Abstract
Background
The association between the triglyceride glucose (TyG) index and the risk of early-onset atherosclerotic cardiovascular disease (ASCVD) events or all-cause mortality in young and middle-aged people is not fully elucidated.
Methods
The present study included 64,489 young and middle-aged people who participated in the 2006 Kailuan Study physical examination. Multivariate Cox proportional hazards models and restricted cubic spline curves were used to assess the association of TyG index with early-onset ASCVD events and all-cause mortality.
Results
During a median of 11-year follow-up, 1984 (3.08%) participants experienced at least one ASCVD event and 1,392 (2.16%) participants experienced all-cause death. A higher TyG index was significantly associated with a higher risk of early-onset ASCVD events (HR: 1.61, 95% CI 1.38–1.89) and all-cause mortality (HR: 1.39, 95% CI 1.17–1.65), respectively. For each unit increase in TyG index, the risk of early-onset ASCVD events increased by 20%. In addition, there was a non-linear association between the TyG index and early-onset ASCVD events (P for non-linear < 0.01), and a linear association between TyG index and all-cause mortality (P for non-linear = 0.476).
Conclusions
A higher TyG index is significantly associated with an increased incidence of early-onset ASCVD events and all-cause mortality in a young and middle-aged population from North China.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is a major contributor to the global burden of disease affecting over 523 million people globally [1, 2]. Current studies have identified insulin resistance (IR) is one of the most important risk factors for ASCVD [3]. It has been accepted that the hyperinsulinemic-euglycemic clamp technique is the gold standard for assessing IR, however it is not easy to apply this technique on a large scale in the clinic [4]. As a surrogate for IR, the triglyceride-glucose (TyG) index is less expensive and easier to perform. Previous studies have demonstrated that the TyG index is significantly associated with the new-onset ASCVD events in the elderly [5,6,7,8,9]. However, no study has yet to be conducted to investigate the association between the TyG index and the risk of ASCVD events in a young and middle-aged population. Therefore, our study aimed to fill this gap by investigating the association between the TyG index and the risk of early-onset ASCVD events or all-cause mortality in a young and middle-aged population from North China.
Methods
Study participants
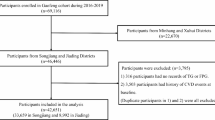
The Kailuan Study is a prospective cohort study conducted in the community of Tangshan, China. The relevant design of the Kailuan study has been described in detail in previous articles [10,11,12]. Here, young and middle-aged participants were defined as males aged less than 55 years or females aged less than 65 years [13]. A total of 101,510 participants initially participated the Kailuan study in the year of 2006, among which, there are 66,180 young and middle-aged participates. We excluded participates who had experienced myocardial infarction (MI) (n = 349), stroke (n = 435), revascularization therapy (n = 33), heart failure (HF) (n = 24) and cancer (n = 166) before baseline enrollment. Except that, 684 subjects who lacked fasting blood glucose (FBG) or triglyceride (TG) data at baseline were further excluded. Finally, a total of 64,489 participants were enrolled in our current study (Fig. 1).
Data collection and definitions
The participants’ demographic characteristics, lifestyle characteristics, medical history, and medication history were collected, respectively. The diagnosis of hypertension was based on a self-reported history of hypertension, a mean blood pressure ≥ 140/90 mmHg on two measurements at physical examination, or a normal blood pressure that was being treated with antihypertensive medication [14]. The diagnosis of diabetes mellitus was based on a self-reported history of diagnosed diabetes mellitus or a FBG ≥ 7.0 mmol/L or normal blood glucose but on hypoglycemic treatment [15]. Blood was collected after fasting for more than 8 h for every participant. Biochemical parameters consist of high-sensitivity C-reactive protein (hs-CRP), high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), TG, and low-density lipoprotein cholesterol (LDL-C) were analyzed using an automated analyzer (Hitachi, Tokyo, Japan). These parameters were monitored by professional quality control personnel to ensure accuracy.
Calculation of the TyG index
The TyG index was calculated as ln [TG (mg/dL) × FBG (mg/dL)/2] [7]. Based on the quartiles of the TyG index, the subjects were divided into four groups: quartile 1 (Q1) (3.61 ≤ TyG < 8.17), quartile 2 (Q2) (8.17 ≤ TyG < 8.57), quartile 3 (Q3) (8.57 ≤ TyG < 9.06), and quartile 4 (Q4) (9.06 ≤ TyG ≤ 12.25).
