Abstract
Background
Insulin resistance is a risk factor for cardiovascular disease. Recently, we have developed a novel index, FLAIS (Fasting Laboratory Assessment of Insulin Sensitivity), which accurately reflects insulin sensitivity, measured with hyperinsulinemic-euglycemic clamp, in different groups of subjects. The aim of the present study was to assess the relationship of FLAIS with cardiovascular risk factors in a population-based study.
Methods
The study group comprised 339 individuals from the ongoing Białystok Plus study, without previously known diabetes. Clinical examination, oral glucose tolerance test and the measurement of blood laboratory parameters were performed.
Results
Prediabetes (impaired fasting glucose and/or impaired glucose tolerance) was diagnosed in 165 individuals whereas type 2 diabetes was diagnosed in 19 subjects. FLAIS was lower in individuals with prediabetes and diabetes in comparison with individuals with normal glucose tolerance. FLAIS was significantly related to waist circumference, systolic and diastolic blood pressure, triglycerides, HDL-cholesterol and LDL-cholesterol in the entire study group and in the subgroups with normal glucose tolerance and with prediabetes/diabetes. HOMA-IR, QUICKI and Matsuda index were not related to blood pressure and LDL-cholesterol in individuals with normal glucose tolerance. Majority of the adjusted models with FLAIS were characterized by better fit with the data in comparison with other indices for all cardiovascular risk factors except waist circumference.
Conclusions
FLAIS represents useful index to assess the cluster of insulin resistance-associated cardiovascular risk factors in general population.
Similar content being viewed by others
Background
Insulin resistance is a risk factor for type 2 diabetes and cardiovascular disease (CVD) [1, 2]. Insulin resistance may accelerate atherogenesis and may contribute to CVD through numerous pathogenic pathways [1,2,3]. The causality of insulin resistance in coronary heart disease (CHD) development is supported by Mendelian randomization study, which demonstrated that single nucleotide polymorphisms influencing insulin resistance were associated with an increased risk of CHD [4]. In a mathematical modeling (“Archimedes model”) of simulated young (20–30 years) nondiabetic population, entered into a series of simulated clinical trials, insulin resistance was identified as the most important single cause of CHD. It was estimated that preventing insulin resistance in young adults would prevent 42% of myocardial infarctions [5].
Insulin resistance is associated with a cluster of CVD risk factors, such as central obesity, increased blood pressure, atherogenic dyslipidemia (increased triglycerides and decreased HDL-cholesterol), disturbances of glucose tolerance, which are together termed as metabolic syndrome [1, 6, 7]. These factors coexist together more often that may be explained by chance, and insulin resistance seems to play a crucial role in this clustering [1]. Insulin resistance may aggravate each of the components of metabolic syndrome, but may also independently promote inflammation and atherogenesis [1,2,3, 8]. It should also be noted that metabolic syndrome criteria are not effective in identifying insulin resistant individuals, and insulin resistant individuals not identified are also at increased CVD risk [9].
LDL-cholesterol is a well-established causal factor of atherosclerotic CVD [10]. Insulin decreases LDL-cholesterol through an increase in LDL receptor activity and LDL clearance [11]. In insulin resistant states, such as type 2 diabetes, LDL catabolism is decreased [12]. In the study of 1340 individuals with childhood or youth onset type 2 diabetes, the prevalence of dyslipidemia was 82% and high LDL-cholesterol was the most common lipid abnormality, present in 64.5% of individuals [13].
Current guidelines for CVD prevention in clinical practice include, together, with the factors describes above, conditions with the established link with insulin resistance, like increased body mass index (BMI) and type 2 diabetes, as well as interventions directed at improving insulin sensitivity, such as heathy diet and regular physical activity [14]. It is worth noting that even in nonobese nondiabetic individuals insulin resistance is predictor of CVD [15].
