Abstract
Background
Coronary three-vessel disease (CTVD) accounts for one-third of the overall incidence of coronary artery disease, with heightened mortality rates compared to single-vessel lesions, including common trunk lesions. Dysregulated glucose metabolism exacerbates atherosclerosis and increases cardiovascular risk. The stress hyperglycemia ratio (SHR) is proposed as an indicator of glucose metabolism status but its association with cardiovascular outcomes in CTVD patients undergoing percutaneous coronary intervention (PCI) remains unclear.
Methods
10,532 CTVD patients undergoing PCI were consecutively enrolled. SHR was calculated using the formula: admission blood glucose (mmol/L)/[1.59×HbA1c (%)–2.59]. Patients were divided into two groups (SHR Low and SHR High) according to the optimal cutoff value of SHR. Multivariable Cox regression models were used to assess the relationship between SHR and long-term prognosis. The primary endpoint was cardiovascular (CV) events, composing of cardiac death and non-fatal myocardial infarction (MI).
Results
During the median follow-up time of 3 years, a total of 279 cases (2.6%) of CV events were recorded. Multivariable Cox analyses showed that high SHR was associated with a significantly higher risk of CV events [Hazard Ratio (HR) 1.99, 95% Confidence interval (CI) 1.58–2.52, P < 0.001). This association remained consistent in patients with (HR 1.50, 95% CI 1.08–2.10, P = 0.016) and without diabetes (HR 1.97, 95% CI 1.42–2.72, P < 0.001). Additionally, adding SHR to the base model of traditional risk factors led to a significant improvement in the C-index, net reclassification and integrated discrimination.
Conclusions
SHR was a significant predictor for adverse CV outcomes in CTVD patients with or without diabetes, which suggested that it could aid in the risk stratification in this particular population regardless of glucose metabolism status.
Similar content being viewed by others
Background
Coronary artery disease (CAD) remains a major threat to public health, with coronary three-vessel disease (CTVD) accounting for one-third of the overall incidence of CAD [1, 2]. Furthermore, the mortality rate of patients with CTVD is nearly double that of individuals with single-vessel lesions [3]. The high incidence and mortality rates render CTVD a particularly noteworthy type of CAD in clinical settings.
It is well established that individuals with dysregulated glucose metabolism or diabetes often carry a more severe burden of atherosclerosis and face a higher risk of adverse cardiovascular events [4, 5]. Hyperglycemic over-stress and diabetes lead to ischemic heart disease and adverse cardiovascular outcomes through a series of epigenetic, molecular, and cellular adaptive mechanisms. These mechanisms include microRNA-155 (miR-155) mediated changes in insulin sensitivity [6]; pericoronary fat over-inflammation, which increases the risk of ischemic heart disease in patients with pre-diabetes compared to normoglycemic patients, resulting in poorer outcomes regardless of PCI [7, 8] or thrombus aspiration [9, 10]. Furthermore, hyperglycemic over-stress induces upregulation of Sodium-glucose cotransporter-2 (SGLT2) expression in cardiomyocytes [11] and using SGLT2 inhibitors can improve cardiac function in diabetic cardiomyopathy by reducing JunD expression [12]. Additionally, hyperglycemia-induced over-inflammation and oxidative stress can be seen as the main triggers of atherogenesis and plaque instability with rupture, leading to plaque instability and rupture [13], and adverse cardiovascular outcomes [14]. Notably, these mechanisms could be seen independently from the diabetes status. In summary, hyperglycemic over-stress induces a pro-oxidative/inflammatory status that alters molecular, metabolic, electrical, and mechanical cardiac functions, potentially leading to heart failure with reduced ejection fraction [15].
Moreover, stress hyperglycemia, which was characterized as elevated admission blood glucose (ABG), is associated with mortality in CAD patients [16, 17]. ABG and hemoglobin A1c (HbA1c) are commonly utilized markers for assessing glycemic status. However, HbA1c primarily reflects chronic glycemic levels, while ABG is subject to variations influenced by individual chronic glycemic profiles. Consequently, neither marker adequately captures the condition of stress-induced hyperglycemia. The stress hyperglycemia ratio (SHR), which was calculated by the formula [ABG (mmol/L)]/[1.59×HbA1c (%) − 2.59)] [18, 19], is considered a reflective indicator of state of glucose metabolism and has been reported to be associated with cardiovascular risk and poor prognosis in previous studies [19,20,21]. However, the association between SHR and the long-term prognosis of CTVD patients undergoing percutaneous coronary intervention (PCI) remains unclear.
In this large-scale retrospective cohort study, we consecutively included 10,532 patients with CTVD who underwent PCI and were subjected to a three-year follow-up. The aim of this study was to evaluate the association between the SHR and the long-term prognosis of patients with CTVD.
Methods
Study design and population
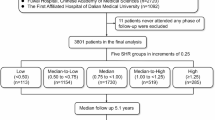
This current study was a single-center prospective cohort study. From January 2017 to December 2018, a total of 12,674 patients who underwent PCI for CTVD were consecutively enrolled at Fuwai Hospital, National Center for Cardiovascular Diseases.
