Abstract
Background
Triglyceride-glucose index (TyG) has been widely used to predict cardiovascular outcomes. However, it remains unclear whether TyG holds prognostic significance for patients with coronary chronic total occlusions (CTO). Thus, our study aimed to evaluate the predictive accuracy and prognostic value of TyG in individuals who underwent successful percutaneous coronary intervention (PCI) for CTO.
Methods
A total of 331 consecutive patients with ≥ 1 successful CTO-PCI were included. The baseline and angiographic data were acquired. The duration of follow-up ranged from 32 to 79 months, with a median of 44 months and an interquartile range of 39 to 67 months. The primary outcome measured was the occurrence of major adverse cardiac and cerebrovascular events (MACCE), including mortality, target vessel revascularization, recurrent myocardial infarction, and stroke.
Results
After controlling for confounders, multivariate Cox regression analysis revealed that TyG remained statistically significant, regardless of being a continuous or categorical variable. In the partially adjusted regression model, the Hazard ratio (95%CI) for MACCE was 2.54 (1.12–5.79) in tertile 3 and 1.61 (1.22–2.12) per SD increase in the TyG.Kaplan-Meier survival analysis demonstrated significant differences in MACCE-free survival rates across tertiles of the TyG, as indicated by the log-rank test (p = 0.001). ROC analysis was conducted to evaluate the predictive ability of TyG for MACCE, resulting in an AUC of 0.677.
Conclusion
The TyG index demonstrates independent predictive capabilities for MACCE in patients who have undergone successful CTO-PCI. These findings suggest that TyG holds the potential as a valuable tool in risk stratification and the identification of patients who may benefit from early intervention in the management of CTO.
Similar content being viewed by others
Introduction
Coronary artery disease (CAD) is a global health burden, and within CAD, coronary chronic total occlusion (CTO) is observed in approximately 15–25% of patients undergoing coronary angiography [1, 2]. Despite the progression of percutaneous coronary intervention (PCI) technique, the prognosis of patients with CTO is often poor. Emerging evidence suggests that successful CTO-PCI is associated with several benefits compared to unsuccessful CTO-PCI and optimal medical treatment alone [3, 4]. These benefits include improvements in ventricular function, quality of life, and symptoms. However, the long-term prognosis of CTO-PCI remains a topic of debate, particularly for patients with metabolic abnormalities [2, 5, 6].
Metabolic abnormalities are important risk factors for CAD and cardiovascular adverse outcomes, in which insulin resistance (IR) plays a core role [7,8,9]. Although the homeostasis model assessment of insulin resistance (HOMA-IR) and the hyperinsulinemic-euglycemic clamp are established tools for evaluating IR, they are not commonly used in routine clinical practice. This is primarily due to several practical limitations, including complexity, time consumption, and cost. Triglyceride-glucose index (TyG) is a surrogate parameter that has been proposed as an indicator of IR. It is a simple calculation derived from fasting triglyceride (TG) and fasting blood glucose (FBG) levels [9, 10]. Considerable evidence suggests that TyG is superior to the HOMA-IR model in predicting arterial stiffness and metabolic syndrome [11, 12]. Moreover, TyG index has been shown to be associated with the incidence of cardiovascular diseases and their complications [13,14,15].
Previous studies have reported the association between TyG and adverse prognosis in different subgroups of CAD patients [15,16,17]. However, the prognostic values of TyG index have not been fully explored among patients with CTO,especially in successful CTO-PCI patients. As an important sub-type of CAD, it is urgently needed to investigate a valuable tool in risk stratification and the identification of CTO patients who may benefit from early intervention.Hence, the present study aimed to investigate the relationship between TyG index and prognostic outcomes in patients who have undergone successful PCI for CTO.
Methods
Study population
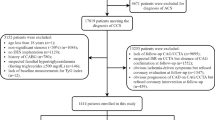
This retrospective cohort study was performed in compliance with the Declaration of Helsinki after obtaining approval from the Ethics Review Committee of the same university. From January 2016 to December 2019, 566 consecutive patients with ≥ 1 CTO lesion who received PCI treatment in the catheterization room were recruited. CTO lesions were characterized by total obstruction of the coronary artery, resulting in a complete absence of forward blood flow according to the thrombolysis in MI (TIMI) flow grade 0 criteria, with a duration of more than 3 months [18].
