Abstract
Background
Current guidelines recommend life-long use of statin for patients with type 2 diabetes (T2D), however, a number of patients discontinue statin therapy in clinical practice. We aimed to estimate the optimal statin therapy including statin therapy duration, statin intensity, and low-density lipoprotein cholesterol (LDL-C) level among patients with T2D in a real-world setting.
Methods
From Korean National Health Insurance Service Cohort (2007–2015), 8937 patients with T2D (≥ 40 years of age) who received statin therapy for at least 90 days were included. Risk of major adverse cardiovascular event (MACE) including ischemic heart disease, ischemic stroke, and cardiovascular death was estimated according to statin intensity, achieved serum LDL-C level, and statin therapy duration, respectively. The relative contributions of these factors to MACE risk were quantified by calculating the proportion of log-likelihood explained by each factor.
Results
The hazard ratio (HR) of MACE was lower in patients receiving moderate- or high-intensity statins than in those receiving low-intensity statins (HR, 0.72; p = 0.027). Among patients who received moderate- or high-intensity statins, lower achieved LDL-C level was associated with lower cardiovascular risk. Notably, the longer the patients received statins, the lower was the risk of MACE; the HR of MACE was significantly reduced after at least 18 months (adjusted HR, 0.70; p = 0.009) as a reference to 3–6 months of therapy. The proportion of explainable log-likelihood for MACE was greatest for statin duration (2.55), followed by achieved LDL-C level (2.18), and statin intensity (0.95).
Conclusions
Statin therapy duration is as important as or more crucial than statin intensity or achieved LDL-C level for the reduction of cardiovascular risk in T2D patients. The concept of “longer is better” regarding statin therapy should be considered in clinical practice.
Similar content being viewed by others
Background
Type 2 diabetes (T2D) is frequently accompanied by dyslipidemia, which is characterized by increased triglyceride (TG), decreased high-density lipoprotein cholesterol (HDL-C), and increased small dense low-density lipoprotein cholesterol (LDL-C) particles [1, 2]. Previous studies reported that LDL-C lowering with statin therapy substantially reduces the risk of atherosclerotic cardiovascular events in patients with T2D [3,4,5], accordingly, current guidelines for dyslipidemia management generally recommend life-long use of moderate- or high-intensity statins in adult patients with T2D [6, 7].
However, debates persist regarding whether the use of statins is crucial or whether achieved LDL-C concentration determines the risk reduction of atherosclerotic cardiovascular disease. The so-called statin and LDL-C hypotheses have been supported by evidence provided by randomized controlled trials (RCT). However, these hypotheses are often not reproducible in population-based studies [8], probably due to biases that are difficult to control. One of the major biases is non-adherence to statin therapy in clinical practice. In a meta-analysis, half of the patients who newly received statins discontinued therapy within a year [9]. Therefore, adherence to statin therapy may be critical for explaining the cardiovascular benefits of statins in clinical practice. We noted that only a few studies regarding statin therapy duration have been conducted [10, 11]. In addition, the duration of follow-up in many previous RCT on statins was often not long enough to observe the life-long effects of statin therapy [12,13,14]. Moreover, despite the numerous trials of statins, there are only few studies targeted patients with T2D [4, 15].
This study aimed to estimate the optimal statin therapy, especially the duration of statin therapy, among patients with type 2 diabetes in a real-world setting. We also aimed to compare the relative importance of the components of statin therapy, including statin intensity, achieved LDL-C level, and statin therapy duration, for cardiovascular risk reduction.
Methods
Data source and patient selection
We used the Korean National Health Insurance Service-Health Screening Cohort (NHIS-HEALS). This database contains longitudinal (2002–2015) information of 514,866 Koreans, including individuals’ demographic details, disease diagnoses according to the International Classification of Disease, Tenth Revision (ICD-10), prescription records, medical procedures, hospitalizations, death records, and health examination data, including laboratory data, anthropometric measures, and questionnaires for medical conditions. This cohort represented 10% of all health screening participants aged 40–79 years randomly selected in South Korea. The protocols have been described previously [16].
