Abstract
Background
Type 2 diabetes (T2D) patients have an increased risk of heart failure (HF). There are limited data on the association between HF and T2D in specific healthcare settings. This study sought to analyse the prevalence and incidence of HF in a contemporary cohort of T2D patients attending cardiology and endocrinology outpatient clinics.
Methods
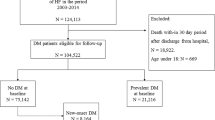
We conducted an observational multicentre prospective study (DIABET-IC) that enrolled patients with a T2D diagnosis attending cardiology and endocrinology outpatient clinics in 30 centres in Spain between 2018 and 2019. The prevalence at the start of the study and the incidence of HF after a 3 year follow-up were calculated. HF was defined as the presence of typical symptoms and either: a) LVEF < 40%; or b) LVEF ≥ 40% with elevated natriuretic peptides and echocardiographic abnormalities.
Results
A total of 1249 T2D patients were included in the present analysis (67.6 ± 10.1 years, 31.7% female). HF was present in 490 participants at baseline (prevalence 39.2%), 150 (30.6%) of whom had a preserved ejection fraction. The presence of adverse social determinants and chronic conditions such as chronic kidney disease and atherosclerotic cardiovascular disease were more frequent in HF patients. During the study period, there were 58 new diagnoses of HF (incidence 7.6%) among those without baseline HF. The incidence rate was 3.0 per 100 person-years. Independent predictors of incident HF were smoking, left ventricular ejection fraction, NT-ProBNP, history of tachyarrhythmia and treatment with pioglitazone, oral anticoagulants, or diuretics. Despite an average suboptimal glycaemic control, the use of antidiabetic drugs with cardiovascular benefits was low (30.4% for sodium-glucose cotransporter-2 inhibitors and 12.5% for glucagon-like peptide-1 receptor agonists).
Conclusions
In this contemporary cohort of T2D patients attending cardiology and endocrinology outpatient clinics, the prevalence and incidence of HF were high, comorbidities were frequent, and the use of antidiabetic agents with cardiovascular benefit was low. Outpatient care seems to be a unique opportunity for a comprehensive T2D approach that encompasses HF prevention, diagnosis, and treatment.
Graphical Abstract

Similar content being viewed by others
Background
Heart failure (HF) is a major health problem that affects more than 50 million people worldwide, constituting a main cause of quality-of-life impairment and disability for individuals, and a major economic problem for health systems [1]. Up to 2% of healthcare budgets are allocated to HF, with most of the costs attributed to hospitalisation [2, 3]. The prevalence of HF and related hospitalisations has increased over the last decade, and this trend is expected to exacerbate because of the ageing population, posing a challenge for healthcare services [4]. Thus, adequate allocation of healthcare resources and the implementation of policies aimed at the prevention and early diagnosis of this condition are of utmost importance.
Type 2 diabetes (T2D) is a growing pandemic estimated to affect up to 529 million individuals globally, with a substantial impact on healthcare costs and patient morbimortality and quality of life [5, 6]. Although cardiovascular disease prevention and management of patients with T2D have traditionally focused on atherosclerotic cardiovascular disease, the bidirectional relationship between T2D and HF is receiving growing attention in light of the favourable effects of novel antidiabetic drugs on HF-related outcomes and quality of life [7,8,9,10]. Patients with T2D have 2 to 5 increased risks of HF and the prevalence of HF in these patients is reported to be up to 22% [11,12,13]. However, this association might be even greater under active surveillance using contemporary tools and updated diagnostic criteria for HF that enable diagnosis at initial stages.
The purpose of this study was to assess the prevalence and incidence of HF in a nationwide multicentre prospective cohort of T2D patients using contemporary diagnostic methods. Second, we aimed to describe the characteristics and predictors of incident HF in these patients.