Outcomes and follow-up
The outcomes observed in this study were ASCVD events and all-cause mortality. Here, ASCVD events consist of MI, ischemic stroke (IS), and revascularization therapy [(coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI)]. MI and IS were identified by ICD-10 codes, CABG and PCI were identified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. All-cause mortality refers to death from any cause. The state of life is obtained through inquiry by the Human Resources and Social Security Bureau of Hebei Province or through direct contact with the participant’s family members. All outcomes were reviewed by medical professionals.
Follow-up visits were conducted annually since the 2006 physical examination. Participants were followed until the first occurrence of any ASCVD events, death, or reaching 55 years old for males or 65 years old for females. The date of the last follow-up visit was December 31, 2021. When all-cause mortality was studied, it was considered as an independent outcome.
Statistical analysis
All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA). Participants were divided into four groups based on the TyG index quartiles. Baseline characteristics are expressed as the mean ± standard deviation or as frequencies and percentages. Incidence densities per 1000 person-years were calculated based on follow-up time and number of events. Incidence curves for ASCVD events, subtypes, and all-cause mortality were plotted using the Kaplan–Meier method, and the log-rank test was used to assess between-group differences in incidence rates. Hazard ratios (HR) and 95% confidence intervals (95% CI) for composite ASCVD events, ASCVD events subtypes and all-cause mortality were calculated using Cox proportional hazards regression modeling, respectively. The proportional risk assumption was assessed by examining the Schoenfeld residuals. P values for trends were calculated using quartiles of changes in the TyG index as an ordinal variable. The robustness of the association between the TyG index and the risk of ASCVD events or all-cause mortality was also analyzed. First, the TyG index was included in the model as a continuous variable. Second, to rule out the potential effect of reverse causality, the main analyses were repeated, excluding participants who developed ASCVD events or all-cause mortality during the first 2 years of follow-up. Subgroup analyses were conducted after stratification by sex, BMI, presence of hypertension, presence of diabetes mellitus, smoking status, and drinking status. Likelihood ratios were used to test for the presence of multiplicative interactions between the TyG index and these variables. In addition, we examined the predictive value of the TyG index for early-onset ASCVD events and all-cause mortality by calculating the C-statistic, net reclassification index (NRI), and integrated discrimination improvement (IDI). A two-sided P < 0.05 was considered to statistical significance.
Results
Characteristics of the study population
The characteristics of 64,489 participants by quartile of the baseline TyG index are shown in Table 1. The patients enrolled in the study had a mean age of 44.9 ± 8.9 years and the percentage of male was 72.07%. The median (IQR) of the baseline TyG index was 8.57 (8.65 ± 0.70). Compared with the lowest quartile group, the higher TyG index groups have more elders, males, smokers and drinkers and with higher prevalence of hypertension, diabetes mellitus, higher usage rate of antihypertensive agents, antidiabetic agents, lipid-lowering agents, higher BMI, SBP, DBP, TC, LDL-C, hs-CRP, lower HDL-C (all P < 0.05).
Association of the TyG index with ASCVD events and all-cause mortality
The median follow-up was 10.8 years (IQR 4.7–14.7 years). During the follow-up period, 1984 participants (3.08%) had composite ASCVD events, with 312 cases of MI, 1104 cases of IS, and 766 revascularization therapies, respectively. A total of 198 patients (0.31%) experienced two or more ASCVD events. In addition, a total of 1392 (2.16%) deaths occurred. The incidence of composite ASCVD events increased from 1.48 (1.31–1.67) per 1000 person-years in Q1 to 5.66 (5.28–6.06) per 1000 person-years in Q4. In addition, the incidence of all-cause mortality also increased from 1.42 (1.25–1.61) per 1000 person-years in Q1 to 3.38 (3.09–3.70) per 1000 person-years in Q4 (Table 2). In addition, the Kaplan-Meier curve revealed that the cumulative incidence of composite ASCVD events, ASCVD events subtypes, and all-cause mortality were higher in Q4 than in the other quartiles (Fig. 2).
Cox regression analysis showed that, compared to Q1, the adjusted HR (95% CI) for composite ASCVD events in Q2–Q4 were 1.30 (1.11–1.52), 1.34 (1.15–1.57), and 1.61 (1.38–1.89), respectively (P for trend < 0.001). The adjusted HR (95% CI) for all-cause mortality in Q2–Q4 were 1.18 (1.00-1.40), 1.16 (0.98–1.38) and 1.39 (1.17–1.65), respectively (P for trend = 0.003). In the analysis of ASCVD event subtypes, a higher TyG index (Q4) was significantly associated with higher risks of MI (HR: 2.46, 95% CI 1.60–3.79) (P for trend < 0.001) and revascularization therapy (HR: 2.37, 95% CI 1.81–3.10) (P for trend < 0.001). However, a higher TyG index was only significantly associated with a higher risk of IS in model 1 (HR: 2.22, 95% CI 1.85–2.67) (P for trend < 0.001) (Table 2).
