Abstract
Aims
Reduced lung function and adverse health outcomes are often observed. This study characterizes genetic susceptibility for reduced lung function and risk of developing a range of adverse health outcomes.
Methods
We studied 27,438 middle-aged adults from the Malmö Diet and Cancer study (MDCS), followed up to 28.8 years. Trait-specific Polygenic scores (PGS) for forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) were constructed for each participant using MDCS genetic data and summary statistics from the latest GWAS of lung function. Linear regression models and cox proportional hazards regression models were used to assess associations between adverse health outcomes and lung function-PGS.
Results
FEV1-PGS and FVC-PGS were significantly associated with mean sBP at baseline after adjustments (FEV1-PGS Q1 (highest PGS = highest lung function): 140.7mmHg vs. Q4: 141.5mmHg, p-value 0.008). A low FVC-PGS was significantly associated with the risk of future diabetic events after adjustments (Q4 vs. Q1 HR: 1.22 (CI 1.12–1.32), p-trend < 0.001) and had added value to risk prediction models for diabetes. Low FEV1-PGS was significantly associated with future coronary events (Q4 vs. Q1 HR: 1.13 (CI: 1.04–1.22), p-trend 0.008). No significant association was found between PGS and sudden cardiac death, chronic kidney disease or all-cause mortality. Results remained largely unchanged in a subgroup of subjects when further adjusted for apolipoproteins.
Conclusion
Genetic susceptibility for reduced lung function is associated with higher sBP, increased risk of diabetes and to a lesser extent, future coronary events, suggesting etiological roles of lung function on these outcomes. Using PGS, high-risk groups could be early detected to implement early lifestyle changes to mitigate the risk.
Similar content being viewed by others
Introduction
Many observational studies have shown associations between low levels of lung function and future adverse health events, including diabetes, myocardial infarction (MI), sudden cardiac death (SCD) and all-cause mortality [1,2,3,4,5]. Although these relationships have been found independently of commonly shared risk factors (e.g. in cohorts of life-long never smokers), they remain vulnerable to unmeasured confounders present in life-style choices that are difficult to fully take into account in observational studies.
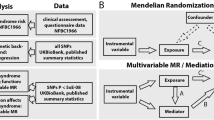
Polygenic scores (PGS) are a useful instrument in providing genetic risk prediction by aggregating the effects from a large number of genetic variants associated with particular traits identified from genome-wide association studies (GWAS) [6]. PGS, being less likely affected by non-genetic factors, have shown promising applications in disease prediction and early screening [7, 8]. PGS were also used to examine putative causal relationships with good statistical power [9] and were suggested as an approach in complement to Mendelian randomization (MR) [9, 10] though horizontal pleiotropy need be well considered. Moreover, PGS, representing a personalized score for evaluating one’s life-time risk, is an emerging approach in precision medicine.
A GWAS has discovered 279 risk loci for chronic obstructive pulmonary disease (COPD) [11]. Based on this, PGS have been constructed in predicting pulmonary diseases such as COPD [12,13,14,15,16]. Less is known for PGS cross trait prediction such as cardio-metabolic events. Although previous MR studies have found lung function to be inversely related to coronary artery disease (CAD) [17,18,19], stroke, type 2 diabetes mellitus (T2DM) and systolic blood pressure (sBP) [18], we are not aware of studies of PGS for lung function systematically assessing its predictive values in predicting a range of future incident outcomes.
Herein, we assessed the risk of cardio-metabolic outcomes (major adverse cardiovascular events (MACE), sudden cardiac death (SCD), sBP and diabetes), chronic kidney disease (CKD) and all-cause mortality in relation to PGS for forced expiratory volume in 1 s (FEV1) and for forced vital capacity (FVC) using the the Malmö Diet and Cancer study (MDCS) in 27,438 subjects.
Methods
Study population
The Malmö Diet and Cancer study (MDCS) is a large prospective cohort study of men and women from Malmö, Sweden. Between 1991 and 1996, subjects aged 44–73 years living in Malmö were recruited to take part in the study. All men born between 1923 and 1945 and women born between 1923 and 1950 were invited to participate. Participation rate was approximately 40%. A total of 30,446 men and women underwent baseline examinations. All participants provided written consent, and the Ethical Committee at Lund University, Lund, Sweden approved the study (LU 51–90, LU 2009/633, LU 2011/356). Subjects with missing genotype data were excluded (n = 1151). Additionally, subjects with missing information on key variables for model adjustments were excluded (n = 1857). As exclusion of prevalent disease at baseline is not necessary for prediction of incident events if genetic risk is the exposure, we included prevalent cases where later a further event was recorded for the same subject for coronary events (CE) and chronic kidney disease endpoints but not SCD and diabetes. As SCD by definition is a sudden event in someone who is not known to previously have coronary heart disease, we excluded all prevalent cases of CE for the outcome of SCD. Prevalent cases of diabetes at baseline that occurred earlier than baseline were excluded for the purposes of this analysis to ensure that the majority of diabetes events included were type 2 diabetes mellitus (T2DM). The number of subjects examined for each outcome are illustrated in Fig. 1.