Methods
Study design and setting
The DIABET-IC study is a multicentre, observational, and prospective cohort study carried out in 30 centres in Spain and promoted by the Spanish Society of Cardiology and the Spanish Society of Diabetes. The main aim was to evaluate the prevalence and incidence of HF in T2D patients visiting cardiology and endocrinology outpatient clinics in Spain. The baseline data of the cohort and sex-differences at presentation have been reported previously [14]. Enrolment of the study participants occurred between 2018 and 2019 and the follow-up time was 3 years. Recruitment was limited to the first 20 patients with a T2D diagnosis attending a designated cardiologist and endocrinologist clinics at each participating centre. Written informed consent was obtained from all the participants. The protocol was approved by the Clinical Research Ethics Committee of the University Hospital of Toledo (identification number 243) and the study was conducted in accordance with institutional and Good Clinical Practice guidelines. The current work follows the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines for reporting observational studies [15].
Participants
Consecutive patients who attended cardiology and endocrinology outpatient clinics were considered eligible if they were aged 18 years or older and had a diagnosis of T2D at least one year prior to enrolment. The exclusion criteria were negative or inability to provide informed consent, end-stage chronic kidney disease, life expectancy inferior to three years due to cancer or other severe conditions and participation in an ongoing clinical trial. During the study design, it was expected that approximately half of the patients would be recruited from cardiology departments and the other half from endocrinology departments. However, due to slightly lower recruitment rates in the former, the final percentages were 61.9% and 38.1%, respectively.
The baseline visit consisted of a detailed medical history, physical examination, electrocardiogram, 2-dimensional echocardiography, and laboratory tests including N-terminal pro-B-type natriuretic peptide (NT-ProBNP) and glycosylated haemoglobin (HbA1c). After inclusion, periodic follow-up with at least a planned annual visit for 3 years was conducted. If HF was suspected by an endocrinologist, the cardiologist of that centre was responsible for making the definitive diagnosis and monitoring the confirmed cases throughout the study. The detailed criteria for HF diagnosis are specified in the next apart. All the participants received standard of care and enrolment did not imply additional interventions deviating from the routine practice management and treatment of HF and T2D.
Variables, data sources and measurement
The following categories of variables were collected: demographic, comorbidities, HF and T2D treatment, echocardiographic and laboratory. T2D was defined according to the 2018 American Diabetes Association criteria [16]. HF was defined as the presence of a documented hospitalisation with a main diagnosis of HF during the previous year or the fulfilment of the 2016 European Society of Cardiology guidelines criteria for HF [17]. In brief, a HF diagnosis required the presence of typical symptoms plus additional echocardiographic and NT-proBNP abnormalities. For patients with HF with reduced ejection fraction (HFrEF), the presence of symptoms and a LVEF < 40% was enough. For patients with HF with mid-range ejection fraction HFmrEF (LVEF 40–49%) and HF with preserved ejection fraction HFpEF (LVEF ≥ 50%), both elevated levels of natriuretic peptides (NT-proBNP > 125 pg/mL) and functional (diastolic dysfunction) or structural (left ventricular hypertrophy or left atrial enlargement) abnormalities on echocardiogram were required. The HF diagnosis was confirmed in all cases by the reference cardiologist. Hypertension was defined as confirmed systolic blood pressure ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or use of antihypertensive medications. Dyslipidaemia was defined as use of lipid-lowering medications or total cholesterol levels > 240 mg/dl and/or LDL cholesterol > 160 mg/dl and/or triglycerides > 200 mg/dl and/or HDL cholesterol < 40 mg/dl in males or < 50 mg/dl in females. Chronic kidney disease was defined as a defined as the presence of an estimated glomerular filtration rate less than 60 ml/min /1.73 m2. Coronary artery disease was defined as documentation of acute myocardial infarction, acute coronary syndrome, coronary revascularization, or coronary stenosis > 50%. Peripheral artery disease was defined as the presence of lower extremity arteriopathy. Cerebrovascular disease was defined as documentation of ischemic or haemorrhagic stroke or carotid stenosis > 50%.