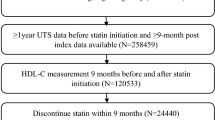
A flow diagram of the study subject selection process is shown in Additional file 1: Fig. S1. From the original cohort, we first selected adults (> 40 years) diagnosed with T2D who had received statins for at least 90 days between January 1, 2007 and December 31, 2013 since serum lipid profiles were available from 2007. Subjects without documented lipid profiles before statin therapy initiation were excluded. T2D was defined based on ICD-10 codes of T2D (E11-14), with the use of any glucose-lowering agent, including insulin. Subjects who had changed statin intensity during follow-up (n = 425) and those who were not covered by regular medical insurance (n = 113) were excluded. Finally, 11,219 patients were included in the study. Among them, 383 received low-intensity statins and 10,836 received moderate- or high-intensity statins. Statin intensity was classified according to the 2013 American Heart Association/American College of Cardiology guidelines on the management of blood cholesterol [17]. The following are classified as low-intensity statins: Simvastatin 10 mg, Pravastatin 10–20 mg, Lovastatin 20 mg, Fluvastatin 20–40 mg, and Pitavastatin 1 mg. These other statins have been classified as moderate- or high-intensity statins: Atorvastatin 10–80 mg, Rosuvastatin 5–40 mg, Simvastatin 20–40 mg, Pravastatin 40–80 mg, Lovastatin 40 mg, Fluvastatin XL 80 mg or 40 mg twice daily, and Pitavastatin 2–4 mg.
To assess the effects of statin intensity on cardiovascular risk reduction, propensity score matching (maximum 1:27) was performed for those who received low-intensity statins and those who received moderate- or high-intensity statins to balance covariates between groups. The propensity score model was derived from a multiple logistic regression that included age, sex, pre-existing cardiovascular disease (CVD), smoking status (never, former, or current), alcohol consumption (never, ≤ 2 times/week, or ≥ 3 times/week), physical activity (never, ≤ 2 times/week, or ≥ 3 times/week), socioeconomic status (low, middle, high), body mass index (BMI), fasting blood glucose level, systolic blood pressure (SBP), serum creatinine level, use of anti-thrombotic agents, use of anti-hypertensive agents according to class (renin–angiotensin–aldosterone system inhibitors, calcium channel blockers, beta blockers, alpha blockers, vasodilators, or diuretics), duration of diabetes, and baseline LDL-C levels (< 2.6, 2.6–3.3, ≥ 3.4 mmol/L).
All patients were followed-up from the first date of receiving statin therapy to the earliest occurrence of any cardiovascular outcomes described below, death, or the end of the cohort period (December 31, 2015). This study was approved by the Institutional Review Board of the Korea University Anam Hospital (IRB number ED17181). All data were anonymized; thus, the NHIS approved the study without requiring informed consent from each person.
Outcome measures
The primary outcome measure was the occurrence of major adverse cardiovascular events (MACE) including ischemic heart disease (IHD), ischemic stroke (IS), or cardiovascular death. IHD was defined as hospitalization for IHD (identified by ICD-10 codes I20-I25) plus coronary artery angiography or procedures. IS was defined as hospitalization for IS (identified by ICD-10 code I63) plus brain imaging studies or procedures for IS. Cardiovascular death was defined as death from CVD (ICD codes I00-I99).
Statistical analysis
Data are presented as mean and standard deviation (SD) for continuous variables and as number (n) and percentage (%) for categorical variables. A generalized estimating equation for matched data was used for the intergroup comparison (low-intensity group vs. moderate- or high-intensity group). For the primary outcome, we calculated incidence rates per 100 person-years and hazard ratios (HRs) with 95% confidence intervals (95% CIs) using Cox proportional hazard regression models. These analyses were performed according to statin intensity, achieved LDL-C concentration, and statin therapy duration. The achieved LDL-C concentration was defined as the minimum of LDL-C levels from 3 months after initiating statin therapy to the occurrence of outcomes or the end of follow-up. This was analyzed as a continuous variable, and the adjusted HR of MACE according to achieved LDL-C level was drawn using a cubic spline curve. Statin therapy duration was obtained by summing the length of a continuous statin prescription from the first day of study enrolment to the last day of follow-up. If the next prescription was filled within 30 days of the expected end date of the previous prescription, then therapy was considered uninterrupted. The duration of statin therapy was categorized into groups at intervals of 6 months: < 6, 6–12, 12–18, 18–24, 24–30, 30–36, and ≥ 36 months. The statin therapy duration was also analyzed as a continuous variable.
