Abstract
Background
People with type 2 diabetes (T2D) are at elevated risk of cardiovascular disease (CVD) including stroke, yet existing real-world evidence (RWE) on the clinical and economic burden of stroke in this population is limited. The aim of this cohort study was to evaluate the clinical and economic burden of stroke among people with T2D in France.
Methods
We conducted a retrospective RWE study using data from the nationally representative subset of the French Système National des Données de Santé (SNDS) database. We assessed the incidence of stroke requiring hospitalization between 2012 and 2018 among T2D patients. Subsequent clinical outcomes including CVD, stroke recurrence, and mortality were estimated overall and according to stroke subtype (ischemic versus hemorrhagic). We also examined the treatment patterns for glucose-lowering agents and CVD agents, health care resource utilization and medical costs.
Results
Among 45,331 people with T2D without baseline history of stroke, 2090 (4.6%) had an incident stroke requiring hospitalization. The incidence of ischemic stroke per 1000 person-years was 4.9-times higher than hemorrhagic stroke (6.80 [95% confidence interval (CI) 6.47–7.15] versus 1.38 [1.24–1.54]). During a median follow-up of 2.4 years (interquartile range 0.6; 4.4) from date of index stroke, the rate of CVD, stroke recurrence and mortality per 1000 person-years was higher among hemorrhagic stroke patients than ischemic stroke patients (CVD 130.9 [107.7–159.0] versus 126.4 [117.2–136.4]; stroke recurrence: 86.7 [66.4–113.4] versus 66.5 [59.2–74.6]; mortality 291.5 [259.1–327.9] versus 144.1 [134.3–154.6]). These differences were not statistically significant, except for mortality (adjusted hazard ratio 1.95 [95% CI 1.66–2.92]). The proportion of patients prescribed glucagon-like peptide-1 receptor agonists increased from 4.2% at baseline to 6.6% during follow-up. The proportion of patients prescribed antihypertensives and statins only increased slightly following incident stroke (antihypertensives: 70.9% pre-stroke versus 76.7% post-stroke; statins: 24.1% pre-stroke versus 30.0% post-stroke). Overall, 68.8% of patients had a subsequent hospitalization. Median total medical costs were €12,199 (6846; 22,378).
Conclusions
The high burden of stroke among people with T2D, along with the low proportion of patients receiving recommended treatments as per clinical guidelines, necessitates a strengthened and multidisciplinary approach to the CVD prevention and management in people with T2D.
Similar content being viewed by others
Background
Despite improvements in the management of conventional cardiovascular risk factors [1], cardiovascular disease remains an important cause of premature morbidity and mortality among people with type 2 diabetes (T2D) [2,3,4,5,6,7]. People with T2D have a 1.5- to twofold elevated risk of stroke compared to the general population, and post-stroke outcomes [8], including mortality, are worse among people with T2D as compared to the general population without diabetes [9,10,11,12].
Newer glucose-lowering agents such as glucagon-like peptide 1 receptor agonists (GLP-1 RA) or sodium-glucose-like cotransporter 2 inhibitors (SGLT2i) have established cardiovascular disease benefits [13, 14]. Clinical guidelines, such as those from the American Diabetes Association (ADA), the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC), recommend the use of these agents in people with T2D with previous cardiovascular disease or who are at high risk for cardiovascular disease [15,16,17]. While the use of these agents is growing, evidence indicates that they are not prescribed per guideline recommendations [6, 18, 19]. Specifically, evidence from the CAPTURE study, a cross-sectional study conducted across 13 countries, indicated that these agents were prescribed in people with T2D in 2019 at a similar rate regardless of whether the patient had previous cardiovascular disease [6]. This therefore represents a missed opportunity to prevent incident or recurrent neurological and cardiovascular events.
While the clinical and economic burden of cardiovascular disease in people with T2D has been previously described using national databases in Europe [20], less is known about post-stroke clinical outcomes, management practices and costs in the T2D population in real-world settings. The French national health database, the Système National des Données de Santé (SNDS), which captures claims data for 99% of the French population (\( \sim 66 \) million), offers unique opportunities to examine treatment practices, clinical outcomes, health care resource utilization and costs following incident stroke in a nationally representative sample of people with T2D. The overall objective of the present study was to estimate the clinical and economic burden of stroke among people with T2D in France.
Methods
Study population
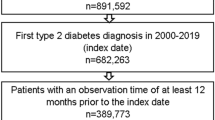
Data for this retrospective cohort study were extracted from the Echantillon Général des Bénéficiaires (EGB), a random sample of the SNDS database including approximately 700,000 people. Data from this source are linked via unique social security numbers to primary care, hospital, pharmacy, and death registration databases.
