Abstract
Background
Several large observational prospective studies have reported a protection by the traditional Mediterranean diet against type 2 diabetes, but none of them used yearly repeated measures of dietary intake. Repeated measurements of dietary intake are able to improve subject classification and to increase the quality of the assessed relationships in nutritional epidemiology. Beyond observational studies, randomized trials provide stronger causal evidence. In the context of a randomized trial of primary cardiovascular prevention, we assessed type 2 diabetes incidence according to yearly repeated measures of compliance with a nutritional intervention based on the traditional Mediterranean diet.
Methods
PREDIMED (‘‘PREvención con DIeta MEDiterránea’’) was a Spanish trial including 7447 men and women at high cardiovascular risk. We assessed 3541 participants initially free of diabetes and originally randomized to 1 of 3 diets: low-fat diet (n = 1147, control group), Mediterranean diet supplemented with extra virgin olive (n = 1154) or Mediterranean diet supplemented with mixed nuts (n = 1240). As exposure we used actual adherence to Mediterranean diet (cumulative average), yearly assessed with the Mediterranean Diet Adherence Screener (scoring 0 to 14 points), and repeated up to 8 times (baseline and 7 consecutive follow-up years). This score was categorized into four groups: < 8, 8–< 10, 10– < 12, and 12–14 points. The outcome was new-onset type 2 diabetes.
Results
Multivariable-adjusted hazard ratios from time-varying Cox models were 0.80 (95% confidence interval, 0.70–0.92) per + 2 points in Mediterranean Diet Adherence Screener (linear trend p = .001), and 0.46 (0.25–0.83) for the highest (12–14 points) versus the lowest (< 8) adherence. This inverse association was maintained after additionally adjusting for the randomized arm. Age- and sex-adjusted analysis of a validated plasma metabolomic signature of the Mediterranean Diet Adherence Screener (constituted of 67 metabolites) in a subset of 889 participants also supported these results.
Conclusions
Dietary intervention trials should quantify actual dietary adherence throughout the trial period to enhance the benefits and to assist results interpretation. A rapid dietary assessment tool, yearly repeated as a screener, was able to capture a strong inverse linear relationship between Mediterranean diet and type 2 diabetes.
Trial registration ISRCTN35739639
Similar content being viewed by others
Background
Diabetes prevention represents an uppermost priority for public health, with an expected global number of 643 million of persons with diabetes by 2030 [1]. Dietary habits are powerful determinants of diabetes risk [2]. Observational studies consistently reported inverse associations between the traditional Mediterranean diet (MedDiet) [3] and type 2 diabetes [4,5,6]. In particular, the MedDiet and the Mediterranean lifestyle are associated with lower frequency of metabolic syndrome and reduced all-cause mortality in Spain [7]. Even a modest increase in adherence to the MedDiet is linked to a decreased incidence of type 2 diabetes [8]. In addition to other mechanisms, the MedDiet has been reported to reduce advanced glycation end-products [9, 10]. In one center of the ‘‘Prevención con Dieta Mediterránea’’ (PREDIMED) trial, nut consumption, a component of the MedDiet pattern, was reported to be associated with a shift of the lipoprotein subfraction profile to a less atherogenic pattern, as well as with lower circulating concentrations of branched-chain aminoacids and decreased insulin resistance [11].
Furthermore, two randomized trials supported these benefits for the MedDiet, with 40% relative risk reduction for a MedDiet supplemented with extra-virgin olive oil (EVOO) [12] and increased remission rates with a low-carbohydrate MedDiet [13]. A much clearer understanding of these benefits can be attained by examining the actual compliance of participants in preventive trials, given that dietary interventions usually face suboptimal compliance and their results might not be generalizable to those following the same diet, but with a different compliance. The 14-item Mediterranean Adherence Screener (MEDAS) is a rapid assessment tool which validly appraises conformity to the MedDiet [14] and has been used and recommended in different countries [15,16,17,18]. This sort of dietary tools are useful in the context of a trial, because they can be repeated at different time intervals to assess dietary changes and provide immediate feedback to participants. The frequent repetition of assessments is a key methodological point, because repeated dietary measurements capture changes over time, thus increasing the validity and robustness of diet-disease associations [19]. We assessed the effect of adherence to the MedDiet on diabetes incidence in a large randomized trial using yearly repeated measurements.
Methods
Study design
PREDIMED is a primary cardiovascular prevention trial, whose methods were previously described [20, 21]. Briefly, participants were randomly allocated to one of three interventions in a 1:1:1 ratio: Mediterranean diet supplemented with EVOO (MedDiet + EVOO), Mediterranean diet supplemented with mixed nuts (MedDiet + nuts), or a control diet (low-fat diet). Intention-to-treat effects on type 2 diabetes incidence were previously reported [12], but that report did not consider actual compliance. Current recommendations for pragmatic trials encourage the assessment of actual compliance [22].
Setting & participants
Randomized participants were 7447 men (55 to 80 years) or women (60 to 80 years) initially free of cardiovascular disease at baseline who were at high cardiovascular risk [21]. For this paper, only participants without type 2 diabetes at baseline and with assessment of glycemic control during the trial (n = 3541) were considered (1154 in MedDiet + EVOO group, 1240 in MedDiet + nuts group, 1147 in control diet). Participants in the three arms had personal interviews with a dietitian and small group meetings every 3 months to receive repeated education on the allocated diet, with practical advices on how to upgrade MedDiet (or low-fat diet) including recipes, seasonal food descriptions, shopping lists, meal plans, and menus. The MEDAS score, ranging from 0 (minimum) to 14 (maximum adherence) [14,15,16,17,18] of each participant was annually recorded in face-to-face interviews by the dietitians [21, 23].