Furthermore, to compare the relative contributions of statin intensity, achieved LDL-C level, and statin therapy duration for predicting MACE, we calculated the proportion of log-likelihood explained by each factor. Log-likelihoods are useful for quantifying the predictive information contained in a variable compared with the information contained in the entire set of variables. The fraction of log-likelihood explained is analogous to R2 in an ordinary linear model. The partial effect of each risk factor was quantified by calculating the proportion of log-likelihood explained by each risk factor. A strong risk factor would contribute more, as compared with a weak risk factor, to the predictive ability of the model [18, 19]. The predictors included in the analyses were statin intensity, achieved LDL-C level, statin therapy duration, age, sex, socioeconomic status, duration of diabetes, BMI, fasting glucose, SBP, creatinine level, smoking, alcohol consumption status, exercise status, pre-existing CVD, and concurrent medication (anti-thrombotic agents, anti-hypertensive agents by class, and anti-diabetic agents by class). The statin therapy and diabetes duration were included as time-dependent variables.
All statistical analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at a two-sided p value < 0.05.
Results
The baseline characteristics of the low-intensity and moderate- or high-intensity statin therapy groups were well balanced (Table 1). The mean age of the study participants was 63 years. Of them, 59.4% were male and 15% had pre-existing CVD. The mean LDL-C concentration was 3.3 mmol/L; 45.7% of the subjects had LDL-C levels of 3.4 mmol/L or higher, 33.6% of 2.6–3.3 mmol/L, and 20.7% of less than 2.6 mmol/L.
Additional file 1: Table S1 shows the changes in the serum lipid profiles with statin therapy. The reduction of LDL-C levels (− 1.4 mmol/L vs − 1.1 mmol/L, p = 0.004) and non-HDL-C levels (− 1.6 mmol/L vs − 1.4 mmol/L, p = 0.001) was greater in the moderate- or high-intensity statin group than in the low-intensity statin group. The mean changes in HDL-C and TG levels were similar between groups.
Statin intensity and risk of major cardiovascular events
A total of 861 major cardiovascular events occurred during follow-up (median, 41.9 months; interquartile range, 30.1–55.1 months). The incidence rate per 100 person-years was 3.76 in the low-intensity statin group versus 2.69 in the moderate- or high-intensity statin group. The risk of MACE was significantly lower in the moderate- or high-intensity statin group than in the low-intensity statin group (HR, 0.72; 95% CI 0.54–0.96) (Table 2 and Additional file 1: Fig S2). The risks of IHD, IS, and cardiovascular death were also lower in the moderate- or high-intensity statin group than in the low-intensity statin group, although the difference was not statistically significant.
Achieved LDL-C Level and risk of major cardiovascular events
Given that the risk of MACE was determined by statin intensity, further analyses were performed with patients treated with moderate- or high-intensity statins (n = 8554). We evaluated the association between achieved LDL-C levels and the risk of MACEs. In the cubic spline curve analysis with achieved LDL-C as a continuous variable, patients with lower LDL-C levels had a lower cardiovascular risk (Fig. 1).
