rate (eGFR) was calculated using the modification of diet in renal disease (MDRD) equation: 175 × Scr– 1.234 × Age– 0.179 × 0.79 (if female) [20]. Chronic kidney disease (CKD) was defined as eGFR < 60 mL/min/1.73 m2. The study population was divided into three subgroups: Stage 1, patients with eGFR > 90 mL/min/1.73 m2 (no renal dysfunction); Stage 2 patients with eGFR between 60 and 89 mL/min/1.73 m2 (mild renal dysfunction); and Stage 3–5, patients with eGFR < 59 mL/min/1.73 m2 (moderate and severe renal dysfunction).
Ablation protocol and periprocedural management
The RFCA protocol for AF in our department has been previously reported [21]. In brief, all patients underwent cardiac computed tomography angiography prior to ablation to evaluate the size and structure of the left atrium as well as the morphology of the pulmonary veins. RFCA was performed under general anesthesia for all patients, with continuous monitoring of their vital signs. A coronary sinus electrode was placed into the left subclavian vein, and a ventricular electrode was inserted into the right femoral vein. The electrophysiological examination indicated persistent AF or paroxysmal AF.
In cases of paroxysmal AF, the adjustable curved sheath was directed to the left atrium. A pressure-sensing ablation catheter was infused with 50 watts and 15 mL/min of cold saline. Subsequently, the bilateral pulmonary vein was electrically isolated after ablation, indicating the completion of the procedure. If AF persisted, a Swarts long sheath was placed via the right femoral vein puncture through the Swarts long sheath puncture chamber interval. The adjustable sheath was placed into the pentary electrode in the left chamber. The CARTO 3 navigation system was utilized to guide the modeling of the descending left atrial anatomy, while gathering the contact bipolar cavity electrical graph signal throughout the left chamber. Following this, the left atrial matrix was mapped during sinus rhythm and AF, and the ablation circuit was designed based on these mapping results.
Ablation was performed using pressure sensing with the catheter and cold saline (50 watts, 15 mL/min), leading to the improvement of the left atrial matrix (e.g., anterior and posterior pulmonary veins, BOX). If AF transitioned to atrial flutter or atrial tachycardia during ablation, the ablation area was electro-isolated. If AF changed to sinus rhythm during ablation, the procedure was concluded.
If the patients did not have any contraindications, all patients were given oral anticoagulants and amiodarone for at least 3 months after the procedure, adhering to the guidelines of the European Society of Cardiology [14]. In instances where oral amiodarone could not maintain sinus rhythm during this period, electrocardioversion was conducted.
Outcome and follow‑up
After discharge, scheduled follow-up visits were performed at 3, 6, and 12 months. The follow-up methods included outpatient appointments with an AF specialist, readmission, and telephonic follow-up. All patients were advised to undergo a 7-day long-course ECG during regular follow-up appointments. The blank period within 90 days following RFCA was taken into account for any occurrence of atrial arrhythmia (AF, atrial flutter, or atrial tachycardia) and was not deemed as AF recurrence. Late AF recurrence was defined as all 30-second AF events (atrial arrhythmia) continuously recorded by any ECG or Holter monitoring device after the 90-day gap period [22]. The primary endpoint in this study is the late recurrence of AF during the follow-up period following the blank period.
Statistical analysis
R software (Version 4.3.2) and SPSS 26.0. were used to perform the statistical analyses. The normality of the data distribution was evaluated utilizing the Kolmogorov-Smirnov test. Continuous variables were expressed as mean with standard deviation (SD) or median with interquartile range (IQR) as appropriate, and the comparison between two groups was analyzed using the t-test or Mann–Whitney U-test as applicable. Categorical variables were displayed as frequencies and percentages, and the comparison between two groups was assessed using the chi-square test or Fisher’s exact test as appropriate.