Mediterranean diet assessment
For each item in the MEDAS score, one point was awarded, briefly: preference of olive oil as the main culinary source of fat; preference of white meat over red/processed meat; daily consumption of olive oil (≥ 4 servings/d), vegetables (≥ 2 servings/d), fruit (≥ 3 pieces/d), red meat (< 1 serving/d), butter or margarine or cream (< 1 serving/d), and carbonated or sugar-sweetened beverages (< 1 cup/d); and weekly consumption of wine (≥ 7 cups/wk), pulses (≥ 3 servings/wk), fish/seafood (≥ 3 servings/wk), tree nuts (≥ 3 servings/wk), commercial pastry (< 2 servings/wk), and `sofrito´ (a sauce of tomato, garlic, onion or leeks sauteed in olive oil; ≥ 2 times/wk).
Ascertainment of type 2 diabetes
The American Diabetes Association criteria were used to adjudicate new-onset cases of type 2 diabetes during follow-up. These criteria are: HbA1c ≥ 6.5% by a certified and standardized method according to the Diabetes Control and Complication trial, OR fasting (at least 8 h) plasma glucose ≥ 126 mg/dL (7 mmol/L), OR 2 h plasma glucose ≥ 200 mg/dL (11.1 mmol/L) during a standardized (75 g) oral glucose tolerance test, OR classic symptoms of hyperglycemia or hyperglycemic crisis with a random plasma glucose ≥ 200 mg/dL (11.1 mmol/L). In the absence of unequivocal hyperglycemia, diagnosis using these criteria requires two abnormal test results from the same sample or in two separate test samples [24]. Medical doctors, blinded to random allocations, reviewed patient medical records on a yearly basis and submitted potential type 2 diabetes cases to the Clinical Event Adjudication Committee of PREDIMED. This Committee confirmed incident cases blindly to the intervention groups. Only cases occurring during the trial’s intervention period (June 2003 to December 2010) were included in statistical analyses [21].
Covariates
Other covariates collected in the PREDIMED trial have been previously described [20, 21]. Briefly, trained personnel measured blood pressure (in triplicate) and collected sociodemographic and lifestyle variables, including physical activity, using validated questionnaires [21]. Total energy intake was derived from a validated 137-item FFQ repeated yearly. We adjusted for the cumulative average of total energy intake at each yearly visit, and not only for baseline values.
Statistical methods
The association between upgraded adherence to the MedDiet (using yearly cumulative averages) and type 2 diabetes was analyzed with multivariable time-varying Cox models. In these time-varying Cox models, the values of the variable that changed over time was the yearly cumulative average up to the current visit of each patient. For that aim, we time split the dataset into multiple rows per participant based on each visit (please see a very small synthetic example to mimic the data in the Supplementary material). Robust variance estimators were used to account for potential intra-cluster correlations among members of the same household or the same clinic in a small subset of participants. The main exposure were cumulative averages of MEDAS score, calculated as the mean of all time points up to that follow-up visit, including the baseline assessment and up to 7-year follow-up (i.e., 8 time points). Participants with missing values for MEDAS at any time point were assigned the mean of the score between the previous and posterior visit. Hazard Ratios (HRs) were calculated for the three categories of cumulative averages of the MEDAS ( 8 to < 10, 10 to < 12, and ≥ 12 scores) using as reference category the group with lowest adherence (MEDAS < 8). An additional HR was calculated for each 2-point increment in the MEDAS score (roughly equivalent to its standard deviation), considered as a quantitative variable. To quantify a linear trend, we conducted a Wald test for linear trend by assigning the median intake within each of the four categories and modeling this as a continuous variable. Multivariate model 1 was adjusted for age, sex, smoking status (never/current/former), dyslipidemia, hypertension, total energy intake level (kcal/d), physical activity (quintiles), and education (primary/secondary/university). Multivariable model 2 was additionally adjusted for propensity scores derived from estimated probabilities of allocation in the trial [21]. As an ancillary analysis, we also adjusted for the randomized arm of the trial. All models were stratified by recruitment center.
Subgroup analyses by sex, age (< 70 or ≥ 70 years), trial arm, BMI (< 30 or ≥ 30 kg/m2), and smoking were conducted. Interaction cross product-terms with cumulative averages of MEDAS (quantitative variable) were assessed with likelihood ratio tests in fully-adjusted models. To account for multiple testing these p values were corrected for the false discovery rate (FDR), using the Simes method [25]. We applied the same method to correct for multiple testing in the between-group comparison of baseline characteristics, after ANOVA for quantitative variables or after chi squared for categorical variables.
Incidence of diabetes was plotted by joint classification according to average MEDAS scores from years 1 to 7 (< 10 or ≥ 10) and randomized arm (merging both MedDiet groups together, and, only in an ancillary analysis by comparing only MedDiet + EVOO versus control). For these plots, we used standardization with inverse probability weighting (IPW) to control for confounding. Weighting factors were the previously mentioned potential confounders.
We also run (only as a reference) a conventional Cox model using baseline MEDAS as exposure and adjusting for all baseline potential covariates.