Cubic spline curve of adjusted hazard ratio for major cardiovascular events according to achieved LDL-C levels (mmol/L). Adjusted HR* (blue line) and 95% CI (shaded area) for major cardiovascular events according to on-treatment LDL-C levels with a reference of 2.6 mmol/L. The achieved LDL-C levels of the points at which 95% CI meets the reference line (HR = 1) are 1.9 mmol/L and 4.2 mmol/L. *Adjusted for age, sex, socioeconomic status, duration of diabetes, body mass index, fasting blood glucose, systolic blood pressure, creatinine, smoking, alcohol consumption, exercise, pre-existing cardiovascular disease (ischemic heart disease, ischemic stroke, and heart failure), and concurrent medications (anti-thrombotic agents, anti-hypertensive agents by class, and anti-diabetic agents by class)
Statin duration and risk of major cardiovascular events
We estimated the HRs of MACEs according to the statin therapy duration. First, the adjusted HRs of MACE were calculated by categorizing the duration of statin therapy. Compared to patients who received statin therapy for less than 6 months, the risk of MACE was gradually reduced with an increase in statin therapy duration. Adjusted HRs were 0.70 (95% CI 0.54–0.92), 0.71 (95% CI 0.53–0.96), 0.63 (95% CI 0.45–0.89), and 0.64 (95% CI 0.48–0.85) for patients who received statin therapy for 18–24, 24–30, 30–36, and ≥ 36 months, respectively (Fig. 2). The duration of statin use was also analyzed as a continuous variable. Figure 3 shows the cubic spline curve of the adjusted HR according to statin therapy duration. The longer the patients received statins, the lower was the risk of MACE.
Risk of major cardiovascular events according to statin therapy duration in patients who received moderate- or high-intensity statins. *Adjusted for age, sex, socioeconomic status, duration of diabetes, body mass index, fasting blood glucose, systolic blood pressure, creatinine, smoking, alcohol consumption, exercise, pre-existing cardiovascular disease (ischemic heart disease, ischemic stroke, and heart failure), concurrent medications (anti-thrombotic agents, anti-hypertensive agents by class, and anti-diabetic agents by class), and pre-treatment LDL-C level
Cubic spline curve of adjusted hazard ratio for major cardiovascular events according to statin therapy duration. Adjusted HR* (solid line) and 95% CI (shaded area) for major cardiovascular events according to statin therapy duration were calculated with a reference of 3 months. *Adjusted for age, sex, socioeconomic status, duration of diabetes, body mass index, fasting blood glucose, systolic blood pressure, creatinine, smoking, alcohol consumption, exercise, pre-existing cardiovascular disease (ischemic heart disease, ischemic stroke, and heart failure), and concurrent medications (anti-thrombotic agents, anti-hypertensive agents by class, and anti-diabetic agents by class), and pre-treatment LDL-C level
Relative importance of statin intensity, achieved LDL-C level, and statin therapy duration
Given that statin intensity, achieved LDL-C, and statin therapy duration were all determining factors for the risk of cardiovascular events, we compared the relative importance of these factors. The relative contributions were estimated by computing the proportion of explainable log-likelihood explained by each factor; the strongest predictor of the risk of MACE was statin therapy duration (2.55), followed by achieved LDL-C level (2.18) and statin intensity (0.95) (Fig. 4 and Additional file 1: Table S2).
Relative importance of statin therapy duration, statin intensity, and achieved LDL-C levels as predictors for MACE. The relative contributions of statin therapy duration, statin intensity, and achieved LDL-C levels were quantified by calculating the proportion of log-likelihood explained by each risk factor. Other variables in the model included age, sex, socioeconomic status, duration of diabetes, body mass index, fasting blood glucose, systolic blood pressure, creatinine, smoking, alcohol consumption, exercise, pre-existing cardiovascular disease (ischemic heart disease, ischemic stroke, and heart failure), and concurrent medication (anti-thrombotic agents, anti-hypertensive agents by class, and anti-diabetic agents by class). The statin therapy and diabetes durations were included as time-dependent variables
Discussion
In this study, we found that all three components of statin therapy—statin intensity, achieved LDL-C level, and statin therapy duration—significantly affected cardiovascular risks in T2D patients. Higher statin intensity, lower achieved LDL-C, and longer statin therapy duration reduced the risk of MACE. When all factors were included in a model for assessing cardiovascular risk, the statin therapy duration was even more important than statin intensity or achieved LDL-C level.
