Abstract
Background
Sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RA) lower blood pressure (BP). When SGLT2i and GLP-1RA are combined, synergistic effects on BP have been observed. The mechanisms underlying these BP reductions are incompletely understood. The aim of this study was to assess the mechanisms underlying the BP reduction with the SGLT2i dapagliflozin, GLP-1RA exenatide, and dapagliflozin-exenatide compared with placebo in people with obesity and type 2 diabetes.
Methods
Sixty-six people with type 2 diabetes were randomized to 16 weeks of dapagliflozin 10 mg/day, exenatide 10 µg twice daily, dapagliflozin-exenatide, or placebo treatment. The effect of treatments on estimates of: (1) plasma volume (calculated by Strauss formula, bioimpedance spectroscopy, hematocrit, (2) autonomic nervous system activity (heart rate variability), (3) arterial stiffness (pulse wave applanometry), (4) systemic hemodynamic parameters including peripheral vascular resistance, cardiac output and stroke volume (all derived from non-invasively systemic hemodynamic monitoring), and (5) natriuresis (24-hour urine collection) were assessed after 10 days and 16 weeks of treatment.
Results
After 10 days, dapagliflozin reduced systolic BP (SBP) by − 4.7 mmHg, and reduced plasma volume. After 16 weeks, dapagliflozin reduced SBP by − 4.4 mmHg, and reduced sympathetic nervous system (SNS) activity. Exenatide had no effect on SBP, but reduced parasympathetic nervous system activity after 10 days and 16 weeks. After 10 days, dapagliflozin-exenatide reduced SBP by − 4.2 mmHg, and reduced plasma volume. After 16 weeks, dapagliflozin-exenatide reduced SBP by − 6.8 mmHg, and the reduction in plasma volume was still observed, but SNS activity was unaffected.
Conclusions
The dapagliflozin-induced plasma volume contraction may contribute to the initial SBP reduction, while a reduction in SNS activity may contribute to the persistent SBP reduction. Dapagliflozin-exenatide resulted in the largest decrease in SBP. The effect on plasma volume was comparable to dapagliflozin monotherapy, and SNS activity was not reduced, therefore other mechanisms are likely to contribute to the blood pressure lowering effect of this combination, which need further investigation.
Trial registration Clinicaltrials.gov, NCT03361098.
Similar content being viewed by others
Introduction
Type 2 diabetes (T2D) is associated with cardiovascular (CV) morbidity and mortality, due to a combination of effects of hyperglycemia and frequently associated obesity, dyslipidemia and hypertension. In the last decades, two novel drug classes have been developed, which reduce multiple cardiovascular risk factors: inhibitors of the sodium-glucose cotransporter 2 (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RAs) [1].
SGLT2i improve CV outcomes (3-MACE), in particular (hospitalization for) heart failure, and mortality in patients with atherosclerotic disease, irrespective of the presence of diabetes [2,3,4], suggesting that the CV benefit occurs beyond glucose lowering. Blood pressure (BP) reduction could partially contribute to the improved CV outcomes. The systolic BP lowering effect of SLGT2i is around 4 mmHg [5]. The underlying mechanisms for the BP lowering effect remain incompletely understood, but a sustained reduced plasma volume could contribute [6, 7]. Because reductions in plasma volume and (arterial) BP occur without a rise in heart rate (HR), it has been suggested that sympathetic nervous system (SNS) activity is also reduced [3, 8,9,10]. Improvements in arterial stiffness and improved endothelial function have also been proposed to contribute to the long-term BP reduction [11,12,13].
Similar to SGLT2i, GLP-1RAs reduce cardiovascular disease (CVD) in T2D patients [14,15,16,17,18], and their mode of action is also not completely understood, but is likely multifactorial. GLP-1RAs reduce BP (the size of the reduction is dependent of the agent used), which may contribute to the reduction in CVD [19,20,21]. Mechanisms of the BP effect of GLP-1-RA may include contributions from reduced vascular resistance, natriuresis and body weight reduction [22].
Treatments that address more than one regulatory pathway are intended to enhance efficacy by synergistic responses that result from potentially engaging complementary mechanisms. Therefore, given their unique mechanisms of lowering glucose and body weight, the combination of SGLT2i and GLP-1RA appears promising [23,24,25]. Importantly, in DURATION-8, dapagliflozin plus exenatide resulted in a synergistic (i.e., larger than the sum of the BP reductions with both individual treatments) SBP reduction (− 4.3 mmHg) versus dapagliflozin or exenatide monotherapy after 28 weeks (− 1.8 mmHg and − 1.2 mmHg respectively) [25]. In two other trials, the addition of GLP-1RA to ongoing SGLT2i treatment also further reduced SBP (semaglutide − 4.7 mmHg, dulaglutide − 4.5 mmHg) [24, 26]. Both agents may reduce BP via similar pathways, but also potentially intervene in different regulatory pathways, which could induce a synergistic SBP reduction. Therefore, the aim of this study was to assess the mechanisms underlying the blood pressure reduction (i.e., changes in plasma volume, autonomic nervous system (ANS) activity, arterial stiffness, vascular resistance, and natriuresis) with dapagliflozin, exenatide, and dapagliflozin plus exenatide compared with placebo in people with obesity and type 2 diabetes.