In a subset of 889 participants, information on a validated plasma metabolomic signature of MEDAS, comprised of 67 metabolites, was available. This signature has been well validated in PREDIMED and other cohorts with a reported r = 0.31–0.37 in PREDIMED [26]. A linear regression model was used to assess the predicted values of MEDAS with this 67-metabolite signature as predictor. Subsequently, an age- and sex-adjusted Cox model was fitted to obtain the HRs for diabetes according to categories of the metabolomic signature of MEDAS and per 2 additional points in the signature score.
Two tailed P values < 0.05 were considered significant and 95% confidence intervals were always computed.
Results
Description of participants
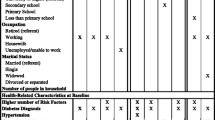
Baseline characteristics according to baseline MEDAS scores are shown in Additional file 4, Table S1. Table 1 shows characteristics of participants classified into four categories according to the combination of their average MEDAS during the entire follow-up period (< 10 points or ≥ 10 points, averaging repeated measures from year 1 to 7, i.e., excluding baseline values) and their randomized group control or MedDiet group (both MedDiets were merged). In this case we only used two categories of MEDAS (instead of the 4 previously mentioned categories of time-dependent cumulative averages) to obtain a sufficient number of subjects in this joint classification. Groups with higher average MEDAS score (i.e. ≥ 10 points) had a greater proportion of men, higher physical activity and energy intake but lower adiposity indexes and blood triglycerides.
Median follow-up was 4.1 years (interquartile range, 2.5 to 5.7). As expected, participants randomly allocated the two MedDiets attained a significantly better upgrading in MEDAS than those in the control group (P < 0.01 for each yearly comparison). After year 1, average ± SD MEDAS was 10.1 ± 1.4 in the MedDiet + EVOO group, 10.2 ± 1.5 in the MedDiet + nuts group, and 8.7 ± 1.5 in the control group. During follow-up, a MEDAS score ≥ 10 was observed in 57.8% of the MedDiet + EVOO group, in 62.5% of the MedDiet + nuts group, and in only 23.2% of the control group (Additional file 1: Figure S1).
Changes in medications that may influence onset of diabetes, such as antihypertensive drugs, statins, corticoids, or estrogens, were distributed evenly among groups (Additional file 2: Figure S2).
Outcome data
During follow-up, 273 incident cases of type 2 diabetes were blindly adjudicated by the Clinical Events Committee. Incidence rates per 1000 person-years by cumulative averages of MEDAS were 27.8 (< 8 points in MEDAS), 20.1 (8 to < 10), 16.1 (10 to < 12) and 13.8 (≥ 12 points in MEDAS), showing a monotonic descending trend as MEDAS increased (Additional file 4: Table S2). For each 2-point increment in MEDAS, the multivariable-adjusted analysis showed a 20% decrease in type 2 diabetes incidence (HR = 0.80; 95% CI, 0.70–0.92, p for linear trend = 0.001). Compared with participants in the lowest category (< 8 points in MEDAS), multivariable-adjusted HRs were 0.66 (95% CI 0.48 to 0.90) for the group scoring 8 to < 10 points, 0.56 (95% CI 0.40 to 0.79) for those scoring 10 to < 12 points, and 0.46 (95% CI 0.25 to 0.83) for those scoring ≥ 12 points, p for trend < 0.001 (Table 2 and Fig. 1). Additional adjustment for the randomized groups only slightly attenuated these results with HRs of 0.67 (95% CI 0.49–0.93) for 8 to < 10 points, 0.59 (95% CI 0.41–0.84) for 10 to < 12 points and 0.48 (95% CI 0.26–0.90) for ≥ 12 points, p for trend = 0.003 (Fig. 1). In the multivariable model adjusted for the randomized arm, a 2-point increment in MEDAS was associated with HR = 0.82 (95% CI 0.71–0.96). Therefore, higher adherence to the MedDiet linearly resulted in lower risk of diabetes, regardless of whether the participant was in the extra virgin olive oil or in the nuts intervention group.
Hazard Ratios (HR) of developing type 2 diabetes according to cumulative adherence to the Mediterranean diet (0 to 14 score of the MEDiterranean diet Adherence Screener or MEDAS). Multivariable adjusted hazard ratios for successive categories of the MEDAS (cumulative averages using yearly repeated measures) according to estimates adjusted only for age and sex (grey bars) or according to estimates with multivariable adjustment for age, sex, baseline smoking status (never, current, or former smoker), fasting glucose level, prevalence of dyslipidemia (yes/no) and hypertension (yes/no), total energy intake level (kcal/d), physical activity level (metabolic equivalent of min/d), education level (primary education, secondary education, academic/graduate), propensity scores for group allocation and randomized group allocated (adjacent bars in sand color). All estimates were stratified by recruitment center, and robust SEs were used. MEDAS Mediterranean Diet Adherence Screener, CI confidence interval.
These findings using cumulative averages were in contrast with the non-significant results found when only baseline MEDAS was assessed. The multivariable-adjusted HR per a 2-point difference in the baseline MEDAS was 0.95 (0.84 to 1.08, p = 0.44) and multivariable-adjusted HRs in categorical analyses were 0.91 (0.67 to 1.24) for 8 to < 10 points in baseline MEDAS; 0.87 (0.63 to 1.21) for 10 to < 12 points; and 0.64 (0.33 to 1.24) for ≥ 12 points.