Study size
A sample size of 1510 participants was calculated in the initial protocol. This calculation was based on the primary study hypothesis that the prevalence of HF in a contemporary cohort of T2D patients visiting cardiology and endocrinology outpatient clinics is significantly higher than previously reported rates. To ensure adequate power to detect an estimated prevalence rate of 30% at baseline and an incidence rate of 3% over a 3 year follow-up period, we made the following assumptions: a confidence level of 95%, a precision of 3%, and an anticipated loss to follow-up rate of 15%.
Statistical methods
Categorical variables are presented as counts (percentages) and continuous variables are summarized as mean ± standard deviation or median (interquartile range) according to their distribution. Normality was assessed using the Shapiro–Wilk test and QQ plots. Between-group comparisons were performed using the chi-square test for categorical data and Student’s t-test or Wilkoxon rank-sum test for continuous data. Multivariable Cox regression was used to determine significant predictors for incident HF. The Cox model was built using backward stepwise elimination, initially including clinically relevant variables and those with a p < 0.100 in the univariable models. The proportional hazards assumption was assessed using Schoenfeld residuals. For all tests, a two-sided p < 0.05 was considered significant.
Results
Study population
A total of 1517 T2D patients attending cardiology and endocrinology outpatient clinics at 30 Spanish centres were enrolled between January 2018 and December 2019. Of them, 1249 patients with available follow-up data were included in the current analyses. The mean age was 67.6 ± 10.1 years and 31.7% were women. The mean duration of T2D was 6.8 ± 10.0 years. The prevalence of comorbidities other than T2D was high: hypertension (81.3%), dyslipidaemia (81.3%), chronic kidney disease (CKD) (23.5%), atrial fibrillation (AF) (23.0%), coronary artery disease (43.0%), peripheral artery disease (10.8%), cerebrovascular disease (8.2%), and obesity (47.6%). Most of the patients received metformin (73.6%) and one in three were treated with insulin. The prescription of antidiabetic drugs with direct cardiovascular benefits was low, with 30.4% of the participants receiving sodium-glucose cotransporter-2 (SGLT2) inhibitors and only 12.5% receiving glucagon-like peptide-1 (GLP-1) receptor agonists (Fig. 1). Half of the patients received diuretic treatment (51.4%).
Prevalence of heart failure and comparison of the characteristics between HF and non-HF patients at the initial visit
The prevalence of HF at the initial visit was 39.2% (490 patients). Of these, 246 (50.2%) had HFrEF, 94 (19.2%) had HFmrEF, and 150 (30.6%) had a HFpEF. Of the 490 prevalent HF cases, 315 (64.3%) had a prior HF hospitalisation. There were 22 newly HF cases discovered through systematic screening at baseline: 5 (22.7%) with HFrEF, 6 (27.2%) with HFmrEF, and 11 (50%) with HFpEF. The characteristics of the participants grouped according to HF diagnosis at the initial visit are shown in Table 1. There were no sex differences between the groups. Conversely, HF patients were older, had lower levels of education, were less likely to be active workers, and were less frequently living with a partner. T2D complications such as diabetic nephropathy and diabetic foot were more frequent among HF patients. In half of the participants, HbA1c levels were above the recommended target: 7.0 (6.3–7.8) and 7.2 (6.5–7.9) %, in HF and non-HF patients, respectively (p = 0.073). There were significant differences in the burden of comorbidities between the two groups. Chronic obstructive pulmonary disease, sleep apnoea, CKD, peripheral artery disease, cerebrovascular disease, coronary heart disease and AF were more prevalent in the HF group. The average body mass index was high in both groups: 30.1 ± 5.6 vs. 30.2 ± 5.5 in HF and non-HF patients, respectively (p = 0.609). Among the laboratory results, c-LDL levels were slightly lower in the HF group, but these participants presented a more adverse lipid profile reflected by a higher triglyceride/c-HDL ratio (3.2 [2.3–4.9] vs. 2.9 [1.9–4.6], p < 0.001). NT-ProBNP levels were obviously higher in the HF group (784 [289–2090] vs 132[60–306] pg/mL, p < 0.001). With respect to the electrocardiogram findings, AF, pacemaker rhythm, and left bundle branch block were more frequent in the HF group. Conversely, right bundle branch block was more frequently reported among non-HF participants.