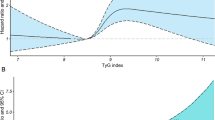
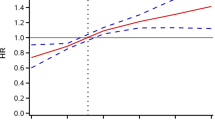
Restricted cubic spline analysis showed that there was a non-linear relationship between the TyG index and the risk of ASCVD events or MI (P for non-linear < 0.01), while there was a linear association between the TyG index and all-cause mortality (P for non-linear = 0.476). However, a significant association between TyG index and IS was not confirmed (Fig. 3).
Restricted cubic splines for the association of TyG index with A ASCVD events, B MI, C IS, D revascularization therapy, E all-cause mortality. A–E adjusted for age, sex, education, smoking status, drinking status, snoring, BMI, SBP, history of hypertension, history of diabetes mellitus, family history of CVD, use of antidiabetic agents, lipid-lowering agents, antihypertensive medications, TC, HDL-C, LDL-C, hs-CRP and the TyG index. Data were fitted using a Cox regression model of restricted cubic spline with three knots (at the 5th, 50th, and 95th percentiles). Adjusting for potential covariates. The reference point for the TyG index was the median of the reference group. Red lines indicate adjusted hazard ratios, and black lines indicate the 95% confidence interval bands
Sensitivity analysis
The sensitivity analysis between the TyG index and incidence of ASCVD events is shown in Table 3. When the TyG index was considered a continuous variable, the risk of ASCVD events increased by 20% (HR: 1.20, 95% CI 1.12–1.28, P < 0.05) and the risk of all-cause mortality increases by 16% (HR: 1.16, 95% CI 1.07–1.26, P < 0.05) with every increase of 1 unit in the TyG index. After excluding participants who occurred events at the first 2-year follow-up, the fully adjusted risk of composite ASCVD events, ASCVD subtypes events and all-cause mortality remained consistent with the main model.
Subgroup analysis
To further investigate the association between the TyG index and ASCVD events or all-cause mortality across diverse population, we stratified the population based on sex, BMI, history of hypertension, history of diabetes mellitus, smoking status and drinking status. The results showed that the association between the TyG index and ASCVD events were stronger in non-smokers (HR: 1.87, 95% CI 1.53–2.29) compared to smokers (HR: 1.31, 95% CI 1.02–1.67) (P for interaction = 0.042), as well as in non-drinkers (HR: 1.91, 95% CI 1.56–2.33) compared to drinkers (HR: 1.25, 95% CI 0.97–1.60) (P for interaction = 0.001). In addition, the association between the TyG index and all-cause mortality were stronger in participants with BMI ≥ 28 (HR: 1.50, 95% CI 0.95–2.35) compared to participants with BMI < 28 (HR: 1.43, 95% CI 1.18–1.73) (P for interaction = 0.010), as well as in participants without hypertension (HR: 1.60, 95% CI 1.27–2.01) compared to participants with hypertension (HR: 1.11, 95% CI 0.86–1.45) (P for interaction = 0.003) (Table 4).
Incremental predictive value of the TyG index
When adjusting TG, FBG, or TyG index into the adjusting models on the base of clinical risk factors, the C-index for predicting ASCVD events were 0.7870 (95% CI 0.7776–0.7963) (P < 0.001), 0.7877 (95% CI 0.7783–0.7970) (P < 0.001), and 0.7883 (95% CI 0.7790–0.7976) (P < 0.001); the category-free NRI were 0.1021 (95% CI 0.0588–0.1454) (P < 0.001), 0.0455 (95% CI 0.0009–0.0902) (P = 0.0459), and 0.1607 (95% CI 0.1160–0.2054) (P < 0.001); the IDI are < 0.0001 (95% CI 0–0.0010) (P = 0.3513), 0.0003 (95% CI 0–0.0.0006) (P = 0.0198), and 0.0004 (95% CI 0.0002–0.0006) (P = 0.0003). Although the C-index for predicting ASCVD events in all models were statistically significant, a statistic significance of the IDI by adjusting TG on the base of clinical risk factors was not confirmed.