Methods
Trial design
This was a prespecified secondary analysis of the DECREASE study: a monocenter, randomized, double-blind, placebo-controlled trial primarily designed to assess the separate and combined effects of dapagliflozin and exenatide versus placebo on activity in central reward and satiety circuits in response to food related stimuli in obese T2D subjects [27]. The study was conducted between September 2017 and May 2020 at the Amsterdam University Medical Centers, location VUmc, Amsterdam, The Netherlands. The study protocol, protocol amendments, and any other protocol-specific documents were reviewed and approved by local authorities and the ethics review board of the Amsterdam University Medical Center, location VUmc. The study complied with the Declaration of Helsinki and Good Clinical Practice guidelines and was registered at the ClinicalTrials.gov (NCT03361098).
Participants
Participants were recruited from our outpatient clinic database and by advertisement in local newspapers. Eligible participants were men or postmenopausal women, aged 18–75 years, with a stable body weight (< 5% reported change during the previous 3 months), a BMI > 25 kg/m2, and diagnosed with T2D. For the current treatment of T2D metformin with or without sulfonylurea derivatives was allowed (stable dose for ≥ 3 months). HbA1c levels for participants treated with metformin monotherapy were 7–10% (53–86 mmol/mol) and for metformin plus sulfonylurea 7.5–10% (58–86 mmol/mol). Exclusion criteria were a history of severe cardiovascular, renal or liver disease, malignancies (excluding basal cell carcinoma), uncontrolled thyroid disease, the use of any centrally acting agent or oral glucocorticoids, substance abuse, neurological or psychiatric disease including eating disorders and depression and MRI contra-indications. Written informed consent was obtained from all participants.
Study protocol
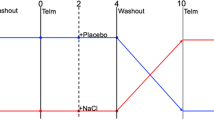
The detailed study protocol was previously published [27]. In short, participants were randomized using block randomization (1:1:1:1) to one of the four treatment groups: (1) SGLT2i dapagliflozin 10 mg/day in combination with placebo of the GLP-1RA exenatide, (2) exenatide 10 µg twice daily in combination with placebo of dapagliflozin, (3) combination of both dapagliflozin plus exenatide, or (4) double placebo. To maintain blinding throughout the study, participants were treated in a double-dummy design. There was no difference in appearance between exenatide and placebo injections or dapagliflozin or placebo tablets. Adherence was followed up by counting the remaining capsules and injection pens at all visits.
Endpoint measurements
The study consisted of three endpoint visits: at baseline, after 10 days of treatment (short-term effects), and after 16 weeks of treatment (long-term effects). At each visit, measurements of anthropometrics were performed and blood was drawn for fasting outcome variables. On each visit, patients arrived at 8:30 am after an overnight fast at the research unit. They were instructed to refrain from vigorous physical activity and alcohol ingestion for at least 24 h, and to withhold from caffeine for more than 12 h.
Prior to each measurement patients were acclimatized for at least 10 min. All measurements were performed in the fasting state, in a semi-supine position, and in a temperature controlled room (23.0 ± 1.0 °C). Measurements were performed at the non-dominant arm comfortably placed at heart level and appropriate cuff sizes were used where applicable.
Heart rate variability measures
Using an electrocardiogram (ECG)-equipped Nexfin device, 5-min RR-interval recordings were obtained, during which patients were instructed to breath spontaneously (range 10–18 breaths/min) and to refrain from sleeping or speaking. ECG-measurements were visually inspected and artifacts were manually corrected using linear interpolation. ECG recordings were loaded into Kubios heart rate variability (HRV) analysis software 2.2 (University of Eastern Finland, Biosignal Analysis and Medical Imaging Group, Kuopio, Finland). After additional automated low-level artifact correction and removal of trend components, Fast Fourier spectral analyses were performed to obtain normalized low frequency (LF; 0.04–0.15 Hz) and high frequency (HF; 0.15–0.5 Hz) bands, from which the low frequency/high frequency ratio (LF/HF ratio), a validated marker for cardiac sympathovagal-balance [13], was calculated. In addition, the standard deviation of the R-R intervals (SDNN), and the root mean square of successive differences (RMSSD) were calculated as measures of heart rate variability. Parasympathetic activity was assessed by RMSSD and SDNN, whereas LF/HF ratio assessed sympathovagal-balance, with LF contributing to the sympathetic activity and HF to the parasympathetic activity [28, 29].
Systemic hemodynamic function
SBP, DBP, mean arterial pressure (MAP), and HR were determined by an automated oscillometric device (Dinamap, GE Healthcare, Little Chalfont, UK). All measurements were performed in triplicate at 1–2 min intervals, the mean of the three measurements was used for each time point. Pulse pressure (PP) was calculated by subtracting DBP from SBP. Stroke volume (SV), cardiac output (CO) and systemic vascular resistance (SVR) were calculated from noninvasive beat-to-beat finger arterial photoplethysmography BP measurements (Nexfin, Amsterdam, The Netherlands). The finger BP-measurements were performed over a period of 30s, and a mean was derived using dedicated software (Nexfin@PC version 2.0, BM Eye, Amsterdam, The Netherlands).