The study population included adults (age > 18 years) with T2D who had an incident stroke requiring hospitalization between 1 January 2012 and 31 December 2018. Index date was the date of stroke hospital admission, and baseline was the 24 months prior to index date. Patients were followed from index date until the earliest of 31 December 2019 or date of death (Additional file 1: Fig. S1). All patients excluding those that died were followed for a minimum of 12 months.
People with T2D were identified either using the International Classification of Disease, version 10 (ICD-10) code E11 in the long-term disease database or from a hospital discharge diagnosis, or using at least three records for reimbursements of oral antidiabetics or insulin. People with both a diagnostic record for type 1 diabetes (ICD-10: E10) and insulin monotherapy were excluded. Incident stroke events were identified with relevant ICD-10 diagnostic codes (ischemic stroke: I63 or G45 [principal diagnosis], combination of G46 [principal diagnosis] + I63 [secondary diagnostic]; hemorrhagic stroke: I60-I62 [principal diagnosis], combination of G46 [principal diagnosis] + I60-I62 [secondary diagnosis]; unspecified stroke: I64 [principal diagnosis], combination of G46 [principal diagnosis] + I64 [secondary diagnosis]). Patients with any prior history of stroke were excluded.
Study variables and definitions
Patient baseline demographics (age and sex) and clinical characteristics including time from first evidence of T2D to first stroke, comorbidities, Charlson Comorbidity index [21], diabetes treatments (biguanides, sulfonylureas, insulin, dipeptidyl peptidase-4 inhibitor [DPP-4 inhibitors], meglitinides, alpha-glucosidase inhibitors, thiazolidinediones, GLP-1 RA), and cardiovascular disease treatments (anti-hypertensives, anticoagulants, antiplatelets, statins) were collected during the baseline period. SGLT2i were excluded from the list of diabetes treatments since they had not entered the French market during the study period. The GLP-1 RA exenatide and liraglutide entered the French market in 2008 and 2009, respectively, while dulaglutide did not enter until 2016. As such, usage of GLP-1 RA reported in this study represents early uptake. Full definitions of all variables are presented in Additional file 1: Table S1.
Clinical outcomes
Stroke recurrence was defined based on ICD-10 diagnostic codes and was assessed from index date + 21 days until date of stroke recurrence, death or end of follow-up [22]. Development of cardiovascular diseases, defined as coronary artery disease, cardiac arrhythmias, cerebrovascular disease (including stroke), peripheral arterial disease (PAD), heart failure or aortic disease, as well as thromboembolic events, were defined based upon the identification of relevant codes during the follow-up period. All-cause mortality was assessed from index date until end of follow-up.
Treatments
Diabetes and cardiovascular disease treatments administered during follow-up were captured and presented among patients who did not die without the corresponding treatments recorded.
Health care resource utilization (HCRU)
Patient HCRU during follow-up was captured under the following categories: index stroke hospitalization, subsequent hospitalizations (day and overnight stay cases/overnight stays only/intensive care unit stays), outpatient physician visits according to specialty, physical rehabilitation therapy visits.
Costs
Annual costs of HCRU per patient were estimated in Euros during follow-up, including index date. Costs included all costs incurred within hospital, external consultation costs and outpatient costs.
Statistical analysis
The crude incidence of stroke among people with T2D in the study period was estimated per 1000 person-years. The corresponding two-sided 95% confidence interval (CI) was calculated using the Poisson distribution. Directly age-standardized incidence rates were calculated using the French population as the reference population. Baseline and outcome variables were described overall and per stroke subtype using descriptive statistics. Differences in baseline characteristics between ischemic stroke patients and hemorrhagic stroke patients were assessed using Mann–Whitney tests or t-tests for continuous variables, and with Chi-square tests for categorical variables; where more than 25% of the cells exhibited expected counts below 5, the Fisher Exact test was applied. Incidence of clinical and HCRU outcomes were estimated per 1000 person-years of follow-up with corresponding 95% CIs. Differences in time to event outcomes between ischemic stroke and hemorrhagic stroke patients were assessed using Kaplan–Meier curves and compared using log-rank tests. We also used Cox proportional hazards models to estimate hazard ratios (HRs) and 95% CIs for the incidence of outcomes in patients with ischemic vs. hemorrhagic stroke, after adjusting for age, sex and baseline history of arrythmia (which was significantly associated with stroke subtypes at baseline).
Results
Incidence of stroke
Overall, data for 45,331 people with T2D were extracted (Additional file 1: Fig. S2). Of these, 2090 (4.6%) people had an incident stroke between 2012 and 2018. This equated to an overall crude stroke incidence rate of 9.0 per 1000 person-years. Age-standardized incidence rates of stroke declined from 10.3 per 1000 person-year in 2012 to 7.6 per 1000 person-year in 2018.
Of the 2090 incident strokes, 1582 (75.7%) were ischemic strokes, 325 (15.6%) were hemorrhagic strokes, and 183 (8.6%) were unspecified stroke. The incidence of ischemic stroke was 4.9-times higher than that of hemorrhagic stroke (6.8 versus 1.4 per 1000 person-years).