The four IR indices were standardized using Z-scores and incorporated into the unadjusted or adjusted Cox proportion hazards regression models to assess the impact of a 1.0-SD increase in the indices on the late recurrence of AF. Before constructing the multivariate model, univariate logistic regression was performed to select the covariates. To identify the association between the four IR indexes and the late recurrence of AF in the enrolled individuals, covariates such as sex, AF type, AF history, BNP, HGB, LAD, and CKD were evaluated for collinearity prior to constructing the multivariate model based on a significance level of P < 0.05. The Cox regression model included three models according to different confounding factors. Model 1 was not adjusted any covariates. Model 2 was adjusted for sex and AF type. Model 3 was adjusted for sex, AF type, AF history, LAD, and eGFR. The relationship between TyG index, TyG-BMI, TG/HDL-C, METS-IR, and recurrence of AF was also investigated by restricted cubic spline (RCS) model with 3 knots (10th, 50th, and 90th percentiles, respectively).
The receiver operating characteristic (ROC) curves were employed to assess the predictive power of the basic model (including sex, AF type, the duration of AF, LAD, and CKD) and the basic model plus each of the four IR indices for late AF recurrence, respectively. The Kaplan–Meier method was performed to evaluate the probability of free from the primary outcome between groups according to the optimal cutoff point of the IR index and discrepancies between groups were evaluated by log-rank tests. Furthermore, the predictive performance of the addition of the IR index to the risk prediction models was assessed using the C-statistic, the continuous net reclassification improvement (NRI) and the integrated discrimination improvement (IDI). Subsequently, subgroup analyses were also carried out, stratified by DM, to evaluate the predictive capability of METS-IR across different glycemia statuses, and the P-value for interaction was calculated. A two-sided P-value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 910 AF patients (65.98 ± 10.3 years, 50.4% female) who underwent RFCA and completed the follow-up were enrolled for the final analysis (Table 1). During a median follow-up of 12.00 months (IQR, 12.00 to 15.00 months), 189 patients (20.77%) experienced late AF recurrence. Compared to patients without late AF recurrence, those with late AF recurrence tended to be male, have a higher prevalence of persistent AF, a longer duration of AF, higher levels of BMI, triglycerides, LAD, eGFR, and CHA2DS2-VASc score, as well as a lower levels of HDL-C and hemoglobin. The non-insulin-based IR indices, including the TyG index, TG/HDL-C, METS-IR, and TyG-BMI index, were higher in patients who experienced late AF recurrence.
The predictive value of the IR indices for the risk of late AF recurrence
The results of univariate and multivariate Cox proportional hazards regression analyses and predictors for late AF recurrence are presented in Table 2. After adjusting for BNP and hemoglobin, multivariate Cox proportional hazards regression showed that sex, AF type, the duration of AF, LAD, and CKD were independent predictors for late AF recurrence in AF patients after RFCA (all P < 0.05). The four IR indices were also significantly associated with late AF recurrence (P < 0.05, Table 3). After adjusting for sex, AF type, the duration of AF, LAD, and CKD, the four IR indices were still independent hazard factors for late AF recurrence. Based on the optimal cutoff value of the four IR indices, the Kaplan–Meier analysis revealed that the cumulative incidence of late AF recurrence was significantly higher in patients with a higher level of IR (log-rank test, all P < 0.01) (Fig. 1A, D).
Freedom from late AF recurrence over Time Shown are Kaplan–Meier estimates of the primary end point, freedom from recurrence of any atrial tachyarrhythmia (atrial fibrillation, atrial flutter, or atrial tachycardia) lasting 30 s or longer days after the initiation of catheter ablation in patients stratified by the optimal cutoff value of A TyG index, B TyG-BMI index, C TG/HDL ratio, and D METS-IR. HR indicates hazard ratio
We further assessed whether a linear or nonlinear association existed between the IR index and late AF recurrence using multivariate adjusted RCS. Interestingly, the TyG index and TyG-BMI exhibited a significantly linear relationship with late AF recurrence, while TG/HDL and METS-IR did not show such a relationship (Fig. 2A, D).