When adjusting TG, FBG, or TyG index into the adjusting models on the base of clinical risk factors, the C-index for predicting all-cause mortality are 0.7135 (95% CI 0.7007–0.7263) (P < 0.001), 0.7138 (95% CI 0.7011–0.7266) (P < 0.001), and 0.7143 (95% CI 0.7015–0.7271) (P < 0.001); the category-free NRI are 0.0784 (95% CI 0.0275–0.1293) (P = 0.0038), − 0.0309 (95% CI − 0.0837–0.0218) (P = 0.2536), 0.1235 (95% CI 0.0705–0.1766) (P < 0.001); the IDI are < 0.0001 (95% CI 0–0.0001) (P = 0.0890), 0.0010 (95% CI 0.0005–0.0015) (P < 0.001), and 0.0003 (95% CI 0.0002–0.0005) (P < 0.001). Similarly, although the C-index for predicting all-cause mortality in all models were statistically significant, a statistic significance of the IDI by adjusting TG, the category-free NRI by adjusting FBG were not confirmed (Table 5).
Discussion
For the first time, we revealed that a higher TyG index is significantly correlate to both early-onset ASCVD events and all-cause mortality in a young and middle-aged population from North China. Indeed, the association of the TyG index with early-onset ASCVD events and all-cause mortality in a young and middle-aged population has not been fully elucidated in previous studies. Xu et al. studied 4,754 African American and white adults aged from 18 to 30 years from the CARDIA study. During a median 25-year follow-up, 158 incident CVD events and 246 cases of all-cause mortality were reported, respectively. The results showed that for each one-unit increase in the TyG index, there was a 96% higher risk of CVD (HR: 1.96, 95% CI 1.44–2.66) and an 85% higher risk of all-cause mortality (HR:1.85, 95% CI 1.45–2.36). Individuals in the high TyG index trajectory group had a significantly increased risk of CVD events (HR: 2.35, 95% CI 1.34–4.12) and all-cause mortality (HR: 3.04, 95% CI 1.83–5.07) compared to those in the low TyG index trajectory group [16]. Cho et al. studied 6,675,424 Korean adults aged from 20 to 39. Over an average follow-up period of 7.4 years, there were 8,506 cases of stroke, 12,312 cases of MI, and 22,667 deaths recorded. The highest TyG index quartile indicated a higher risk of stroke (HR: 1.253, 95% CI 1.167–1.346), MI (HR: 1.258, 95% CI 1.187–1.334), and mortality (HR: 1.151, 95% CI 1.104–1.200) compared to those in the lowest TyG index quartile [17].
However, the results of our current study indicated a weak association between TyG index and IS. Inconsistent with our results, Xu et al. studied 35,999 participants from the Kailuan study. The average age of the participants was 30.8 ± 5.7 years, with 77.1% being male. Over a median follow-up period of 11 years, there were 281 stroke events, including 62 cases of hemorrhagic stroke (HS) and 219 cases of IS. After adjusting for relevant confounders in the Cox proportional hazards model, it was found that subjects with higher TyG index groups had significantly higher risks of early-onset stroke [17]. The reason for our deviating findings probably depends on the following points. First, Xu included the participants aged less than 40 years, which are much younger than those in our study. Second, the study outcome in Xu’s study was stroke in broad terms, which consists both HS and IS, however, we only took IS into consideration in our current study. Third, the relevant confounders adjusted in Cox proportional hazard models were the different.
In addition, our results showed that the association between the TyG index and ASCVD events were stronger in non-smokers than smokers, as well as in non-drinkers compared to drinkers. In addition, the association between the TyG index and all-cause mortality were stronger in participants with BMI ≥ 28 than participants with BMI < 28, as well as in participants without hypertension than participants with hypertension. A special attention should be paid for people with those characteristics. However, because the Kailuan group is a company in the coal industry, considerably more males than females were employed, it is unclear whether this finding is applicable to in a general population.
Furthermore, we demonstrated that although the C-index for predicting ASCVD events or all-cause mortality in all models were statistically significant, a statistic significance of the IDI and the category-free NRI was only confirmed by adjusting TyG index rather than TG or FBG alone. Regarding this, Xu et al. assessed the predictive value of a pooled cohort equations model. The results showed that the C index increased from 0.773 to 0.776 (P < 0.001) when taking TyG index into consideration. Moreover, there was a notable improvement in discriminatory power and risk reclassification, with an IDI of 0.010 (95% CI 0.004–0.017) and an NRI of 0.231 (95% CI 0.074–0.389) [16]. In addition, Yao et al. demonstrated that the C-indices of models incorporating TyG for all-cause/non-CV deaths exhibited notably higher predictive values for non-cardiovascular mortality compared to models utilizing TG or FBG alone [18].
Our study has several limitations. First, since the population studied is Chinese, the conclusion applies to the population of Chinese origin. Furthermore, our participants were mainly workers in coal mines in northern China with a higher proportion of males in the population. Therefore, it remains uncertain if the present results are applicable to a general young and middle-aged population. Second, although our results indicated that TyG index improves the prediction of early-onset ASCVD events or all-cause mortality compared to TG and FBG alone, a comparison between TyG index and other IR indices such as homeostatic model assessment for IR was not conducted in our study.