Previously we developed and validated a plasma signature (a weighted combination of 67 metabolites) that well predicted MEDAS in both PREDIMED (Pearson correlation with MEDAS = 0.31–0.37, P < 0.001) and three independent US cohorts [26]. The age- and sex-adjusted Cox model showed HR = 0.59 (95% CI 0.39–0.89) for a metabolomic signature for MEDAS of 8 to < 10 and a HR = 0.49 (0.29–0.84) for a signature > = 10 as compared to the metabolomic signature for MEDAS of < 8. A HR = 0.73 (0.54–0.99) was found per 2-point increment in the metabolomic signature for MEDAS.
In the time-dependent models using the whole sample (n = 3541), the absolute adjusted rate reduction was 14.4 cases prevented per 1000 persons-years, when comparing the highest (≥ 12 points) versus the lowest (< 8) category of MEDAS cumulative scores. Therefore, the estimated number needed to treat each year to prevent one case of type 2 diabetes was 69.
Subgroup analyses assessed per 2-point increments in cumulative MEDAS average during follow-up showed consistent inverse associations with type 2 diabetes. No significant interactions with stratifying variables were found, regardless of whether or not we corrected for the FDR (Additional file 3: Figure S3).
Figure 2 shows the cumulative risk (Nelson Aalen estimates) of type 2 diabetes (T2D) according to the joint classification by average MEDAS scores attained beyond baseline, i.e., during years 1 to 7 of the trial (dichotomized at ≥ 10 points) and randomized arm (the 2 MedDiet groups merged together vs the control group). The intention-to-treat assessment of the effect of the randomized intervention observed a significant type 2 diabetes rate reduction when comparing the control group to MedDiet + VOO, but not to MedDiet + nuts [12]. Additional file 1 : Figure S1 shows cumulative risk of diabetes according to the joint exposure to MedDiet + VOO and average complicance.
Cumulative incidence (Nelson-Aalen curves) of diabetes according to average MEDAS scores during years 1 to 7 and randomized intervention group. MEDAS scores are dichotomized, where ≥ 10 points are regarded as high adherence. Both intervention groups with Mediterranean Diet have been merged and they were compared against the control group. Adjusted for age, sex, baseline smoking status (never, current, or former smoker), prevalence of dyslipidemia (yes/no) and hypertension (yes/no), family history of CVD, total energy intake level (kcal/d), physical activity level (metabolic equivalent of min/d), education level (primary education, secondary education, and academic/graduate) and recruitment center using inverse probability weighting
The main apparent factor responsible for the diverging rates was adherence to MEDAS after 1-year follow-up. Only within the group of participants attaining highest MEDAS scores (≥ 10) after baseline there was a lower risk of type 2 diabetes among those belonging to the MedDiet intervention groups than in the control group (Additional file 2: Table S2). The respective rates of type 2 diabetes per 1000 person-years were 25.3 in the control group with low adherence, 24.5 in the intervention groups with low adherence, 18.3 in the control group with high adherence and 14.5 in the intervention groups with high adherence.
Discussion
Findings in context
A robust and strong protective effect against type 2 diabetes of actually upgraded adherence to the MedDiet was found in the PREDIMED trial among men and women at high cardiovascular risk. The use of yearly repeated measures of adherence to the diet in a large randomized trial represents the novelty of our study. Participants who exhibited a higher adherence during the trial –regardless of their randomized group– had a substantially lower risk of type 2 diabetes. Even after adjusting for the randomized group, a highly significant inverse linear dose–response relationship was noted for each 2-point improvement in MEDAS and higher adherence to the MedDiet linearly resulted in lower risk of diabetes, regardless of the provision of extra virgin olive oil or nuts in the intervention program. In addition, an objective multi-metabolite signature of adherence to the MedDiet measured in plasma [26] confirmed these results. These findings are consistent with those of most previous studies reporting benefits of the MedDiet against type 2 diabetes [8, 27,28,29,30,31], however, our results provide a more robust assessment of the adherence to the MedDiet by using yearly repeated measurements and accounting for cumulative exposure with a yearly updated information which was not been used in previous papers.
The importance of capturing actual compliance with the intended diet
In nutritional epidemiology, repeated measurements of exposure are highly informative because they best represent long-term diet and minimize within-subject variation [19, 32]. As expected in large, long-term behavioural trials, even after random assignment to intervention, suboptimal compliance is usually observed. Close to one-third of participants assigned to the MedDiet arms did not attain a MEDAS ≥ 10, and 21% of participants in the control group followed the MedDiet on their own and reached a MEDAS ≥ 10 (Table 1), which was associated with reduced risk. Our previous intention-to-treat assessment found a statistically significant effect when comparing the control group to MedDiet + VOO, but no significance was found for MedDiet + nuts. Nevertheless, now we show that high compliers belonging to both MedDiet intervention groups received the greatest benefit regarding diabetes prevention. The advantage of intervention groups can be related to the likely higher consumption of freely provisioned EVOO and nuts, even after keeping constant the MEDAS score, particularly given the consistency, coherence and biological plausibility for their beneficial effect.