Incidence of heart failure and comparison of the characteristics between HF patients and non-HF patients at follow-up
After a 3-year follow-up, new-onset HF was diagnosed in 58 of the 759 participants with no HF at baseline, resulting in an incidence of 7.6% and an incidence rate of 3.0 per 100 person-years. Of these, 14 (24.1%) were HFrEF, 17 (29.3%) were HFmrEF, and 27 (46.6%) HFpEF. The baseline characteristics of the participants, according to the occurrence of HF at follow-up and excluding those patients with HF at the initial visit, are shown in Table 2. In the unadjusted analysis, incident HF was not associated with age or sex but was more frequent in patients with lower education levels. Hypertension, CKD, and atherosclerotic cardiovascular diseases were not associated with incident HF. Conversely, a history of tachyarrhythmia was a predictor of HF. With respect to laboratory data, incident HF patients had higher baseline NT-ProBNP levels [220 (87–709) vs. 126 (56–296) pg/mL, p = 0.015) but comparable levels of HbA1c. In the Cox adjusted analysis, the significant predictors of incident HF were smoking, LVEF, NT-ProBNP, prior tachyarrhythmia and treatment with pioglitazone, oral anticoagulants, or diuretics (Table 3).
Clinical events
After a mean follow-up period of 2.6 years, 122 deaths were reported. Of these, 46 were attributed to cardiovascular causes: HF (n = 26), acute coronary syndrome (n = 6), stroke (n = 10), and sudden cardiac death (n = 4). HF hospitalization occurred in 30 patients. No patients received advanced heart failure therapies such as heart transplantation or left ventricular assist devices.
Discussion
In this contemporary cohort of T2D patients visiting cardiology and endocrinology outpatient clinics in Spain, the main findings were as follows: (1) the prevalence and incidence of HF were high; (2) certain features were associated with prevalent and incident HF; and (3) the prescription of antidiabetic drugs with cardiovascular benefits was low despite suboptimal metabolic control.
This study extends the literature on the association between HF and T2D. In the Framingham study, the incidence rate of HF in T2D participants was 7.6 per 1000 person-years for men and 11.4 per 1000 person-years for women, which was 1.8 and 3.8 times higher than for their non T2D counterparts [12]. Other observational studies have confirmed this association and linked T2D to structural and functional cardiac abnormalities, such as increased left ventricular mass, left atrial enlargement, and impaired left ventricular systolic or diastolic function [18,19,20]. Overall, the strength of the association between HF and T2D seems to be strongly influenced by the characteristics of the analysed population, with greater risks of HF reported in those studies including elderly populations and coronary artery disease patients [21, 22]. In this regard, we found a remarkably high prevalence (39.2% at the initial visit) and incidence rate of HF (3.0 per 100 person-years) in this cohort of cardiology and endocrinology outpatient attendees, providing a solid foundation for the opportunistic screening of HF in this setting, in which HF prevalence seems particularly high. Boonman-de Winter et al. reported a prevalence of HF of 27.7% using an active comprehensive search of HF in T2D patients that also included echocardiography and natriuretic peptides assessment [23]. The slightly lower prevalence found in this study might be explained by the different characteristics of the included cohort, that was representative of a general population of T2D patients, with a lower burden of comorbidities such as coronary artery disease or CKD. In addition to age, we found an association between HF and certain disadvantageous socioeconomic factors such as a low level of education and unemployment. These adverse determinants have been previously associated with both T2D and HF, leading to an increased risk of HF, higher mortality rates and lower access to HF therapies [24,25,26,27]. The coexistence of these factors with cardiac and noncardiac comorbidities such as AF, hypertension, atherosclerotic cardiovascular disease, obesity, or CKD, should prompt clinicians to consider an underlying HF diagnosis in T2D patients [28]. In this