The following exclusion criteria were used: (1) patients with failed CTO-PCI (n = 127); (2) patients without triglyceride (TG) and fasting plasma glucose (FPG) data (n = 8); (3) patients diagnosed with acute ST-elevation MI within 72 h prior to admission (n = 11). Therefore, out of the initial 420 patients, a follow-up was conducted between July 2022 and August 2022 via telephone. A total of 331 patients (78.8%) successfully completed the follow-up (Fig. 1).
Data collection and definitions
Demographic, clinical and angiographic information were acquired from medical records by trained clinicians who were unaware of the study objective. Peripheral venous blood was sampled before the coronary procedure in the morning following a minimum 8 h of fasting to determine blood biochemical parameters. TyG was measured as Ln [FPG (mg/dL) × fasting TG (mg/dL) / 2] [10]. SYNTAX scores were used to assess the severity of CAD. Multivessel disease was characterized by the presence of significant (> 50% diameter) stenosis in a minimum of two major coronary arteries. Poor coronary collateral circulation(CCC) (Grades 0 and 1) was grouped according to the Rentrop classification [19]. DM was evaluated based on the following criteria: FPG levels ≥ 7.0 mmol/L, random blood glucose (RBG) levels ≥ 11.1 mmol/L, 2-h plasma glucose levels after an oral glucose tolerance test (OGTT) ≥ 11.1 mmol/L, or the utilization of insulin or oral hypoglycemic agents [20]. Hyperlipidemia was characterized using the ICD-10 code E78 in combination with lipid-lowering medications or a total cholesterol level of ≥ 240 mg/dL [21]. Hypertension was described as having a systolic blood pressure of ≥ 140 mmHg or higher and/or a diastolic blood pressure of ≥ 90 mmHg, or being treated with antihypertensive drugs [22].
PCI
The procedures for CTO-PCI were carried out by experienced cardiac intervention experts according to the current standard guidelines. Indications for coronary revascularization were based on symptomatic angina and/or positive results on functional ischemia studies.The success of the PCI procedure was determined based on the achievement of residual stenosis of less than 30% with TIMI flow grade 3 at the conclusion of the procedure,without any periprocedural complications.Following PCI, a standard dual-antiplatelet medication regimen was continued for a minimum of 12 months.The details of risk factor management after PCI were in accordance with current guidelines on myocardial revascularization [23].The treatment targets such as LDL-C and blood pressure are precisely managed according to each patient’s comorbidities and specific risk classification.The dosages of all medications were maximized to meet the recommendations as allowed by heart rate, blood pressure, and side effects in the absence of justifiable relative contraindications.
Endpoints
MACCE occurrence was the primary endpoint of this study, which consisted of non-fatal stroke (hemorrhagic, ischemic, or unspecified), target vessel revascularization(TVR), non-fatal MI, and all-cause mortality (cardiac or non-cardiac mortality). The diagnosis of MI was defined in accordance with the criteria outlined in the Third Universal Definition [24]. TVR was specifically defined as the need for revascularization of the target vessel, which could be accomplished through PCI or coronary artery bypass grafting [25]. The information of target lesion revascularization (TLR) and any revascularization were also recorded. TLR has defned repeat revascularization at the same CTO lesion.Any revascularization was defined as any unplanned revascularization in follow up, including non-target vessels.