Baseline examinations
Standing height was measured using a fixed stadiometer calibrated in centimetres. Weight was measured whilst subjects wore light clothing and no shoes using a balance beam scale to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight (kg)/height2(m). Blood pressure was measured using a mercury column sphygmomanometer after 10 min of rest in the supine position. Non-fasting blood samples were taking at enrolment. Serum and plasma were separated within one hour and stored at -80 degrees centigrade. Serum concentrations of Apolipoprotein A1 (Apo A-1) and Apolipoprotein B (Apo B) were measured by Quest Diagnostics (San Juan Capistrano, CA) using an immunonephelometric assay run on the Siemens BNII (Siemens, Newark, DE). Smoking status was ascertained from self-administered questionnaire responses. Higher education was defined as gaining university level education. Low physical activity was defined as the lowest quintile of the physical activity score, described in detail elsewhere [20]. Use of inhaled corticosteroids was defined as R03BA codes in the ATC (Anatomical, Therapeutic, Chemical classification) register. Baseline prevalent diabetes was defined as self-reported history of physician’s diagnosis of diabetes or use of anti-diabetic medication. Baseline prevalent CE and CKD were defined using national registers. No lung function was measured at the baseline MDCS but a subset of participants were re-examined as part of the Malmö Preventive Project cohort (MPP), where spirometry was measured. (n = 14 961 with FEV1 (L) and 14 979 with FVC (L)).
Genotyping and quality control of the Malmö Diet and Cancer study
MDCS participants were genotyped using Illumina GSA v1 genotyping array. Quality controls (QC) on the genotyped variants were conducted by removing variants for probe to genome mismatch, incorrect assignment of allelic variant, failed genotype calling, call rate less than 99%, minor allele frequency (MAF) less than 0.01 or failed Hardy-Weinberg Equilibrium test at p < 1 × 10− 15. For sample QC, samples were excluded if genetic sex did not match pedigree sex or had an overall sample call rate less than 90%. The FlashPCA [21] was implemented for principal component analysis (PCA) on the genotyped data. Imputation was performed using the reference panel of Haplotype Reference Consortium (HRC r1.1) [22].
Polygenic risk scores (PGS) for lung function
A Bayesian regression framework PRS-continuous shrinkage (PRS-CS) [23] was applied to build PGS for lung function. PRS-CS had shown superior performances in the prediction of common diseases and quantitative traits [23]. PRS-CS was used to infer posterior single-nucleotide polymorphism (SNP) effect sizes based on linkage disequilibrium reference panel of 1000 Genomes Project (European sample, n = 503) and GWAS summary statistics on FEV1 (n = 400 102) and FVC (n = 400 102) from meta-analysis on the UK Biobank and SpiroMeta, respectively, where age, age squared, sex, height and smoking was adjusted in the association analyses [11]. We restricted SNPs that are biallelic, having MAF no less than 0.01 and consistent directions in sub studies of GWAS of meta-analysis. Using the PLINK (version 1.90) [24], PGS for FEV1 and FVC on 29 295 MDC samples were then constructed by aggregating the obtained posterior effect sizes for FEV1 (635 689 SNPs) and FVC (634 755 SNPs).
Through the study, PGS for FEV1 or FVC are a relative measure of lung function in arbitrary units. High PGS represent high measures of FEV1 or FVC, implying high lung function and vice versa.
Endpoint ascertainment
SCD was defined as a fatal CE where death took place within the first 24 h, in individuals without a previous CE. This included those cases where death occurred outside of hospital. International Classification of Diseases (ICD) 9 codes included 410, 412 and 414; and ICD 10 codes I21, I24 and I25 [25, 26]. Major adverse cardiovascular events (MACE) were defined as CE, coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI) with ICD 9 codes 410, 412, 414 and ICD 10 codes I20, I21, I24 and I25. For CE, data linkage with the National Cause of Death Registry, Swedish Hospital Discharge registry and the Malmö Myocardial Infarction Register was used to retrieve cases [27]. Incident diabetes was defined using the Malmö HbA1c register (MHR), the Swedish national Diabetes register (NDR), the Swedish hospital discharge register, the Swedish outpatient register, the cause of death register, the Swedish drug prescription register, the regional Diabetes 2000 register of the Scania region and the All New Diabetics in Scania (ANDIS) registry. Incident cases of diabetes were also retrieved from re-examination of MDCS subjects in the MPP (2002–2006), MDCS baseline screening in the cardiovascular cohort (1992–1994), MDCS 5 year rescreening (1997–2001) and MDC cardiovascular rescreening (2007–2012). Incident CKD events were defined as ICD-10 codes N18 or N19. The Swedish inpatient registry had been in operation during the entire follow-up period and data from this registry has been found to have acceptable validity for epidemiological research [28]. All subjects were followed from the baseline examinations until the event of interest, death from other causes, emigration or last follow-up date (31st December 2019), whichever came first.