Restricted cubic spline curves for late AF recurrence by IR indices A TyG index; B TyG-BMI index; C TG/HDL ratio; D METS-IR. Hazard ratios are indicated by solid lines and 95% CIs by shaded areas. AF, atrial fibrillation; CI, confidence interval, TyG triglyceride and glucose, TyG-BMI triglyceride glucose-body mass index, TG/HDL-C triglyceride to high-density lipoprotein cholesterol ratio, METS-IR metabolic score for insulin resistance
Incremental effect of the IR indices on risk stratification for late AF recurrence
The area under the ROC curve (AUC) of the basic model and the basic model plus TyG index, TG/HDL-C, METS-IR, or TyG-BMI index, was 0.681, 0.694, 0.719, and 0.715, respectively (Fig. 3). The C-statistic, NRI and IDI were presented in Table 4. The results showed a significant incremental predictive ability by the four IR indices when added to the basic risk model for predicting late AF recurrence, as indicated by the IDI values (all P < 0.001). Meanwhile, among the four non-insulin-based IR indices, METS-IR exhibited the most significant incremental effect on the basic model for predicting late AF recurrence (Table 4).
The receiver operating characteristic curves of the IR indices as a marker to predict late AF recurrence. Basic model versus Basic model + TyG index, Z = 1.484, P = 0.1377; Basic model versus Basic model + TyG-BMI index, Z = 2.772, P = 0.006; Basic model versus Basic model + TG/HDL, Z = 1.948, P = 0.051; Basic model versus Basic model + METS-IR, Z = 3.045, P = 0.002
Subgroup analyses of METS-IR for predicting late AF recurrence
Next, we further performed exploratory subgroup analyses stratified by age, sex, the duration of AF, AF type, hypertension, DM, CKD, HBG, BNP, and LAD (Fig. 4). The results indicated that there was a significant interaction between age, sex, the duration of AF, AF type, CKD, HBG, BNP, or LAD subgroups and METS-IR on the incidence of late AF recurrence (all P for interaction < 0.05). Moreover, METS-IR demonstrated a significant association with late AF recurrence specifically in AF patients with DM (HR: 1.697, 95% CI 1.397 − 2.063, P < 0.001).
Subgroups analyses of METS-IR for late AF recurrence. Hazard ratios are presented as per 1.0-SD increase in the METS-IR for late AF recurrence. CI confidence interval, METS-IR metabolic score for insulin resistance, BMI body mass index, AF atrial fibrillation, PAF paroxysmal atrial fibrillation, NPAF nonparoxysmal atrial fibrillation, CKD chronic kidney disease, BNP B-type natriuretic peptide, LAD left atrial diameter
Discussion
Given the scarcity of data on evaluating the predictive value of IR indices in AF patients who underwent RFCA, we conducted the present study to investigate the association between non-insulin-based IR indices and late AF recurrence in patients undergoing RFCA. Our findings show that IR was associated with late AF recurrence in patients who underwent RFCA for AF. Even after adjusting for potential confounding factors, the four non-insulin-based IR indices remained independent predictors of late AF recurrence. To the best of our knowledge, this study demonstrates, for the first time, that incorporating the non-insulin-based IR index enhances the predictive performance of the basic model for late AF recurrence in AF patients undergoing RFCA. Our study results suggest that targeting IR may optimize the clinical management of AF patients undergoing RFCA.
In the most recent guideline, catheter ablation has become a first-line therapy for AF because of multiple RCTs and evidence from large registries [6]. Meanwhile, recurrences of AF are common following an initial ablation procedure, with rates ranging from 30 to 40% in contemporary clinical trials [23, 24]. This often results in repeated cardioversions, the use of antiarrhythmic drugs, or additional ablation procedures. Antiarrhythmic drug therapies may exhibit significant drug-drug interactions and lead to serious side effects [25]. Similarly, although complication rates associated with AF ablation are generally low, repeat ablations have been identified as an independent predictor of adverse outcomes. These risks are rare but include pulmonary vein stenosis and stiff left atrium syndrome [26,27,28]. Thus, preventing recurrent AF is beneficial for individuals undergoing catheter ablation.
