Abstract
Background
The effect of diabetes mellitus (DM) on the long-term outcomes of coronary artery bypass graft (CABG) remained debatable and various strategies exist for CABG; hence, clarifying the effects of DM on CABG outcomes is difficult. The current study aimed to evaluate the effect of DM on clinical and graft-related outcomes after CABG with bilateral internal thoracic artery (BITA) grafts.
Methods
From January 2001 to December 2017, 3395 patients who underwent off-pump CABG (OPCAB) with BITA grafts were enrolled. The study population was stratified according to preoperative DM. The primary endpoint was cardiac death and the secondary endpoints were myocardial infarction (MI), revascularization, graft failure, stroke, postoperative wound infection, and a composite endpoint of cardiac death, MI, and revascularization. Multiple sensitivity analyses, including Cox proportional hazard regression and propensity-score matching analyses, were performed to adjust baseline differences.
Results
After CABG, the DM group showed similar rates of cardiac death, MI, or revascularization and lower rates of graft failure at 10 years (DM vs. non-DM, 19.0% vs. 24.3%, hazard ratio [HR] 0.711, 95% confidence interval [CI] 0.549–0.925; P = 0.009) compared to the non-DM group. These findings were consistent after multiple sensitivity analyses. In the subgroup analysis, the well-controlled DM group, which is defined as preoperative hemoglobin A1c (HbA1c) of < 7%, showed lower postoperative wound infection rates (well-controlled DM vs. poorly controlled DM, 3.7% vs. 7.3%, HR 0.411, 95% CI 0.225–0.751; P = 0.004) compared to the poorly controlled DM group, which was consistent after propensity-score matched analysis.
Conclusions
OPCAB with BITA grafts showed excellent and comparable long-term clinical outcomes in patients with and without DM. DM might have a protective effect on competition and graft failure of ITA. Strict preoperative hyperglycemia control with target HbA1c of < 7% might reduce postoperative wound infection and facilitate the use of BITA in CABG.
Similar content being viewed by others
Background
Coronary artery bypass graft (CABG) is the recommended treatment for revascularization in patients with diabetes mellitus (DM) and coronary artery disease (CAD), especially in three-vessel diseases [1]. However, DM could worsen the prognosis after CABG because it frequently involves diffuse CAD that involves the left main, multi-vessel, or smaller vessels [2] and has higher chances of recurrent myocardial infarction (MI) and other comorbidities postoperatively [3, 4]. Additionally, the effect of DM on the long-term outcomes of CABG remained debatable based on published studies so far [5,6,7,8,9].
Importantly, various strategies exist for CABG, and when these are mixed in the same study, clarifying the effects of DM on CABG outcomes becomes difficult [5,6,7, 9]. Particularly, regarding graft selection, a wide variety of graft selection strategies exist in previous studies although internal thoracic artery (ITA) is proven patent in the long-term and is the graft choice for left anterior descending artery anastomosis [5,6,7,8,9]. Additionally, off-pump CABG (OPCAB) might remove the detrimental effects of cardiopulmonary bypass; however, a great deal of variability related to use of cardiopulmonary bypass exists for each center [5, 7]. Therefore, this study aimed to determine the effects of DM on patients who underwent OPCAB using bilateral ITA (BITA) grafts only.
Postoperative sternal wound infection is one of the most worrisome complications after CABG using BITA. Preoperative hemoglobin A1c (HbA1c) has been studied as a prognostic factor for postoperative wound infection in patients with DM who underwent cardiac surgery [10, 11]. The effect of HbA1c on postoperative morbidities, including mediastinal wound infection, was tried to define in this homogenous cohort.
Methods
Study design and populations
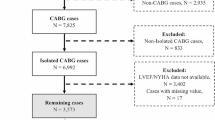
This retrospective and the observational study included 6691 consecutive patients who underwent CABG using BITA in a single large tertiary center from January 2001 to December 2017. Patients younger than 18 years (n = 14), with missing angiographical data (n = 40), who underwent CABG other than BITA grafts (n = 1916), on-pump CABG (n = 781), concomitant heart surgery (n = 456), and had previous CABG history (n = 89) were excluded (Fig. 1). Patients were divided into two groups, the non-DM and DM groups. Patients in the DM group were divided into two subgroups, namely, the well-controlled (preoperative HbA1c of < 7%) and poorly controlled DM groups (HbA1c of ≥ 7%) [12].