Statistical analysis
All statistical analyses were carried out using SPSS V.26 (IBM, Armonk, New York, USA) and STATA v14.0. Cox regression models were implemented to obtain hazard ratios (HR) for all endpoints by quartiles of FEV1-PGS and FVC-PGS (Q1 highest PGS –reference) and by 1-SD increase of FEV1-PGS and FVC-PGS. Adjustments were kept to a minimum but were made for potentially key confounders known from the literature (Model 1: unadjusted, Model 2: age, sex, height, weight, smoking, sBP, prevalent diabetes (except for the outcome of diabetes), and the first 5 principal components (PCs) of population structures. The outcomes of diabetes and hypertension were additionally adjusted for inhaled corticosteroids. PC allow us to adjust for underlying population structures, where genetic ancestry may explain associations between variants and a specific phenotype. As Apo A-1 and Apo B levels were available for fewer subjects, a further analysis was carried in these subjects after adjustment for Apo A-1 and Apo B (number of subjects by outcome with apolipoproteins available= SCD = 26,035, MACE = 26,273, diabetes = 25,376, CKD = 26,534, all-cause mortality = 26,536 and sBP = 26,536). Time dependent covariate analysis and Kaplan Meier curves were used to assess the proportional hazards assumptions. Using the time-dependent covariate analysis, proportional hazards assumptions were fulfilled for all adjusted outcomes. Univariate regression models were used to assess mean sBP by quartiles of FEV1-PGS and quartiles of FVC-PGS, adjusted for potential confounders known from the literature. A p-value of < 0.05 was considered statistically significant, however, to take into account the role of multiple testing, a Bonferroni adjusted p-value of < 0.01 was used to assess p-trend across quartiles.
We assessed the improvement of prediction models of coronary heart disease and diabetes after the addition of PGS for lung function to the prediction models. Performance of the models was assessed using log-likelihood ratio tests and a category-free net reclassification index (NRI) [29]. For incident MACE, risk prediction was carried out in non-diabetic (at baseline) subjects, with no known intermittent claudication and no known previous CE (n = 22,065 subjects). Covariates in the risk prediction model included age, sex, smoking status, sBP, ApoA1 and ApoB and BP medication. For incident diabetes, risk prediction was carried out in non-diabetic subjects (at baseline) (n = 25,655 subjects). Covariates in the risk prediction model included age, sex, sBP, parental history of diabetes, ApoA1, ApoB and BMI.
Results
Subjects were followed up for an average of 28.8 years (SD ± 6.5). Baseline characteristics are shown in Table 1 for quartiles of FVC-PGS and Supplement Table 1 for quartiles of FEV1-PGS.
There was a significant association between FEV1-PGS and FVC-PGS quartiles and height, sBP and proportion of subjects with prevalent diabetes and proportion with higher education at baseline. Additionally, FVC-PGS quartiles were also significantly associated with BMI (Table 1), whilst FEV1-PGS quartiles were significantly associated with inhaled corticosteroid use (Supplement Table 1) Of the 27,438 subjects in the baseline MDCS cohort, 14 961 subjects had information on FEV1 (L) and 14 979 subjects had information on FVC (L). In these subjects Pearson’s correlation coefficient between FEV1-PGS and FEV1 (L) was 0.031 (p-value < 0.001) and FVC-PGS and FVC (L) was 0.019 (p-value 0.018). In 27,438 subjects, there was a negative correlation between FEV1-PGS and FVC-PGS with height (-0.030, p-value < 0.001 and − 0.018, p-value 0.003, respectively), however height was already adjusted in the GWAS analyses of lung function which may have resulted in over-adjustment for height in the present cohort and therefore observed negative correlations. FEV1-PGS was significantly associated with mean sBP at baseline in 27,438 subjects after adjustment for potential confounders (Mean BP (mmHg) FEV1-PGS Q1: 140.7 vs. Q4: 141.5, p-value 0.008). Similar associations were found for FVC-PGS and mean sBP. A significant reduction in sBP was observed per 1-SD increase in FEV1 and FVC-PGS (Table 2). After further adjustments for Apo-A1 and Apo-B the results remained largely unchanged (Supplement Table 2).
Health outcomes by quartiles of PGS
HR of cardio-metabolic, renal and mortality outcomes by quartiles of and 1-SD increase in FVC and FEV1-PGS are shown in Table 3 and Supplement Table 3, respectively and Fig. 2. A low FVC-PGS was significantly associated with the risk of future diabetic events (Model 2, Q1 vs. Q4 HR: 1.22 (1.12–1.32), p-trend < 0.001 (significant at Bonferroni adjusted p-value), HR per 1-SD increase in FVC-PGS 0.94 (0.92–0.97) p-value < 0.001). Although this association was also found for FEV1-PGS, the results for FEV1-PGS quartiles were not significant at the Bonferroni adjusted p-value (p-value = 0.015) and borderline significant per 1-SD increase in FEV1-PGS (p = 0.04). A low FEV1-PGS was however significantly associated with future MACE events (Model 2 Q1 vs. Q4 HR: 1.13 (1.04–1.22), p-trend 0.008, HR per 1-SD increase in FEV1-PGS 0.97 (0.94-1.00), p < 0.05). No significant association was observed between low FVC or FEV1-PGS and SCD, CKD or all-cause mortality. The results for HR of outcomes by FEV1-PGS and FVC-PGS after further adjusting model 2 for Apo-A1 and Apo-B are shown in Supplement Table 4. The results were found to remain largely the same, with a small increase in significance for the p-values related to the MACE outcomes.
As we found that higher education was significantly associated with PGS quartiles in the baseline analysis (Table 1and Supplement Table 1) we additionally added higher education level to the adjustments in Supplement Table 4 and found that results again remained largely unchanged. A 1-SD increase in the FEV1-PGS was no longer associated with diabetes after adjusting for higher education, however this association was very borderline significant previously (p = 0.046) and the conclusion that FVC-PGS are more strongly associated with diabetes than FEV1-PGS with diabetes remained. The association between sBP and PGS became slightly attenuated after adjusting for higher education however the associations for both quartiles (p-value for Q1 vs. Q4 for FEV1-PGS = 0.018 and for FVC-PGS = 0.003) and per 1-SD increase (change in sBP per 1-SD increase in FEV1-PGS: -0.289, p-value = 0.008, and per 1-SD increase in FVC-PGS: -0.297, p-value = 0.006) remain statistically significant.