Biological plausibility of our findings
The specific mechanisms by which the MedDiet reduces the risk of type 2 diabetes are not yet fully understood. However, some have been proposed. Excessive body weight, especially abdominal fat, substantially increases insulin resistance [33]. Better adherence to the MedDiet usually results in greater and more sustained weight loss as compared to other isocaloric, healthy plant-based diets [34, 35] and lower adiposity as supported by several randomized trials [36,37,38]. Furthermore, adherence to MEDAS was strongly inversely associated with abdominal obesity in our baseline assessment of the PREDIMED cohort [35]. The replacement of rapidly absorbed carbohydrates by monounsaturated fat from EVOO or polyunsaturated fat from tree nuts contributes to avoid insulin resistance [39]. Insulin sensitivity is also improved by the richness in fruits, vegetables, legumes, EVOO and whole grains in the MedDiet, delaying carbohydrate absortion and providing phenolic compounds with beneficial antioxidant and anti-inflammatory properties. Closer conformity to the MedDiet involves a higher dietary fiber intake and overall improvements in carbohydrate quality with substantial benefits against type 2 diabetes [40]. In fact, the MedDiet has been repeatedly reported to be associated with lower levels of inflammatory biomakers [41, 42], increased levels of adiponectin [43, 44] and reductions in advanced glycation end products [10].
Effects of specific components of the Mediterranean diet
Individual components of the MedDiet have also been associated with lower risk of diabetes [45, 46]. Insulin sensitivity can be improved by phenolic compounds found in olive oil, especially EVOO, showing anti-inflammatory and anti-oxidative properties [47] and by whole grain consumption, but worsened by red meat, processed meat and sugar-sweetened beverage consumption. Tree nuts and peanuts have a low glycemic index and are rich in nutrients beneficial for diabetes risk, such as fiber, unsaturated fatty acids, magnesium, and phenolic compounds [5]. However, inverse associations of nut consumption with type 2 diabetes were not apparent in a meta-analysis of observational studies [48].
Clinical usefulness of rapid dietary screeners
The MEDAS tool has attracted great interest in many Mediterranean and non-Mediterranean countries [14,15,16,17,18]. MEDAS allows rapid feedback to patients and certain goals may be easily set to improve adherence to the MedDiet, particularly in primary care settings. However, some potential disavantages of the MEDAS, particularly for its transferabilty to other countries have been reported [49, 50], including the difficulties to appraise the item for ‘‘sofrito’’, the absence of an upper limit in the item for wine, the restriction to pastries in the cereal group and the inability to capture total energy intake. Notwithstanding, in our present assessment and in many other instances the MEDAS showed validity for predicting hard clinical outcomes in the long-term. Our results show that by improving only 2 items (an easily attainable and practical goal), a relative reduction in type 2 diabetes by 20% can be achieved.
Limitations and strengths
Limitations in our study include, first, that our participants were at high risk of cardiovascular disease and they belonged to a Mediterranean country, thus reducing generalizability. Nevertheless, external validity should take into account biological plausibility and not only representativeness in the merely statistical interpretation used for surveys. Secondly, even though we accounted for many potential confounders, a potential for residual confounding exist; however, previous intention-to-treat results were reasonably free of residual confounding and also showed strong benefits. Thirdly, a certain degree of measurement error using MEDAS may have occurred; however, the face-to-face interviews by expert and well-trained dietitians to collect the MEDAS questionnaires may miminize this risk; also, the use of cumulative averages is known to reduce measurement errors [19, 32]. Furthermore, the objective exposure assessment with a plasma metabolomic-based measurement corroborated our findings.
Strengths of our study included addressing the important issue of the assessment of the effect of actual compliance with a dietary intervention in a large randomized trial. Secondly, those variables which met the requirements as to be considered major potential confounders were appropriately controlled for in the statistical analyses (we did not adjust for intermediate links in the causal pathway, to avoid overadjustment). In any case, it was reassuring that the results did not materially change after a variety of multivariable adjustments. Thirdly, we used cumulative averages of diet scores, which accounted for previous dietary exposures and reduced measurement errors. Fourth, biomarkers of adherence in a large subset of participants were used to confirm the validity of results.
Conclusions
Our study found that upgraded adherence to the Mediterranean dietary pattern, high in virgin olive oil, fruits, vegetables, legumes, whole grains, nuts, fish and seafood; with moderate consumption of alcohol; and low intake of red and processed meat, whole-fat dairy, sodas, and sweets reduced the incidence of type 2 diabetes in subjects at high cardiovascular risk. These findings represent a practical and affordable approach to reduce the growing population burden of diabetes.
Availability of data and materials
We will be happy to provide access to the data supporting the results reported in this article (including data dictionaries), making possible the replication of the analyses used for the present article. Due to the restrictions imposed by the Informed Consent and the Institutional Review Board, bona fide investigators interested in analyzing the dataset used for the present article may submit a brief proposal and statistical analysis plan to the corresponding author (mamartinez@unav.es). Upon approval from the Predimed Steering Committee and Institutional Review Boards, the data will be made available to them using an onsite secure access data enclave.
Abbreviations
- CI:
-
Confidence intervals
- EVOO:
-
Extra-virgin olive oil
- HR:
-
Hazard ratio
- MEDAS:
-
Mediterranean diet adherence screener
- MedDiet:
-
Mediterranean diet
- PREDIMED:
-
PREvención con DIeta MEDiterránea (Prevention with Mediterranean Diet)
References
Magliano DJ, Boyko EJ. IDF diabetes atlas. 10th ed. Brussels: International Diabetes Federation; 2021.
Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med. 2009;169:798–807.
Trichopoulou A, Martínez-González MA, Tong TY, Forouhi NG, Khandelwal S, Prabhakaran D, Mozaffarian D, de Lorgeril M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med. 2014;12:112.
Toi PL, Anothaisintawee T, Chaikledkaew U, Briones JR, Reutrakul S, Thakkinstian A. Preventive role of diet interventions and dietary factors in type 2 diabetes mellitus: an umbrella review. Nutrients. 2020;12:2722.
Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383:1999–2007.
Milenkovic T, Bozhinovska N, Macut D, Bjekic-Macut J, Rahelic D, Velija Asimi Z, Burekovic A. Mediterranean diet and type 2 diabetes mellitus: a perpetual inspiration for the scientific world. A Rev Nutr. 2021;13:1307.
Sotos-Prieto M, Ortolá R, Ruiz-Canela M, Garcia-Esquinas E, Martínez-Gómez D, Lopez-Garcia E, Martínez-González MÁ, Rodriguez-Artalejo F. Association between the Mediterranean lifestyle, metabolic syndrome and mortality: a whole-country cohort in Spain. Cardiovasc Diabetol. 2021;20:5.
Sarsangi P, Salehi-Abargouei A, Ebrahimpour-Koujan S, Esmaillzadeh A. Association between adherence to the Mediterranean diet and risk of type 2 diabetes: an updated systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr. 2022;13:1787–98.
Yubero-Serrano EM, Gutiérrez-Mariscal FM, Gómez-Luna P, Alcalá-Diaz JF, Pérez-Martinez P, López-Miranda J. Dietary modulation of advanced glycation end products metabolism on carotid intima-media thickness in type 2 diabetes patients: From the CORDIOPREV study. Clin Investig Arterioscler. 2023;35:105–14.
Gutierrez-Mariscal FM, Cardelo MP, de la Cruz S, Alcala-Diaz JF, Roncero-Ramos I, Guler I, et al. Reduction in circulating advanced glycation end products by mediterranean diet is associated with increased likelihood of type 2 diabetes remission in patients with coronary heart disease: from the CORDIOPREV study. Mol Nutr Food Res. 2021;65: e1901290.
García-Gavilán JF, Connelly MA, Babio N, Mantzoros CS, Ros E, Salas-Salvadó J. Nut consumption is associated with a shift of the NMR lipoprotein subfraction profile to a less atherogenic pattern among older individuals at high CVD risk. Cardiovasc Diabetol. 2022;21:189.
Salas-Salvadó J, Bulló M, Estruch R, Ros E, Covas MI, Ibarrola-Jurado N, et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med. 2014;160:1–10 (Erratum in: Ann Intern Med. 2018;169:271-272).
Esposito K, Maiorino MI, Petrizzo M, Bellastella G, Giugliano D. The effects of a Mediterranean diet on the need for diabetes drugs and remission of newly diagnosed type 2 diabetes: follow-up of a randomized trial. Diabetes Care. 2014;37:1824–30.
Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–5.
Vadiveloo M, Lichtenstein AH, Anderson C, Aspry K, Foraker R, Griggs S, et al. Rapid diet assessment screening tools for cardiovascular disease risk reduction across healthcare settings: a scientific statement from the American heart association. Circ Cardiovasc Qual Outcomes. 2020;13: e000094.
Rasmussen E, Fosnacht Morgan AM, Munson R, Ong A, Patel S, Yucus C, et al. Use of an electronic medical record to track adherence to the mediterranean diet in a us neurology clinical practice. Mayo Clin Proc Innov Qual Outcomes. 2018;2:49–59.
Hebestreit K, Yahiaoui-Doktor M, Engel C, Vetter W, Siniatchkin M, Erickson N, Halle M, Kiechle M, Bischoff SC. Validation of the German version of the Mediterranean diet adherence screener (MEDAS) questionnaire. BMC Cancer. 2017;17:341.
García-Conesa MT, Philippou E, Pafilas C, Massaro M, Quarta S, Andrade V, et al. Exploring the validity of the 14-Item mediterranean diet adherence screener (MEDAS): a cross-national study in seven European countries around the mediterranean region. Nutrients. 2020;12:2960.
Satija A, Yu E, Willett WC, Hu FB. Understanding nutritional epidemiology and its role in policy. Adv Nutr. 2015;6:5–18.
Martínez-González MÁ, Corella D, Salas-Salvadó J, Ros E, Covas MI, Fiol M, et al. Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol. 2012;41:377–85.
Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378: e34.
Hernán MA, Robins JM. Per-Protocol Analyses of Pragmatic Trials. N Engl J Med. 2017;377:1391–8.
Zazpe I, Sanchez-Tainta A, Estruch R, Lamuela-Raventos RM, Schröder H, Salas-Salvado J, et al. A large randomized individual and group intervention conducted by registered dietitians increased adherence to Mediterranean-type diets: the PREDIMED study. J Am Diet Assoc. 2008;108:1134–44.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S19–40.
Simes RJ. An improved Bonferroni procedure for multiple tests of significance. Biometrika. 1986;73:751–4.
Li J, Guasch-Ferré M, Chung W, Ruiz-Canela M, Toledo E, Corella D, et al. The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J. 2020;41:2645–56.
Jannasch F, Kröger J, Schulze MB. Dietary patterns and type 2 diabetes: a systematic literature review and meta-analysis of prospective studies. J Nutr. 2017;147:1174–82.
Zeraattalab-Motlagh S, Jayedi A, Shab-Bidar S. Mediterranean dietary pattern and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of prospective cohort studies. Eur J Nutr. 2022;61:1735–48.
Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ. 2008;336:1348–51.
de Koning L, Chiuve SE, Fung TT, Willett WC, Rimm EB, Hu FB. Diet-quality scores and the risk of type 2 diabetes in men. Diabetes Care. 2011;34:1150–6.