Study flow diagram. A total of 3395 patients who underwent OPCAB with a bilateral internal thoracic artery in a single tertiary center were enrolled. Patients were divided into non-DM and DM groups. Patients in the DM group were divided into well-controlled (HbA1c < 7%) and poorly controlled DM groups (HbA1c ≥ 7%). OPCAB indicates off-pump coronary artery bypass graft; DM: diabetes mellitus; HbA1c: hemoglobin A1c
The Institutional Review Board of Samsung Medical Center approved this study (SMC 2021-11-157, date of approval: December 1, 2021), which waived informed consent from individual patients because this retrospective study poses minimal risk for patients.
Data collection and clinical follow-up
The baseline demographic, echocardiographic, laboratory, and follow-up clinical outcomes were retrospectively collected through medical record review. Extracted data were revalidated by our research coordinators and physicians for clarity.
The primary endpoint was cardiac death at 10 years postoperative and the secondary endpoints included MI, revascularization, graft failure, stroke, postoperative wound infection, and major adverse cardiovascular events (MACE; a composite endpoint of cardiac death, MI, and revascularization). The mean clinical outcome follow-up duration was 4.01 years. The mortality data for patients who were lost to follow-up were confirmed using the National Death Records. MI was defined as elevated cardiac troponin or myocardial band fraction of creatine kinase that is greater than the upper reference limit with concomitant ischemic symptoms or electrocardiography findings indicative of ischemia. Left ventricular dysfunction was classified as follow: normal (left ventricular ejection fraction more than 50%); mild dysfunction (left ventricular ejection fraction 40% to 49%); ≥ moderate dysfunction (left ventricular ejection fraction less than 40%). Graft patency was assessed using coronary computed tomography angiography or invasive coronary angiography, according to operator discretion (Additional file 1: Table S1). Grafts were evaluated following the FitzGibbon A, B, and O classification and interpreted by an independent cardiology expert who was blinded to treatment strategy. Postoperative early clinical outcomes included clinical outcomes within 30 days of the surgery. Outcome variables were defined according to the definition of the Society of Thoracic Surgeons Adult Cardiac Surgery Database version 4.20 [13].
Surgical procedure and perioperative management
The surgical technique for OPCAB was performed following relevant standard guidelines [1, 14]. and described in our earlier report in detail [15]. BITA was prepared using the skeletonization technique. After opening the pericardium, the right ITA was anastomosed to the left side of the left ITA as a Y-composite graft. Achieving complete revascularization of all vessels with a 1-mm or larger diameter and 50% or more angiographic diameter stenosis was intended in all patients. The left ITA was first anastomosed to the left anterior descending artery and its branches, and the right ITA was sequentially anastomosed to branches of the circumflex artery. The right coronary territory was revascularized last. The quality of the anastomosis was assessed by transit-time flow measurement with a Transsonic Flowmeter (Transonic Systems, Ithaca, NY).
Strict glycemic control before, during, and after the surgery has been implemented under standard institutional protocols. Target blood glucose control in patients with DM was set to < 180 mg/dL [12, 16] by intermittent regular insulin injection (Humulin; Eli Lilly and Company, Indianapolis, Ind) intraoperatively and continuous regular insulin infusion postoperatively in the intensive care unit (ICU). Blood glucose level was measured every 1 h in the operative room and every 4 h in the ICU. If the ideal glycemic control was not made, glucose concentration was checked at an interval of 2 h until the target level was achieved in the ICU.
Guideline-directed medical therapy including a combination of antiplatelet agents, beta-blockers, statins, and angiotensin-converting enzyme (ACE) inhibitors and/or angiotensin receptor blockers (ARBs) was applied to all patients undergoing CABG, unless contraindicated [1, 17].