AF has been recognized as a disease continuum that requires diverse strategies across various stages, encompassing prevention, lifestyle modifications, risk factor management, screening, and therapeutic interventions [6]. Notably, risk factor management has been underscored as a crucial aspect across the entirety of the disease continuum [6]. Both metabolic syndrome and DM have been established as independent risk factors, not only for the development of AF [9, 29], but also for its recurrence following RFCA [30, 31]. Meanwhile, IR is a prevalent characteristic of both metabolic syndrome and DM, and it is considered a potential mechanism contributing to the development of AF [32, 33]. Monitoring IR levels may assist in identifying individuals at increased risk of AF, thereby enabling the prompt implementation of effective interventions.
HOMA-IR, an insulin-based IR index, is the most widely used indicator for IR. Hijioka et al. reported that HOMA-IR was an independent predictor of recurrence in patients with paroxysmal AF [34]. Another study found that the HOMA-IR was independently associated with AF recurrence in patients without diabetes [35]. However, the clinical use of HOMA-IR is constrained by the necessity for serum insulin measurement, which may not be readily available in primary hospitals, especially in developing countries, due to the lack of instrumentation and reimbursement [13]. Non-insulin-based indices are typically more convenient for routine screening in clinical practice compared to the HOMA-IR index. Our study identified the non-insulin-based IR indices, namely the TyG index, TG/HDL-C ratio, METS-IR, and TyG-BMI index, as independent predictors of delayed AF recurrence in patients undergoing RFCA. Among the four non-insulin-based IR indices, the METS-IR has best incremental effect on the basic model for predicting late AF recurrence. In subgroup analysis, METS-IR was positively associated with delayed AF recurrence in DM patients, regardless of the type of AF. Interestingly, the trajectories of TyG index during the blank period were significantly associated with the outcomes of AF recurrence in AF patients who underwent RFCA [36]. Therefore, monitoring IR levels may help in identifying individuals at high risk of AF recurrence, enabling the timely implementation of effective interventions.
Although extensive clinical research has confirmed the impact of IR on the onset and recurrence of AF, the detailed pathogenesis mechanism still remains largely unknown. In animal studies, Chan et al., demonstrated that IR induced both atrial structural remodeling and abnormal intracellular calcium homeostasis, thereby contributing to an increased susceptibility to AF [12]. The recurrence rate of AF after ablation was significantly higher in the patients with metabolic syndrome [31], indicating that the atrial arrhythmogenic substrate may be a dynamic entity and a single ablation-based “substrate modification” may be insufficient for individuals with IR [37]. Notably, research has demonstrated that both metformin and dipeptidyl peptidase 4 inhibitors reduced the risk of AF in patients with DM [38, 39]. Moreover, the use of SGLT2 inhibitors in diabetic patients was associated with a decreased risk of arrhythmia recurrence following AF ablation [7]. These findings suggest that by addressing IR, these antidiabetic medications may have the potential to prevent atrial remodeling, AF onset, and AF recurrence in individuals with IR [12]. Investigating the potential contribution of IR to atrial structural remodeling and exploring the correlation between non-insulin IR indices and different echocardiography and electrophysiology parameters, including left atrial volume index, E/e’, degree of reverse remodeling post-ablation, and voltage mapping findings such as low voltage zone extent, can further enhance comprehension of the mechanisms linking IR to late recurrence of AF.
Limitations
The study has some limitations. It is a single-center, observational study with a relatively small sample size, exclusively involving the Chinese population. The interpretation of the results warrants caution and should undergo further validation through multicenter studies with larger sample sizes. Patient-triggered detection devices or implantable loop recorders were not employed in this study, potentially resulting in the oversight of asymptomatic recurrences among patients and consequently underestimating the AF recurrence rate. Although the present study adhered to the established protocols for detecting AF recurrences in China, this limitation must be noted. The parameters for IR indices were collected at baseline upon admission, potentially influenced by the use of lipid-lowering and antidiabetic medications during the follow-up period. Further investigation is necessary to determine if the trajectories of IR indices influence their predictive capabilities for the prognosis of patients with AF undergoing radiofrequency catheter ablation. Clinical trials are also needed to confirm whether improving IR can lead to favorable clinical outcomes for these patients.