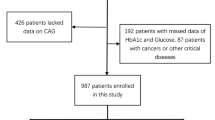
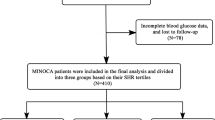
CTVD was defined as angiographic stenosis ≥ 50% in all 3 main coronary arteries, including the left anterior descending, circumflex, and right coronary artery, with or without involvement of the left main artery [22, 23]. The main exclusion criteria were incomplete data on SHR, severe hepatic or kidney dysfunction, decompensated heart failure, systemic inflammatory disease, malignant tumor, acute infection, and loss to follow-up. Ultimately, a total of 10,532 participants were analyzed in the present study. The detailed flow chart is shown in Fig. 1.
Patients were stratified into two groups based on SHR tertiles: SHR Low (including T1 and T2, ≤ 0.88) and SHR High (including T3, > 0.88). The cutoff value of 0.88 for SHR was consistent with the results obtained from the receiver operating characteristic (ROC) curve analysis. The optimal cutoff values were determined according to the maximum Youden Index, which equals the sum of sensitivity and specificity minus 1.
This study was conducted in compliance with the Declaration of Helsinki and was approved by the Ethics Committee of Fuwai Hospital (2016-847). The informed consent form version number is AS2016-1.1. All participants provided written informed consent for both study participation and interventional procedures before enrollment. Relevant information, including the study’s purpose, procedures, potential risks and benefits, confidentiality measures, and the rights of the participants, was provided to all participants before including them in the study. All participants in this study provided written informed consent before intervention.
PCI procedure and medication treatment
All PCI procedures and medical therapies were performed in accordance with the recommendations outlined in the guidelines and at the discretion of the cardiologist, as previously detailed [24]. All patients received loading doses of aspirin (300 mg), clopidogrel (600 mg), or ticagrelor (180 mg) before PCI. After the coronary intervention, the characteristics of the coronary disease, including the number of stenotic vessels, unusual types of coronary stenosis, the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score [25], and data related to stent implantation, were analyzed and recorded by two coronary intervention specialists who were blinded to the baseline data.
Data collection and definitions
Baseline demographic and clinical characteristics were prospectively collected for all participants in the study. Demographic information encompassed age, sex, body mass index (BMI), concurrent diseases, smoking status, family history of CAD, and previous myocardial infarction (MI) or revascularization history (PCI or coronary artery bypass grafting [CABG]). Clinical data comprised the primary diagnosis upon hospital admission, findings from physical examinations, diagnostic imaging, laboratory analyses, and the pharmacological treatment regimen prescribed at the time of discharge.
Admission blood glucose (ABG) analyses were conducted utilizing LABOSPECT 008 system (Hitachi, Tokyo, Japan), while HbA1c levels were quantified employing high-performance liquid chromatography on a Tosoh G8 HPLC Analyzer (Tosoh Bioscience, Tokyo, Japan). The concentrations of triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and creatinine were determined through enzymatic assays using an automated biochemical analyzer (Hitachi 7150, Tokyo, Japan). The measurement of high-sensitivity C-reactive protein (hsCRP) was performed using standard biochemical methodologies at the core laboratory of Fuwai Hospital. Left ventricular ejection fraction (LVEF) at rest was evaluated in accordance with the modified biplane Simpson’s rule [26].
The estimated average chronic glycemic level was calculated using the formula [1.59×HbA1c(%)–2.59] mmol/L [18]. Subsequently, SHR was defined as ABG (mmol/L) divided by the estimated average chronic glycemic value [19].
Diabetes mellitus (DM) status was documented under the following criteria: if the patient had a prior diagnosis of DM, was undergoing glucose-lowering therapy, or exhibited fasting blood glucose levels ≥ 7.0 mmol/L, glycated hemoglobin (HbA1c) levels ≥ 6.5%, or 2-hour plasma glucose levels ≥ 11.1 mmol/L during an oral glucose tolerance test [27, 28]. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or the use of antihypertensive therapy [29]. Stroke was defined as a previous history of cerebral bleeding, ischemic stroke, or transient ischemic attack; diagnosis of chronic coronary syndrome (CCS) and acute coronary syndrome (ACS) on admission was according to the latest guideline [30, 31].
Follow-up and end point definitions
Patients were followed-up at 6-month intervals for a duration of 3 years following discharge, utilizing medical records, clinical visits, and/or telephone interviews conducted by trained investigators who were blinded to the patients’ clinical data. The primary endpoint was defined as CV events, a composite of cardiac death and non-fatal MI. The ICD-10 code for cardiac death, specifically for sudden cardiac death, is I46.1. The ICD-10 code for a non-fatal myocardial infarction (heart attack) is I21.4. Secondary endpoint was defined as the two composite events. Death was considered cardiac unless unequivocal non-cardiovascular cause could be established. Nonfatal MI was characterized by the presence of positive cardiac troponins accompanied by typical chest pain, typical serial changes in the electrocardiogram, identification of an intracoronary thrombus through angiography or imaging evidence indicating new loss of viable myocardium or a new regional wall-motion abnormality [32].