Statistical analysis
Descriptive statistics for categorical variables were reported as frequency and percentage, whereas continuous variables were reported as mean ± standard deviation or median (range). Categorical variables were compared between the groups using the χ2 test or Fisher’s exact test, whereas continuous variables were compared using the two-sample t-tests or the Wilcoxon rank-sum test. Continuous data were checked for distribution normality using the Shapiro–Wilk test and graphical methods. The cumulative incidence of clinical events is estimated using a Fine–Gray model to account for the competing risk of death from non-cardiovascular causes.
Multiple sensitivity analyses, including multivariable Cox proportional hazard regression and propensity-score matched analyses, were performed to reduce biased effects. The Cox proportional hazard regression model considered variables that were significant in the univariable analysis or clinically relevant in the multivariable analysis. Variables included age, sex, body mass index, DM, HbA1c, an initial diagnosis of ischemic heart disease, hypertension, dyslipidemia, smoking history, end-stage renal disease requiring dialysis, previous cerebrovascular accident, abdominal aortic aneurysm, peripheral arterial disease, chronic obstructive pulmonary disease, peak troponin I, peak creatine kinase-MB, glomerular filtration rate, ejection fraction, left ventricular dysfunction, 3 vessel disease, left main involvement, and urgent surgery. The backward elimination method was used for model selection in the multivariable analysis. The results were reported as hazard ratio (HR) and 95% confidence interval (CI).
Propensity-score analyses were used to adjust covariate differences between the two groups. The variables included in the propensity-score model were as follows: age, sex, body mass index, angina, hypertension, dyslipidemia, previous stroke history, chronic kidney disease, chronic obstructive pulmonary disease, smoking history, left ventricular dysfunction, preoperative significant mitral valve regurgitation, urgent surgery, the number of anastomoses, and the number of diseased coronary arteries. A total of 1393 patients in the non-DM group and 1393 patients in the DM group were matched in a 1:1 manner using nearest-neighbor matching. Additionally, for subgroup analysis, a total of 452 patients in the well-controlled DM group and 452 patients in the poorly controlled DM group were matched in a 1:1 manner using nearest-neighbor matching. The balance between the two groups after propensity-score matching was assessed by calculating the standardized mean difference (SMD) between selected variables, with an SMD of < 0.20 suggesting an appropriate balance (Additional file 2: Fig. S1, Additional file 1: Tables S2 and S3).
All statistical tests were two-sided, with an alpha level of 0.05. Statistical analysis was performed using Statistical Package for the Social Sciences software (version 25.0, SPSS, Chicago, IL, USA) and R statistical software (version 4.0.2; R Foundation of Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
A total of 3395 patients underwent CABG during the study period, including 1511 (44.5%) patients with DM and 1884 (55.4%) patients without DM (Fig. 1). The mean age of the patients was 63.3 years and 2619 (77.2%) patients were males. Additionally, 1898 (55.9%) patients had acute coronary syndrome, and 683 (20.1%) had left ventricular dysfunction. The mean number of anastomosis during CABG was 3.97 and postoperative guideline-directed medications, including aspirin, P2Y12 inhibitors, beta-blockers, ACE inhibitors or ARB, and statins were prescribed in 3300 (97.2%), 2046 (60.2%), 2530 (74.5%), 999 (29.4%), and 2721 (80.1%) patients, respectively.
Patients with DM were older (64.16 years vs. 62.62 years, P < 0.001) and more likely to have hypertension, smoking history, an end-stage renal disease requiring dialysis, previous cerebrovascular accident, abdominal aortic aneurysm, and peripheral arterial disease compared to patients without DM (Table 1). Additionally, patients with DM had a higher proportion of left ventricular dysfunction (25% vs. 16%, P < 0.001) and three-vessel diseases (75.6% vs. 64.8%, P < 0.001) and a bigger number of anastomosis (4.10 vs. 3.87, P < 0.001) during CABG than those without DM.
Clinical outcomes
Incidences of postoperative mortality, bleeding requiring reoperation, and graft-related reoperation were 0.32%, 1.08%, and 0.38%, respectively. The DM group had higher rates of acute kidney injury (8.57% vs. 3.83%, P < 0.001), wound infection (5.69% vs. 1.70%, P < 0.001), and repeated wound infection (1.0% vs. 0.4%, P = 0.043) than in the non-DM group in the early postoperative period (Table 2).