Romaguera D, Guevara M, Norat T, Langenberg C, Forouhi NG, Sharp S, et al. Mediterranean diet and type 2 diabetes risk in the European prospective investigation into cancer and nutrition (epic) study: the interact project. Diabetes Care. 2011;34:1913–8.
Bernstein AM, Rosner BA, Willett WC. Cereal fiber and coronary heart disease: a comparison of modeling approaches for repeated dietary measurements, intermediate outcomes, and long follow-up. Eur J Epidemiol. 2011;26:877–86.
Eckel RH, Kahn SE, Ferrannini E, Goldfine AB, Nathan DM, Schwartz MW, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? J Clin Endocrinol Metab. 2011;96:1654–63.
Estruch R, Ros E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev Endocr Metab Disord. 2020;21:315–27.
Martínez-González MA, García-Arellano A, Toledo E, Salas-Salvadó J, Buil-Cosiales P, Corella D, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS ONE. 2012;7: e43134.
Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, et al. Weight loss with a low-carbohydrate Mediterranean or low-fat diet. N Engl J Med. 2009;2008(359):229–41 (Erratum in: N Engl J Med. 361:2681).
Schwarzfuchs D, Golan R, Shai I. Four-year follow-up after two-year dietary interventions. N Engl J Med. 2012;367:1373–4.
Mancini JG, Filion KB, Atallah R, Eisenberg MJ. Systematic review of the mediterranean diet for long-term weight loss. Am J Med. 2016;129:407-415.e4.
Ludwig DS, Aronne LJ, Astrup A, de Cabo R, Cantley LC, Friedman MI, et al. The carbohydrate-insulin model: a physiological perspective on the obesity pandemic. Am J Clin Nutr. 2021;114:1873–85.
Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393:434–45.
Hart MJ, Torres SJ, McNaughton SA, Milte CM. Dietary patterns and associations with biomarkers of inflammation in adults: a systematic review of observational studies. Nutr J. 2021;20:24.
Schwingshackl L, Hoffmann G. Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis. 2014;24:929–39.
Fragopoulou E, Panagiotakos DB, Pitsavos C, Tampourlou M, Chrysohoou C, Nomikos T, Antonopoulou S, Stefanadis C. The association between adherence to the Mediterranean diet and adiponectin levels among healthy adults: the ATTICA study. J Nutr Biochem. 2010;21:285–9.
Li S, Shin HJ, Ding EL, van Dam RM. Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2009;302:179–88.
Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, Schlesinger S. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ. 2019;366: l2368.
Schwingshackl L, Hoffmann G, Lampousi AM, Knüppel S, Iqbal K, Schwedhelm C, et al. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32:363–75.
Martínez-González MA, Sayón-Orea C, Bullón-Vela V, Bes-Rastrollo M, Rodríguez-Artalejo F, Yusta-Boyo MJ, García-Solano M. Effect of olive oil consumption on cardiovascular disease, cancer, type 2 diabetes, and all-cause mortality: a systematic review and meta-analysis. Clin Nutr. 2022;41:2659–82.
Becerra-Tomás N, Paz-Graniel I, Hernández-Alonso P, Jenkins DJA, Kendall CWC, Sievenpiper JL, Salas-Salvadó J. Nut consumption and type 2 diabetes risk: a systematic review and meta-analysis of observational studies. Am J Clin Nutr. 2021;113:960–71.
Chiriacò M, Tubili C, Bo S, Parillo M, Vetrani C, Mazzotti A, et al. Critical evaluation of the questionnaires assessing adherence to the Mediterranean diet that are based on servings. Nutr Metab Cardiovasc Dis. 2023;33:724–36.
Hutchins-Wiese HL, Bales CW, Porter Starr KN. Mediterranean diet scoring systems: understanding the evolution and applications for Mediterranean and non-Mediterranean countries. Br J Nutr. 2022;128:1371–92.
Acknowledgements
We thank all PREDIMED participants, all family doctors involved in the recruitment of participants (see please, ref. 16, Additional file, pages 4-5), and the dietitians and nurses who participated in the field work of PREDIMED.
Abstract presentation
Part of this manuscript content was previously presented as an Abstract, in the meeting of the American Diabetes Association 80th Scientific Sessions, virtual, June 12, 2020.
Funding
Primary Funding Source Instituto de Salud Carlos III. The PREDIMED trial was supported by Instituto de Salud Carlos III (ISCIII), the official funding agency for biomedical research of the Spanish government, through grants provided to research networks specifically developed for the trial (RTIC G03/140, to Ramón Estruch during 2003–2005; RTIC RD 06/0045, to Miguel A. Martínez-González during 2006–2013 and through Centro de Investigación Biomédica en Red de Fisiopatología de la Obesidad y Nutrición [CIBEROBN]), and by grants from Centro Nacional de Investigaciones Cardiovasculares (CNIC 06/2007), Fondo de Investigación Sanitaria–Fondo Europeo de Desarrollo Regional (PI04-2239, PI 05/2584, CP06/00100, PI07/0240, PI07/1138, PI07/0954, PI 07/0473, PI10/01407, PI10/02658, PI11/01647, P11/02505, PI13/00462, and JR17/00022), Ministerio de Ciencia e Innovación (AGL-2009–13906-C02, AGL2010- 22319-C03, AGL2011-23430, and SAF2016–80532-R), Fundación Mapfre 2010 (no role in the design, implementation, analysis or interpretation of the data), Consejería de Salud de la Junta de Andalucía (PI0105/2007), Public Health Division of the Department of Health of the Autonomous Government of Catalonia, Generalitat Valenciana (PROMETEO 17/2017, and PROMETEO 21/2021), Fundació La Marató-TV3 (grants 294/C/2015 and 538/U/2016 (no role in the design, implementation, analysis or interpretation of the data)), Agencia Canaria de Investigación, Innovación y Sociedad de la Información-EU FEDER (PI 2007/050 and CS2011-AP-042), and Regional Government of Navarra (P27/2011). The metabolomic study was supported by research grant NIDDK-R01DK 102896 from the National Institutes of Health. Donations of olive oil, walnuts, almonds, and hazelnuts were made respectively by the Fundación Patrimonio Comunal Olivarero and Hojiblanca (Malaga, Spain), California Walnut Commission (Sacramento, California), Borges (Reus, Spain), and Morella Nuts (Reus, Spain). Prof. Jordi Salas-Salvadó is partially supported by ICREA, under the ICREA Academia programme.