Plasma volume
Participants collected 24 h urine samples that ended on the night before testing. Urinary excretion of volume, sodium and glucose were subsequently measured. Bioimpedance spectroscopy (BIS) (ImpediMed Limited, Pinkenba, Queensland, Australia) for assessment of extra- and intracellular volume was performed. Blood was drawn from the cubital vein to measure hematocrit. The percentage change in estimated plasma volume (ePV) was calculated by the Strauss formula [30,31,32]:
Pulse wave analysis
Pulse wave analysis (PWA) was performed at the radial artery using applanation tonometry with a high fidelity micromanometer (SPT-301; Millar Instruments, Houston, Texas, USA) coupled to a SphygmoCor® System (Atcor Medical, West Ryde, Australia) to assess arterial stiffness [33, 34]. The average of two recordings (of ≥ 12 s) was used, which needed to have adequate pulse wave profiles and a high-quality control, defined as an in-device quality index of more than 80%. The central aortic pressure wave form was derived from the radial artery waveform using the software’s mathematical transfer function [33, 34]. The augmentation index (an indicator of arterial stiffness) was calculated as the augmentation pressure, that is, the pressure of the second systolic peak minus the pressure at the inflection point, expressed as percentage of the pulse pressure and normalized for a HR of 75 bpm (AIX@HR75).
Statistical analyses
All statistical analyses were performed using SPSS 26.0 (IBM SPSS). Linear mixed models (LMM) were performed to investigate treatment effects versus placebo over time in the per protocol population. For the change in BP, within group differences were also calculated. Treatment allocation was set as independent variable in dummy variables, and the endpoint of interest as dependent variable. Time was added as fixed factor. The treatment allocation interaction with time, as well as a random intercept were included in the model. Also, corresponding baseline values were added as independent variable. P value < 0.05 was considered as statistically significant. No corrections for multiple testing were performed, because we felt that false-negative findings would be more troublesome for this mechanistic study compared with false-positive findings.
Results
Baseline characteristics
One hundred and six people were screened, of whom 68 were included. Before randomisation three patients were excluded due to undiagnosed claustrophobia (important for primary endpoint). Two patients dropped out just before the last test visit, one because of personal reasons (placebo group), the other one because of ongoing nausea (combination group). In total, seven patients were excluded in the analysis for ANS activity; five patients with atrial fibrillation (n = 1 dapagliflozin, n = 3 combination, n = 1 placebo), one patient with severe sinus arrhythmia in the combination group, and one patient who started metoprolol during the study in the placebo group (Fig. 1). Baseline characteristics of the per protocol population (n = 56) were well balanced between treatment (Table 1). For all participants, the medications used at baseline, remained unchanged during the study. Medication adherence for dapagliflozin (or placebo) was 99.0% and for exenatide (or placebo) 97.5%.
Glycemic and body weight effects
All active treatments resulted in significant reductions in HbA1c and body weight, with the largest reduction in the dapagliflozin plus exenatide group compared with placebo after adjustment for baseline (HbA1c%: − 1.2 ± 0.19%; body weight: − 2.8 ± 0.5 kg) [27].
Blood pressure and heart rate
After 10 days, dapagliflozin treatment resulted in SBP reduction of − 4.7 ± 2.1 mmHg (p = 0.047), and after 16 weeks in a SBP reduction of − 4.4 ± 2.7 mmHg (p = 0.13). Exenatide had no significant effect on SBP. After 10 days, dapagliflozin-exenatide reduced SBP by − 4.2 ± 1.9 mmHg (p = 0.046), and after 16 weeks by − 6.8 ± 2.4 mmHg (p = 0.015). Placebo had no significant effect on SBP (Table 2). After correction for placebo values dapagliflozin numerically reduced BP after 10 days of treatment (− 4.5 ± 2.9 mmHg, p = 0.13). Exenatide had no effect on SBP. Dapagliflozin plus exenatide resulted in the largest BP reduction of − 6.4 ± 3.0 mmHg (p = 0.039) after 10 days, and − 6.7 ± 3.1 mmHg (p = 0.033) after 16 weeks. HR was numerically increased by exenatide and dapagliflozin plus exenatide, but not by dapagliflozin (Table 2).
Indicators of plasma volume
Dapagliflozin compared with placebo tended to increase urine volume by 419.4 ± 220.6 ml/24 h (p = 0.06; 10 days), but not after 16 weeks (244.1 ± 224.1 ml/24 h, p = 0.28). Dapagliflozin compared with placebo showed a small non-significant increase in hematocrit (1.2 ± 0.8%, p = 0.17). Dapagliflozin compared with placebo decreased extracellulair fluid (− 1.1 ± 0.4 L, p = 0.013) after 10 days, but not after 16 weeks (− 0.6 ± 0.4 L, p = 0.17). Dapagliflozin compared with placebo reduced estimated plasma volume (ePV) by − 3.5% (95% CI − 7.7 to − 0.7, p = 0.001) after 10 days, but not after 16 weeks (− 1.3%, 95% CI − 4.3 to 6.7, p = 0.55) (Table 3).
After 10 days, exenatide compared with placebo had no effect on any of the 24 h urine measurements. After 16 weeks of treatment, exenatide compared with placebo tended to decrease urine volume by − 429.6 ± 222.4 ml/24 h (p = 0.056). Hematocrit was decreased by − 2.4 ± 0.9% (p = 0.006). Extracellular fluid and ePV were unaffected (Table 3).
Dapagliflozin plus exenatide compared with placebo tended to increase urine volume after 10 days (391.9 ± 231.5 ml/24 h, p = 0.09), but not after 16 weeks of treatment. Hematocrit was increased by 2.0 ± 0.9% (p = 0.029) after 10 days, but only showed a small numerical increase after 16 weeks (1.3 ± 0.9%, p = 0.16). Dapagliflozin plus exenatide compared with placebo numerically reduced extra-cellular fluid after 10 days (− 0.7 ± 0.4, p = 0.13), but not after 16 weeks. Dapagliflozin plus exenatide compared with placebo reduced ePV by − 4.2% (95% CI − 8.8 to − 0.4, p = 0.014) after 10 days, and by − 3.9% (95% CI − 9.8 to − 1.9, p = 0.045) after 16 weeks (Table 3; Fig. 2).