In the long-term, no differences were found in the rates of cardiac death, MI, repeat revascularization, stroke, and MACE between the DM and non-DM groups (Table 2).
Multivariable Cox proportional hazard models and propensity-score matched analyses consistently showed similar results for patients in both groups (Table 2, Figs. 2 and 3).
Cumulative incidence curves for cardiac death (A), myocardial infarction (B), repeat revascularization (C), and MACE (D) according to DM. Non-cardiac death was accounted as a competing event in the Fine–Gray model. MACE indicates major adverse cardiovascular and cerebrovascular events; DM: diabetes mellitus
ITA graft outcomes
The mean time from surgery to graft failure was 2.60 ± 2.99 years. Patients in the DM group had lower rates of ITA graft failure (19.0% vs. 24.3%, HR = 0.711, P = 0.009), ITA graft failure with FitzGibbon grade O (16.6% vs. 21.7%, HR = 0.695, P = 0.010), and right ITA graft failure (13.4% vs. 18.1%, HR = 0.696, P = 0.025). Multivariable Cox proportional hazard models and propensity-score matched analyses consistently showed similar results for patients in both groups (Table 2, Fig. 3A).
Subgroup analysis
Compared with patients with poorly controlled DM, patients with well-controlled DM were older and more likely to have hypertension, end-stage renal disease that requires dialysis, and previous cerebrovascular accidents (Table 3). However, no statistical differences were seen between the two groups regarding preoperative echocardiography, coronary angiography, and operative characteristics. In the long-term, there were no differences found in the rates of cardiac death, MI, repeat revascularization, stroke, and MACE between the well-controlled DM and poorly controlled DM groups (Additional file 2: Figs. S2 and S3). However, patients with well-controlled DM had a lower proportion of postoperative wound infection (3.7% vs. 7.3%, HR = 2.064, 95% CI 1.210–2.521, P = 0.0007; Table 4). Multivariable Cox proportional hazard models and propensity-score matched analyses consistently showed similar results for patients in the well-controlled and poorly controlled DM groups.
Multivariable analysis for outcomes
Preoperative dialysis (HR = 2.256, 95% CI 1.223–4.161, P = 0.009) and glomerular filtration rate of < 60 mL/min/1.73 m2 (HR = 1.684, 95% CI 1.188–2.387, P = 0.003) were significant predictors of MACE in the multivariable analysis (Table 5). Additionally, age at operation (HR = 0.986, 95% CI 0.974–0.998, P = 0.028) and DM (HR = 0.718, 95% CI 0.556–0.929, P = 0.011) were prognostic factors for postoperative graft failure. Female sex (HR = 0.359, 95% CI 0.241–0.510, P < 0.001), DM (HR = 3.264, 95% CI 2.158–4.938, P < 0.001), and HbA1c of < 7% (HR = 0.333, 95% CI 0.219–0.505, P = 0.001) were significant prognostic factors for postoperative wound infection.
Discussion
This study revealed the following key findings: (1) DM had no significant impact on long-term clinical outcomes, including cardiac death and MACE after OPCAB with BITA, (2) patients with DM had lower rates of postoperative graft failure compared to those without DM, and (3) patients with well-controlled DM, which is defined as preoperative HbA1c of < 7%, had a lower proportion of postoperative wound infection compared to those with poorly controlled DM.
Patients with DM who undergo intervention for CAD might have a poorer prognosis than those without DM, although the impact of DM on long-term mortality remained controversial [5, 6, 8, 18]. Patients with DM have more left main or multi-vessel CAD with a diffuse disease that involves smaller vessels [2], and they have a greater atherosclerotic burden and increased number of lipid-rich plaques, which are prone to rupture [19,20,21].
However, long-term survival and MACE between the DM group and non-DM groups in this study were not statistically different due to several reasons. First, CABG might have a protective effect against recurrent MI in patients with DM [22]. In complex CAD, the most common cause of mortality might be MI-related death [23], which tends to cluster within the proximal third of major coronary vessels [24]. CABG might provide the coverage of anatomic zones at risk for MI [25] and have the effect of preventing recurrent MI in patients with DM because graft insertion sites seem to be consistently located distal to acute thrombosis sites in patients with CABG.