Thus, an early detection of insulin resistance may be important for CVD prevention. However, hyperinsulinemic-euglycemic clamp, “the gold standard” in measurement of insulin action in vivo [16], is laborious, costly and difficult to apply in everyday clinical practice. Indirect indices of insulin sensitivity/resistance utilize mainly fasting or oral glucose tolerance test (OGTT) glucose and insulin concentrations [17,18,19], however they usually display weaker accuracy in population without overt metabolic disturbances. The method of the measurement of insulin sensitivity may largely influence the results, as insulin sensitivity measured with hyerinsulinemic-euglycemic clamp, but not fasting insulin, was a predictor of CHD and stroke/transient ischemic attack [20, 21].
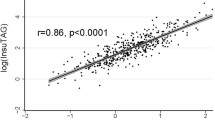
We developed a novel insulin sensitivity index, based on fasting laboratory parameters, called FLAIS (Fasting Laboratory Assessment of Insulin Sensitivity) [22], which accurately reflects insulin sensitivity, measured with hyperinsulinemic-euglcemic clamp, in different groups of subjects. This index utilizes red blood cell count (RBC), alanine aminotransferase (AlAt) activity, serum C-peptide, sex hormone-binding globulin (SHBG), adiponectin and insulin-like growth factor-binding protein 1 (IGFBP-1) concentrations. FLAIS displayed stronger correlations with clamp-derived insulin sensitivity than other indices studied [22]. Thus, we hypothesized that FLAIS may be associated with CVD risk factors.
The aim of the present study was to assess the relationship of FLAIS with CVD risk factors in a population-based study.
Methods
Study group
The study group comprised 339 individuals, 146 males and 193 females, without previously known diabetes. Participants aged 20–80 were randomly recruited from the city population database in order to reflect the general population as described previously [23]. All underwent clinical examination and appropriate laboratory tests [24]. Subject with active inflammation (CRP > 10 ng/mL) were excluded. OGTT was performed with the measurement of plasma glucose and serum insulin. Diabetes was diagnosed in patients with a glucose level at 2 h in OGTT ≥ 200 mg/dL. Prediabetes, impaired fasting glucose (IFG), and impaired glucose tolerance (IGT) were diagnosed as follows: IFG was diagnosed in patients with both fasting glucose levels 100–125 mg/dL and a glucose level at 2 h in OGTT < 140 mg/dL, and IGT was diagnosed in patients with a glucose level at 2 h in OGTT between 140 and 199 mg/dL. Glucose metabolism was considered normal if the fasting glucose level was < 100 mg/dL and the glucose level at 2 h in OGTT was < 140 mg/dL. Prediabetes (IFG and/or IGT) was diagnosed in 165 individuals whereas type 2 diabetes was diagnosed in 19 subjects. Due to the small number of subject with type 2 diabetes, individuals with prediabetes and individuals with newly diagnosed type 2 diabetes were pooled in the analyses (184 subjects, 96 males and 88 females). The remaining 155 subjects (50 males and 105 females) had normal glucose tolerance. There were no patients with unclear diabetic status in the study. In the entire study group, 14 individuals (4 with normal glucose tolerance and 10 with prediabetes/diabetes) had established CVD, including 7 with previous myocardial infarction (one person had also previous stroke), 4 with stable coronary heart disease, 3 with peripheral artery disease. Furthermore, in the entire study group, 219 individuals were not taking any medications influencing glucose metabolism or CVD risk factors, whereas 120 individuals were taking medications (most of them were taking more than one drug), including 31 receiving statins, 5—fibrates, 59—beta-blockers, 2—alpha-blockers, 22—acetylsalicylic acid, 43—angiotensin-converting enzyme inhibitors, 21—angiotensin receptor blockers, 28—calcium channel blockers, 22—diuretics, 22—levothyroxine and 3—steroids. The study protocol was approved by the local ethics committee of the Medical University of Białystok, Poland, Approval no: R-I-002/108/2016. A written informed consent was obtained from all individuals before their participation in the study.