Added value of PGS to prediction models for incident MACE and Incident diabetes
An added value of FVC-PGS was observed in predicting diabetes measured by both the NRI and LR test (Table 4). For the category free NRI, more subjects with diabetes events were correctly reclassified as diabetes events than as non-diabetic events after the addition of FVC-PGS (Z-score) to the prediction model. However, the addition of FVC-PGS mainly reclassified non-events of diabetes, where more subjects without diabetes events were correctly reclassified as not having a diabetes events after the addition of FVC-PGS to the prediction model. Similarly, the addition of FVC-PGS improved the fit of the model for prediction of diabetes (LR test p-value < 0.001). There was no significant NRI after the addition of FEV1-PGS to prediction models for diabetes, however LR test showed a marginal improvement in model fit (p-value 0.0308). There was no significant NRI or improved goodness of fit for MACE prediction after adding PGS to the prediction models.
Discussion
To our knowledge, the present study is the first PGS study for lung function that has assessed a range of different health outcomes beyond COPD, along with its added benefit in risk prediction models. We show that PGS of low lung function is associated with higher sBP at baseline and increased future risk of diabetes in a cohort of middle-aged subjects. There is also a strong added benefit of FVC-PGS in risk prediction models for the outcome of future diabetes. The finding is more strongly observed for low FVC-PGS than FEV1-PGS, re-enforcing previous knowledge that highlights the importance of vital capacity of the lung on health.
Studies of PGS for different health outcomes have recently generated considerable interest [30]. Identification of high-risk groups using PGS can be thought of as the equivalent to having additional risk factor for an outcome that could be used in the clinical setting for risk stratification. Additionally, as we also found, PGS can improve risk prediction of certain health outcomes. Tikkanen et al. found that combining traditional risk factors for CAD with a PGS improved risk prediction and risk discrimination for CAD [31]. Previous studies of lung function PGS have mainly assessed respiratory outcomes, predominantly COPD. Lung function PGS can identify subjects at significantly increased risk of COPD and shows improved prediction for COPD when combined with clinical risk factors [12]. We believe we are the first study assessing a broad range of outcomes outside of pulmonary disease for PGS for lung function.
We found a small but significant increase in sBP with lower lung function PGS. The association between BP and lung function has previously found in observational studies [32, 33]. It has been suggested that hypertension in combination with the use of antihypertensive medication and not high BP itself is associated with lower lung function in the general population [34]. Our findings suggest that genetic susceptibility for reduced lung function has a small but significant effect on sBP. However, as BP is so widely affected by objective and subjective factors, the risk of higher sBP associated with genetic susceptibility for lower levels of lung function may be part of variety of other factors influencing the observed measurement. Further studies assessing long-term changes in sBP associated with genetic susceptibility for reduced lung function may help clarify this relationship further.
The significant association found between FVC-PGS and diabetes provides additional evidence of causality, given that causal effect for lung function on diabetes was observed by previous MR analyses [18, 35]. Lung function has been known to be associated with diabetes where adults with diabetes are known to have lower FVC and FEV1 than non-diabetic adults. The direction of association and mechanisms had remained unclear in the past [36], however there is now emerging evidence for a bi-directional causal association between lung function and diabetes [35]. An association between low vital capacity as a predictor of diabetes has been consistently found in previous observational studies [5,37,38,39]. The possible explanations for this link have included reduced physical activity due to poor lung function leading to central obesity, hypoxaemia induced insulin resistance, adverse foetal or early-life conditions that effect organogenesis and metabolic pathway programming leading to insulin resistance and inflammation [37]. We have previously found low lung function to be a significant predictor of diabetes which was not fully explained by obesity, inflammation or smoking [5], concluding that common genetic determinants for low lung function and diabetes could be a potential area for further investigation. The current study adds strong evidence to suggest that genetic susceptibility for reduced lung function can predict the development of diabetes and has added value in prediction models.
A significant association was found between MACE and PGS-FEV1 even after further adjustment for apolipoproteins. Previous findings from many observational studies have found low lung function to be repeatedly independently associated with many cardiovascular outcomes [3, 40]. Previous 2-sample MR studies have found higher lung function to potentially protect against CAD and stroke [18]. Results from an MR study in 2018 found a clear inverse relationship between FEV1 and CAD but results were less robust for FVC [17]. This is in accordance with our findings where the trend for MACE across quartiles of PGS was stronger for FEV1 than for FVC-PGS. A proposed potential explanation for this was that residual confounding due to height in previous observational studies may have led to an observed association between FVC and CAD. FVC is measure of the lung capacity whereas FEV1 is thought of as a measure of severity of airflow limitation, where the former is thought to be more so affected by height and the latter by smoking [17]. This is, however, in contrast to recent findings from a 2-sample MR study on lung function and cardiovascular disease (CVD)[19]. Higbee et al. [19] found FVC to be independently and causally related to CAD, but not FEV1 and it was again proposed that confounding may explain the previous observed associations between FEV1 and cardiovascular events. [19].