Statistical analysis
Categorical data were presented with frequency or percentage, and were analyzed with the chi-square test or Fisher exact test accordingly. Continuous data were expressed as mean ± standard deviation (SD) or median (P25 and P75), as appropriate. In the case of a non-Gaussian distribution, the Kruskal-Wallis H test or Mann-Whitney U test was employed, whereas for a Gaussian distribution, the Student’s t-test or ANOVA test was used. Spearman or Pearson correlation analysis was conducted to investigate the relationships between TyG and cardiovascular risk factors. The survival curves were drawn by the Kaplan-Meier approach, and the differences between the two curves were compared by Log-rank. Multivariate Cox regression analysis was conducted to evaluate the independent correlation between TyG index and MACCE occurrence. Two regression models were constructed: model 1 (adjusted for gender and age), and model 2 (a partially adjusted model that included variables with p < 0.05 in univariate analysis). Subgroup analysis was performed based on gender, diabetes mellitus (DM), hypertension, hyperlipidemia, multi-CTO, and multivessel involvement to investigate potential differences in the relationship between TyG and MACCE among different subgroups. The p-value for interaction was determined to assess the significance of subgroup differences. Receiver operating characteristic (ROC) curves were obtained, and the area under the curve (AUC) was measured. Statistical analyses were conducted with SPSS v25.0 and R v4.1.3. Two-tailed P < 0.05 was deemed statistically significant.
Results
Baseline features
This study included 331 patients with successful CTO-PCI (mean age = 64.50 ± 10.36 years). All patients were assigned to three groups based on the tertile of TyG index level: TyG < 8.57 (tertile 1,n = 110); 8.57 ≤ TyG < 9.07 (tertile 2,n = 111) and TyG ≥ 9.07 (tertile 3,n = 110). Significant differences could be found in age, FPG, HDL-C, TC, TG, the proportion of DM, hypertension, hyperlipidemia, multiple CTO lesions, hypoglycemic drugs use, MACCE, and LCX lesion among the three groups. No significant difference was observed for the secondary endpoints and other indicators (Table 1).
Correlation between TyG index and cardiovascular risk factors
TyG was negatively correlated with age and HDL-C, while positively correlated with FPG, BMI, TG, TC, and eGFR (p < 0.05). No significant correlation was found between the TyG and LVEF, LDL-C, UA and SYNTAX score (Table 2).
TyG index and MACCE
All patients were followed-up for a period ranging from 32 to 79 months, with a median follow-up of 44 months and an interquartile range of 39 to 67 months. During this follow-up period, there were 53 cases of MACCEs, which accounted for 16.0% of the study population. These MACCEs consisted of 11 cases of non-fatal stroke (3.3%), 20 cases of coronary artery revascularization (6.0%), 5 cases of non-fatal MI (1.5%), and 17 cases of all-cause death (5.1%). The cumulative incidence of MACCE-free survival across tertiles of TyG was analyzed using Kaplan-Meier survival plots. The log-rank test demonstrated an obvious difference in the cumulative incidence of MACCE-free survival between the tertiles (p = 0.001), as depicted in Fig. 2. Furthermore, univariate Cox regression analysis was conducted to identify risk factors for MACCE. The analysis found that several factors were associated with an increased risk of MACCE, including DM, hypertension, FPG, TG, UA, use of hypoglycemic drugs, and TyG. Notably, the unadjusted HR (95%CI) for the probability of MACCE increased by one SD in TyG was 1.69 (1.33–2.15) (Supplementary Table 1).
After controlling for confounders, multivariate Cox regression analysis revealed that TyG remained statistically significant, regardless of being a continuous or categorical variable. In the partially adjusted regression model, the risk of MACCE elevated by 61% for each SD increase in TyG (HR = 1.61; 95%CI: 1.22–2.12). The partially adjusted HRs for MACCE in the middle and highest tertiles were 1.92 (95%CI: 0.84–4.40) and 2.54 (95%CI: 1.12–5.79), respectively, when compared to those in the lowest tertile. The results demonstrated a statistically significant trend of increased MACCE risk from tertile 1 to tertile 3 (ptrend=0.026). (Table 3).
The prognostic performance of TyG index
Subgroup analyses were conducted to examine the association between TyG and MACCE in specific subgroups of the study population. While no interaction was detected between TyG and gender, hypertension, DM, dyslipidemia, and multi-CTO for the incidence of MACCE (all p ≥ 0.202), a substantial connection between TyG and MACCE was found primarily among single CTO, patients with hypertension and patients without DM (Fig. 3). ROC analyses were carried out to further analyze the prognostic performance of TyG, yielding an AUC of 0.677 (95% CI 0.597–0.754)(Fig. 4). The AUC value of triglyceride and glucose levels were also calculated (Fig. 4).The interaction analysis of blood triglyceride and glucose in a COX regression for MACE found no interaction between them(p = 0.407).After analyze these points,the results show that TyG is more effective than triglyceride or blood glucose level alone.