Linear mixed models were used to compare baseline corrected treatment effects with placebo. Changes in A autonomic balance, B indirect measurements of plasma volume after dapagliflozin (blue circle), exenatide (red square), dapagliflozin plus exenatide (purple upward triangle after 10 days, and 16 weeks of treatment. Data points represent mean with SEM. Statistically significant mean differences of treatments compared with placebo corrected for baseline values are indicated as *(P < 0.05), **(P < 0.01), ***(P < 0.001)
Autonomic nervous system activity
After 10 days, dapagliflozin compared with placebo had no effect on LF/HF ratio. Dapagliflozin compared with placebo tended to reduce LF/HF ratio by − 1.1 ± 0.6 (p = 0.06) after 16 weeks (an indicator of reduced sympathetic activity) (Table 3; Fig. 2). No effect on SDNN or RMSSD was observed.
After 10 days and 16 weeks, exenatide compared with placebo had no effect on LF/HF ratio. After 16 weeks, exenatide significantly reduced SDNN (− 8.1 ± 3.6, p = 0.027) and tended to reduce RMSSD (− 8.4 ± 4.4, p = 0.058) (an indicator of reduced parasympathetic activity) (Table 3; Fig. 2).
Although dapagliflozin plus exenatide compared with placebo had no effect on LH/HF ratio after 10 days and 16 weeks, dapagliflozin plus exenatide reduced RMSSD (10 days: − 11.4 ± 4.6 p = 0.015; 16 weeks: − 10.7 ± 4.8 p = 0.029) and SDNN (10 days: − 9.6 ± 3.7 p = 0.012; 16 weeks: − 8.7 ± 3.9 p = 0.030) (an indicator of reduced parasympathetic activity) (Table 3; Fig. 2).
Systemic hemodynamic function
Dapagliflozin compared with placebo had no effect on SV, CO or SVR. Exenatide compared with placebo reduced SV by − 10.4 ± 4.2 ml (p = 0.014) after 16 weeks of treatment. CO and SVR were unaffected by exenatide treatment. Dapagliflozin plus exenatide compared with placebo tended to reduce SV by − 7.2 ± 4.4 ml (p = 0.11) after 16 weeks of treatment (Table 3; Fig. 2). CO and SVR were unaffected in the combination group.
Arterial stiffness
None of the treatments had a statistical significant effect on arterial stiffness (AIX@HR75 or PP) (Table 3).
Discussion
This secondary prespecified analysis of a randomized double-blind placebo controlled trial investigated potential mechanisms underlying the BP reduction with SGLT2i and GLP-1RA, and their combination, in obese people with type 2 diabetes. We observed that dapagliflozin reduced SBP, and combination of dapagliflozin and exenatide caused a superior effect on SBP lowering, which is in line with previous studies [24,25,26, 35, 36]. Dapagliflozin induced plasma volume contraction after 10 days of treatment, which could contribute to the acute drop in SBP. After 16 weeks of treatment, measures of plasma volume returned to baseline levels, but dapagliflozin reduced SNS activity, possibly contributing to the persistent SBP reduction. Dapagliflozin plus exenatide also induced plasma volume contraction after 10 days, contributing to the acute drop in SBP, and to a lesser extent after 16 weeks of treatment, possibly contributing to the persistent reduction in SBP. However, after 16 weeks of treatment, there was no reduction in SNS activity in the combination group, suggesting that other mechanisms contribute to the synergistic SBP reduction after 16 weeks of treatment.
We investigated underlying mechanisms which could explain the decrease in BP with dapagliflozin. SGLT2i may induce plasma volume contraction, leading to reductions in cardiac pre- and after-load [6]. Sodium- and glucose-excretion may contribute to the acute plasma volume contraction. However, observed natriuresis with SGLT2i is modest when compared with diuretics, and is transient, as is returns to pretreatment levels within days [37]. The osmotic diuretic effect induced by glucosuria may not be the only contributing factor to plasma volume contraction, as similar changes in plasma volume are observed in individuals with minimal glucosuria [38, 39]. In the current study dapagliflozin reduced ePV after 10 days of treatment. In addition, dapagliflozin significantly increased glucose excretion, and numerically increased 24 h urinary volume, increased hematocrit, and decreased extracellular fluid after short-term treatment. This plasma volume contraction however, was no longer observed after 16 weeks of treatment. This suggest that plasma volume contraction contributes in particular to the acute drop in SBP with SGLT2i treatment. Although the effect on ePV in the current study was larger, these findings are in line with a previous study, in which no effect on natriuresis (after standardized sodium intake), and no significant prolonged changes in plasma volume (directly measured with indocyanine green indicator dilution method) were observed [40].