Another important question is the influence of DM on the long-term patency of ITA grafts. Raza et al. [26] investigated postoperative angiograms quantifying stenosis in ITA grafts in patients who underwent primary isolated CABG and found that DM did not influence the long-term patency of bypass grafts. Early ITA graft patency was even better in patients with DM than in those without DM in the same study [26]. Additionally, Ralf et al. found that not having DM was a predictor of ITA graft failure and which might have been caused by competitive flow in their well-designed study with completed angiographic follow-up [27]. ITA grafts can autoregulate depending on flow requirements; thus, they may close due to competitive blood flow in the native vessel, especially in patients without DM [28,29,30]. In the current study, the non-DM group had higher rates of graft failure than the DM group and most of the cases were within the early phase, which is consistent with previously described studies. We might infer that most graft failures might have been caused by competition, not by surgical occlusion or atherosclerosis from the observation that most graft failures occurred in the early phase, not in the immediate postoperative or late phase. Additionally, most graft failures occurred in the form of occlusion rather than stenosis, and in RITA rather than in LITA, which might have a lower chance of competition due to the low number of anastomosis per graft [27] compared to RITA. Severe stenotic coronary disease in DM might have a protective effect on graft patency, which might need further investigation. Fractional flow reserve-guided CABG, which is now in practice at our center, might avoid graft failure caused by competition and enhance long-term outcomes, especially in patients without DM [31, 32].
HbA1c, which reflects the mean glycemia over the previous 8–12 weeks [33, 34], has been investigated as a parameter exerting an adverse influence on outcomes in patients with DM who underwent cardiac surgery [10, 11]. In this study, postoperative wound infection, which is the major drawback of using bilateral ITA grafts for CABG in patients with DM, was significantly lower in the well-controlled DM group, although without differences regarding cardiac mortality and MACE between the well-controlled and poorly controlled DM groups. The preoperative strict control of hyperglycemia might lower the incidence of postoperative wound infection and facilitate the use of BITA when performing CABG.
The present study has the following limitations. First, this is a retrospective study in a single tertiary center and might have selection bias. Second, we did not routinely perform invasive coronary angiography or coronary computed tomography angiography after CABG and the graft-related outcomes might be overestimated. Last, the adherence of medical treatment was lower than expected and not considered in the present analysis. However, important strengths of our study include its large sample size, homogeneous group using identical strategy in performing CABG, and strict adjustment for confounding factors using multiple sensitivity analysis.
In conclusion, OPCAB with BITA grafts showed excellent and comparable long-term clinical outcomes in patients with and without DM. DM might have a protective effect on competition and graft failure of ITA, and strict preoperative control of hyperglycemia with target HbA1c of < 7% might reduce postoperative wound infection and facilitate the use of BITA in CABG.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BITA:
-
Bilateral internal thoracic artery
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- HbA1c:
-
Hemoglobin A1c
- ITA:
-
Internal thoracic artery
- ICU:
-
Intensive care unit
- DM:
-
Diabetes mellitus
- MI:
-
Myocardial infarction
- MACE:
-
Major adverse cardiovascular events
- OPCAB:
-
Off-pump coronary artery bypass grafting
References
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Ledru F, Ducimetiere P, Battaglia S, Courbon D, Beverelli F, Guize L, et al. New diagnostic criteria for diabetes and coronary artery disease: insights from an angiographic study. J Am Coll Cardiol. 2001;37(6):1543–50.
Deedwania PC, Ahmed MI, Feller MA, Aban IB, Love TE, Pitt B, et al. Impact of diabetes mellitus on outcomes in patients with acute myocardial infarction and systolic heart failure. Eur J Heart Fail. 2011;13(5):551–9.
Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17(1):53.
Mohammadi S, Dagenais F, Mathieu P, Kingma JG, Doyle D, Lopez S, et al. Long-term impact of diabetes and its comorbidities in patients undergoing isolated primary coronary artery bypass graft surgery. Circulation. 2007;116(11 Suppl):I220–5.