Statistical analysis
Continuous variables were presented as the mean ± standard deviation if they followed a normal distribution; otherwise depicted as the median (interquartile range). Meanwhile, categorical variables were exhibited as frequencies (percentages). Group discrepancies were evaluated utilizing either one-way ANOVA, the Kruskal‒Wallis H test, Pearson’s chi-square test, or Fisher’s exact test, accordingly.
The Kaplan-Meier curves were employed to depict the cumulative incidence of clinical endpoints across different groups, while the log-rank test was utilized to compare these incidences. Hazard ratios (HRs) along with their corresponding 95% confidence intervals (CIs) were calculated using both univariable and multivariable Cox regression models. The multivariable Cox regression model incorporated various potential confounders, including age, male sex, BMI, hypertension, AMI, previous MI, previous PCI, previous CABG, smoking status, previous stroke, LVEF, TC, LDL-C, eGFR, hsCRP, serum creatinine, preprocedural SYNTAX score, calcification, total stent length, aspirin use, clopidogrel use and statins use.
We constructed Restricted Cubic Spline (RCS) plots to examine the linearity assumptions regarding the association between SHR and clinical endpoints. Additionally, in the RCS model, adjustments were made for other confounding factors as detailed above. To evaluate enhancements in risk discrimination, we employed Harrell’s C-statistic, as well as the continuous net reclassification improvement (NRI) and the integrated discrimination improvement (IDI), modified for survival analyses [33, 34]. Statistical significance was defined as two-tailed P values < 0.05. All statistical analyses were conducted using R version 4.0.2 (The R Foundation).
Results
Baseline characteristics according to clinical outcomes or SHR levels
Between January 2017 and December 2018, a total of 10,532 CTVD patients were finally included in this study. The average age of the enrolled participants was 60.64 ± 9.89 years old, and 77.6% of them were male. The average value of SHR was 0.86 ± 0.20 in the whole population. Comparisons of the baseline characteristics between participants with and without clinical outcomes were shown in Table 1. Compared with event-free patients, those who suffered from adverse events tended to be older, have higher proportion of comorbidities, including diabetes (higher FBG and HbA1c), heart failure (lower LVEF), renal dysfunction, prior MI and prior CABG, and have higher level of SHR. SHR showed a normal distribution among the total population (Additional file 1: Figure S1). The clinical presentation of patients with events were more likely to be AMI. Regarding the angiographic characteristics, the lesions in patients who developed events during the follow-up period were further complicated by calcification. The baseline characteristics grouped by the levels of SHR were presented in Additional file 1: Table S1. The GLM regression analysis indicated LVEF (P < 0.001), Diabetes mellitus (P < 0.001), Smoking (P = 0.007), Previous MI (P = 0.011) were associated with post-PCI QFR value (Additional file 1: Table S2).
SHR and the long-term prognosis in CTVD patients
During the median follow-up time of 3 years, a total of 279 cases (2.6%) of CV events, including 204 cases (1.9%) of all-cause death and 75 cases (0.7%) of non-fatal MI, were recorded. In the total population, the Kaplan-Meier curves showed a significantly higher incidence of CV events, cardiac death and non-fatal MI in the group of high SHR level (all log-rank P < 0.001) (Fig. 2). In the multivariable Cox regression analyses, patients with high levels of SHR had significantly higher risks of CV events (HR 1.99, 95% CI 1.58–2.52, P < 0.001), cardiac death (HR 1.81, 95% CI 1.37–2.38, P < 0.001) and non-fatal MI (HR 2.26, 95% CI 1.62–4.03, P < 0.001) (Table 2). When considered as a continuous variable, SHR (per one-unit increase) was also an independent predictor for CV events (HR 2.53, 95% CI 1.65–3.89, P < 0.001), cardiac death (HR 2.15, 95% CI 1.28–3.62, P = 0.004) and non-fatal MI (HR 3.66, 95% CI 1.70–7.86, P = 0.001) (Additional file 1: Table S3). Restricted cubic spline showed a dose-response relationship between SHR and CV events (P for overall < 0.001, P for nonlinearity = 0.139), and similar results were observed for cardiac death and non-fatal MI (Fig. 3).