Conclusions
Our study showed that the TyG index is associated with a high risk of early-onset ASCVD events or all-cause mortality in a young and middle-aged population from North China.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CVD:
-
Cardiovascular disease
- TyG:
-
Triglyceride–glucose
- IR:
-
Insulin resistance
References
Collaborators GDI. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuniga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214–223.
Wen J, Pan Q, Du LL, Song JJ, Liu YP, Meng XB, Zhang K, Gao J, Shao CL, Wang WY, et al. Association of triglyceride-glucose index with atherosclerotic cardiovascular disease and mortality among familial hypercholesterolemia patients. Diabetol Metab Syndr. 2023;15(1):39.
Qu H, Long LZ, Chen L, Wu HT, Fu CG, Zhang SS. Triglyceride-glucose index and estimated 10-year risk of a first hard cardiovascular event. Front Cardiovasc Med. 2022;9:994329.
Fiorentino TV, Marini MA, Succurro E, Andreozzi F, Sesti G. Relationships of surrogate indexes of insulin resistance with insulin sensitivity assessed by euglycemic hyperinsulinemic clamp and subclinical vascular damage. BMJ Open Diabetes Res Care. 2019;7(1):e000911.
Liu Y, Zhu B, Zhou W, Du Y, Qi D, Wang C, Cheng Q, Zhang Y, Wang S, Gao C. Triglyceride-glucose index as a marker of adverse cardiovascular prognosis in patients with coronary heart disease and hypertension. Cardiovasc Diabetol. 2023;22(1):133.
Xu W, Zhao H, Han X, Liu J, Li H, Sun J, Xing A, Chen S, Wu S, Wu Y. Relationship between early-onset stroke and triglyceride-glucose index among young Chinese adults. Lipids Health Dis. 2023;22(1):3.
Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, Wang A. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20(1):19.
Wang A, Tian X, Zuo Y, Chen S, Meng X, Wu S, Wang Y. Change in triglyceride-glucose index predicts the risk of cardiovascular disease in the general population: a prospective cohort study. Cardiovasc Diabetol. 2021;20(1):113.
Wu Y, Liu Q, Ma Y, Han X, Zhao X, Zhao H, Song M, Sun J, Wang X, Wu S. Effect of parental arterial stiffness in offspring: the Kailuan study. J Hypertens. 2022;40(1):102–7.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 2019;139(25):e1082-143.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–52.
American Diabetes Association. Classification and diagnosis of diabetes standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S15-33.
Xu X, Huang R, Lin Y, Guo Y, Xiong Z, Zhong X, Ye X, Li M, Zhuang X, Liao X. High triglyceride-glucose index in young adulthood is associated with incident cardiovascular disease and mortality in later life: insight from the CARDIA study. Cardiovasc Diabetol. 2022;21(1):155.
Cho YK, Han KD, Kim HS, Jung CH, Park JY, Lee WJ. Triglyceride–glucose index is a useful marker for predicting future cardiovascular disease and mortality in young Korean adults: a nationwide population-based cohort study. J Lipid Atheroscler. 2022;11(2):178–86.
Yao Y, Wang B, Geng T, Chen J, Chen W, Li L. The association between TyG and all-cause/non-cardiovascular mortality in general patients with type 2 diabetes mellitus is modified by age: results from the cohort study of NHANES 1999–2018. Cardiovasc Diabetol. 2024;23(1):43.
Acknowledgements
The authors thank the investigators who made this cohort study possible.
Funding
This study was supported by the Hebei Provincial Medical Science Research Project (No. 20221802).
Author information
Authors and Affiliations
Contributions
Qiqi Hou, Qi Qi, and Shuohua Chen made substantial contributions to data collection, data analysis and manuscript writing. Shouling Wu, Quanle Han, and Kangbo Li made substantial contributions to the study design and intellectual direction. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project protocol was approved by the ethics committee of the Ethics Committee of the Kailuan Medical Group and was approved by the guidelines of the Helsinki Declaration, and all study individuals in this project signed an informed consent form at enrollment.
Consent for publication
If the manuscript is accepted, we approve it for publication in Cardiovascular Diabetology.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hou, Q., Qi, Q., Han, Q. et al. Association of the triglyceride-glucose index with early-onset atherosclerotic cardiovascular disease events and all-cause mortality: a prospective cohort study. Cardiovasc Diabetol 23, 149 (2024). https://doi.org/10.1186/s12933-024-02249-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02249-4