Kogan A, Ram E, Levin S, Fisman EZ, Tenenbaum A, Raanani E, et al. Impact of type 2 diabetes mellitus on short- and long-term mortality after coronary artery bypass surgery. Cardiovasc Diabetol. 2018;17(1):151.
Koshizaka M, Lopes RD, Reyes EM, Gibson CM, Schulte PJ, Hafley GE, et al. Long-term clinical and angiographic outcomes in patients with diabetes undergoing coronary artery bypass graft surgery: results from the Project of Ex-vivo Vein Graft Engineering via transfection IV trial. Am Heart J. 2015;169(1):175–84.
Onuma Y, Wykrzykowska JJ, Garg S, Vranckx P, Serruys PW, Arts I, et al. 5-Year follow-up of coronary revascularization in diabetic patients with multivessel coronary artery disease: insights from ARTS (arterial revascularization therapy study)-II and ARTS-I trials. JACC Cardiovasc Interv. 2011;4(3):317–23.
Wit MA, de Mulder M, Jansen EK, Umans VA. Diabetes mellitus and its impact on long-term outcomes after coronary artery bypass graft surgery. Acta Diabetol. 2013;50(2):123–8.
Corazzari C, Matteucci M, Kolodziejczak M, Kowalewski M, Formenti AM, Giustina A, et al. Impact of preoperative glycometabolic status on outcomes in cardiac surgery: systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2021. https://doi.org/10.1016/j.jtcvs.2021.05.035.
Kim HJ, Shim JK, Youn YN, Song JW, Lee H, Kwak YL. Influence of preoperative hemoglobin A1c on early outcomes in patients with diabetes mellitus undergoing off-pump coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2020;159(2):568–76.
American Diabetes Association Professional Practice Committee, Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, et al. 6. Glycemic targets: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S83–96.
STS Adult Cardiac Surgery Database Data Specifications Version 4.20.2. Published 2020. https://www.sts.org/sites/default/files/ACSD_DataSpecifications_V4_20_2.pdf. Accessed 4 Apr 2022.
Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124(23):e652-735.
Jeong DS, Sung K, Lee YT, Ahn JH, Carriere KC, Kim WS, et al. Pure bilateral internal thoracic artery grafting in diabetic patients with triple-vessel disease. Ann Thorac Surg. 2015;100(6):2190–7.
Lazar HL, McDonnell M, Chipkin SR, Furnary AP, Engelman RM, Sadhu AR, et al. The Society of Thoracic Surgeons practice guideline series: blood glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87(2):663–9.
Pinho-Gomes AC, Azevedo L, Ahn JM, Park SJ, Hamza TH, Farkouh ME, et al. Compliance with guideline-directed medical therapy in contemporary coronary revascularization trials. J Am Coll Cardiol. 2018;71(6):591–602.
Marui A, Kimura T, Nishiwaki N, Mitsudo K, Komiya T, Hanyu M, et al. Five-year outcomes of percutaneous versus surgical coronary revascularization in patients with diabetes mellitus (from the CREDO-Kyoto PCI/CABG Registry Cohort-2). Am J Cardiol. 2015;115(8):1063–72.
Silva JA, Escobar A, Collins TJ, Ramee SR, White CJ. Unstable angina. A comparison of angioscopic findings between diabetic and nondiabetic patients. Circulation. 1995;92(7):1731–6.
Moreno PR, Murcia AM, Palacios IF, Leon MN, Bernardi VH, Fuster V, et al. Coronary composition and macrophage infiltration in atherectomy specimens from patients with diabetes mellitus. Circulation. 2000;102(18):2180–4.
Marso SP, Mercado N, Maehara A, Weisz G, Mintz GS, McPherson J, et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc Imaging. 2012;5(3 Suppl):S42-52.
Doenst T, Haverich A, Serruys P, Bonow RO, Kappetein P, Falk V, et al. PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. J Am Coll Cardiol. 2019;73(8):964–76.
Milojevic M, Head SJ, Parasca CA, Serruys PW, Mohr FW, Morice MC, et al. Causes of death following PCI versus CABG in complex CAD: 5-year follow-up of SYNTAX. J Am Coll Cardiol. 2016;67(1):42–55.