Conclusion
The non-insulin-based IR indices were independent prognostic predictors of late AF recurrence after RFCA in all AF patients. After adding to the basic models, the IR indices improvs the ability of the basic models to stratify risk and predict prognosis of AF patients undergoing RFCA. METS-IR, among the four non-insulin-based IR indices, displayed the most substantial incremental effect on the basic model for predicting late AF recurrence, notably in AF patients with DM. Our findings suggest that the IR indices could serve as predictors of late AF recurrence and have the potential to influence the management and therapeutic approach. Implementation of novel therapies targeting IR improvement may contribute to the amelioration of AF and enhance clinical prognosis.
Data availability
The datasets used and/or analyzed in the study are available from the corresponding author upon reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- IR:
-
Insulin resistance
- DM:
-
Diabetes mellitus
- RFCA:
-
Radiofrequency catheter ablation
- TyG:
-
Triglyceride-glucose
- TG:
-
Triglyceride
- HDL-C:
-
High density lipoprotein-cholesterol
- FBG:
-
Fasting blood glucose
- METS-IR:
-
Metabolic score for insulin resistance
- BMI:
-
Body mass index
- LAD:
-
Left atrial diameter
- LVEF:
-
Left ventricular ejection fraction
- BNP:
-
Brain natriuretic peptide
- eGFR:
-
Estimated glomerular filtration rate
- CKD:
-
Chronic kidney disease
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the ROC curve
- NRI:
-
Continuous net reclassification improvement
- IDI:
-
Integrated discrimination improvement
References
Weng LC, Preis SR, Hulme OL, Larson MG, Choi SH, Wang B, Trinquart L, McManus DD, Staerk L, Lin H, et al. Genetic predisposition, clinical risk factor Burden, and lifetime risk of Atrial Fibrillation. Circulation. 2018;137(10):1027–38.
Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, Odutayo AA. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ. 2016;532:h7013.
Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482.
Ruddox V, Sandven I, Munkhaugen J, Skattebu J, Edvardsen T, Otterstad JE. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(14):1555–66.
Papanastasiou CA, Theochari CA, Zareifopoulos N, Arfaras-Melainis A, Giannakoulas G, Karamitsos TD, Palaiodimos L, Ntaios G, Avgerinos KI, Kapogiannis D, et al. Atrial fibrillation is Associated with cognitive impairment, all-cause dementia, vascular dementia, and Alzheimer’s Disease: a systematic review and Meta-analysis. J Gen Intern Med. 2021;36(10):3122–35.
Joglar JA, Chung MK, Armbruster AL, Benjamin EJ, Chyou JY, Cronin EM, Deswal A, Eckhardt LL, Goldberger ZD, Gopinathannair R, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation. 2024;149(1):e1–156.
Abu-Qaoud MR, Kumar A, Tarun T, Abraham S, Ahmad J, Khadke S, Husami R, Kulbak G, Sahoo S, Januzzi JL et al. Jr.: Impact of SGLT2 Inhibitors on AF Recurrence After Catheter Ablation in Patients With Type 2 Diabetes. JACC Clin Electrophysiol 2023, 9(10):2109–2118.
Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, Sowers JR. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. 2021;119:154766.
Ahn HJ, Han KD, Choi EK, Jung JH, Kwon S, Lee SR, Oh S, Lip GYH. Cumulative burden of metabolic syndrome and its components on the risk of atrial fibrillation: a nationwide population-based study. Cardiovasc Diabetol. 2021;20(1):20.
Creta A, Providência R, Adragão P, de Asmundis C, Chun J, Chierchia G, Defaye P, Schmidt B, Anselme F, Finlay M, et al. Impact of Type-2 diabetes Mellitus on the outcomes of catheter ablation of Atrial Fibrillation (European Observational Multicentre Study). Am J Cardiol. 2020;125(6):901–6.
Bohne LJ, Johnson D, Rose RA, Wilton SB, Gillis AM. The Association between Diabetes Mellitus and Atrial Fibrillation: clinical and mechanistic insights. Front Physiol. 2019;10:135.