respect, we observed a greater burden of comorbidities among HF patients in this contemporary cohort of T2D patients, highlighting the importance of a multifactorial and holistic management of these individuals. To our knowledge, there are no Spanish nationwide population-based studies detailing the characteristics of T2D patients with HF of Spain. Escobar et al. characterized a population of 21,851 HF patients from 7 regions in Spain, of whom 7371 had a T2D diagnosis [29]. The population included in the study was older (mean age 77.4 ± 10.3), with a higher proportion of women (45.4%) and a lower prevalence of coronary heart disease, which is consistent with the different healthcare setting, that not only included hospitals but also community health centres. Despite the different contexts, It should be noted than the burden of non-cardiac comorbidities was also high in this population, with 37.3% of the patients presenting CKD and 20.4% chronic obstructive pulmonary disease. In this regard, the inclusion of patients with end-stage kidney disease in this study, might have resulted in even higher rates of HF owing to the close association between the two conditions.
Despite the presence of a broad spectrum of comorbidities, NT-ProBNP has been proven to predict the risk of HF and mortality in T2D patients and is a widely available and useful tool for the early diagnosis of HF [30, 31]. In a recent consensus document of the Heart Failure Association of the European Society of Cardiology, an age-adjusted NT-ProBNP based algorithm for the diagnosis of HF in asymptomatic T2D patients was proposed [32]. In our study, we found that more than half of the patients with no baseline HF had NT-ProBNP levels greater than 125 pg/mL at the initial visit. These patients had a twofold higher risk of incident HF at 3 years. It should be acknowledged that the use of NT-ProBNP is limited in obese patients, in whom HF diagnosis might be particularly challenging due to the masking of HF related signs and symptoms [33].
Over the last decade, we have witnessed significant advancements in the pharmacological armamentarium for T2D that have led to a person-centred treatment approach that focuses not only on achieving glycaemic goals, but also on preventing and treating cardiovascular and renal comorbidities [34]. Specifically, SGLT2 inhibitors have been demonstrated to reduce the risk of heart failure hospitalization, kidney disease progression and mortality in T2D patients [35,36,37]. Despite the proven cardiovascular benefits of SGLT2 inhibitors and GLP-1 receptor agonists, the implementation of these therapies in our study was low, which probably explains the lack of cardioprotective effect. Less than one third of the participants receiving sodium-glucose SGLT2 inhibitors and only one in eight receiving GLP-1 receptor agonists, which might be partly related to the year of enrolment but also to other factors such as therapeutic inertia or cost containment policies on pharmaceutical expenditure within the Spanish Public Health System [38]. The gap between the benefits and the low use of these therapies in daily practice has been reported in other recent nationwide registries [39, 40]. In aggregate, the high rates of HF and the low implementation of antidiabetic drugs with cardiovascular benefits found in this cohort of T2D patients, reveal a widely untapped opportunity for HF screening, prevention, and early initiation of treatment in T2D patients visiting cardiology and endocrinology outpatient clinics.
There are several limitations of this study that should be noted. First, clinicians and high-volume hospitals willing to provide the best care for patients presenting the two conditions might be overrepresented, potentially leading to selection bias. Second, these results may not be generalizable to T2D patients in other countries with different health policies or to contemporary patients in Spain. Since the cohort was enrolled a few years ago, the implementation of T2D drugs with cardiovascular benefits was low. Higher prescription rates of these drugs might have modified our findings. Last, the outbreak of the COVID-19 pandemic during the study period reduced the number of planned visits and influenced HF admission patterns [41, 42].