Discussion
To our knowledge, this is the first study that focuses on the relationship between TyG index and adverse outcomes in successful CTO-PCI patients. The following results were obtained: (1) TyG was markedly associated with traditional cardiovascular risk actors. (2) TyG was independently related to increased risk of MACCE in successful CTO-PCI patients. (3) The significant relationship between TyG index and MACCE was primarily found among single CTO, patients with hypertension, and patients without DM. Overall, TyG index proves to be a predictive indicator for patients after successful recanalization of CTO.
Despite the advancements in interventional devices and techniques for treating CTO, patients still face a significant risk of cardio-cerebrovascular events. Existing research has demonstrated that patients with CTO experience poorer prognosis compared to those without CTO [26]. In addition, metabolic abnormalities are important risk factors for the increased adverse prognosis after PCI equivalent of CTO [27]. As a core of metabolic abnormalities, IR contributes to cardiovascular disease by causing endothelial dysfunction, oxidative stress, and systemic inflammation [28,29,30]. In this context, TyG, a straightforward surrogate marker for IR, has been established as a prognostic indicator for CAD [31, 32]. Moreover, emerging studies have demonstrated a potential association between TyG and cardiovascular events in patients undergoing PCI [33, 34]. Zhu et al. reported that TyG was related to in-stent restenosis in ACS patients who underwent PCI [35]. Jiao et al. identified TyG as an independent predictor of long-term adverse outcomes in older ACS patients [16].Previous studies have also explored the role of TyG in predicting adverse outcomes in patients with CTO [36, 37]. However, after subgroup analysis, it was found that the prognosis of TyG for successful or failed CTO-PCI is still controversial. Therefore,the present study was dedicated to uncover the prognostic value of TyG in successfully treated CTO-PCI patients.
The exact mechanism underlying the association between TyG index and cardiovascular disease prognosis is remain unclear. The TyG index is a reliable marker of IR, which may contribute to the association.IR causes imbalanced glucose metabolism and chronic hyperglycemia, resulting in oxidative stress and inflammation that contributes to atherosclerosis and plaque progression [38].Moreover, IR can cause oxidative stress,endothelial disruption, systemic inflammation, clotting imbalance, poor myocardial reperfusion, and adverse vascular remodeling, all of which can compromise cardiac system [14, 38,39,40].IR, was also strongly associated with the prevalence and progression of coronary artery calcification ,which could be another important mechanism [41].The present study revealed significant associations between TyG and other risk factors. Previous research has also identified connections between TyG and renal insufficiency, dyslipidemia, and obesity [15, 42]. These correlations may partially explain the prediction of TyG on cardiovascular events.Taken together, these findings provide a plausible explanation for why a high TyG could predict cardiovascular events in patients with CTO.
Similarly, the association between TyG index and MACCE was found to be significant only in non-diabetic patients [32]. In patients with DM, accurately determining TyG becomes challenging due to the use of hypoglycemic agents. Moreover, in patients with DM, classical risk factors are the main predictors of cardiovascular events, and the role of IR alone is relatively weak [43]. Interestingly, our study revealed a significant association between TyG and MACCE primarily in patients with hypertension, which contradicts previous findings [32]. This discrepancy may be attributed to differences in data characteristics. Both TyG and IR can be influenced by different antihypertensive drugs [44]. Moreover, epidemiological studies have documented that IR predispose to hypertension [45]. The limited predictive value of TyG in patients with multiple CTOs may be attributed to the fact that these cases involve advanced coronary lesions with a higher burden and often coincide with more severe risk factors. These factors potentially explain some of the inconsistencies in the predictive power of TyG observed in this study.