Laboratory analyses
Plasma glucose, serum insulin, lipids were measured with standard laboratory procedures as described previously [23]. We also analyzed indirect indices of insulin sensitivity/resistance based on fasting or OGTT plasma glucose and serum insulin concentrations, homeostasis model assessment-insulin resistance (HOMA-IR) [17], quantitative insulin sensitivity check index [18] and Matsuda index (available in 337 subjects because no insulin measurements from OGTT were available in 2 subjects) [19].
Blood morphology, serum aspartate aminotransferase (AspAt) and AlAt activities were measured as previously described [22]. For the remaining measurements, serum and plasma samples were stored at − 80 °C until analyses. Serum C-peptide, SHBG, adiponectin and IGFBP-1 concentrations were measured as previously described [22].
Calculation of FLAIS
FLAIS was calculated as described previously [22]:
Statistical analysis
The statistical analysis was performed using STATISTICA 13.5 software (StatSoft Poland, Kraków). The descriptive data are presented as mean ± SD. Shapiro–Wilk test was used to asses normal distribution. Variables, which did not have normal distribution (fasting and post-OGTT insulin, triglycerides, HOMA-IR, Matsuda index, AlAt, SHBG, adiponectin and IGFBP-1) were log-transformed prior to an analyses. For the purpose of the data presentation, absolute values are shown in “Results” section. The differences between the groups with and without disturbance of glucose tolerance were estimated with the unpaired Student’s t test. The relationships between variables were studied with Pearson product moment correlation analysis and with multiple regression analysis. The differences between 2 correlation coefficients were analyzed with Fisher z transformation and two-tailed Fisher z test. The level of significance was accepted at p < 0.05.
Different multiple regression analysis models estimating the relationships of FLAIS and other indices of insulin sensitivity/resistance with CVD risk factors adjusted for age, sex, taking medications (or not) and glucose tolerance status, were compared using Akaike Information Criterion (AIC) with GraphPad Prism version 9.3.1 (GraphPad Software, San Diego, CA, USA). AIC determines which model out of 2 models analyzed better fits the data. The better model is characterized by lower AIC. Analysis of AIC indicates also the probability that the preferred model is correct.
Results
The characteristics of the study group
Subjects with prediabetes/diabetes had higher BMI, waist circumference, systolic and diastolic blood pressure, fasting and post-OGTT glucose and insulin, HOMA-IR and lower QUICKI and Matsuda index in comparison with individuals with normal glucose tolerance (all p < 0.001) (Table 1). Triglycerides (p < 0.001) and LDL-cholesterol (p = 0.014) were higher and HDL-cholesterol (p = 0.014) was lower in subjects with prediabetes/diabetes (Table 1).
All parameters forming the FLAIS index differed between the group with normal glucose tolerance and the group with prediabetes/diabetes. RBC (p = 0.012), AlAt, C-peptide (both p < 0.001) were higher whereas SHBG (p = 0.002), adiponectin and IGFBP-1 (both p < 0.001) were lower in individuals with prediabetes/diabetes in comparison with individuals with normal glucose tolerance (Table 1). FLAIS was lower in the group with prediabetes/diabetes in comparison with the group with normal glucose tolerance (p < 0.001) (Table 1).
Correlations between FLAIS, other indices of insulin sensitivity/resistance and cardiovascular risk factors
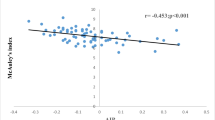
FLAIS was related to systolic and diastolic blood pressure, waist circumference, log triglycerides, HDL-cholesterol and LDL-cholesterol in the entire study group (Table 2). Correlations of FLAIS with CVD risk factors had coefficients higher or comparable as those observed for other indices of insulin sensitivity/resistance. We were able to detect statistically significant differences for the correlations of FLAIS with systolic blood pressure and HDL-cholesterol in comparison with the correlations of other indices with these parameters (systolic blood pressure, HOMA-IR p = 0.033; QUICKI, p = 0.024; HDL-cholesterol, HOMA-IR and QUICKI, p = 0.036; Matsuda p = 0.0007; p values for the comparison between 2 correlation coefficients). The correlation coefficients for FLAIS were higher than for the parameters forming FLAIS analyzed separately, except AlAt and LDL-cholesterol (Table 3). Exclusion of subjects with established CVD or receiving any treatment did not change the results (data not shown).