For DM patients, multivariable Cox analyses revealed a 1.50-fold increased risk for CV events (HR 1.50, 95% CI 1.08–2.10, P = 0.016), a 1.73-fold increased risk for cardiac death (HR 1.73, 95% CI 1.13–2.64, P = 0.011), and a 2.26-fold increased risk for non-fatal MI (HR 2.12, 95% CI 1.12–4.03, P = 0.021) (Table 2; Additional file 1: Figure S2A-C). Per one-unit increase in SHR led to a 2.34-fold increased risk for CV events (HR 2.34, 95% CI 1.37–3.99, P = 0.002), a 2.01-fold increased risk for cardiac death (HR 2.01, 95% CI 1.04–3.89, P = 0.038), and a 3.13-fold increased risk for non-fatal MI (HR 3.13, 95% CI 1.25–7.87, P = 0.015) (Additional file 1: Table S3). There were also observed linear relationships between SHR and the occurrence of CV events, cardiac death, non-fatal MI in the DM population (all P for nonlinearity > 0.05) (Additional file 1: Figure S2A-C). Similar results were noted in patients without DM, except that the continuous SHR was not an independent predictor for cardiac death (HR 2.30, 95% CI 0.99–5.38, P = 0.053) (Additional file 1: Table S3).
After adjusting for potential confounders, DM was an independent predictor for CV events in the total population (HR 1.36, 95% CI 1.08–1.73, P = 0.015) (Additional file 1: Table S4). When combined the status of DM and the levels of SHR, the total population were divided into four groups: SHR Low with and without DM, and SHR High with and without DM. As shown in Fig. 4, compared to those in the SHR Low/non-DM group, patients in the high SHR/non-DM and high SHR/DM groups had significantly higher risks of CV events (HR 1.85, 95% CI 1.32–2.53, P < 0.001; HR 2.06, 95% CI 1.51–2.82, P < 0.001). Among the four groups, patients with high levels of SHR and DM had the highest risk of CV events (P for trend < 0.001).
Hazard rations (95% CI) for CV events according to SHR groups and DM status. CV events cardiovascular events, SHR stress hyperglycemia ratio, DM Diabetes mellitus. Adjusted for age, male sex, BMI, hypertension, AMI, previous MI, previous PCI, previous CABG, smoking status, previous stroke, LVEF, TC, LDL-C, hsCRP, serum creatinine, preprocedural SYNTAX score, calcification, total stent length, aspirin use, clopidogrel use and statins use
Predictive value of SHR for CV events in CTVD patients
Introducing SHR into the model of traditional risk factors led to a significant improvement on the predictive ability for CV events. Table 3 indicated that the addition of SHR raised the C-index from 0.676 (95% CI 0.652, 0.691) to 0.694 (95% CI 0.672, 0.701). After adding SHR into the model of traditional risk factors, the NRI (0.83, P = 0.038) and IDI (0.18, P = 0.008) of CV events were also significantly increased. Similar results were observed in in the DM and non-DM population (Table 3). However, the NRI (0.87, P = 0.098) was not significantly increased after the addition of SHR to the base model in DM population.
Subgroup analysis
Subgroup analyses were conducted to examine the association between SHR and CV events based on age (> 60 years old), sex, hypertension, hyperlipidemia, smoking status, and MI history. The main results remained robust in all subgroups, with no significant interaction observed (Additional file 1: Table S5).
Sensitivity analysis
To verify the reliability of the relationship between SHR and long-term adverse cardiovascular outcomes in patients with three-vessel disease, we conducted a sensitivity analysis. Based on the median SHR, all 10,532 included patients were divided into two groups: the SHR Below Median group and the SHR Above Median group, with each group comprising 5,266 patients.
In the multivariable Cox regression analyses, patients from SHR Above Median group had significantly higher risks of CV events (HR 1.61, 95% CI 1.27–2.05, P < 0.001), cardiac death (HR 1.78, 95% CI 1.11–2.85, P = 0.017) and non-fatal MI (HR 1.55, 95% CI 1.17–2.05, P = 0.002) (Table S6).
Discussion
The present study was to investigate the association between SHR and long-term prognosis in patients with or without diabetes who had undergone PCI. For the first time, we found that high SHR was an independent predictor for long time adverse cardiovascular outcomes in CTVD patients, regardless of the diabetes status. When combining the diabetes status and SHR levels, patients with high levels of SHR and DM had the highest risk of CV events. After adding SHR to the base model of traditional risk factors, the C-index, NRI and IDI of the base model significantly improved.
Stress-induced hyperglycemia refers to a state of transient hyperglycemia triggered by the activation of the hypothalamic-pituitary-adrenal axis and the excessive secretion of cortisol and adrenaline in response to stress [35]. Moderate hyperglycemia is a protective mechanism to provide sufficient energy during stressful situations [36]. However, immoderate stress hyperglycemia can have negative effect, and several mechanisms may participate in this pathological process. First, stress-induced hyperglycemia is frequently associated with an upregulation of the immune-inflammatory response, leading to an increase in the release of pro-inflammatory cytokines such as interleukin-1, interleukin-6, and tumor necrosis factor-α [37,38,39,40]. Second, hyperglycemia significantly contributes to increased thrombotic activity, enhancing platelet aggregation and fibrinogen levels, thus promoting intra-coronary thrombus formation. This exacerbates adverse outcomes in STEMI patients, including larger infarct sizes and impaired microvascular function [10, 41, 42]. Sigirci et al. showed that in STEMI patients without diabetes undergoing primary PCI, admission hyperglycemia was an independent predictor of large thrombus burden (TIMI grades 4 or 5) [43].