Previous studies have found that multiple underlying processes are likely to contribute to the association between lung function and mortality [41]. It is likely that many unmeasured confounders could explain the associations between lung function and all-cause mortality in observational studies. Additionally, although low levels of lung function have been associated with CVD mortality and pulmonary disease mortality in observational studies, the associations with other causes of mortality are less well established, which may have affected the observed relationships in our study.
Limitations
The main limitation of genetic studies of this nature is representation. Currently many biobanks recruit subjects mainly from European ancestry. This was also the case for the GWAS study we used to base our PGS on and the study population for the MDCS. This limits the use of genetic screening tools created from subsequent findings to subjects from specific populations that are represented in the biobank databases. Our results are also therefore limited for use in subjects from European ancestry.
Another limitation is potential horizontal pleiotropic effects when using PGS as instrument in inferring putative causal relationships. However, our PGS were constructed using GWAS on lung function [11] where age, age squared, sex, height, smoking, and population structures were considered. PGS associated factors such as sBP, weight, prevalent DM and the actual height of the participants were also accounted in our cox regression models. However, horizontal pleiotropic effects cannot be ruled out and PGS in estimating causal relationships should be interpreted carefully. A complementary approach such as MR analysis is often needed. Indeed, MR analyses have shown causal effects for low lung function on the risk of diabetes and CAD, which is in line with our findings [18, 35].
Spirometry data from MPP has limitations as only one acceptable measurement was needed, and it was done before the current guidelines (e.g. no nose clips were used) and therefore was prone to measurement errors. However, we observed a significant correlation between PGS and lung function measures. The correlation coefficient is relatively low probably due to a low SNP-based heritability of lung function (< 5%) and in part also explained by some of the measurement issues described.
Conclusion
Genetic susceptibility for reduced lung function is associated with higher sBP and strongly related to an increased risk of future diabetes and to a lesser extent, future coronary events. Using PGS, high risk groups could be early detected so they can make early lifestyle changes attempting to mitigate that risk.
Data availability
The authors do not own the data underlying this study. The data are owned by Lund University, and the approval for research from this database is obtained through the Malmö Diet and Cancer Study (MDCS) steering committee. The data cannot be made publicly available without ethical approval. Data are available upon request for interested researchers by applying to MDCS steering committee. Please email (Anders.Dahlin@med.lu.se) with requests for the data.
Abbreviations
- MI:
-
myocardial infarction
- SCD:
-
sudden cardiac death
- PGS:
-
polygenic scores
- GWAS:
-
genome wide association studies
- MR:
-
mendelian Randomization
- COPD:
-
chronic obstructive pulmonary disease
- CAD:
-
coronary artery disease
- T2DM:
-
type 2 diabetes mellitus
- sBP:
-
systolic blood pressure
- FEV1:
-
forced expiratory volume in 1 s
- FVC:
-
forced vital capacity
- MDCS:
-
malmö diet and cancer study
- CE:
-
coronary events
- CKD:
-
chronic kidney disease
- Apo A-1:
-
apolipoprotein A1
- Apo B:
-
apolipoprotein B
- MPP:
-
malmö preventive project
- QC:
-
quality control
- MAF:
-
minor allele frequency
- PCA:
-
principal component analysis
- PRS-CS:
-
PRS-continuous shrinkage
- SNP:
-
single-nucleotide polymorphism
- ICD:
-
international Classification of Diseases
- MACE:
-
major adverse cardiovascular events
- CABG:
-
coronary artery bypass graft
- PCI:
-
percutaneous coronary intervention
- MHR:
-
malmö HbA1c register
- NDR:
-
swedish national Diabetes register
- ANDIS:
-
all New Diabetics in Scania
- PC:
-
principal components
- NRI:
-
net reclassification index
- BMI:
-
body mass index
- HR:
-
hazard ratios
- Q:
-
quartile
- LR test:
-
log-likelihood ratio test
- CVD:
-
cardiovascular disease
References
Friedman GD, Klatsky AL, Siegelaub AB. Lung function and risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1976;294(20):1071–5.
Schroeder EB, Welch VL, Couper D, Nieto FJ, Liao D, Rosamond WD, Heiss G. Lung function and incident coronary heart disease: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2003;158(12):1171–81.
Lange P, Nyboe J, Jensen G, Schnohr P, Appleyard M. Ventilatory function impairment and risk of cardiovascular death and of fatal or non-fatal myocardial infarction. Eur Respir J. 1991;4(9):1080–7.
Young RP, Hopkins R, Eaton TE. Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Respir J. 2007;30(4):616–22.
Zaigham S, Nilsson PM, Wollmer P, Engstrom G. The temporal relationship between poor lung function and the risk of diabetes. BMC Pulm Med. 2016;16(1):75.
Sun J, Wang Y, Folkersen L, Borné Y, Amlien I, Buil A, Orho-Melander M, Børglum AD, Hougaard DM, Lotta LA, Jones M, Baras A, Melander O, Engström G, Werge T, Lage K, Regeneron genetics C. translating polygenic risk scores for clinical use by estimating the confidence bounds of risk prediction. Nat Commun. 2021;12(1):5276.
Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield M, Devlin JJ, Nordio F, Hyde C, Cannon CP, Sacks F, Poulter N, Sever P, Ridker PM, Braunwald E, Melander O, Kathiresan S, Sabatine MS. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385(9984):2264–71.