Baseline characteristics
Baseline characteristics of the 2090 incident stroke patients are presented in Table 1, overall and according to stroke subtype; results on unspecified stroke are not presented. The mean (standard deviation [SD]) age of the study population was 75.0 (11.4) years, and 1156 (55.3%) were male. The most common comorbid conditions among patients included hypertension (83.0%), dyslipidemia (63.6%) and cardiac arrhythmias (19.4%).
Clinical outcomes
Overall, the 1-year cumulative incidence of stroke recurrence was 10.7% (95% CI 9.2–12.2), with no significant difference when stratified by subtype of index stroke (p = 0.094) (Fig. 1). During a mean follow-up of 2.8 years from index stroke, 53.2% of patients (55.9% versus 38.5% of ischemic and hemorrhagic stroke patients, respectively) were hospitalized for cardiovascular disease (Table 2). The most common cardiovascular disease outcomes were cardiac arrhythmias, coronary heart disease (CHD), and heart failure, with rates of 106.2 (95% CI 97.8–115.3), 69.8 (63.5–76.7) and 69.3 (62.7–76.6) per 1000 person-years, respectively. There was no significant difference in risk of any subsequent cardiovascular disease according to stroke subtype after adjustment (Table 2). Time to first cardiovascular event for each clinical outcome and according to index stroke subtype is presented in Additional file 1: Fig. S3.
The overall mortality rate was 164.9 (155.6–174.7) per 1,000 person-years, and risk of mortality was significantly higher among hemorrhagic stroke patients than ischemic stroke patients (adjusted HR [95% CI] 1.95 [1.66–2.92]) (Fig. 2, Table 2). Overall, the 30-day and one-year mortality rates were 16.3% and 28.3%, respectively. Hemorrhagic stroke mortality rate at 30-days was 23 percentage points higher than for ischemic stroke (Table 2).
Treatment patterns
Metformin was the most prescribed glucose-lowering agent, used in 56.3% patients pre-stroke and 54.8% patients during follow-up (Fig. 3). The use of insulin increased from 27.7% pre-stroke to 37.5% during follow-up. The use of GLP-1 RA increased from 4.2% pre-stroke to 6.6% during follow-up. The use of most cardiovascular therapies increased following incident stroke (Fig. 4). In the 24 months prior to stroke, 78.3% of patients were prescribed anti-hypertensive medications and this increased to 85.5% during follow-up. The proportion of patients prescribed statins following the index stroke remained largely unchanged compared to the previous 24-months (30.0% versus 31.4%) (Fig. 4), with only a small proportion (8%) of untreated patients switching to statins during the first 12 months following the index stroke (Fig. 5). Treatment patterns trends were similar for patients with index ischemic and hemorrhagic stroke.
Health care resource utilization
Approximately two thirds of the cohort (68.8%) had a subsequent hospitalization following the index stroke hospitalization (Table 3). The rate of subsequent hospitalizations was 2234 per 1000 person-years overall and was considerably higher in hemorrhagic stroke patients than in ischemic stroke patients (hemorrhagic stroke: 3110 per 1000 person-years, ischemic stroke:1926 per 1000 person-years). Among the 63.7% of the cohort who had a subsequent overnight hospitalization, the median (IQR) length of stay was 7.5 (5.0–11.3) days; it was similar according to stroke subtype.
During follow-up, 81.7% of patients had a record of outpatient visits with a greater proportion of ischemic stroke (85.5%) patients having outpatient visits than hemorrhagic stroke patients (63.4%). The overall rate of outpatient visits was 9213 per 1000 person-years. The most common outpatient visits were to general practitioners (68.9%) and cardiovascular specialists (31.3%). Stroke rehabilitation visits occurred in more than half the cohort during follow-up (54.6%) at a rate of 12,404 per 1000 person-years.
Costs
Overall, the median (IQR) yearly hospital admission costs for stroke patients with T2D, including the cost of all hospitalizations (including index hospitalization), procedures, and drugs administered in hospitals was €5683 (2634–11,292). Median yearly hospital admission costs were higher for hemorrhagic stroke patients than ischemic stroke patients: €6727 (3366–12,080) versus €5,375 (2485–10,627), respectively. The median (IQR) yearly outpatient costs, including cost of visits and consultations, drugs, and procedures outside of hospitals was €4890 (1599–11,316). The median (IQR) overall total yearly cost incorporating hospital admissions, external consultations, and all outpatient costs was €12,199 (6846–22,378), with no significant difference by index stroke subtype (ischemic stroke: 11,947 [6851–21,764], hemorrhagic stroke: 11,985 [6236–21,753]).