Chan YH, Chang GJ, Lai YJ, Chen WJ, Chang SH, Hung LM, Kuo CT, Yeh YH. Atrial fibrillation and its arrhythmogenesis associated with insulin resistance. Cardiovasc Diabetol. 2019;18(1):125.
Liu L, Luo Y, Liu M, Tang C, Liu H, Feng G, Wang M, Wu J, Zhang W. Triglyceride glucose-related indexes and lipid accumulation products-reliable markers of insulin resistance in the Chinese population. Front Nutr. 2024;11:1373039.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
2. Classification and diagnosis of diabetes: standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–31.
Che B, Zhong C, Zhang R, Pu L, Zhao T, Zhang Y, Han L. Triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio as potential cardiovascular disease risk factors: an analysis of UK biobank data. Cardiovasc Diabetol. 2023;22(1):34.
Qian T, Sheng X, Shen P, Fang Y, Deng Y, Zou G. Mets-IR as a predictor of cardiovascular events in the middle-aged and elderly population and mediator role of blood lipids. Front Endocrinol (Lausanne). 2023;14:1224967.
Xiong S, Chen Q, Long Y, Su H, Luo Y, Liu H, Chen Y, Feng Q, Peng X, Jiang M, et al. Association of the triglyceride-glucose index with coronary artery disease complexity in patients with acute coronary syndrome. Cardiovasc Diabetol. 2023;22(1):56.
Cheng Y, Fang Z, Zhang X, Wen Y, Lu J, He S, Xu B. Association between triglyceride glucose-body mass index and cardiovascular outcomes in patients undergoing percutaneous coronary intervention: a retrospective study. Cardiovasc Diabetol. 2023;22(1):75.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, Xu JS, Huang SM, Wang LN, Huang W, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–44.
Luo Y, Tang Y, Huang W, Xiong S, Long Y, Liu H. Age, creatinine, and ejection fraction (ACEF) score as predictive values for late non-valvular atrial fibrillation recurrence after radiofrequency ablation. Clin Exp Hypertens. 2023;45(1):2207784.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Heart Rhythm. 2017;14(10):e445–94.
Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE, Noseworthy PA, Rosenberg YD, Jeffries N, Mitchell LB, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and Cardiac arrest among patients with Atrial Fibrillation: the CABANA Randomized Clinical Trial. JAMA. 2019;321(13):1261–74.
Kuck KH, Fürnkranz A, Chun KR, Metzner A, Ouyang F, Schlüter M, Elvan A, Lim HW, Kueffer FJ, Arentz T, et al. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur Heart J. 2016;37(38):2858–65.
Konieczny KM, Dorian P. Clinically important drug-drug interactions between antiarrhythmic drugs and anticoagulants. J Innov Card Rhythm Manag. 2019;10(3):3552–9.
Reddy YNV, El Sabbagh A, Packer D, Nishimura RA. Evaluation of shortness of breath after atrial fibrillation ablation-Is there a stiff left atrium? Heart Rhythm. 2018;15(6):930–5.
Szegedi N, Széplaki G, Herczeg S, Tahin T, Salló Z, Nagy VK, Osztheimer I, Özcan EE, Merkely B, Gellér L. Repeat procedure is a new independent predictor of complications of atrial fibrillation ablation. Europace. 2019;21(5):732–7.
Schoene K, Sepehri Shamloo A, Sommer P, Jahnke C, Paetsch I, Hindricks G, Arya A. Natural course of acquired pulmonary vein stenosis after radiofrequency ablation for atrial fibrillation-Is routine follow-up imaging indicated or not? J Cardiovasc Electrophysiol. 2019;30(10):1786–91.
Norhammar A, Bodegård J, Nyström T, Thuresson M, Eriksson JW, Nathanson D. Incidence, prevalence and mortality of type 2 diabetes requiring glucose-lowering treatment, and associated risks of cardiovascular complications: a nationwide study in Sweden, 2006–2013. Diabetologia. 2016;59(8):1692–701.
Wang A, Truong T, Black-Maier E, Green C, Campbell KB, Barnett AS, Febre J, Loring Z, Al-Khatib SM, Atwater BD, et al. Catheter ablation of atrial fibrillation in patients with diabetes mellitus. Heart Rhythm O. 2020;2(3):180–8.