As an indicator of glucose metabolism, TyG has been widely studied for the value in predicting the risk of CAD and evaluating prognosis [16, 33, 34].Notably,other indices of impaired glucose metabolism such as stress-induced hyperglycemia may hold prognostic value in patients with CTO, given their established association with adverse angiographic outcomes in patients with AMI [37, 46, 47].Further research could be designed to explore these indices to identify valuable tool in risk stratification and the identification of patients who may benefit from early intervention in the management of CTO.
Nevertheless, the present study has several limitations. Firstly, the sample size was limited due to the retrospective design conducted at a single center.Number of cardiovascular events which occurred during follow-up was also small,which might limit a sound statistical analysis and made it difficult to elaborate the associations between the TyG index and the individual components of MACCE.The results of stratified analysis for such a small number of participants or events need to be interpreted with caution. Secondly, despite performing multivariate analysis, there may still be unadjusted confounders that could impact the observed associations. Thirdly, the laboratory parameters were only assessed once at admission, and longitudinal data during follow-up were not systematically collected. Lastly, this study did not account for nutritional status and lifestyle factors, which could potentially influence TyG and outcomes. To strengthen the conclusions drawn from this research, further prospective multi-center studies with larger sample sizes are needed.
Conclusion
In summary, TyG index could potentially be a predictor of MACCE in patients who undergo successful PCI for CTO. This finding highlights the significance of TyG as a simple and robust tool for predicting prognosis in CTO patients. By incorporating TyG index into clinical practice, healthcare professionals could potentially identify high-risk patients and implement appropriate measures to improve outcomes in this population.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- UA:
-
Uric acid
- HDL-C:
-
High-density lipoprotein cholesterol
- TyG:
-
Triglyceride-glucose
- CTO:
-
Coronary chronic total occlusion
- MACE:
-
Major adverse cardiovascular event
- TVR:
-
Target vessel revascularization
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curves
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- OR:
-
Odds ratio
- CI:
-
Confdence interval
- BMI:
-
Body mass index
- LVEF:
-
Left ventricle ejection fraction
- MI:
-
Myocardial infarction
- FH-CAD:
-
Family history of coronary artery disease
- DM:
-
Diabetes mellitus
- FPG:
-
Fasting plasma glucose
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL-C:
-
Low-density lipoprotein-cholesterol
- eGFR:
-
Estimated glomerular filtration rate
- CCC:
-
Coronary collateral circulation
References
Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59(11):991–7.
Tomasello SD, Boukhris M, Giubilato S, Marza F, Garbo R, Contegiacomo G, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions. Eur Heart J. 2015;36(45):3189–98.
Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39(26):2484–93.
Zhao S, Chen Y, Wang Q, Zhu B, Wei Z, Wang Z, et al. Benefits of successful percutaneous coronary intervention in chronic total occlusion patients with Diabetes. Cardiovasc Diabetol. 2022;21(1):271.
Lee SW, Lee PH, Ahn JM, Park DW, Yun SC, Han S, et al. Randomized Trial evaluating percutaneous coronary intervention for the Treatment of Chronic Total Occlusion. Circulation. 2019;139(14):1674–83.
van Veelen A, Elias J, van Dongen IM, Hoebers LPC, Claessen B, Henriques JPS. Percutaneous coronary intervention versus medical therapy for chronic total coronary occlusions: a systematic review and meta-analysis of randomised trials. Neth Heart J. 2021;29(1):30–41.
Beverly JK, Budoff MJ, Atherosclerosis. Pathophysiology of insulin resistance, hyperglycemia, hyperlipidemia, and inflammation. J Diabetes. 2020;12(2):102–4.
Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and Atherosclerosis. Cell Metab. 2011;14(5):575–85.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Abbasi F, Reaven GM. Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides x glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism. 2011;60(12):1673–6.
Son DH, Lee HS, Lee YJ, Lee JH, Han JH. Comparison of triglyceride-glucose index and HOMA-IR for predicting prevalence and incidence of metabolic syndrome. Nutr Metab Cardiovasc Dis. 2022;32(3):596–604.