Author information
Authors and Affiliations
Contributions
MA MG was involved in the conception, design, and conduct of this study, and, with PM, in the analysis and interpretation of the results. PM, MRC and MAMG wrote the first draft of this manuscript. All authors edited and reviewed the manuscript and provided important intellectual and scientific content. All authors approved the final version of the manuscript. MA, MG is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial protocol complied with the Declaration of Helsinki, was approved by local institutional review boards, registered under the International Standard Randomized Controlled Trial Number ISRCTN35739639 (http://www.isrctn.com/ISRCTN35739639), as described in previous publications [15, 16]. All participants provided written informed consent before joining the trial.
Consent for publication
Not applicable.
Competing interests
E.R. reported receiving grants, personal fees, and nonfinancial support from the California Walnut Commission, personal fees and nonfinancial support from Alexion, and nonfinancial support from the International Nut and Dried Fruit Council outside the submitted work. R.E. reported receiving olive oil for the trial from Fundacion Patrimonio Comunal Olivarero during the conduct of the study and personal fees from Brewers of Europe, Fundación Cerveza y Salud, Interprofesional del Aceite de Oliva, Instituto Cervantes, Instituto Cervantes, Pernaud Richar, Fundación Dieta Mediterránea, Wine and Culinary International Forum; nonfinancial support from Sociedad Española de Nutrición and Fundación Bosch y Gimpera. J. S–S. reported receiving research support from the California Walnut Commission, Patrimonio Comunal Olivarero, La Morella Nuts, and Borges S.A; receiving consulting fees or travel expenses from Danone, California Walnut Commission, Eroski Foundation, Instituto Danone and Nestle, receiving nonfinancial support from Hojiblanca, Patrimonio Comunal Olivarero, and Almond Board of California; serving on the board of and receiving grant support through his institution from the International Nut and Dried Foundation and the Eroski Foundation; and grants and personal fees from Instituto Danone. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Risk of type 2 diabetes according to the joint classification to the Mediterranean diet+extravirgin olive oil (EVOO) or control group and averaged attained cumulative adherence to the Mediterranean diet (MEDAS score) during years 1 to 7 of follow-up. Cumulative incidence (Nelson-Aalen curves) considering only 2 randomized groups: Mediterranean Diet+extravirgin olive oil (EVOO) or control group (the group allocated to Mediterranean Diet + nuts was excluded). MEDAS scores are dichotomized, where ≥10 points are regarded as high adherence. Adjusted for age, sex, baseline smoking status (never, current, or former smoker), prevalence of dyslipidemia (yes/no) and hypertension (yes/no), family history of CVD, total energy intake level (kcal/d), physical activity level (metabolic equivalent of min/d), education level (primary education, secondary education, and academic/graduate) and recruitment center using inverse probability weighting.
Additional file 2 :Figure S2.
Changes in medication according to subgroups defined by the joint combination of average cumulative adherence to the Mediterranean diet (MEDAS, with cut-off point=10) and randomized group. The statin group was included in the lipid-lowering group, but it is also presented separately. MEDAS Mediterranean diet adherence score. HRT hormone replacement therapy (only considering women)
Additional file 3: Figure S3.
Subgroup analysis of multivariable adjusted hazard ratios for each 2-point increment in MEDAS (cumulative averages using yearly repeated measures). P-values for interaction were calculated for subgroups of sex, age, intervention allocation, body mass index (BMI) and smoking status. Adjusted for age, sex, baseline smoking status (never, current, or former smoker), fasting glucose level, prevalence of dyslipidemia (yes/no) and hypertension (yes/no), total energy intake level (kcal/d), physical activity level (metabolic equivalent of min/d), education level (primary education, secondary education, academic/graduate), and propensity scores. Stratified by recruitment center, and robust SEs were used.
Additional file 4: Table S1.
Baseline characteristics of the study populationa. Table S2. Incidence of diabetes after a median follow-up of 4.1 years in the PREDIMED trial according to the randomized group and to attained cumulative average adherence to the Mediterranean diet (MEDAS score) during follow-up (across years 1 to 7).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martínez-González, M.A., Montero, P., Ruiz-Canela, M. et al. Yearly attained adherence to Mediterranean diet and incidence of diabetes in a large randomized trial. Cardiovasc Diabetol 22, 262 (2023). https://doi.org/10.1186/s12933-023-01994-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01994-2