Discussion
Key findings
In this real-world study using data representative of the overall French population, the incidence of stroke was high, affecting 4.6% of the people with T2D. Of the incident strokes, 75.7% were ischemic and 15.6% were hemorrhagic. The overall clinical and economic burden of stroke was substantial, with a 1-year cumulative incidence of stroke recurrence of 10.7%, 1-year mortality rate of 28.3%, and a median total yearly cost of €12,199. Risk of mortality was significantly higher following hemorrhagic stroke than ischemic stroke (adjusted HR: 1.95 [1.66–2.92]), though there was no significant difference in subsequent cardiovascular disease outcomes by stroke subtype.
Relation to previous studies
The observed overall age-standardized incidence rate of stroke of 9.0 per 1000 person-year during the study period aligns closely with data from the Swedish National Diabetes Register for the period 1998–2012 in which incidence rate of stroke among people with T2D was 8.8 per 1000 person-years [2]. Similarly, data from Australia indicated a crude incidence rate for hospitalization for stroke of 6.5 per 1000 person-years among people with T2D in 2018 [23]. Disparities in incidence rates between earlier data and the present study likely reflect key differences in the distribution and management of cardiovascular risk factors between the countries and over time. The decline in incidence of stroke in the present study between 2012 and 2018 illustrates the likely impact of improvements in cardiovascular disease risk factor management. Nonetheless, the incidence of stroke among patients with T2D remains considerably higher than observed in the general population. Data from the Global Burden of Disease collaborators indicated that the overall age-standardized incidence rate of stroke was 1.5 (1.4–1.7) per 1000 person-year in 2019 among the general population with or without diabetes [24].
The Incidence rate for ischemic stroke reported in the present study (6.8 per 1000 person-year) also aligns closely with findings from national registries in Scotland [9]. In contrast, findings from Sweden indicate an ischemic stroke incidence rate of 3.7 per 1000 person-years in 2013, a possible reflection of difference in distribution and management of cardiovascular disease risk factors between French and Swedish populations [9, 25].
These data highlight that while there have been reductions in the incidence of cardiovascular outcomes such as stroke over time, people with T2D remain at an elevated risk of developing stroke [26, 27].
There are limited contemporary data on post-stroke outcomes for T2D populations. However, most evidence indicates that people with T2D are at elevated risk of adverse outcomes following stroke compared to people without T2D [2, 11, 28, 29]. The burden of cardiovascular disease following stroke in the present study was considerable. Cardiac arrhythmias were the most common cardiovascular outcome following incident stroke, with an overall rate of 106.2 (97.8–115.3) per 1000 person-years.
The proportion of patients receiving anticoagulation therapy during follow-up (40.0%) surpassed the proportion of patients with cardiac arrhythmias (24.3%). This finding likely reflects the use of anticoagulants for the prevention and/or treatment of other indications such as thromboembolic diseases. For example, 24.5% of patients had evidence of pulmonary embolism during follow-up. Another potential explanation might be the potential under-estimation of cardiac arrhythmias due to the use of hospital discharge diagnosis codes to detect this outcome. The probability of atrial fibrillation following ischemic stroke has been demonstrated to be high, regardless of whether the stroke can be attributed to other non-cardioembolic causes such as large-artery atherosclerotic disease or small-vessel occlusive disease [30,31,32]. Given that atrial fibrillation increases the risk of ischemic stroke five-fold [33], the findings highlight the importance of accurate cardiac arrythmia evaluation and subsequent antithrombotic therapy in stroke patients with T2D. Though not statistically significant, the incidence of cardiac arrythmias following stroke was also higher among ischemic stroke than hemorrhagic stroke patients (108.93 [95% CI 99.4–119.4] vs. 94.7 [73.6–121.7]). This finding has been demonstrated in previous studies conducted among the general population [34]. For example, in a US-based study ischemic stroke patients had a higher rate of death due to arrhythmia than hemorrhagic stroke patients (7.3% vs. 18.7%) [34]. The incidence of coronary heart disease and carotid artery disease was also higher among ischemic stroke than hemorrhagic stroke in the current study. In a study undertaken using the UK Clinical Practice Research Datalink, rates of coronary heart disease were slightly higher among ischemic stroke than hemorrhagic stroke patients (1.19 per 100 person-years vs. 1.07 per 100 person-years), though this difference was not significant [35].