Wang S, Shi J, Peng Y, Fang Q, Mu Q, Gu W, et al. Stronger association of triglyceride glucose index than the HOMA-IR with arterial stiffness in patients with type 2 Diabetes: a real-world single-centre study. Cardiovasc Diabetol. 2021;20(1):82.
Li H, Zuo Y, Qian F, Chen S, Tian X, Wang P, et al. Triglyceride-glucose index variability and incident Cardiovascular Disease: a prospective cohort study. Cardiovasc Diabetol. 2022;21(1):105.
Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in Cardiovascular Diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68.
Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with Diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):80.
Jiao Y, Su Y, Shen J, Hou X, Li Y, Wang J, et al. Evaluation of the long-term prognostic ability of triglyceride-glucose index for elderly acute coronary syndrome patients: a cohort study. Cardiovasc Diabetol. 2022;21(1):3.
Luo E, Wang D, Yan G, Qiao Y, Liu B, Hou J, et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation Myocardial Infarction after percutaneous coronary intervention. Cardiovasc Diabetol. 2019;18(1):150.
Di Mario C, Mashayekhi KA, Garbo R, Pyxaras SA, Ciardetti N, Werner GS. Recanalisation of coronary chronic total occlusions. EuroIntervention. 2022;18(7):535–61.
Cohen M, Sherman W, Rentrop KP. Determinants of collateral filling observed during sudden controlled coronary artery occlusion in human subjects. J Am Coll Cardiol. 1989;13(2):297–303.
American Diabetes A. 2. Classification and diagnosis of Diabetes: standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):14–S31.
Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic Cardiovascular Disease: a population-based study. BMC Med. 2020;18(1):361.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial Hypertension. Eur Heart J. 2018;39(33):3021–104.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of Myocardial Infarction. J Am Coll Cardiol. 2012;60(16):1581–98.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–51.
Rangaswami J, Soman S, McCullough PA. Key updates in Cardio-Nephrology from 2018: springboard to a bright future. Rev Cardiovasc Med. 2018;19(4):113–6.
Wang P, Yuan D, Jia S, Zhu P, Zhang C, Liu Y, et al. 5-Year clinical outcomes of successful recanalisation for coronary chronic total occlusions in patients with or without type 2 Diabetes Mellitus. Front Cardiovasc Med. 2021;8:691641.
Di Pino A, DeFronzo RA. Insulin resistance and Atherosclerosis: implications for insulin-sensitizing agents. Endocr Rev. 2019;40(6):1447–67.
Lambie M, Bonomini M, Davies SJ, Accili D, Arduini A, Zammit V. Insulin resistance in Cardiovascular Disease, uremia, and peritoneal dialysis. Trends Endocrinol Metab. 2021;32(9):721–30.
Raghavan VA. Insulin resistance and Atherosclerosis. Heart Fail Clin. 2012;8(4):575–87.
Luo JW, Duan WH, Yu YQ, Song L, Shi DZ. Prognostic significance of triglyceride-glucose index for adverse Cardiovascular events in patients with coronary artery Disease: a systematic review and Meta-analysis. Front Cardiovasc Med. 2021;8:774781.
Wu Z, Liu L, Wang W, Cui H, Zhang Y, Xu J, et al. Triglyceride-glucose index in the prediction of adverse cardiovascular events in patients with premature coronary artery Disease: a retrospective cohort study. Cardiovasc Diabetol. 2022;21(1):142.
Hu C, Zhang J, Liu J, Liu Y, Gao A, Zhu Y, et al. Discordance between the triglyceride glucose index and fasting plasma glucose or HbA1C in patients with acute coronary syndrome undergoing percutaneous coronary intervention predicts cardiovascular events: a cohort study from China. Cardiovasc Diabetol. 2020;19(1):116.
Zhao Q, Zhang TY, Cheng YJ, Ma Y, Xu YK, Yang JQ, et al. Triglyceride-glucose index as a surrogate marker of insulin resistance for Predicting Cardiovascular outcomes in nondiabetic patients with Non-ST-Segment elevation Acute Coronary Syndrome undergoing percutaneous coronary intervention. J Atheroscler Thromb. 2021;28(11):1175–94.