Due to the influence of background glycemic status, admission glucose level could not reflect the extent of stress hyperglycemia exactly. Thus, SHR, calculated by both admission blood glucose and estimated chronic blood glucose, was proposed by Robert et al. [19]. to represent relative hyperglycemia in patients at risk of critical illness. Accumulating studies have demonstrated that SHR was an independent risk factor of CV events in patients with different kinds of cardiovascular diseases, including AMI [44, 45], acute decompensated heart failure [20], severe aortic stenosis [46], ischemia and nonobstructive coronary arteries (INOCA) [47, 48], and acute ischemia or hemorrhagic stroke [49, 50].
Compared to single-vessel disease, CTVD increased the complexity of PCI procedure, and was associated with a worse prognosis [51, 52]. However, the prognostic value of SHR in patients with CTVD has not been investigated yet. For the first time, we found that an increased SHR was associated with elevated CV risks in patients with CTVD, whether they had T2DM or not. In recent years, whether SHR has the same prognostic value in diabetes and non-diabetes still remains a controversial topic. Similar to our results, Cui et al. and Fu et al. found that SHR was an independent predictor for in-hospital mortality and long-term prognosis in AMI patients regardless of diabetes status [53,54,55]. Interestingly, Zhang et al. found that SHR was positively correlated with the risk of multi-vessel CAD in patients with pre-DM or DM, while no significant correlation was observed between SHR and the incidence of multi-vessel CAD [44]. However, it is worth noting that Zhang’s study only investigated the relationship between SHR and the severity of CAD in a cross-sectional design, without presenting any follow-up data.
The linear or non-linear correlation between SHR and unfavorable prognosis has been argued in the previous studies. Yang et al. demonstrated that there was a U-shaped association between SHR and 2-year adverse prognosis in 5,562 ACS patients [56]. Similarly, in a study of 5,190 ACS patients, a U-shaped association was found between SHR and cardiovascular mortality at 4-year follow-up [21]. As for short-term outcomes, Wei et al. found a J-shaped association between SHR and in-hospital mortality in 1099 patients with STEMI [57]. Conversely, a dose-response relationship was observed between SHR and in-hospital mortality (nonlinear P value = 0.260) in a substantial population of 19,929 CAD patients [58]. In the present study, we found a positive linear association between SHR and CV events in patients with CTVD (nonlinear P value = 0.139). The inconsistency of this trend in such studies may be due to differences in sample size and population selection across studies. Therefore, further studies are still required to investigate the association between SHR and CV risk in CTVD patients through large-scale, prospective cohort studies or randomized controlled trials (RCTs).
There are several limitations of this study that need to be acknowledged. First, due to the inherent limitation of the cohort study design, undetected confounders may still exist, although all the potential confounders have been adjusted in the multivariable Cox analysis. Second, we initially categorized anti-diabetic medications into insulin injections and oral anti-diabetic drugs. This categorization limited our ability to provide detailed information on the specific types of oral anti-diabetic medications, including incretin treatment like GLP-1 receptor agonists and SGLT2 inhibitors. GLP-1 receptor agonists have been widely used and proven to improve cardiovascular clinical outcome in patients with acute myocardial infarction (NSTEMI and STEMI) treated with PCI [59, 60]. SGLT2 inhibitors are also recognized for improving clinical outcomes through their pleiotropic effects on atherosclerosis of coronary plaque [61, 62]. Third, detailed medication follow-up data were not available in this study. Last but not least, although a relative large-scale population was included, the present study was conducted in a single center of east Asia, the selection bias could not be avoided.
Conclusions
SHR was a significant predictor for adverse CV outcomes in CTVD patients with or without diabetes, which suggested that it could aid in the risk stratification in this particular population regardless of glucose metabolism status.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CV:
-
Cardiovascular
- CIs:
-
Confidence intervals
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- FBG:
-
Fasting blood glucose
- HF:
-
Heart failure
- HDL-C:
-
High-density lipoprotein cholesterol
- HbA1c:
-
Glycosylated hemoglobin A1c
- HRs:
-
Hazard ratios
- hs-CRP:
-
High-sensitivity C-reactive protein
- LVEF:
-
Left ventricular ejection faction
- LDL-C:
-
Low-density lipoprotein cholesterol
- PCI:
-
Percutaneous coronary intervention
- PAD:
-
Peripheral artery disease
- RCSs:
-
Restricted cubic splines
- SHR:
-
Stress hyperglycaemia ratio
- CTVD:
-
Coronary three-vessel disease
References
D’Ascenzo F, Presutti DG, Picardi E, Moretti C, Omede P, Sciuto F, et al. Prevalence and non-invasive predictors of left main or three-vessel coronary disease: evidence from a collaborative international meta-analysis including 22 740 patients. Heart. 2012;98(12):914–9.