A reduction in BP and diuretic actions usually promote baroreflex-mediated increase in SNS activity, leading to an increase in heart rate. SGLT2i however, reduce BP without an increase in heart rate, which may suggest dampening of SNS activity [9]. After 10 days and 16 weeks of treatment we indeed found no reflex-mediated sympathetic activation. In line with these results, a previous study showed that 5 days of empagliflozin did not affect muscle SNS activation despite lowering BP in T2D patients [8]. In addition, another study found that 12 weeks of dapagliflozin compared with gliclazide reduced SBP, without affecting HR or SNS activity in metformin treated T2D patients [10]. Interestingly, we even found a reduction in SNS activity after 16 weeks of treatment. These findings are in line with data from animal models [41]. It could be suggested that a reduction in SNS activity contributes to the long-term BP reduction, as we only observed a reduction after 16 weeks of treatment. Improvements in glucose, insulin resistance, and hyperinsulinemia may have contributed to the reduction in SNS activity [42, 43]. Whether the effect of dapagliflozin on SNS activity is independent of these improvements needs further investigation.
Dapagliflozin plus exenatide resulted in the largest BP reduction which is in line with large combination trials [24,25,26]. The combination of dapagliflozin and exenatide reduced ePV, and tended to reduce SV, accompanied by increases in hematocrit, 24 h urinary volume and glucose excretion, reflecting plasma volume contraction after short-term treatment. After 16 weeks, the combination reduced ePV, but the other parameters were unaffected. As with dapagliflozin monotherapy, plasma volume contraction may contribute mainly to the acute drop in SBP, and to a lesser extent to the persistent SBP reduction. Interestingly, the dapagliflozin-induced reduction in SNS activity after 16 weeks was not observed in combination therapy. Instead, PNS activity was reduced, as was observed with exenatide monotherapy. It could be suggested that combination with exenatide blunted the reduction in SNS activity observed with dapagliflozin, and therefore the potential contribution of a reduced SNS activity on BP reduction. However, the combination group showed the largest SBP reduction after 16 weeks of treatment, suggesting that other mechanisms than plasma volume contraction and SNS reduction could contribute to the observed synergistic reduction in SBP with the combination therapy of SGLT2i and GLP-1RA [25]. We suggest that non osmotic sodium storage, changes in baroreceptor reflex set point/renal sympathetic nerve activity, or a central neural pathway may play an important role.
A reduction in arterial stiffness could also contribute to BP lowering effect of SGLT2i. Some studies showed a reduction in arterial stiffness, measured as augmentation index or as carotid-femoral pulse-wave velocity after acute or chronic SGLT2i treatment in patients with T2D [10, 44,45,46]. In this study we found no reduction in arterial stiffness (measured as augmentation index) with dapagliflozin or dapagliflozin plus exenatide. It should be noticed that pulse wave velocity is a more sensitive marker to detect changes in arterial stiffness in older individuals and might have been a better measure in our population [47].
Exenatide numerically reduced SBP from baseline (− 1.3 mmHg). Although some GLP-1RA induce more SBP reduction [48], the SBP reduction in this study is slightly less than the modestly observed SBP reduction with exenatide in larger trials [20, 49, 50]. In this study baseline SBP was relatively low [51]. In our study exenatide had no effect on natriuresis, SNS activity, or arterial stiffness, which is in line with previous studies [52,53,54]. SV decreased without a change in CO, which could suggest systemic vasodilation with subsequent reflex tachycardia to maintain stable perfusion. However, in this study non-invasively measured vascular resistance was not affected, but had a large standard deviation, which suggests the need for further research in a larger sample. The observed increase in HR could reduce ventricular filling time which would reduce SV, while keeping cardiac output unaffected [55]. This is in line with a previous study, in which 12 weeks of liraglutide also increased heart rate, while reducing systolic blood pressure and stroke volume, whereas vascular resistance and cardiac output where unaffected [54]. This suggest that other mechanisms, such as changes in neuroendocrine hormones (i.e. angiotensin II, ANP), or a central neural pathway may contribute to BP lowering effect of GLP-1RA [56, 57]. The increase in HR did not reach statistical significance, but the point estimate was comparable to the average increase of 2–3 bpm found in other trials [20]. Although SNS activity was unchanged, we did find a reduction in PNS activity, which may contribute to the increase in HR, confirming animal models in which a significant depression of parasympathetic modulation of heart rate was found [58, 59]. A direct effect of GLP-1RA on sino-atrial node cells was also a hypothesized mechanisms for the increase in HR, and recently demonstrated in a mice model [59]. However, cardiac GLP-1 receptor circuits controlling HR required neural inputs, as the increase in HR was not observed in isolated perfused heart or mouse atria ex vivo [59]. Therefore it could be suggested that both, direct effects on the GLP-1 receptor and reduced PNS activity contribute to the increase in HR.
While the double-blinded, double-dummy, randomized 4-armed design is a major strength, this study also has some limitations. First, although this was a mechanistic prespecified secondary outcome, the sample size was small. Due to limited statistical power, this may have led to under detection of potential changes. Therefore, the results should be interpret with caution, and be considered hypothesis generating only. A dedicated clinical trial with more power is required to confirm these findings. Second, some patients used beta blockers and RAAS inhibitors. Although these medications were equally distributed among the groups, and discontinued at the day of the measurements, they may have influenced the effect on blood pressure reduction. However, the high percentage of patients using blood pressure lowering medication is in line with clinical practice and previous clinical trials in patients with diabetes. Third, although 24 h urine collection is the gold standard method to measure sodium excretion, measurements during standardized sodium intake and multiple 24 h collections may have been more precise [60]. However, the study might have been too short of duration to detect changes in arterial stiffness. Systemic hemodynamic parameters were calculated from non-invasive pulse pressure measurement devices, but these are well validated against intra-arterial measurements [61].