We also analyzed correlations of FLAIS with cardiovascular risk factors n the groups of subjects with normal glucose tolerance and with prediabetes/diabetes separately. In the group with normal glucose tolerance, FLAIS was related to systolic and diastolic blood pressure, waist circumference, triglycerides, HDL-cholesterol and LDL-cholesterol. In this group, none of other indices analyzed was related to systolic blood pressure, diastolic blood pressure and LDL-cholesterol (Table 4).
In the group with prediabetes/diabetes, FLAIS was also related to systolic and diastolic blood pressure, waist circumference, log triglycerides, HDL-cholesterol and LDL-cholesterol. Correlations of FLAIS with systolic and diastolic blood pressure and HDL-cholesterol had slightly higher correlation coefficients than those observed for other indices whereas those for other parameters analyzed they were comparable (Table 5).
Multiple regression analysis
After adjustment for age, sex, taking (or not) medications, and for glucose tolerance status (normal glucose tolerance vs prediabetes/diabetes), FLAIS was still significantly related to all analyzed cardiovascular risk factors (Table 6). Regarding other indices, none of them was significantly related to systolic blood pressure in the adjusted models. In most cases, R2 of the models with FLAIS was higher than for HOMA-IR, QUICKI and Matsuda index for all cardiovascular risk factors except waist circumference.
The direct comparison between adjusted models containing FLAIS with adjusted models containing other indices using AIC is presented in Table 6. In most cases, models with FLAIS were preferred over the models with HOMA-IR, QUICKI or Matsuda index for all cardiovascular risk factors analyzed. The exceptions were: waist circumference (all indices), triglycerides and the model with Matsuda index. For systolic blood pressure the probability that the model with FLAIS is the preferred model was over 90% and for LDL-cholesterol it was over 95% (Table 6). For triglycerides (except the model with Matsuda index) and HDL-cholesterol the probability that the model with FLAIS is the preferred model ranged from 63.7 to 83.9%, whereas for diastolic blood pressure the range of the probability was from 56.2 to 79.6% in comparison with the models with 3 other indices analyzed (Table 6).
Discussion
In the present study, we demonstrated that novel insulin sensitivity index, FLAIS, is significantly associated with CVD risk factors in population-based cohort study and thus can be applied in general population, both in individuals with normal glucose tolerance and with individuals with prediabetes/diabetes. Furthermore, HOMA-IR, QUICKI and Matsuda index were not related to blood pressure and LDL-cholesterol in individuals with normal glucose tolerance. Majority of the adjusted models with FLAIS were characterized by better fit with the data in comparison with other indices for all risk factors except waist circumference.
Identification of insulin resistance in population without disturbances in glucose tolerance may be important for CVD prevention. In our study, FLAIS was significantly related to waist circumference, systolic and diastolic blood pressure, triglycerides, HDL-cholesterol and LDL-cholesterol not only in the entire study group, but also in the subgroup with normal glucose tolerance. Importantly, none of other indices analyzed was significantly related to all CVD risk factors in the group with normal glucose tolerance. In the aforementioned study with insulin sensitivity as a negative predictor of CHD, the population was nondiabetic and approx. 80% had normal glucose tolerance at the baseline of 10-year observation [20]. In the study of 295 adolescents, insulin resistance assessed with hyperinsulinemic-euglycemic clamp was associated with CVD risk factors, systolic blood pressure, triglycerides, HDL-cholesterol and fasting insulin, and interacted with obesity in these associations [25]. It is well established that insulin resistance is related to blood pressure [26] and that subjects with hypertension demonstrate a decreased insulin sensitivity even at the early stage of the disease [27]. In this context, the relationships of FLAIS with systolic and diastolic blood pressure in the group with normal glucose tolerance provide a possible advantage of FLAIS over other indices based on glucose and insulin measurements in assessing insulin resistance-associated CVD risk in a population with normal glucose tolerance.