Linder R, Zeidler J, Verheyen F, von der Schulenburg JG, Haverich A, Schilling T. Guidelines versus reality: is coronary stent application in three-vessel disease standard or the exception? Eur J Health Econ. 2018;19(6):821–30.
Thuijs D, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394(10206):1325–34.
Guo L, Wang J, Ding H, Meng S, Zhang X, Lv H, et al. Long-term outcomes of medical therapy versus successful recanalisation for coronary chronic total occlusions in patients with and without type 2 diabetes mellitus. Cardiovasc Diabetol. 2020;19(1):100.
Luscher TF, Creager MA, Beckman JA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Circulation. 2003;108(13):1655–61.
Jankauskas SS, Gambardella J, Sardu C, Lombardi A, Santulli G. Functional role of miR-155 in the pathogenesis of diabetes mellitus and its complications. Noncoding RNA. 2021;7(3):39.
Sardu C, D’Onofrio N, Torella M, Portoghese M, Mureddu S, Loreni F, et al. Metformin therapy effects on the expression of sodium-glucose cotransporter 2, leptin, and SIRT6 levels in pericoronary fat excised from pre-diabetic patients with acute myocardial infarction. Biomedicines. 2021;9(8):904.
Sardu C, D’Onofrio N, Torella M, Portoghese M, Loreni F, Mureddu S, et al. Pericoronary fat inflammation and major adverse cardiac events (MACE) in prediabetic patients with acute myocardial infarction: effects of metformin. Cardiovasc Diabetol. 2019;18(1):126.
Sardu C, Barbieri M, Balestrieri ML, Siniscalchi M, Paolisso P, Calabro P, et al. Thrombus aspiration in hyperglycemic ST-elevation myocardial infarction (STEMI) patients: clinical outcomes at 1-year follow-up. Cardiovasc Diabetol. 2018;17(1):152.
Sardu C, D’Onofrio N, Mauro C, Balestrieri ML, Marfella R. Thrombus aspiration in hyperglycemic patients with high inflammation levels in coronary thrombus. J Am Coll Cardiol. 2019;73(4):530–1.
Marfella R, Scisciola L, D’Onofrio N, Maiello C, Trotta MC, Sardu C, et al. Sodium-glucose cotransporter-2 (SGLT2) expression in diabetic and non-diabetic failing human cardiomyocytes. Pharmacol Res. 2022;184:106448.
Marfella R, D’Onofrio N, Trotta MC, Sardu C, Scisciola L, Amarelli C, et al. Sodium/glucose cotransporter 2 (SGLT2) inhibitors improve cardiac function by reducing JunD expression in human diabetic hearts. Metabolism. 2022;127:154936.
Sardu C, Modugno P, Castellano G, Scisciola L, Barbieri M, Petrella L, et al. Atherosclerotic plaque fissuration and clinical outcomes in pre-diabetics vs. normoglycemics patients affected by asymptomatic significant carotid artery stenosis at 2 years of follow-up: role of microRNAs modulation: the ATIMIR study. Biomedicines. 2021;9(4):401.
Sardu C, Paolisso G, Marfella R. Inflammatory related cardiovascular diseases: from molecular mechanisms to therapeutic targets. Curr Pharm Des. 2020;26(22):2565–73.
Sardu C, Paolisso P, Sacra C, Santamaria M, de Lucia C, Ruocco A, et al. Cardiac resynchronization therapy with a defibrillator (CRTd) in failing heart patients with type 2 diabetes mellitus and treated by glucagon-like peptide 1 receptor agonists (GLP-1 RA) therapy vs. conventional hypoglycemic drugs: arrhythmic burden, hospitalizations for heart failure, and CRTd responders rate. Cardiovasc Diabetol. 2018;17(1):137.
Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773–8.
Kosiborod M, Rathore SS, Inzucchi SE, Masoudi FA, Wang Y, Havranek EP, et al. Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction: implications for patients with and without recognized diabetes. Circulation. 2005;111(23):3078–86.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ, et al. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31(8):1473–8.
Roberts GW, Quinn SJ, Valentine N, Alhawassi T, O’Dea H, Stranks SN, et al. Relative hyperglycemia, a marker of critical illness: introducing the stress hyperglycemia ratio. J Clin Endocrinol Metab. 2015;100(12):4490–7.
Zhou Q, Yang J, Wang W, Shao C, Hua X, Tang YD. The impact of the stress hyperglycemia ratio on mortality and rehospitalization rate in patients with acute decompensated heart failure and diabetes. Cardiovasc Diabetol. 2023;22(1):189.
Wang M, Su W, Cao N, Chen H, Li H. Prognostic implication of stress hyperglycemia in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2023;22(1):63.
Zhang C, Jiang L, Xu L, Tian J, Liu J, Zhao X, et al. Implications of N-terminal pro-B-type natriuretic peptide in patients with three-vessel disease. Eur Heart J. 2019;40(41):3397–405.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–72.