Conclusion
In this contemporary cohort of T2D patients attending cardiology and endocrinology outpatient clinics, the prevalence and incidence of HF were markedly elevated. HF was associated with unfavourable social determinants of health and additional comorbidities, particularly cardiometabolic diseases. The use of antidiabetic drugs with cardiovascular benefits was limited. Thus, outpatient cardiology and endocrinology care represent a unique opportunity for a comprehensive T2D approach that includes the diagnosis, prevention, and treatment of HF.
Availability of data and materials
The dataset analysed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- CKD:
-
Chronic kidney disease
- GLP1:
-
Glucagon-like peptide-1
- HF:
-
Heart failure
- LVEF:
-
Left ventricular ejection fraction
- NT-ProBNP:
-
N-terminal pro-B-type natriuretic peptide
- SGLT2:
-
Sodium-glucose cotransporter-2
- T2D:
-
Type 2 diabetes
References
Yan T, Zhu S, Yin X, et al. Trends burden inequalities of heart failure globally 1990 to 2019: a secondary analysis based on the global burden of disease 2019 study. J Am Heart Assoc. 2023. https://doi.org/10.1161/JAHA.122.027852.
Bhatnagar R, Fonarow GC, Heidenreich PA, Ziaeian B. Expenditure on Heart Failure in the United States: the medical expenditure panel survey 2009–2018. JACC Heart Fail. 2022;10(8):571–80. https://doi.org/10.1016/j.jchf.2022.05.006.
Lesyuk W, Kriza C, Kolominsky-Rabas P. Cost-of-illness studies in heart failure: a systematic review 2004–2016. BMC Cardiovasc Disord. 2018;18(1):1–11. https://doi.org/10.1186/S12872-018-0815-3/TABLES/7.
Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. 2020. https://doi.org/10.21037/amj.2020.03.03.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al KJ. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107. https://doi.org/10.2991/JEGH.K.191028.001.
Ong KL, Stafford LK, McLaughlin SA, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023;402(10397):203–34. https://doi.org/10.1016/S0140-6736(23)01301-6.
Vaduganathan M, Docherty KF, Claggett BL, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet. 2022;400(10354):757–67. https://doi.org/10.1016/S0140-6736(22)01429-5.
Davies MJ, Drexel H, Jornayvaz FR, Pataky Z, Seferović PM, Wanner C. Cardiovascular outcomes trials: a paradigm shift in the current management of type 2 diabetes. Cardiovasc Diabetol. 2022. https://doi.org/10.1186/S12933-022-01575-9.
Naito R, Kasai T. Coronary artery disease in type 2 diabetes mellitus: Recent treatment strategies and future perspectives. World J Cardiol. 2015;7(3):119. https://doi.org/10.4330/WJC.V7.I3.119.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018. https://doi.org/10.1186/S12933-018-0728-6.
Dunlay SM, Givertz MM, Aguilar D, et al. Type 2 diabetes mellitus and heart failure, a scientific statement from the American Heart Association and Heart Failure Society of America. J Card Fail. 2019;25(8):584–619. https://doi.org/10.1016/J.CARDFAIL.2019.05.007.
Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974;34(1):29–34. https://doi.org/10.1016/0002-9149(74)90089-7.
Pandey A, Khan MS, Patel KV, Bhatt DL, Verma S. Predicting and preventing heart failure in type 2 diabetes. Lancet Diabetes Endocrinol. 2023;11(8):607–24. https://doi.org/10.1016/S2213-8587(23)00128-6.
Rodríguez-Padial L, Pérez A, Sánchez MA, Barrios V, Orna JAG, Muñiz J. Characteristics of women with type 2 diabetes and heart failure in Spain. The DIABET-IC study Cardiol J. 2024;31(1):103–10. https://doi.org/10.5603/CJ.A2023.0016.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13–27. https://doi.org/10.2337/DC18-S002.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200m. https://doi.org/10.1093/EURHEARTJ/EHW128.