It is worth to underline that FLAIS, but not other indices, was related to LDL-cholesterol in the group with normal glucose tolerance. LDL-cholesterol is not a component of metabolic syndrome. However, as already mentioned, it may also be related to insulin resistance and it may also act synergistically with the components of metabolic syndrome to accelerate atherogenesis [28].
FLAIS was lower in individuals with prediabetes/diabetes and was also related to all analyzed CVD risk factors in this group. Prediabetes itself is CVD risk factor [29]. It increased the risk of unrecognized myocardial infarction in comparison to normal glucose tolerance in population without CVD at baseline [30]. Prediabetes is also associated with an increased values of the individual components of metabolic syndrome [31], as we also observed in our study. It is important to note that FLAIS was related to all CVD risk factors also in the group with prediabetes/diabetes and the correlations coefficients were slightly higher or comparable to the correlations observed for the indices based on blood glucose and insulin concentrations. One may suppose that FLAIS may accurately reflect the cluster of CVD risk factors associated with insulin resistance also in prediabetes and diabetes. It should be noted that in the adjusted models, FLAIS, but not the presence of prediabetes or diabetes, was a significant predictor of all analyzed cardiovascular risk factors. These data additionally indicate the importance of focusing on insulin resistance in the prevention of CVD.
The correlation coefficients between FLAIS and CVD risk factors were also higher than those observed for individual parameters forming FLAIS. In previous studies, increased RBC was a predictor of CVD events in 6-year follow-up [32]. Serum AlAt activity was associated with most CVD risk factors [33]. Serum C-peptide was identified as a predictor of CVD and overall death in nondiabetic adults, better than glucose and/or insulin-derived measures [34]. Higher serum SHBG was associated with a more favorable cardiometabolic risk profile [35]. Adiponectin is an adipokine with insulin-sensitizing, anti-inflammatory and antiatherogenic properties, which is inversely related to CVD risk factors [36, 37]. IGFBP- was associated with CVD events in an analysis of 3523 Framingham Heart Study participants [38]. These results are in agreement with our data showing significant correlations between parameters forming FLAIS and CVD risk factors in almost all situations (except correlations of adiponectin with LDL-cholesterol). However, the correlation coefficients of FLAIS with CVD risk factors were higher than those observed for individual parameters of FLAIS formula. Thus, similarly to the correlation between FLAIS and clamp-derived insulin sensitivity, the strength of FLAIS comes from the unique combination of the individual parameters and from balancing the contribution of each variable to the final equation.
It should be noted that Białystok Plus study is a population-based study and the individuals recruited for the study had different medical conditions and received different treatment. Our results give a support for the usefulness of FLAIS in the studies of general population. The usefulness of FLAIS as a predictor of CVD should be studies further in prospective studies.
Conclusions
FLAIS represents useful index to assess the cluster of insulin resistance-associated CVD risk factors in general population.
Availability of data and materials
The datasets analysed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- CHD:
-
Coronary heart disease
- BMI:
-
Body mass index
- OGTT:
-
Oral glucose tolerance test
- FLAIS:
-
Fasting laboratory assessment of insulin sensitivity
- RBC:
-
Red blood cells
- AlAt:
-
Alanine aminotransferase
- SHBG:
-
Sex hormone-binding globulin
- IGFBP-1:
-
Insulin-like growth factor-binding protein 1
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- HOMA-IR:
-
Homeostasis model assessment-insulin resistance
- QUICKI:
-
Quantitative insulin sensitivity check index
References
De Fronzo RA. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009. Diabetologia. 2010;53:1270–87.