In people with established cardiovascular disease or at high risk for cardiovascular disease, GLP-1 RA and SGLT2i have been recommended by the consensus reports of the ADA and the EASD since 2018 [36]. This recommendation was based upon established cardiovascular disease benefit as demonstrated in clinical trials and observational studies [13, 14, 37,38,39]. That so few patients were subsequently prescribed GLP-1 RA following incident stroke in the present study (6.6%) likely reflects the lack of recommendations for the use of these treatments to prevent cardiovascular disease in most of the years covered by this study [6]. Nonetheless, the CAPTURE study demonstrated that patients with previous cardiovascular disease were slightly less likely to be prescribed GLP-1 RA than patients without previous cardiovascular disease (9.5% versus 10.4%) [6]. Similar findings were observed in the SWEDEHEART study [40]. Treatment patterns studies have also demonstrated low utilization of these drugs, including among patients with established cardiovascular disease [41, 42]. In the present study, even the utilization of statins remained very low (30.0%) following stroke, despite clinical guidelines for cardiovascular disease management in T2D populations strongly recommending the use of these agents among people at high risk of cardiovascular disease [17, 43]. Stronger adherence to clinical guidelines through enhanced educational activities remains a key priority to expand the use of cardioprotective drugs in this high-risk population. Furthermore, given that there is some evidence to indicate that glycemic control may be associated with stroke severity [44], improved management of hyperglycemia may have beneficial impacts on the incidence and severity of stroke.
This study has also demonstrated the considerable economic burden associated with stroke in T2D populations. The estimated total yearly medical median costs for people with T2D with stroke was €12,199 (6846–22,378) in the present study. This represents a larger estimate than observed in Scotland for incident cerebrovascular disease for the period 2015–2016 (mean annual costs: £7900 [1900–32,000]) [45]. The total mean annual costs for previous stroke among people with T2D in Sweden was more similar to our estimate at €11,397 [20]. This reflected a cost that was 2.2 times higher than that of people without T2D (€5797) and the costs associated with stroke were greater than the impact of atherosclerotic cardiovascular disease generally [20]. A previous study conducted in the French SNDS reported a mean global reimbursed expenditure of €5500 in 2015 for overall T2D patients [46]. The mean total direct medical cost of €18,592 reported in our current study for people with T2D and stroke aligns with the findings from a systematic review describing a median annual cost per patient for cardiovascular disease 3-times higher than in those for people with T2D without cardiovascular disease [47].
Taken together, these findings emphasize the need for a strong and rigorous primary and secondary prevention of cardiovascular diseases such as stroke in the T2D population.
Strengths and limitations
A major strength of the present study was the use of a large, nationally representative sample of people with T2D and incident stroke. The breadth of the EGB database enabled a comprehensive assessment of the clinical and economic burden of stroke in people with T2D. In particular, the use of this database enabled the comprehensive description of direct medical costs and HCRU including outpatient visits. Despite the breadth of the data, data for key clinical variables including glycated hemoglobin, lipid profiles and blood pressure measurements were unavailable for use to explore the potential explanations for the observed treatment patterns at baseline and following incident stroke. A further limitation of the study was that estimates of stroke recurrence are likely to reflect an underestimate of the true stroke recurrence rate. This is since stroke recurrences occurring within 21 days of index date were excluded from the estimates due to difficulties associated with disentangling separate stroke events using administrative databases [22]. Given that the risk of stroke recurrence is greatest in the immediate poststroke period, a considerable number of recurrent strokes are likely to have been excluded [48].
Another important limitation of this study was that ICD-10 codes were used to identify patient comorbidities and clinical outcomes (e.g., cardiac arrythmias) and, in some cases, may not represent the true prevalence and incidence of these conditions. However, previous studies have shown that ICD-10 codes accurately identify patients with cardiovascular disease such as heart failure [49]. Our study also lacks data regarding intravenous thrombolysis and endovascular treatment reperfusion procedures, or any conservative or minimal invasive surgery. Lastly, these data reflect outcomes and treatments for the period between 2012 and 2019, prior to the availability of SGLT2i in France and clinical guideline updates. As such, these data may not reflect current clinical practice trends. Additional studies are required to explore the impact of the widespread availability of SGLT2i on the outcomes of people with T2D with prior stroke.
Conclusions
The incidence of stroke is high among people with T2D, with ischemic stroke being the most common presentation. Stroke is associated with considerable clinical and economic burden among people with T2D, yet only a low proportion of people living with T2D receive recommended cardiovascular risk reducing therapies as per clinical guidelines. These findings highlight the need for the strengthened and multidisciplinary approach for the management of cardiovascular disease in the T2D population.
Availability of data and materials
Data were shared by the French national health insurance: ‘Caisse Nationale d’Assurance Maladie’ (CNAM).
Abbreviations
- ADA:
-
American Diabetes Association
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- CNAM:
-
Caisse Nationale d’Assurance Maladie
- DPP-4:
-
Dipeptidyl peptidase-4
- EASD:
-
European Association for the Study of Diabetes
- EGB:
-
Echantillon Général des Bénéficiaires
- ESC:
-
European Society of Cardiology
- GLP-1:
-
Glucagon-like peptide 1 receptor
- HCRU:
-
Health Care Resource Utilization
- ICD-10:
-
International Classification of Disease, version 10
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- PAD:
-
Peripheral arterial disease
- RA:
-
Receptor agonist
- RWE:
-
Real-world evidence
- SD:
-
Standard deviation
- SGLT2i:
-
Sodium-glucose-like cotransporter 2 inhibitor
- SNDS:
-
French Système National des Données de Santé
- T2D:
-
Type 2 diabetes
References
Wang L, Li X, Wang Z, Bancks MP, Carnethon MR, Greenland P, Feng Y-Q, Wang H, Zhong VW. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999–2018. JAMA. 2021;326(8):704–16.
Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, Zethelius B, Miftaraj M, McGuire DK, Rosengren A, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379(7):633–44.
Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, Deanfield J, Smeeth L, Timmis A, Hemingway H. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015;3(2):105–13.
Wright AK, Suarez-Ortegon MF, Read SH, Kontopantelis E, Buchan I, Emsley R, Sattar N, Ashcroft DM, Wild SH, Rutter MK. Risk factor control and cardiovascular event risk in people with type 2 diabetes in primary and secondary prevention settings. Circulation. 2020;142(20):1925–36.
McGurnaghan S, Blackbourn LAK, Mocevic E, Haagen Panton U, McCrimmon RJ, Sattar N, Wild S, Colhoun HM. Cardiovascular disease prevalence and risk factor prevalence in type 2 diabetes: a contemporary analysis. Diabet Med. 2019;36(6):718–25.
Mosenzon O, Alguwaihes A, Leon JLA, Bayram F, Darmon P, Davis TME, Dieuzeide G, Eriksen KT, Hong T, Kaltoft MS, et al. CAPTURE: a multinational, cross-sectional study of cardiovascular disease prevalence in adults with type 2 diabetes across 13 countries. Cardiovasc Diabetol. 2021;20(1):154.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83.
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Read SH, McAllister DA, Colhoun HM, Farran B, Fischbacher C, Kerssens JJ, Leese GP, Lindsay RS, McCrimmon RJ, McGurnaghan S, et al. Incident ischaemic stroke and Type 2 diabetes: trends in incidence and case fatality in Scotland 2004–2013. Diabet Med. 2018;35(1):99–106.
Gyldenkerne C, Kahlert J, Olesen KKW, Thrane PG, Sørensen HT, Thomsen RW, Maeng M. Twenty-year temporal trends in risk of ischemic stroke in incident type 2 diabetes: a Danish population-based cohort study. Diabetes Care. 2022;45(9):2144–51.
Echouffo-Tcheugui JB, Xu H, Matsouaka RA, Xian Y, Schwamm LH, Smith EE, Bhatt DL, Hernandez AF, Heidenreich PA, Fonarow GC. Diabetes and long-term outcomes of ischaemic stroke: findings from get with the guidelines-stroke. Eur Heart J. 2018;39(25):2376–86.
Morton JI, Ilomäki J, Wood SJ, Bell JS, Shaw JE, Magliano DJ. One-year readmission and mortality following ischaemic stroke by diabetes status, sex, and socioeconomic disadvantage: an analysis of 27,802 strokes from 2012 to 2017. J Neurol Sci. 2022;434: 120149.
McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, Pratley R, Greenberg M, Wang S, Huyck S, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol. 2021;6(2):148–58.
Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, Lopes RD, McMurray JJV, Pratley RE, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9(10):653–62.
Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, Christodorescu RM, Crawford C, Di Angelantonio E, Eliasson B, et al. 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44(39):4043–140.
American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S125-s150.
Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes H-P, Huikuri H. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD-summary. Diab Vasc Dis Res. 2014;11(3):133–73.
Charbonnel BH, Chen H, Cid-Ruzafa J, Cooper A, Fenici P, Gomes MB, Saraiva GL, Medina J, Nicolucci A, Shestakova MV, et al. Treatment patterns and glycated haemoglobin levels over 36 months in individuals with type 2 diabetes initiating second-line glucose-lowering therapy: the global DISCOVER study. Diabetes Obes Metab. 2023;25(1):46–55.
Lim C-E, Pasternak B, Eliasson B, Danaei G, Ueda P. Use of sodium–glucose co-transporter 2 inhibitors and glucagon-like peptide-1 receptor agonists according to the 2019 ESC guidelines and the 2019 ADA/EASD consensus report in a national population of patients with type 2 diabetes. Eur J Prev Cardiol. 2022;30(8):634–43.
Steen Carlsson K, Faurby M, Nilsson K, Wolden ML. Atherosclerotic cardiovascular disease in type 2 diabetes: a retrospective, observational study of economic and clinical burden in Sweden. Diabetes Ther. 2023;14(8):1357–72.
Bannay A, Chaignot C, Blotière PO, Basson M, Weill A, Ricordeau P, Alla F. The best use of the Charlson comorbidity index with electronic health care database to predict mortality. Med Care. 2016;54(2):188–94.
Stahmeyer JT, Stubenrauch S, Geyer S, Weissenborn K, Eberhard S. The frequency and timing of recurrent stroke: an analysis of routine health insurance data. Dtsch Arztebl Int. 2019;116(42):711–7.