Authors/Task Force m, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–619.
Kappetein AP, Head SJ, Morice MC, Banning AP, Serruys PW, Mohr FW, et al. Treatment of complex coronary artery disease in patients with diabetes: 5-year results comparing outcomes of bypass surgery and percutaneous coronary intervention in the SYNTAX trial. Eur J Cardiothorac Surg. 2013;43(5):1006–13.
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on standards, Subcommittee on quantitation of two-dimensional echocardiograms. J Am Soc Echocardiogr. 1989;2(5):358–67.
American Diabetes A. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38 Suppl:S8-S16.
Jin JL, Cao YX, Zhang HW, Sun D, Hua Q, Li YF, et al. Lipoprotein(a) and cardiovascular outcomes in patients with coronary artery disease and prediabetes or diabetes. Diabetes Care. 2019;42(7):1312–8.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720–826.
Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice guidelines. Circulation. 2023;148(9):e9–119.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33(20):2551–67.
Harrell FE Jr., Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87.
Pencina MJ, D’Agostino RB, Sr., Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30(1):11–21.
Marik PE, Zaloga GP. Adrenal insufficiency in the critically ill: a new look at an old problem. Chest. 2002;122(5):1784–96.
Osawa T, Kato Y. Protective role of antioxidative food factors in oxidative stress caused by hyperglycemia. Ann N Y Acad Sci. 2005;1043:440–51.
Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes. 2004;53(8):2079–86.
Heesen M, Bloemeke B, Heussen N, Kunz D. Can the interleukin-6 response to endotoxin be predicted? Studies of the influence of a promoter polymorphism of the interleukin-6 gene, gender, the density of the endotoxin receptor CD14, and inflammatory cytokines. Crit Care Med. 2002;30(3):664–9.
Ishizuka K, Usui I, Kanatani Y, Bukhari A, He J, Fujisaka S, et al. Chronic tumor necrosis factor-alpha treatment causes insulin resistance via insulin receptor substrate-1 serine phosphorylation and suppressor of cytokine signaling-3 induction in 3T3-L1 adipocytes. Endocrinology. 2007;148(6):2994–3003.
Ruan H, Miles PD, Ladd CM, Ross K, Golub TR, Olefsky JM, et al. Profiling gene transcription in vivo reveals adipose tissue as an immediate target of tumor necrosis factor-alpha: implications for insulin resistance. Diabetes. 2002;51(11):3176–88.
Iwakura K, Ito H, Ikushima M, Kawano S, Okamura A, Asano K, et al. Association between hyperglycemia and the no-reflow phenomenon in patients with acute myocardial infarction. J Am Coll Cardiol. 2003;41(1):1–7.
Kersten JR, Toller WG, Tessmer JP, Pagel PS, Warltier DC. Hyperglycemia reduces coronary collateral blood flow through a nitric oxide-mediated mechanism. Am J Physiol Heart Circ Physiol. 2001;281(5):H2097–104.
Sigirci S, Yildiz SS, Keskin K, Cetinkal G, Aksan G, Gurdal A, et al. The predictive value of stress hyperglycemia on thrombus burden in nondiabetic patients with ST-segment elevation myocardial infarction. Blood Coagul Fibrinolysis. 2019;30(6):270–6.
Karakasis P, Stalikas N, Patoulias D, Pamporis K, Karagiannidis E, Sagris M, et al. Prognostic value of stress hyperglycemia ratio in patients with acute myocardial infarction: a systematic review with bayesian and frequentist meta-analysis. Trends Cardiovasc Med. 2023. https://doi.org/10.1016/j.tcm.2023.11.006.
Schmitz T, Freuer D, Harmel E, Heier M, Peters A, Linseisen J, et al. Prognostic value of stress hyperglycemia ratio on short- and long-term mortality after acute myocardial infarction. Acta Diabetol. 2022;59(8):1019–29.
Hu X, Feng D, Zhang Y, Wang C, Chen Y, Niu G, et al. Prognostic effect of stress hyperglycemia ratio on patients with severe aortic stenosis receiving transcatheter aortic valve replacement: a prospective cohort study. Cardiovasc Diabetol. 2024;23(1):73.
Gao S, Huang S, Lin X, Xu L, Yu M. Prognostic implications of stress hyperglycemia ratio in patients with myocardial infarction with nonobstructive coronary arteries. Ann Med. 2023;55(1):990–9.
Mone P, Lombardi A, Salemme L, Cioppa A, Popusoi G, Varzideh F, et al. Stress hyperglycemia drives the risk of hospitalization for chest pain in patients with ischemia and nonobstructive coronary arteries (INOCA). Diabetes Care. 2023;46(2):450–4.
Huang YW, Yin XS, Li ZP. Association of the stress hyperglycemia ratio and clinical outcomes in patients with stroke: a systematic review and meta-analysis. Front Neurol. 2022;13:999536.