Conclusions
In conclusion, our findings suggest that the dapagliflozin-induced plasma volume contraction contributes to the initial measured blood pressure reduction, while a reduction in SNS activity may contribute to the persistent blood pressure reduction. Combination therapy with dapagliflozin plus exenatide resulted in the largest decrease in blood pressure. However, as the effect on plasma volume was comparable to dapagliflozin monotherapy, and SNS activity was not reduced, other mechanisms are likely to contribute to the blood pressure lowering effect of this combination, and need further investigation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SGLT2i:
-
Sodium-glucose cotransporter-2 inhibitors
- GLP-1:
-
RA glucagon-like peptide-1 receptor agonist
- CV:
-
Cardiovascular
- T2D:
-
Type 2 diabetes
- ANS:
-
Autonomic nervous system
- PNS:
-
Parasympathetic nervous system
- SNS:
-
Sympathetic nervous system
- BMI:
-
Body mass index
- SU:
-
Sulfonylurea derivatives
- ACE:
-
Angiotensin converting enzyme
- ARB:
-
Angiotensin-II receptor blocker
- RAAS:
-
Renin–angiotensin–aldosterone system
- ECG:
-
Electrocardiogram
- HRV:
-
Heart rate variability
- LF/HF ratio:
-
Low frequency/high frequency ratio
- SDNN:
-
Standard deviation of the R-R intervals
- RMSSD:
-
Root mean square of successive differences
- BP:
-
Blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- HR:
-
Heart rate
- PP:
-
Pulse pressure
- SV:
-
Stroke volume
- CO:
-
Cardiac output
- SVR:
-
Systemic vascular resistance
- BIS:
-
Bioimpedance spectroscopy
- ePV:
-
Estimated plasma volume
- PWA:
-
Pulse wave analysis
- AIX@HR75:
-
Augmentation index normalized for a heart rate of 75 beats per minute
- LMM:
-
Linear mixed models
References
van Baar MJB, van Ruiten CC, Muskiet MHA, van Bloemendaal L, RG IJ, van Raalte DH. SGLT2 inhibitors in combination therapy: from mechanisms to clinical considerations in type 2 diabetes management. Diabetes Care. 2018;41(8):1543–56.
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008.
Zelniker TA, Braunwald E. Mechanisms of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(4):422–34.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31–9.
Baker WL, Smyth LR, Riche DM, Bourret EM, Chamberlin KW, White WB. Effects of sodium-glucose co-transporter 2 inhibitors on blood pressure: a systematic review and meta-analysis. J Am Soc Hypertens. 2014;8(4):262–75 e9.
Inzucchi SE, Zinman B, Fitchett D, Wanner C, Ferrannini E, Schumacher M, et al. How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME trial. Diabetes Care. 2018;41(2):356–63.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–34.
Jordan J, Tank J, Heusser K, Heise T, Wanner C, Heer M, et al. The effect of empagliflozin on muscle sympathetic nerve activity in patients with type II diabetes mellitus. J Am Soc Hypertens. 2017;11(9):604–12.
Scheen AJ. Effect of SGLT2 inhibitors on the sympathetic nervous system and blood pressure. Curr Cardiol Rep. 2019;21(8):70.
van Bommel EJM, Smits MM, Ruiter D, Muskiet MHA, Kramer MHH, Nieuwdorp M, et al. Effects of dapagliflozin and gliclazide on the cardiorenal axis in people with type 2 diabetes. J Hypertens. 2020. https://doi.org/10.1097/HJH.0000000000002480.
Filippatos TD, Tsimihodimos V, Elisaf MS. Mechanisms of blood pressure reduction with sodium-glucose co-transporter 2 (SGLT2) inhibitors. Expert Opin Pharmacother. 2016;17(12):1581–3.
Lopaschuk GD, Verma S. Mechanisms of cardiovascular benefits of sodium glucose co-transporter 2 (SGLT2) inhibitors: a state-of-the-art review. JACC Basic Transl Sci. 2020;5(6):632–44.
Solini A, Giannini L, Seghieri M, Vitolo E, Taddei S, Ghiadoni L, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16(1):138.
Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228–39.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44.
Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–57.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RHM, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139(17):2022–31.
Sun F, Chai S, Li L, Yu K, Yang Z, Wu S, et al. Effects of glucagon-like peptide-1 receptor agonists on weight loss in patients with type 2 diabetes: a systematic review and network meta-analysis. J Diabetes Res. 2015;2015:157201.
Sun F, Wu S, Guo S, Yu K, Yang Z, Li L, et al. Impact of GLP-1 receptor agonists on blood pressure, heart rate and hypertension among patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetes Res Clin Pract. 2015;110(1):26–37.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2032183.
Muskiet MHA, Tonneijck L, Smits MM, van Baar MJB, Kramer MHH, Hoorn EJ, et al. GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes. Nat Rev Nephrol. 2017;13(10):605–28.
Jabbour SA, Frias JP, Ahmed A, Hardy E, Choi J, Sjostrom CD, et al. Efficacy and Safety over 2 years of exenatide plus dapagliflozin in the DURATION-8 study: a multicenter, double-blind, phase 3, randomized controlled trial. Diabetes Care. 2020. https://doi.org/10.2337/dc19-1350.
Zinman B, Bhosekar V, Busch R, Holst I, Ludvik B, Thielke D, et al. Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019;7(5):356–67.