Morton JI, Lazzarini PA, Shaw JE, Magliano DJ. Trends in the incidence of hospitalization for major diabetes-related complications in people with type 1 and type 2 diabetes in Australia, 2010–2019. Diabetes Care. 2022;45(4):789–97.
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820.
Norhammar A, Bodegård J, Nyström T, Thuresson M, Eriksson JW, Nathanson D. Incidence, prevalence and mortality of type 2 diabetes requiring glucose-lowering treatment, and associated risks of cardiovascular complications: a nationwide study in Sweden, 2006–2013. Diabetologia. 2016;59(8):1692–701.
Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson A-M, Miftaraj M, McGuire DK, Sattar N, Rosengren A, Gudbjörnsdottir S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376(15):1407–18.
Ducluzeau PH, Fauchier G, Herbert J, Semaan C, Halimi JM, Angoulvant D, Fauchier L. Prevalence and incidence of cardiovascular and renal diseases in type 1 compared with type 2 diabetes: a nationwide French observational study of hospitalized patients. Diabetes Metab. 2023;49(3): 101429.
Zhang L, Li X, Wolfe CDA, O’Connell MDL, Wang Y. Diabetes as an independent risk factor for stroke recurrence in ischemic stroke patients: an updated meta-analysis. Neuroepidemiology. 2021;55(6):427–35.
Peng Y, Ngo L, Hay K, Alghamry A, Colebourne K, Ranasinghe I. Long-term survival, stroke recurrence, and life expectancy after an acute stroke in Australia and New Zealand from 2008–2017: a population-wide cohort study. Stroke. 2022;53(8):2538–48.
Kallmünzer B, Breuer L, Kahl N, Bobinger T, Raaz-Schrauder D, Huttner HB, Schwab S, Köhrmann M. Serious cardiac arrhythmias after stroke. Stroke. 2012;43(11):2892–7.
Sposato LA, Lam M, Allen B, Shariff SZ, Saposnik G. First-ever ischemic stroke and incident major adverse cardiovascular events in 93 627 older women and men. Stroke. 2020;51(2):387–94.
Bernstein RA, Kamel H, Granger CB, Piccini JP, Katz JM, Sethi PP, Pouliot E, Franco N, Ziegler PD, Schwamm LH, et al. Atrial fibrillation in patients with stroke attributed to large- or small-vessel disease: 3-year results from the STROKE AF randomized clinical trial. JAMA Neurol. 2023;80(12):1277–83.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991;22(8):983–8.
Cheng CY, Hsu CY, Wang TC, Jeng YC, Yang WH. Evaluation of cardiac complications following hemorrhagic stroke using 5-year centers for disease control and prevention (CDC) database. J Clin Med. 2018;7(12):519.
Akyea RK, Georgiopoulos G, Iyen B, Kai J, Qureshi N, Ntaios G. Comparison of risk of serious cardiovascular events after hemorrhagic versus ischemic stroke: a population-based study. Thromb Haemost. 2022;122(11):1921–31.
Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, Rosas SE, Del Prato S, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2022 a consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Rahman A, Alqaisi S, Saith SE, Alzakhari R, Levy R. The impact of glucagon-like peptide-1 receptor agonist on the cardiovascular outcomes in patients with type 2 diabetes mellitus: a meta-analysis and systematic review. Cardiol Res. 2023;14(4):250–60.
Giugliano D, Scappaticcio L, Longo M, Caruso P, Maiorino MI, Bellastella G, Ceriello A, Chiodini P, Esposito K. GLP-1 receptor agonists and cardiorenal outcomes in type 2 diabetes: an updated meta-analysis of eight CVOTs. Cardiovasc Diabetol. 2021;20(1):189.
Scheen AJ. Cardiovascular and renal outcomes with SGLT2 inhibitors: real-life observational studies in older patients with type 2 diabetes: SGLT2 inhibitors in elderly and real life. Diabetes Epidemiol Manag. 2023;10: 100135.
Ritsinger V, Nyström T, Saleh N, Lagerqvist B, Norhammar A. Heart failure is a common complication after acute myocardial infarction in patients with diabetes: a nationwide study in the SWEDEHEART registry. Eur J Prev Cardiol. 2020;27(17):1890–901.
Lingvay I, Aroda VR, Honoré JB, Ersbøll AS, Nystrup Husemoen LL, Jensen AB, Sommer Matthiessen K, Kosiborod MN. Patterns of new glucagon-like peptide-1 receptor agonist use in patients with type 2 diabetes during 2014–2019 from a US database: prescriber and patient characteristics. J Diabetes. 2023;15(2):190–5.
Nanna MG, Kolkailah AA, Page C, Peterson ED, Navar AM. Use of sodium-glucose cotransporter 2 inhibitors and glucagonlike peptide-1 receptor agonists in patients with diabetes and cardiovascular disease in community practice. JAMA Cardiol. 2023;8(1):89–95.