Chu H, Huang C, Tang Y, Dong Q, Guo Q. The stress hyperglycemia ratio predicts early hematoma expansion and poor outcomes in patients with spontaneous intracerebral hemorrhage. Ther Adv Neurol Disord. 2022;15:17562864211070681.
Toma A, Stahli BE, Gick M, Gebhard C, Nuhrenberg T, Mashayekhi K, et al. Impact of multi-vessel versus single-vessel disease on outcomes after percutaneous coronary interventions for chronic total occlusions. Clin Res Cardiol. 2017;106(6):428–35.
Elgendy IY, Huo T, Mahmoud A, Bavry AA. Complete versus culprit-only revascularization in patients with multi-vessel disease undergoing primary percutaneous coronary intervention: a meta-analysis of randomized trials. Int J Cardiol. 2015;186:98–103.
Cui K, Fu R, Yang J, Xu H, Yin D, Song W, et al. The impact of fasting stress hyperglycemia ratio, fasting plasma glucose and hemoglobin A1c on in-hospital mortality in patients with and without diabetes: findings from the China acute myocardial infarction registry. Cardiovasc Diabetol. 2023;22(1):165.
Cui K, Fu R, Yang J, Xu H, Yin D, Song W, et al. Stress hyperglycemia ratio and long-term mortality after acute myocardial infarction in patients with and without diabetes: a prospective, nationwide, and multicentre registry. Diabetes Metab Res Rev. 2022;38(7):e3562.
Fu R, Cui K, Yang J, Xu H, Yin D, Song W, et al. Fasting stress hyperglycemia ratio and in-hospital mortality after acute myocardial infarction in patients with different glucose metabolism status: results from China acute myocardial infarction registry. Diabetes Res Clin Pract. 2023;196:110241.
Yang J, Zheng Y, Li C, Gao J, Meng X, Zhang K, et al. The impact of the stress hyperglycemia ratio on short-term and long-term poor prognosis in patients with Acute Coronary Syndrome: insight from a large cohort study in Asia. Diabetes Care. 2022;45(4):947–56.
Wei QC, Chen YW, Gao QY, Ren KD, Liu YB, He F, et al. Association of stress hyperglycemia with clinical outcomes in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention: a cohort study. Cardiovasc Diabetol. 2023;22(1):85.
Xu W, Song Q, Wang X, Zhao Z, Meng X, Xia C, et al. Association of stress hyperglycemia ratio and in-hospital mortality in patients with coronary artery disease: insights from a large cohort study. Cardiovasc Diabetol. 2022;21(1):217.
Marfella R, Sardu C, Calabro P, Siniscalchi M, Minicucci F, Signoriello G, et al. Non-ST-elevation myocardial infarction outcomes in patients with type 2 diabetes with non-obstructive coronary artery stenosis: effects of incretin treatment. Diabetes Obes Metab. 2018;20(3):723–9.
Marfella R, Sardu C, Balestrieri ML, Siniscalchi M, Minicucci F, Signoriello G, et al. Effects of incretin treatment on cardiovascular outcomes in diabetic STEMI-patients with culprit obstructive and multivessel non obstructive-coronary-stenosis. Diabetol Metab Syndr. 2018;10:1.
Marfella R, Sardu C, D’Onofrio N, Fumagalli C, Scisciola L, Sasso FC, et al. SGLT-2 inhibitors and in-stent restenosis-related events after acute myocardial infarction: an observational study in patients with type 2 diabetes. BMC Med. 2023;21(1):71.
Sardu C, Trotta MC, Sasso FC, Sacra C, Carpinella G, Mauro C, et al. SGLT2-inhibitors effects on the coronary fibrous cap thickness and MACEs in diabetic patients with inducible myocardial ischemia and multi vessels non-obstructive coronary artery stenosis. Cardiovasc Diabetol. 2023;22(1):80.
Acknowledgements
Not applicable.
Funding
This study is supported by CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-008) and National High Level Hospital clinical Research Funding (No. 2023-GSP-QN-21)
Author information
Authors and Affiliations
Contributions
ZQ, XB performed study design, researched data, contributed to discussion, and wrote, reviewed, and edited the manuscript. CS, CZ and RZ acquired the data, revised the manuscript’s intellectual content. SY, QL and ZL curated data and figures. KD and WM reviewed and edited the manuscript. All authors approved the final version of the manuscript. KD are the guarantors of this work and had full access to all the data in the study and took responsibility for the accuracy of the data analysis and the integrity of the data.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study process was in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of Fuwai hospital. All subjects provided informed written consent for long-term follow-up before intervention.
Consent for publication
The manuscript was approved by all authors for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiao, Z., Bian, X., Song, C. et al. High stress hyperglycemia ratio predicts adverse clinical outcome in patients with coronary three-vessel disease: a large-scale cohort study. Cardiovasc Diabetol 23, 190 (2024). https://doi.org/10.1186/s12933-024-02286-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02286-z