Frias JP, Guja C, Hardy E, Ahmed A, Dong F, Ohman P, et al. Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy (DURATION-8): a 28 week, multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(12):1004–16.
Ludvik B, Frias JP, Tinahones FJ, Wainstein J, Jiang H, Robertson KE, et al. Dulaglutide as add-on therapy to SGLT2 inhibitors in patients with inadequately controlled type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2018;6(5):370–81.
van Ruiten CC, van der Aart-van der Beek AB, IJzerman RG, Nieuwdorp M, Hoogenberg K, van Raalte DH, et al. Effect of exenatide twice daily and dapagliflozin, alone and in combination, on markers of kidney function in obese patients with type 2 diabetes: a prespecified secondary analysis of a randomized controlled clinical trial. Diabetes Obes Metab. 2021. https://doi.org/10.1111/dom.14410.
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017;5:258.
Shaffer F, Meehan ZM. A practical guide to resonance frequency assessment for heart rate variability biofeedback. Front Neurosci. 2020;14:570400.
Dekkers CCJ, Sjostrom CD, Greasley PJ, Cain V, Boulton DW, Heerspink HJL. Effects of the sodium-glucose co-transporter-2 inhibitor dapagliflozin on estimated plasma volume in patients with type 2 diabetes. Diabetes Obes Metab. 2019;21(12):2667–73.
Jensen J, Omar M, Kistorp C, Tuxen C, Gustafsson I, Kober L, et al. Effects of empagliflozin on estimated extracellular volume, estimated plasma volume, and measured glomerular filtration rate in patients with heart failure (empire HF renal): a prespecified substudy of a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2021;9(2):106–16.
Tanaka A, Shimabukuro M, Teragawa H, Okada Y, Takamura T, Taguchi I, et al. Reduction of estimated fluid volumes following initiation of empagliflozin in patients with type 2 diabetes and cardiovascular disease: a secondary analysis of the placebo-controlled, randomized EMBLEM trial. Cardiovasc Diabetol. 2021;20(1):105.
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL, et al. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation. 1997;95(7):1827–36.
Pauca AL, O’Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001;38(4):932–7.
Vasilakou D, Karagiannis T, Athanasiadou E, Mainou M, Liakos A, Bekiari E, et al. Sodium-glucose cotransporter 2 inhibitors for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med. 2013;159(4):262–74.
Georgianos PI, Agarwal R. Ambulatory blood pressure reduction with SGLT-2 inhibitors: dose-response meta-analysis and comparative evaluation with low-dose hydrochlorothiazide. Diabetes Care. 2019;42(4):693–700.
Tanaka H, Takano K, Iijima H, Kubo H, Maruyama N, Hashimoto T, et al. Factors affecting canagliflozin-induced transient urine volume increase in patients with type 2 diabetes mellitus. Adv Ther. 2017;34(2):436–51.
Cherney DZI, Cooper ME, Tikkanen I, Pfarr E, Johansen OE, Woerle HJ, et al. Pooled analysis of Phase III trials indicate contrasting influences of renal function on blood pressure, body weight, and HbA1c reductions with empagliflozin. Kidney Int. 2018;93(1):231–44.
Ferrannini E, Baldi S, Frascerra S, Astiarraga B, Barsotti E, Clerico A, et al. Renal handling of ketones in response to sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care. 2017;40(6):771–6.
Scholtes RA, Muskiet MHA, van Baar MJB, Hesp AC, Greasley PJ, Karlsson C, et al. Natriuretic effect of two weeks of dapagliflozin treatment in patients with type 2 diabetes and preserved kidney function during standardized sodium intake: results of the DAPASALT trial. Diabetes Care. 2021;44(2):440–7.
Wan N, Rahman A, Hitomi H, Nishiyama A. The effects of sodium-glucose cotransporter 2 inhibitors on sympathetic nervous activity. Front Endocrinol. 2018;9:421.
Conde SV, Sacramento JF, Guarino MP, Gonzalez C, Obeso A, Diogo LN, et al. Carotid body, insulin, and metabolic diseases: unraveling the links. Front Physiol. 2014;5:418.
Yamada T, Oka Y, Katagiri H. Inter-organ metabolic communication involved in energy homeostasis: potential therapeutic targets for obesity and metabolic syndrome. Pharmacol Ther. 2008;117(1):188–98.
Bonora BM, Avogaro A, Fadini GP. Extraglycemic effects of SGLT2 inhibitors: a review of the evidence. Diabetes Metab Syndr Obes. 2020;13:161–74.
Chilton R, Tikkanen I, Cannon CP, Crowe S, Woerle HJ, Broedl UC, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17(12):1180–93.
Ramirez AJ, Sanchez MJ, Sanchez RA. Diabetic patients with essential hypertension treated with amlodipine: blood pressure and arterial stiffness effects of canagliflozin or perindopril. J Hypertens. 2019;37(3):636–42.
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR, et al. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005;46(9):1753–60.
Tsapas A, Karagiannis T, Kakotrichi P, Avgerinos I, Mantsiou C, Tousinas G, et al. Comparative efficacy of glucose-lowering medications on body weight and blood pressure in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetes Obes Metab. 2021;23(9):2116–24.
Abd El Aziz MS, Kahle M, Meier JJ, Nauck MA. A meta-analysis comparing clinical effects of short- or long-acting GLP-1 receptor agonists versus insulin treatment from head-to-head studies in type 2 diabetic patients. Diabetes Obes Metab. 2017;19(2):216–27.