Wang JC, Normand SL, Mauri L, Kuntz RE. Coronary artery spatial distribution of acute myocardial infarction occlusions. Circulation. 2004;110(3):278–84.
Jeon C, Candia SC, Wang JC, Holper EM, Ammerer M, Kuntz RE, et al. Relative spatial distributions of coronary artery bypass graft insertion and acute thrombosis: a model for protection from acute myocardial infarction. Am Heart J. 2010;160(1):195–201.
Raza S, Blackstone EH, Houghtaling PL, Rajeswaran J, Riaz H, Bakaeen FG, et al. Influence of diabetes on long-term coronary artery bypass graft patency. J Am Coll Cardiol. 2017;70(5):515–24.
Harskamp RE, Alexander JH, Ferguson TB Jr, Hager R, Mack MJ, Englum B, et al. Frequency and predictors of internal mammary artery graft failure and subsequent clinical outcomes: insights from the project of ex-vivo vein graft engineering via transfection (PREVENT) IV Trial. Circulation. 2016;133(2):131–8.
Villareal RP, Mathur VS. The string phenomenon: an important cause of internal mammary artery graft failure. Tex Heart Inst J. 2000;27(4):346–9.
Shimizu T, Hirayama T, Suesada H, Ikeda K, Ito S, Ishimaru S. Effect of flow competition on internal thoracic artery graft: postoperative velocimetric and angiographic study. J Thorac Cardiovasc Surg. 2000;120(3):459–65.
Hashimoto H, Isshiki T, Ikari Y, Hara K, Saeki F, Tamura T, et al. Effects of competitive blood flow on arterial graft patency and diameter. Medium-term postoperative follow-up. J Thorac Cardiovasc Surg. 1996;111(2):399–407.
Fournier S, Toth GG, De Bruyne B, Johnson NP, Ciccarelli G, Xaplanteris P, et al. Six-year follow-up of fractional flow reserve-guided versus angiography-guided coronary artery bypass graft surgery. Circulation. 2018;11(6):006368.
Spadaccio C, Glineur D, Barbato E, Di Franco A, Oldroyd KG, Biondi-Zoccai G, et al. Fractional flow reserve–based coronary artery bypass surgery: current evidence and future directions. Cardiovasc Interv. 2020;13(9):1086–96.
Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther. 2019;21(2):81–5.
Wright LA, Hirsch IB. Metrics beyond hemoglobin A1C in diabetes management: time in range, hypoglycemia, and other parameters. Diabetes Technol Ther. 2017;19(S2):S16–26.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
IP contributed to data interpretation, drafted the manuscript and handled the submission. KBC performed the analysis and drafted the manuscript. JHA contributed to data handling, interpretation and critical revision of the manuscript. WSK contributed to data collection and interpretation of the manuscript. YTL contributed to data collection and interpretation of the manuscript. DSJ contributed to data collection, handling, interpretation and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of Samsung Medical Center approved this study (SMC 2021-11-157, date of approval: December 1, 2021). The Institutional Review Board waived informed consent from individual patients because this retrospective study poses minimal risk.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Graft evaluation modalities after CABG according to DM. Table S2. Baseline and operative characteristics in propensity-matched population between the Non-DM group and DM group. Table S3. Baseline and operative characteristics in propensity-matched population between the well-controlled vs. poorly controlled DM groups.
Additional file 2
: Figure S1. Love plots for propensity score matching (A) between DM and non-DM groups and (B) between well-controlled and poorly controlled DM groups. Figure S2. Cumulative incidence curves for cardiac death (A), myocardial infarction (B), repeat revascularization (C), and MACE (D) according to preoperative HbA1c. Non-cardiac death was accounted as a competing event in the Fine-Gray model. Figure S3. Cumulative incidence curves for graft failure (A) and stroke (B) according to preoperative HbA1c. Non-cardiac death was accounted as a competing event in the Fine-Gray model.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, I., Choi, K.B., Ahn, J.H. et al. Impact of diabetes mellitus on long-term clinical and graft outcomes after off-pump coronary artery bypass grafting with pure bilateral skeletonized internal thoracic artery grafts. Cardiovasc Diabetol 21, 243 (2022). https://doi.org/10.1186/s12933-022-01687-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01687-2