It is well established that apolipoprotein B (ApoB)-containing lipoproteins, including LDL, are implicated in the initiation and progression of atherosclerotic changes in the vasculature [20]. Statins exert their effects mainly by increasing LDL clearance from the blood by upregulating LDL receptors [21]. Numerous RCT and meta-analyses confirmed cardiovascular risk reduction with statins in multiple patient groups at different levels of cardiovascular risk [3,4,5, 22]. Based on previous RCT and meta-analyses, current guidelines for dyslipidemia management generally recommend the use of moderate- or high-intensity statins in high-risk patients, including those with T2D [6, 23]. However, controversy persists regarding whether a lower LDL-C level is better. In a population-based cohort study, achieving an LDL-C of 1.8 mmol/L or less with statin therapy did not have additional benefit over a level of 2.6 mmol/L or less in patients with IHD [8]. Although recent trials of proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors and ezetimibe strengthened the concept of “lower is better,” most of those trials included very high-risk groups [24,25,26]. Our study provides evidence that the “lower is better” concept would be applicable to T2D patients with diverse cardiovascular risk. There was no threshold for LDL-C concentrations for discriminating cardiovascular risk. Considering that only a small proportion of patients receiving statins achieved LDL-C targets and late initiation of high-intensity statin appears to be pivotal factors needing to be modified for improving CVD prevention [27] and that primary prevention statin therapy remains underutilized [28], clinicians should be more aggressive for lowering LDL-C levels even in patients without pre-existing CVD.
Besides the LDL-C lowering effects, statins have shown pleiotropic effects, such as inhibition of vascular inflammation, immune modulation, effects on endothelial progenitor stem cells, and effects on thrombogenicity [29]. Especially, higher intensity statin therapy has shown improvements in other pro-atherogenic factors and LDL-related parameters such as non-HDL-C and ApoB [30]. Our study also showed that moderate- or high-intensity statin reduced non-HDL-C more than low-intensity statin did. This could be contributed to greater cardiovascular risk reduction of higher intensity statins as well.
Despite a large number of patients discontinuing statin therapy in clinical practice [9, 31, 32], the effect of statin non-adherence on cardiovascular risk reduction has not been sufficiently studied. We revealed that the constant use of statins was an important factor in determining the cardioprotective effect of statin therapy. Specifically, at least 18 months of statin therapy was associated with a significantly lower risk of MACE compared to less than 6 months of statin therapy. Notably, the longevity of statin use was more important than other statin therapy factors for determining their cardioprotective effects. We suppose that the continued use of statins is critical in reducing exposure to ApoB-containing lipoproteins, which increases an individual’s total atherosclerotic plaque burden. This hypothesis was clearly proven in the spline curve analysis with statin therapy duration as a continuous variable. Recently, it has been reported that inpatient statin use and continuous use of statin was associated with lower in-hospital mortality compared to no statin use and discontinuation of statins in patients with coronavirus disease 2019 [33, 34]. Plausible explanations for these benefits of statins include anti-inflammatory and immunomodulating properties of statins, which may also be associated with lowering cardiovascular risk. Overall, the continuous use of statin should be emphasized in clinical practice.
This study has several limitations. First, due to the retrospective study design, the analyses established only associations between risk factors and outcomes but could not determine any causal relationship. Although we tried to adjust for confounding variables, there might be unmeasured confounders such as the individual’s health consciousness, eating habits and adherence to other medications. Second, we could not adjust for some important variables, including glycated hemoglobin, due to the lack of relevant data. Instead, the average fasting blood glucose was adjusted. Third, the number of patients in the low-intensity group was much smaller than that in the moderate- or high-intensity group. Lastly, LDL-C-lowering medications other than statins were not considered since ezetimibe was not used widely and PCSK9 inhibitors were not approved in South Korea during the study period. Further investigations are required to consider the effects of these agents.
Conclusions
In conclusion, this population-based study suggested that statin therapy duration or adherence should be considered an important factor for cardioprotective effects of statins in clinical practice. We propose the concept “longer is better” for statin therapy rather than “lower is better” for target LDL-C levels.
Availability of data and materials
Additional data are available through approval and oversight by the Korean National Health Insurance Service (available at https://nhiss.nhis.or.kr).