Zhu Y, Liu K, Chen M, Liu Y, Gao A, Hu C, et al. Triglyceride-glucose index is associated with in-stent restenosis in patients with acute coronary syndrome after percutaneous coronary intervention with drug-eluting stents. Cardiovasc Diabetol. 2021;20(1):137.
Li Y, He S, Wu Z, Li W, Jian W, Cheng Z, et al. The predictive value of the triglyceride-glucose index for cardiovascular events in patients with coronary chronic total occlusion. Cardiovasc Diabetol. 2022;21(1):149.
Song Y, Cui K, Yang M, Song C, Yin D, Dong Q, et al. High triglyceride-glucose index and stress hyperglycemia ratio as predictors of adverse cardiac events in patients with coronary chronic total occlusion: a large-scale prospective cohort study. Cardiovasc Diabetol. 2023;22(1):180.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of Cardiovascular Disease. Cardiovasc Diabetol. 2018;17(1):122.
Markus MRP, Rospleszcz S, Ittermann T, Baumeister SE, Schipf S, Siewert-Markus U, et al. Glucose and insulin levels are associated with arterial stiffness and concentric remodeling of the heart. Cardiovasc Diabetol. 2019;18(1):145.
da Silva AA, do Carmo JM, Li X, Wang Z, Mouton AJ, Hall JE. Role of hyperinsulinemia and insulin resistance in Hypertension: metabolic syndrome revisited. Can J Cardiol. 2020;36(5):671–82.
Won KB, Park EJ, Han D, Lee JH, Choi SY, Chun EJ, et al. Triglyceride glucose index is an Independent predictor for the progression of coronary artery calcification in the absence of heavy coronary artery calcification at baseline. Cardiovasc Diabetol. 2020;19(1):34.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, et al. Relationship between the triglyceride-glucose index and risk of Cardiovascular Diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21(1):124.
Nelson AJ, Peterson ED, Pagidipati NJ. Atherosclerotic Cardiovascular Disease and Heart Failure: determinants of risk and outcomes in patients with Diabetes. Prog Cardiovasc Dis. 2019;62(4):306–14.
Mancusi C, Izzo R, di Gioia G, Losi MA, Barbato E, Morisco C. Insulin resistance the Hinge between Hypertension and Type 2 Diabetes. High Blood Press Cardiovasc Prev. 2020;27(6):515–26.
Jia G, Sowers JR. Hypertension in Diabetes: an update of Basic mechanisms and Clinical Disease. Hypertension. 2021;78(5):1197–205.
Stalikas N, Papazoglou AS, Karagiannidis E, Panteris E, Moysidis D, Daios S, et al. Association of stress induced hyperglycemia with angiographic findings and clinical outcomes in patients with ST-elevation Myocardial Infarction. Cardiovasc Diabetol. 2022;21(1):140.
Chu J, Tang J, Lai Y, Gao Y, Ye Z, Guan C, et al. Association of stress hyperglycemia ratio with intracoronary thrombus burden in diabetic patients with ST-segment elevation Myocardial Infarction. J Thorac Dis. 2020;12(11):6598–608.
Acknowledgements
We are grateful to the research team.
Funding
This work was supported by funding from the Anhui Natural Science Foundation of China (grant number:2008085MH239).
Author information
Authors and Affiliations
Contributions
YY, MQM, JZ and XHL contributed to the study design and interpretation of the results. YY, SYJ, JZ, LJ and MQM contributed to the collection, analysis, or interpretation of data. YY prepared the manuscript. YY, MQM,JZ, LJ,DXZ and XHL critically revised the manuscript. All authors read and approved the final submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Committee of the First Affiliated Hospital of Anhui Medical University and followed the principles of the Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent for publication
All authors provide consent for publication of this paper.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Ma, M., Zhang, J. et al. Triglyceride-glucose index in the prediction of clinical outcomes after successful recanalization for coronary chronic total occlusions. Cardiovasc Diabetol 22, 304 (2023). https://doi.org/10.1186/s12933-023-02037-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-02037-6