American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes—2018. Diabetes Care. 2017;41(Supplement1):S86–104.
Hjalmarsson C, Manhem K, Bokemark L, Andersson B. The role of prestroke glycemic control on severity and outcome of acute ischemic stroke. Stroke Res Treat. 2014;2014: 694569.
McMeekin P, Geue C, Mocevic E, Hoxer CS, Ochs A, McGurnaghan S, Colhoun HM, Wild SH, Wu O. Subgroup tSDRNE: the cost of prevalent and incident cardiovascular disease in people with type 2 diabetes in Scotland: data from the Scottish care information-diabetes collaboration. Diabet Med. 2020;37(11):1927–34.
Baudot F-O, Aguadé A-S, Barnay T, Gastaldi-Ménager C, Fagot-Campagna A. Impact of type 2 diabetes on health expenditure: estimation based on individual administrative data. Eur J Health Econ. 2019;20:657–68.
Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value in Health. 2018;21(7):881–90.
Moroney JT, Bagiella E, Paik MC, Sacco RL, Desmond DW. Risk factors for early recurrence after ischemic stroke. Stroke. 1998;29(10):2118–24.
Bosco-Lévy P, Duret S, Picard F, Dos Santos P, Puymirat E, Gilleron V, Blin P, Chatellier G, Looten V, Moore N. Diagnostic accuracy of the international classification of diseases, tenth revision, codes of heart failure in an administrative database. Pharmacoepidemiol Drug Saf. 2019;28(2):194–200.
Acknowledgements
Data were provided by the French Caisse Nationale d’Assurance Maladie (CNAM) and its staff involved in the project, in particular the DEMEX team. Support during the data application process was provided by the Health Data Hub. Medical writing support was provided by Stephanie Read from Certara.
Funding
This project was funded by Novo Nordisk.
Author information
Authors and Affiliations
Contributions
KM: Protocol development, Results interpretation, Manuscript editing; LF: Protocol development, Results interpretation, Manuscript editing; NQ: Study design & implementation, Protocol development, Results interpretation, Manuscript editing; AK: Protocol development, Manuscript editing; TB; Protocol development, Data Analysis, Manuscript writing; RK: Data management, Data analysis, Manuscript editing; KK; Study implementation, Protocol development, Manuscript editing; HR: Study Design, Protocol development, Results interpretation, Manuscript editing; CM: Protocol development, Results interpretation, Manuscript editing; LV: Protocol development, Results interpretation, Manuscript editing, SL: Study design, Protocol development, Results interpretation, Manuscript editing; IS: Protocol development, Results interpretation, Manuscript editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the French Health Data Hub. This study is a non-interventional study not involving the human being, leveraging only anonymized structured data, which according to applicable legal requirements do not contain data subject to privacy laws. Hence, obtaining informed consent from patients was not required.
Consent for publication
As this study involved anonymized structured data, which according to applicable legal requirements do not contain data subject to privacy laws, obtaining consent to publish from patients was not required.
Competing interests
K.M. reports consulting fees from Novo Nordisk; honoraria for lectures, presentations, or speaker bureaus from Novo Nordisk, Astra Zeneca, Boehringer-Ingelheim, Eli Lilly, Sanofi, Lifescan, Abbott, and Bayer; and participation to Advisory Board from Novo Nordisk, Sanofi and Amarin. L.F reports consultant activities for Bayer, BMS/Pfizer, Boehringer Ingelheim, Medtronic, Novartis, Novo Nordisk and XO, and speaker activities for AstraZeneca, Bayer, BMS/Pfizer, Boehringer Ingelheim, Boston Scientific, Medtronic, Novartis, Novo Nordisk and Zoll. NQ, AK, RK and KK are full-time employees at Certara, a contract research organization which received consulting fees to independently conduct this study. TB is a former employee at Certara. HR, CM, LV, and SL are all full-time employees of Novo Nordisk. I.S reports consultant activities for Bayer, BMS/Pfizer, Boehringer Ingelheim, Medtronic, Novartis, Novo Nordisk, Bioprojet, Astra-Zeneca, Alexion and speaker activities for AstraZeneca, Bayer, BMS/Pfizer, Boehringer Ingelheim, Medtronic, Novartis, Novo Nordisk.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12933_2024_2257_MOESM1_ESM.pdf
Table S1. Definition of clinical variables. Figure S1. Study design. Figure S2. Flow chart. Figure S3. Time to first cardiovascular event according to incident stroke subtype. Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohammedi, K., Fauchier, L., Quignot, N. et al. Incidence of stroke, subsequent clinical outcomes and health care resource utilization in people with type 2 diabetes: a real-world database study in France: “INSIST” study. Cardiovasc Diabetol 23, 183 (2024). https://doi.org/10.1186/s12933-024-02257-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02257-4