Ritchie RH, Abel ED. Basic mechanisms of diabetic heart disease. Circ Res. 2020;126(11):1501–25. https://doi.org/10.1161/CIRCRESAHA.120.315913.
Wang Y, Yang H, Huynh Q, Nolan M, Negishi K, Marwick TH. Diagnosis of nonischemic stage B heart failure in type 2 diabetes mellitus: optimal parameters for prediction of heart failure. JACC Cardiovasc Imaging. 2018;11(10):1390–400. https://doi.org/10.1016/J.JCMG.2018.03.015.
Somaratne JB, Whalley GA, Poppe KK, et al. Screening for left ventricular hypertrophy in patients with type 2 diabetes mellitus in the community. Cardiovasc Diabetol. 2011. https://doi.org/10.1186/1475-2840-10-29.
Gottdiener JS, Arnold AM, Aurigemma GP, et al. Predictors of congestive heart failure in the elderly: the cardiovascular health study. J Am Coll Cardiol. 2000;35(6):1628–37. https://doi.org/10.1016/S0735-1097(00)00582-9.
Van Melle JP, Bot M, De Jonge P, De Boer RA, Van Veldhuisen DJ, Whooley MA. Diabetes, glycemic control, and new-onset heart failure in patients with stable coronary artery disease: data from the heart and soul study. Diabetes Care. 2010;33(9):2084–9. https://doi.org/10.2337/DC10-0286.
Boonman-De Winter LJM, Rutten FH, Cramer MJM, et al. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia. 2012;55(8):2154–62. https://doi.org/10.1007/S00125-012-2579-0.
Connolly V, Unwin N, Sherriff P, Bilous R, Kelly W. Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Community Health. 2000;54(3):173–7. https://doi.org/10.1136/JECH.54.3.173.
Ohlsson A, Eckerdal N, Lindahl B, Hanning M, Westerling R. Non-employment and low educational level as risk factors for inequitable treatment and mortality in heart failure: a population-based cohort study of register data. BMC Public Health. 2021. https://doi.org/10.1186/S12889-021-10919-1.
Witte KK, Patel PA, Walker AMN, et al. Socioeconomic deprivation and mode-specific outcomes in patients with chronic heart failure. Heart. 2018;104(12):993–8. https://doi.org/10.1136/HEARTJNL-2017-312539.
Lawson CA, Zaccardi F, Squire I, et al. 20-year trends in cause-specific heart failure outcomes by sex, socioeconomic status, and place of diagnosis: a population-based study. Lancet Public Health. 2019;4(8):e406–20. https://doi.org/10.1016/S2468-2667(19)30108-2.
Loosen SH, Roderburg C, Curth O, et al. The spectrum of comorbidities at the initial diagnosis of heart failure a case control study. Sci Rep. 2022. https://doi.org/10.1038/S41598-022-06618-5.
Escobar C, Varela L, Palacios B, et al. Clinical characteristics, management, and one-year risk of complications among patients with heart failure with and without type 2 diabetes in Spain. Rev Clin Esp. 2022;222(4):195–204. https://doi.org/10.1016/J.RCENG.2021.04.005.
Nambi V, Ballantyne CM, Hoogeveen RC, et al. Natriuretic peptides and integrated risk assessment for cardiovascular disease: an individual-participant-data meta-analysis. Lancet Diabetes Endocrinol. 2016;4(10):840–9. https://doi.org/10.1016/S2213-8587(16)30196-6.
Scirica BM, Bhatt DL, Braunwald E, et al. Prognostic implications of biomarker assessments in patients with type 2 diabetes at high cardiovascular risk: a secondary analysis of a randomized clinical trial. JAMA Cardiol. 2016;1(9):989–98. https://doi.org/10.1001/JAMACARDIO.2016.3030.