Mohanty S, Mohanty P, Di Biase L, Bai R, Pump A, Santangeli P, Burkhardt D, Gallinghouse JG, Horton R, Sanchez JE, et al. Impact of metabolic syndrome on procedural outcomes in patients with atrial fibrillation undergoing catheter ablation. J Am Coll Cardiol. 2012;59(14):1295–301.
Lee Y, Cha SJ, Park JH, Shin JH, Lim YH, Park HC, Shin J, Kim CK, Park JK. Association between insulin resistance and risk of atrial fibrillation in non-diabetics. Eur J Prev Cardiol. 2020;27(18):1934–41.
Azarboo A, Behnoush AH, Vaziri Z, Daneshvar MS, Taghvaei A, Jalali A, Cannavo A, Khalaji A. Assessing the association between triglyceride-glucose index and atrial fibrillation: a systematic review and meta-analysis. Eur J Med Res. 2024;29(1):118.
Hijioka N, Kamioka M, Matsumoto Y, Nodera M, Yamada S, Kaneshiro T, Yoshihisa A, Ishida T, Takeishi Y. Clinical impact of insulin resistance on pulmonary vein isolation outcome in patients with paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2019;30(4):479–86.
Wang Z, Wang YJ, Liu ZY, Li Q, Kong YW, Chen YW, Sun YH, Dong JZ. Effect of insulin resistance on recurrence after Radiofrequency catheter ablation in patients with Atrial Fibrillation. Cardiovasc Drugs Ther. 2023;37(4):705–13.
Jia S, Yin Y, Mou X, Zheng J, Li Z, Hu T, Zhao J, Lin J, Song J, Cheng F, et al. Association between triglyceride-glucose index trajectories and radiofrequency ablation outcomes in patients with stage 3D atrial fibrillation. Cardiovasc Diabetol. 2024;23(1):121.
Asirvatham SJ, Jiao Z. What causes atrial fibrillation and why do we fail with ablation? Insights from metabolic syndrome. J Am Coll Cardiol. 2012;59(14):1302–3.
Chang SH, Wu LS, Chiou MJ, Liu JR, Yu KH, Kuo CF, Wen MS, Chen WJ, Yeh YH, See LC. Association of metformin with lower atrial fibrillation risk among patients with type 2 diabetes mellitus: a population-based dynamic cohort and in vitro studies. Cardiovasc Diabetol. 2014;13:123.
Chang CY, Yeh YH, Chan YH, Liu JR, Chang SH, Lee HF, Wu LS, Yen KC, Kuo CT, See LC. Dipeptidyl peptidase-4 inhibitor decreases the risk of atrial fibrillation in patients with type 2 diabetes: a nationwide cohort study in Taiwan. Cardiovasc Diabetol. 2017;16(1):159.
Funding
This study was supported by the grant from the Scientific Research Project of The Third People’s Hospital of Chengdu (CSY-YN-01-2023-041), the Science and Technology Department of Sichuan (2024NSFSC1709), the National Natural Science Foundation of China (31600942), Liu Hanxiong Famous Doctor Studio of Chengdu (20240216), and the Project of Chengdu Medical Research (2023129, 2023016).
Author information
Authors and Affiliations
Contributions
YL, DL, and GY were major contributors in the collection, analysis and interpretation of data. WH, YT, BX, GH, YY, JH, and HS collected the patient data, and were major contributors in the management of follow-up. LC put forward constructive comments and suggestions. ZZ and HL revised the manuscript for important intellectual content. SX designed the study, drafted the manuscript, and finally approved the manuscript submitted. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approve by the ethics committee of the Third People’s Hospital of Chengdu and strictly complied with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luo, Y., Luo, D., Yang, G. et al. The effect of non-insulin-based insulin resistance indices on the prediction of recurrence in patients with atrial fibrillation undergoing radiofrequency catheter ablation. Cardiovasc Diabetol 23, 291 (2024). https://doi.org/10.1186/s12933-024-02388-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02388-8