Seibert TM, Fan CC, Wang Y, Zuber V, Karunamuni R, Parsons JK, Eeles RA, Easton DF, Kote-Jarai Z, Al Olama AA, Garcia SB, Muir K, Grönberg H, Wiklund F, Aly M, Schleutker J, Sipeky C, Tammela TL, Nordestgaard BG, Nielsen SF, Weischer M, Bisbjerg R, Røder MA, Iversen P, Key TJ, Travis RC, Neal DE, Donovan JL, Hamdy FC, Pharoah P, Pashayan N, Khaw KT, Maier C, Vogel W, Luedeke M, Herkommer K, Kibel AS, Cybulski C, Wokolorczyk D, Kluzniak W, Cannon-Albright L, Brenner H, Cuk K, Saum KU, Park JY, Sellers TA, Slavov C, Kaneva R, Mitev V, Batra J, Clements JA, Spurdle A, Teixeira MR, Paulo P, Maia S, Pandha H, Michael A, Kierzek A, Karow DS, Mills IG, Andreassen OA, Dale AM. Polygenic hazard score to guide screening for aggressive prostate cancer: development and validation in large scale cohorts. BMJ. 2018;360:j5757.
Richardson TG, Harrison S, Hemani G, Davey Smith G. An atlas of polygenic risk score associations to highlight putative causal relationships across the human phenome. Elife 2019;8.
Socrates A, Maxwell J, Glanville KP, Di Forti M, Murray RM, Vassos E, O’Reilly PF. Investigating the effects of genetic risk of schizophrenia on behavioural traits. NPJ Schizophr. 2021;7(1):2.
Shrine N, Guyatt AL, Erzurumluoglu AM, Jackson VE, Hobbs BD, Melbourne CA, Batini C, Fawcett KA, Song K, Sakornsakolpat P, Li X, Boxall R, Reeve NF, Obeidat M, Zhao JH, Wielscher M, Weiss S, Kentistou KA, Cook JP, Sun BB, Zhou J, Hui J, Karrasch S, Imboden M, Harris SE, Marten J, Enroth S, Kerr SM, Surakka I, Vitart V, Lehtimäki T, Allen RJ, Bakke PS, Beaty TH, Bleecker ER, Bossé Y, Brandsma CA, Chen Z, Crapo JD, Danesh J, DeMeo DL, Dudbridge F, Ewert R, Gieger C, Gulsvik A, Hansell AL, Hao K, Hoffman JD, Hokanson JE, Homuth G, Joshi PK, Joubert P, Langenberg C, Li X, Li L, Lin K, Lind L, Locantore N, Luan J, Mahajan A, Maranville JC, Murray A, Nickle DC, Packer R, Parker MM, Paynton ML, Porteous DJ, Prokopenko D, Qiao D, Rawal R, Runz H, Sayers I, Sin DD, Smith BH, Soler Artigas M, Sparrow D, Tal-Singer R, Timmers P, Van den Berge M, Whittaker JC, Woodruff PG, Yerges-Armstrong LM, Troyanskaya OG, Raitakari OT, Kähönen M, Polašek O, Gyllensten U, Rudan I, Deary IJ, Probst-Hensch NM, Schulz H, James AL, Wilson JF, Stubbe B, Zeggini E, Jarvelin MR, Wareham N, Silverman EK, Hayward C, Morris AP, Butterworth AS, Scott RA, Walters RG, Meyers DA, Cho MH, Strachan DP, Hall IP, Tobin MD, Wain LV. New genetic signals for lung function highlight pathways and chronic obstructive pulmonary disease associations across multiple ancestries. Nat Genet 2019;51(3):481–493.
Moll M, Sakornsakolpat P, Shrine N, Hobbs BD, DeMeo DL, John C, Guyatt AL, McGeachie MJ, Gharib SA, Obeidat Me, Lahousse L, Wijnant SRA, Brusselle G, Meyers DA, Bleecker ER, Li X, Tal-Singer R, Manichaikul A, Rich SS, Won S, Kim WJ, Do AR, Washko GR, Barr RG, Psaty BM, Bartz TM, Hansel NN, Barnes K, Hokanson JE, Crapo JD, Lynch D, Bakke P, Gulsvik A, Hall IP, Wain L, Soler Artigas M, Jackson VE, Strachan DP, Hui J, James AL, Kerr SM, Polasek O, Vitart V, Marten J, Rudan I, Kähönen M, Surakka I, Gieger C, Karrasch S, Rawal R, Schulz H, Deary IJ, Harris SE, Enroth S, Gyllensten U, Imboden M, Probst-Hensch NM, Lehtimäki T, Raitakari OT, Langenberg C, Luan Ja, Wareham N, Zhao JH, Hayward C, Murray A, Porteous DJ, Smith BH, Jarvelin M-R, Wielscher M, Joshi PK, Kentistou KA, Timmers PRHJ, Wilson JF, Cook JP, Lind L, Mahajan A, Morris AP, Ewert R, Homuth G, Stubbe B, Weiss S, Zeggini E, Weiss ST, Silverman EK, Dudbridge F, Tobin MD, Cho MH. Chronic obstructive pulmonary disease and related phenotypes: polygenic risk scores in population-based and case-control cohorts. The Lancet Respiratory Medicine. 2020;8(7):696–708.