Fernandez-Real JM, Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev. 2003;24:278–301.
Nigro J, Osman N, Dart AM, Little PJ. Insulin resistance and atherosclerosis. Endocr Rev. 2006;27:242–59.
Ross S, Gerstein HC, Eikelboom J, Anand SS, Yusuf S, Paré G. Mendelian randomization analysis supports the causal role of dysglycaemia and diabetes in the risk of coronary artery disease. Eur Heart J. 2015;36:1454–62.
Eddy D, Schlessinger L, Kahn R, Peskin B, Schiebinger R. Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Diabetes Care. 2009;32:361–6.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Laakso M. Is insulin resistance a feature of or a primary risk factor for cardiovascular disease? Curr Diabetes Rep. 2015;15:105.
Salazar MR, Carbajal HA, Espeche WG, Dulbecco CA, Aizpurúa M, Marillet AG, et al. Relationships among insulin resistance, obesity, diagnosis of the metabolic syndrome and cardio-metabolic risk. Diabetes Vasc Dis Res. 2011;8:109–16.
Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41:2313–30.
Ramakrishnan G, Arjuman A, Suneja S, Das C, Chandra NC. The association between insulin and low-density lipoprotein receptors. Diabetes Vasc Dis Res. 2012;9:196–204.
Duvillard L, Florentin E, Lizard G, Petit JM, Galland F, Monier S, et al. Cell surface expression of LDL receptor is decreased in type 2 diabetic patients and is normalized by insulin therapy. Diabetes Care. 2003;26:1540–4.
Amutha A, Pradeepa R, Chella KS, Anjana RM, Unnikrishnan R, Mohan V. Lipid profile in childhood- and youth-onset type 2 diabetes and their association with microvascular complications. J Assoc Physicians India. 2017;65:42–7.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Yip J, Facchini FS, Reaven GM. Resistance to insulin-mediated glucose disposal as a predictor of cardiovascular disease. J Clin Endocrinol Metab. 1998;83:2773–6.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237:E214–23.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Zethelius B, Lithell H, Hales CN, Berne C. Insulin sensitivity, proinsulin and insulin as predictors of coronary heart disease a population-based 10-year, follow-up study in 70-year old men using the euglycaemic insulin clamp. Diabetologia. 2005;48:862–7.
Wiberg B, Sundström J, Zethelius B, Lind L. Insulin sensitivity measured by the euglycaemic insulin clamp and proinsulin levels as predictors of stroke in elderly men. Diabetologia. 2009;52:90–6.
Karczewska-Kupczewska M, Nikołajuk A, Stefanowicz M, Matulewicz N, Arnoriaga-Rodriguez M, Fernandez-Real JM, et al. Novel laboratory index, based on fasting blood parameters, accurately reflects insulin sensitivity. J Clin Endocrinol Metab. 2021;106:e5208–21.
Chlabicz M, Jamiołkowski J, Łaguna W, Sowa P, Paniczko M, Łapińska M, et al. A similar lifetime CV risk and a similar cardiometabolic profile in the moderate and high cardiovascular risk populations: a population-based study. J Clin Med. 2021;10:1584.
Chlabicz M, Dubatówka M, Jamiołkowski J, Sowa P, Łapińska M, Raczkowski A, et al. Subjective well-being in non-obese individuals depends strongly on body composition. Sci Rep. 2021;11:21797.
Sinaiko AR, Steinberger J, Moran A, Prineas RJ, Vessby B, Basu S, Tracy R, Jacobs DR Jr. Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation. 2005;111:1985–91.
Jung CH, Jung SH, Lee B, Rosenberg M, Reaven GM, Kim SH. Relationship among age, insulin resistance, and blood pressure. J Am Soc Hypertens. 2017;11:359–65.