Bayes-Genis A, Docherty KF, Petrie MC, et al. Practical algorithms for early diagnosis of heart failure and heart stress using NT-proBNP: a clinical consensus statement from the Heart Failure Association of the ESC. Eur J Heart Fail. 2023;25(11):1891–8. https://doi.org/10.1002/EJHF.3036.
Obokata M, Reddy YNV, Melenovsky V, Sorimachi H, Jarolim P, Borlaug BA. Uncoupling between intravascular and distending pressures leads to underestimation of circulatory congestion in obesity. Eur J Heart Fail. 2022;24(2):353–61. https://doi.org/10.1002/EJHF.2377.
Pharmacologic Approaches to Glycemic Treatment. Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S158–78. https://doi.org/10.2337/DC24-S009.
Arnott C, Li Q, Kang A, et al. Sodium-glucose cotransporter 2 inhibition for the prevention of cardiovascular events in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. J Am Heart Assoc. 2020. https://doi.org/10.1161/JAHA.119.014908.
Baigent C, Emberson JR, Haynes R, et al. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Lancet. 2022;400(10365):1788–801. https://doi.org/10.1016/S0140-6736(22)02074-8.
Martín E, López-Aguilera J, González-Manzanares R, et al. Impact of canagliflozin in patients with type 2 diabetes after hospitalization for acute heart failure: a cohort study. J Clin Med. 2021;10(3):1–11. https://doi.org/10.3390/JCM10030505.
Peiró M, Barrubés J. New context and old challenges in the healthcare system. Rev Esp Cardiol. 2012;65(7):651–5. https://doi.org/10.1016/J.RECESP.2012.02.019.
Lim CE, Pasternak B, Eliasson B, Danaei G, Ueda P. Use of sodium-glucose co-transporter 2 inhibitors and glucagon-like peptide-1 receptor agonists according to the 2019 ESC guidelines and the 2019 ADA/EASD consensus report in a national population of patients with type 2 diabetes. Eur J Prev Cardiol. 2023;30(8):634–43. https://doi.org/10.1093/EURJPC/ZWAC315.
Abrahami D, D’Andrea E, Yin H, et al. Contemporary trends in the utilization of second-line pharmacological therapies for type 2 diabetes in the United States and the United Kingdom. Diabetes Obes Metab. 2023;25(10):2980–8. https://doi.org/10.1111/DOM.15196.
González Manzanares R, Pericet Rodríguez C, Gallo Fernández I, Castillo Domínguez JC, Anguita SM. Heart failure hospitalization during COVID-19 pandemic. SEMERGEN. 2020;46(Suppl 1):91–2. https://doi.org/10.1016/J.SEMERG.2020.06.004.
Frankfurter C, Buchan TA, Kobulnik J, et al. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto. Canada Can J Cardiol. 2020;36(10):1680–4. https://doi.org/10.1016/J.CJCA.2020.07.006.
Acknowledgements
Not applicable.
Funding
R. González-Manzanares holds a Río Hortega contract from Instituto de Salud Carlos III (CM22/00259).
Author information
Authors and Affiliations
Consortia
Contributions
Conception and design (RGM, MAG, JM, VB, JAGO, AP, LRP, MA), analysis and interpretation of data (RGM, JM, MA), drafting of the manuscript (RGM), revising it critically for important intellectual content (MAG, JM, VB, JAGO, AP, LRP, MA), final approval of the manuscript submitted (RGM, MAG, JM, VB, JAGO, AP, LRP, MA).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the Declaration of Helsinki and was approved by the lead centre clinical research ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gonzalez-Manzanares, R., Anguita-Gámez, M., Muñiz, J. et al. Prevalence and incidence of heart failure in type 2 diabetes patients: results from a nationwide prospective cohort—the DIABET-IC study. Cardiovasc Diabetol 23, 253 (2024). https://doi.org/10.1186/s12933-024-02358-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02358-0