Moll M, Lutz SM, Ghosh AJ, Sakornsakolpat P, Hersh CP, Beaty TH, Dudbridge F, Tobin MD, Mittleman MA, Silverman EK, Hobbs BD, Cho MH. Relative contributions of family history and a polygenic risk score on COPD and related outcomes: COPDGene and ECLIPSE studies. BMJ Open Respir Res 2020;7(1).
Zhang P-D, Zhang X-R, Zhang A, Li Z-H, Liu D, Zhang Y-J, Mao C. Associations of genetic risk and smoking with incident chronic obstructive pulmonary disease. European Respiratory Journal 2021:2101320.
Kim W, Moll M, Qiao D, Hobbs BD, Shrine N, Sakornsakolpat P, Tobin MD, Dudbridge F, Wain LV, Ladd-Acosta C, Chatterjee N, Silverman EK, Cho MH, Beaty TH. Interaction of cigarette smoking and polygenic risk score on reduced lung function. JAMA Netw Open. 2021;4(12):e2139525.
Gim J, An J, Sung J, Silverman EK, Cho MH, Won S. A Between ethnicities comparison of chronic obstructive pulmonary disease genetic risk. Front Genet. 2020;11:329.
Au Yeung SL, Borges MC, Lawlor DA. Association of genetic instrumental variables for lung function on coronary artery disease risk: A 2-Sample Mendelian Randomization Study. Circ Genom Precis Med. 2018;11(4):e001952.
Au Yeung SL, Borges MC, Lawlor DA, Schooling CM. Impact of lung function on cardiovascular diseases and cardiovascular risk factors: a two sample bidirectional Mendelian randomisation study. Thorax 2021.
Higbee DH, Granell R, Sanderson E, Davey Smith G, Dodd JW. Lung function & cardiovascular disease. A Two Sample Mendelian Randomisation Study. Eur Respir J 2021.
Li C, Aronsson CA, Hedblad B, Gullberg B, Wirfält E, Berglund G. Ability of physical activity measurements to assess health-related risks. Eur J Clin Nutr. 2009;63(12):1448–51.
Abraham G, Qiu Y, Inouye M. FlashPCA2: principal component analysis of Biobank-scale genotype datasets. Bioinformatics. 2017;33(17):2776–8.
McCarthy S, Das S, Kretzschmar W, Delaneau O, Wood AR, Teumer A, Kang HM, Fuchsberger C, Danecek P, Sharp K, Luo Y, Sidore C, Kwong A, Timpson N, Koskinen S, Vrieze S, Scott LJ, Zhang H, Mahajan A, Veldink J, Peters U, Pato C, van Duijn CM, Gillies CE, Gandin I, Mezzavilla M, Gilly A, Cocca M, Traglia M, Angius A, Barrett JC, Boomsma D, Branham K, Breen G, Brummett CM, Busonero F, Campbell H, Chan A, Chen S, Chew E, Collins FS, Corbin LJ, Smith GD, Dedoussis G, Dorr M, Farmaki AE, Ferrucci L, Forer L, Fraser RM, Gabriel S, Levy S, Groop L, Harrison T, Hattersley A, Holmen OL, Hveem K, Kretzler M, Lee JC, McGue M, Meitinger T, Melzer D, Min JL, Mohlke KL, Vincent JB, Nauck M, Nickerson D, Palotie A, Pato M, Pirastu N, McInnis M, Richards JB, Sala C, Salomaa V, Schlessinger D, Schoenherr S, Slagboom PE, Small K, Spector T, Stambolian D, Tuke M, Tuomilehto J, Van den Berg LH, Van Rheenen W, Volker U, Wijmenga C, Toniolo D, Zeggini E, Gasparini P, Sampson MG, Wilson JF, Frayling T, de Bakker PI, Swertz MA, McCarroll S, Kooperberg C, Dekker A, Altshuler D, Willer C, Iacono W, Ripatti S, Soranzo N, Walter K, Swaroop A, Cucca F, Anderson CA, Myers RM, Boehnke M, McCarthy MI, Durbin R. A reference panel of 64,976 haplotypes for genotype imputation. Nat Genet. 2016;48(10):1279–83.
Ge T, Chen CY, Ni Y, Feng YCA, Smoller JW. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nature Communications 2019;10.
Shaun Purcell CC. PLINK v1.90b6.9www.cog-genomics.org/plink/1.9/
Rapola JM, Virtamo J, Korhonen P, Haapakoski J, Hartman AM, Edwards BK, Heinonen OP. Validity of diagnoses of major coronary events in national registers of hospital diagnoses and deaths in Finland. Eur J Epidemiol. 1997;13(2):133–8.
Engström G, Hedblad B, Stavenow L, Tydén P, Lind P, Janzon L, Lindgärde F. Fatality of future coronary events is related to fnflammation-sensitive plasma proteins. Circulation. 2004;110(1):27–31.
Engstrom G, Berglund G, Goransson M, Hansen O, Hedblad B, Merlo J, Tyden P, Janzon L. Distribution and determinants of ischaemic heart disease in an urban population. A study from the myocardial infarction register in Malmo, Sweden. J Intern Med. 2000;247(5):588–96.
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450.
Pencina MJ, D’Agostino RB, Sr., Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30(1):11–21.