Drucker DJ, Buse JB, Taylor K, Kendall DM, Trautmann M, Zhuang D, et al. Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet. 2008;372(9645):1240–50.
Okerson T, Yan P, Stonehouse A, Brodows R. Effects of exenatide on systolic blood pressure in subjects with type 2 diabetes. Am J Hypertens. 2010;23(3):334–9.
Tonneijck L, Smits MM, Muskiet MH, Hoekstra T, Kramer MH, Danser AH, et al. Renal effects of DPP-4 inhibitor sitagliptin or GLP-1 receptor agonist liraglutide in overweight patients with type 2 diabetes: a 12-week, randomized, double-blind, placebo-controlled trial. Diabetes Care. 2016;39(11):2042–50.
Smits MM, Muskiet MH, Tonneijck L, Hoekstra T, Kramer MH, Diamant M, et al. Exenatide acutely increases heart rate in parallel with augmented sympathetic nervous system activation in healthy overweight males. Br J Clin Pharmacol. 2016;81(4):613–20.
Smits MM, Tonneijck L, Muskiet MH, Hoekstra T, Kramer MH, Diamant M, et al. Heart rate acceleration with GLP-1 receptor agonists in type 2 diabetes patients: an acute and 12-week randomised, double-blind, placebo-controlled trial. Eur J Endocrinol. 2017;176(1):77–86.
Zima E, Lippert M, Czygan G, Merkely B. Determination of left ventricular volume changes by intracardiac conductance using a biventricular electrode configuration. Europace. 2006;8(7):537–44.
Goud A, Zhong J, Peters M, Brook RD, Rajagopalan S. GLP-1 agonists and blood pressure: a review of the evidence. Curr Hypertens Rep. 2016;18(2):16.
Katsurada K, Nakata M, Saito T, Zhang B, Maejima Y, Nandi SS, et al. Central glucagon-like peptide-1 receptor signaling via brainstem catecholamine neurons counteracts hypertension in spontaneously hypertensive rats. Sci Rep. 2019;9(1):12986.
Griffioen KJ, Wan R, Okun E, Wang X, Lovett-Barr MR, Li Y, et al. GLP-1 receptor stimulation depresses heart rate variability and inhibits neurotransmission to cardiac vagal neurons. Cardiovasc Res. 2011;89(1):72–8.
Baggio LL, Ussher JR, McLean BA, Cao X, Kabir MG, Mulvihill EE, et al. The autonomic nervous system and cardiac GLP-1 receptors control heart rate in mice. Mol Metab. 2017;6(11):1339–49.
Lerchl K, Rakova N, Dahlmann A, Rauh M, Goller U, Basner M, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015;66(4):850–7.
Bogert LW, Wesseling KH, Schraa O, Van Lieshout EJ, de Mol BA, van Goudoever J, et al. Pulse contour cardiac output derived from non-invasive arterial pressure in cardiovascular disease. Anaesthesia. 2010;65(11):1119–25.
Acknowledgements
The authors thank Renée de Meijer, Jeanette Boerop and Ingrid Knuffman for their assistance during the test visits, as well as the subjects who participated in this study.
Funding
This work was funded by a Grant from AstraZeneca. The funder had no role in the study design, data analyses or interpretation, or drafting of the manuscript, nor in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
CCvR designed the study, conducted the experiments, performed the data analysis and wrote the article. MMS contributed to the analysis and interpretation of the data, and to writing the article. MDK contributed to the data analysis and to writing the manuscript. MHHK contributed to writing the article. EHS contributed to writing the article. DHvR contributed to writing the article. MN contributed to writing the article. RGIJ designed the study, performed the data analysis, and wrote the manuscript. CCvR and RGIJ are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol, protocol amendments, and any other protocol-specific documents were reviewed and approved by local authorities and the ethics review board of the Amsterdam University Medical Center, location VUmc. The study complied with the Declaration of Helsinki and Good Clinical Practice guidelines and was registered at the ClinicalTrials.gov (NCT03361098).
Consent for publication
Not applicable.
Competing interests
R.G.IJ. is principal investigator of studies sponsored by research grants from AstraZeneca, Eli Lilly & Co., and Novo Nordisk. Trough M.H.H.K., the Amsterdam University Medical Centers, location VUmc, received research grants from AstraZeneca, Boehringer Ingelheim, Novo Nordisk and Sanofi-Aventis. D.H.v.R. serves on advisory boards of Boehringer Ingelheim, Eli Lilly Alliance, Novo Nordisk, Sanofi, and Merck Sharp & Dohme (MSD), and received research grants from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Sanofi, and MSD. M.N. is supported by apersonal ZONMW VICI Grant 2020 (09150182010020) and received an unrestricted grant from AstraZeneca and serves on the Scientific Advisory Board of Caelus Pharmaceuticals, the Netherlands, and Kaleido, USA. All authors declare they have not received any fees personally in connection with the roles described above, as all honoraria were paid to their employer (Amsterdam University Medical Centers, location VUmc). None of these potential conflicts of interest are relevant to the current article. C.C.v.R., M.M.S., M.K., and E.H.S have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Ruiten, C.C., Smits, M.M., Kok, M.D. et al. Mechanisms underlying the blood pressure lowering effects of dapagliflozin, exenatide, and their combination in people with type 2 diabetes: a secondary analysis of a randomized trial. Cardiovasc Diabetol 21, 63 (2022). https://doi.org/10.1186/s12933-022-01492-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01492-x