Sironi AM, Pingitore A, Ghione S, De Marchi D, Scattini B, Positano V, et al. Early hypertension is associated with reduced regional cardiac function, insulin resistance, epicardial, and visceral fat. Hypertension. 2008;51:282–8.
Howard BV, Robbins DC, Sievers ML, Lee ET, Rhoades D, Devereux RB, et al. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: The Strong Heart Study. Arterioscler Thromb Vasc Biol. 2000;20:830–5.
Brannick B, Dagogo-Jack S. Prediabetes and cardiovascular disease: pathophysiology and interventions for prevention and risk reduction. Endocrinol Metab Clin N Am. 2018;47:33–50.
Stacey RB, Leaverton PE, Schocken DD, Peregoy JA, Bertoni AG. Prediabetes and the association with unrecognized myocardial infarction in the multi-ethnic study of atherosclerosis. Am Heart J. 2015;170:923–8.
Li C, Ford ES, Zhao G, Mokdad AH. Prevalence of pre-diabetes and its association with clustering of cardiometabolic risk factors and hyperinsulinemia among U.S. adolescents: National Health and Nutrition Examination Survey. Diabetes Care. 2009;32:342–7.
Puddu PE, Lanti M, Menotti A, Mancini M, Zanchetti A, Cirillo M, et al. Red blood cell count in short-term prediction of cardiovascular disease incidence in the Gubbio population study. Acta Cardiol. 2002;57:177–85.
Bekkelund SI. Serum alanine aminotransferase activity and risk factors for cardiovascular disease in a Caucasian population: the Tromsø study. BMC Cardiovasc Disord. 2021;21:29.
Patel N, Taveira TH, Choudhary G, Whitlatch H, Wu WC. Fasting serum C-peptide levels predict cardiovascular and overall death in nondiabetic adults. J Am Heart Assoc. 2012;1:e003152.
Wang Q, Kangas AJ, Soininen P, Tiainen M, Tynkkynen T, Puukka K, et al. Sex hormone-binding globulin associations with circulating lipids and metabolites and the risk for type 2 diabetes: observational and causal effect estimates. Int J Edpidemiol. 2015;44:623–37.
Shibata R, Ouchi N, Murohara T. Adiponectin and cardiovascular disease. Circ J. 2009;73:608–14.
Orlando A, Nava E, Giussani M, Genovesi S. Adiponectin and cardiovascular risk. From pathophysiology to clinic: focus on children and adolescents. Int J Mol Sci. 2019;20:3228.
Ho JE, Lyass A, Courchesne P, Chen G, Liu C, Yin X, et al. Protein biomarkers of cardiovascular disease and mortality in the community. J Am Heart Assoc. 2018;7:e008108.
Acknowledgements
Not applicable.
Funding
Supported by the statutory subvention of Medical University of Białystok, Poland, grant number SUB/1/N/19/002/1208 and SUB/1/N/20/004/1208.
Author information
Authors and Affiliations
Contributions
MKK participated in the study design, performed the statistics, analysed data and wrote the manuscript; AN collected data and analysed data; MK, ZS, and MD collected data; AS participated in the study design and collected data, MS performed the statistics and analysed data; IK participated in the study design and revised the manuscript; KK participated in the study design, collected data and revised the manuscript. All author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocols were approved by the local ethics committee of the Medical University of Białystok, Poland. A written informed consent was obtained from all volunteers from all the groups before their participation in the study.
Consent for publication
Not applicable.
Competing interests
MKK and MS are authors of the patent regarding the presented index. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karczewska-Kupczewska, M., Nikołajuk, A., Kondraciuk, M. et al. The relationships between FLAIS, a novel insulin sensitivity index, and cardiovascular risk factors in a population-based study. Cardiovasc Diabetol 21, 55 (2022). https://doi.org/10.1186/s12933-022-01491-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01491-y