Mosley JD, Gupta DK, Tan J, Yao J, Wells QS, Shaffer CM, Kundu S, Robinson-Cohen C, Psaty BM, Rich SS, Post WS, Guo X, Rotter JI, Roden DM, Gerszten RE, Wang TJ. Predictive accuracy of a polygenic risk score compared with a clinical risk score for incident coronary heart disease. JAMA. 2020;323(7):627–35.
Tikkanen E, Havulinna AS, Palotie A, Salomaa V, Ripatti S. Arteriosclerosis. genetic risk prediction and a 2-stage risk screening strategy for coronary heart disease. Thromb Vascular Biology. 2013;33(9):2261–6.
Sparrow D, Weiss ST, Vokonas PS, Cupples LA, Ekerdt DJ, Colton T. Forced vital capacity and the risk of hypertension. The Normative Aging Study. Am J Epidemiol. 1988;127(4):734–41.
Enright PL, Kronmal RA, Smith VE, Gardin JM, Schenker MB, Manolio TA. Reduced vital capacity in elderly persons with hypertension, coronary heart disease, or left ventricular hypertrophy. Cardiovasc Health Study Chest. 1995;107(1):28–35.
Schnabel E, Nowak D, Brasche S, Wichmann HE, Heinrich J. Association between lung function, hypertension and blood pressure medication. Respir Med. 2011;105(5):727–33.
Zhu J, Zhao H, Chen D, Tse LA, Kinra S, Li Y. Genetic correlation and bidirectional causal association between type 2 diabetes and pulmonary function. Front Endocrinol (Lausanne). 2021;12:777487.
Klein OL, Krishnan JA, Glick S, Smith LJ. Systematic review of the association between lung function and Type 2 diabetes mellitus. Diabet Med. 2010;27(9):977–87.
Yeh HC, Punjabi NM, Wang NY, Pankow JS, Duncan BB, Brancati FL. Vital capacity as a predictor of incident type 2 diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care. 2005;28(6):1472–9.
Engstrom G, Hedblad B, Nilsson P, Wollmer P, Berglund G, Janzon L. Lung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort study. J Intern Med. 2003;253(5):574–81.
Shah CH, Reed RM, Liang Y, Zafari Z. Association between lung function and future risks of diabetes, asthma, myocardial infarction, hypertension and all-cause mortality. ERJ Open Research. 2021;7(3):00178–2021.
Lee HM, Liu MA, Barrett-Connor E, Wong ND. Association of lung function with coronary heart disease and cardiovascular disease outcomes in elderly: the Rancho Bernardo study. Respir Med. 2014;108(12):1779–85.
Sabia S, Shipley M, Elbaz A, Marmot M, Kivimaki M, Kauffmann F, Singh-Manoux A. Why does lung function predict mortality? Results from the Whitehall II Cohort Study. Am J Epidemiol. 2010;172(12):1415–23.
Acknowledgements
The authors acknowledge the information provided by the National Diabetes Register of Sweden, the Malmö HbA1c Register, the Diabetes 2000 register, and the registers provided by the Swedish Board of Health and Welfare.
Funding
We acknowledge support from Swedish Heart -Lung foundation (2020 − 0173), Magnus Bergvall’s foundation (2021–04187) and Lund University Infrastructure grant ”Malmö population-based cohorts” (STYR 2019/2046). The Regeneron Genetics Center is a subsidiary of Regeneron Pharmaceuticals, Inc.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
GE, SZ, IG and JS designed the study. JS and SZ performed the statistical analyses. GE, IG, JS and SZ contributed to the analysis. SZ, GE, JS, IG and Regeneron Genetics Centre contributed to interpretation of the data. SZ drafted the first manuscript. GE, IG, JS, SZ and Regeneron Genetics Centre contributed to the critical revision of the manuscript. GE, IG, JS, SZ and Regeneron Genetics Centre reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For MDCS, all participants provided written consent, and the Ethical Committee at Lund University, Lund, Sweden approved the study (LU 51–90, LU 2009/633, LU 2011/356). For MPP, written consent was not available between 1974 and 1992, however verbal consent was taken for all participants included in the study. The Regional Ethics Committee at Lund (LU 85–2004; LU 2011–412) approved prospective follow-up of the cohort and data linkage with the national Cause of Death and Patient Registers.
Consent for publication
Not applicable.
Competing interests
SZ, IG, GE and JS have no conflicts of interest to declare. The Regeneron Genetics Center is a subsidiary of Regeneron Pharmaceuticals, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Regeneron Genetics Center: A full list of members appears in the Supplementary Information.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12933_2022_1661_MOESM1_ESM.docx
Supplementary Material 1: Supplement Table 1: Baseline association between risk factors and FEV1-PGS (n=27 438). Supplement Table 2: Univariate regression for mean systolic blood pressure by quartiles of PGS further adjusted for apolipoproteins (n=26536). Supplement Table 3: Health outcomes by quartiles of FEV1 PGS and by 1 SD increase in FEV1 PGS. Supplement Table 4: Sensitivity analysis of outcomes after further adjustment for apolipoproteins by FEV1 and FVC PGS.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zaigham, S., Gonçalves, I., Center, R.G. et al. Polygenic scores for low lung function and the future risk of adverse health outcomes. Cardiovasc Diabetol 21, 230 (2022). https://doi.org/10.1186/s12933-022-01661-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01661-y