Abbreviations
- ApoB:
-
Apolipoprotein B
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- HDL-C:
-
High-density lipoprotein cholesterol
- HR:
-
Hazard ratio
- ICD-10:
-
International Classification of Disease, Tenth Revision
- IHD:
-
Ischemic heart disease
- IS:
-
Ischemic stroke
- LDL-C:
-
Low-density lipoprotein cholesterol
- MACE:
-
Major adverse cardiovascular event
- NHIS-HEALS:
-
National Health Insurance Service-Health Screening Cohort
- PCSK9:
-
Proprotein convertase subtilisin/kexin 9
- RCT:
-
Randomized controlled trial
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- T2D:
-
Type 2 diabetes
- TG:
-
Triglyceride
References
Grundy SM. Hypertriglyceridemia, atherogenic dyslipidemia, and the metabolic syndrome. Am J Cardiol. 1998;81:18B-25B.
Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5:150–9.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78.
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–96.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–90.
American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S111–34.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Leibowitz M, Karpati T, Cohen-Stavi CJ, Feldman BS, Hoshen M, Bitterman H, et al. Association between achieved low-density lipoprotein levels and major adverse cardiac events in patients with stable ischemic heart disease taking statin treatment. JAMA Intern Med. 2016;176:1105–13.
Lemstra M, Blackburn D, Crawley A, Fung R. Proportion and risk indicators of nonadherence to statin therapy: a meta-analysis. Can J Cardiol. 2012;28:574–80.
Goriacko P, Andersen M, Fazylov R, Plakogiannis R. What is the appropriate duration of high-dose atorvastatin therapy post-acute coronary syndrome? J Pharm Pract. 2015;28:555–60.
O’Brien KD, Hippe DS, Chen H, Neradilek MB, Probstfield JL, Peck S, et al. Longer duration of statin therapy is associated with decreased carotid plaque vascularity by magnetic resonance imaging. Atherosclerosis. 2016;245:74–81.
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–504.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–207.
Schwartz GG, Olsson AG, Ezekowitz MD, Ganz P, Oliver MF, Waters D, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001;285:1711–8.
Knopp RH, d’Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN). Diabetes Care. 2006;29:1478–85.
Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7:e016640.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129:S1-45.
Harrell F. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. 2nd ed. Cham: Springer; 2015.
Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson A-M, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–44.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38:2459–72.
Vaughan CJ, Gotto AM Jr, Basson CT. The evolving role of statins in the management of atherosclerosis. J Am Coll Cardiol. 2000;35:1–10.
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–58.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73:e285–350.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–97.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107.
Morieri ML, Perrone V, Veronesi C, Degli Esposti L, Andretta M, Plebani M, et al. Improving statin treatment strategies to reduce LDL-cholesterol: factors associated with targets’ attainment in subjects with and without type 2 diabetes. Cardiovasc Diabetol. 2021;20:144.
Metser G, Bradley C, Moise N, Liyanage-Don N, Kronish I, Ye S. Gaps and disparities in primary prevention statin prescription during outpatient care. Am J Cardiol. 2021;161:36–41.
Blum A, Shamburek R. The pleiotropic effects of statins on endothelial function, vascular inflammation, immunomodulation and thrombogenesis. Atherosclerosis. 2009;203:325–30.
Soran H, Liu Y, Adam S, Siahmansur T, Ho JH, Schofield JD, et al. A comparison of the effects of low- and high-dose atorvastatin on lipoprotein metabolism and inflammatory cytokines in type 2 diabetes: results from the Protection Against Nephropathy in Diabetes with Atorvastatin (PANDA) randomized trial. J Clin Lipidol. 2018;12:44–55.
Birtcher K. When compliance is an issue-how to enhance statin adherence and address adverse effects. Curr Atheroscler Rep. 2015;17:471.
Cohen JD, Brinton EA, Ito MK, Jacobson TA. Understanding Statin Use in America and Gaps in Patient Education (USAGE): an internet-based survey of 10,138 current and former statin users. J Clin Lipidol. 2012;6:208–15.
Lohia P, Kapur S, Benjaram S, Cantor Z, Mahabadi N, Mir T, et al. Statins and clinical outcomes in hospitalized COVID-19 patients with and without diabetes mellitus: a retrospective cohort study with propensity score matching. Cardiovasc Diabetol. 2021;20:140.
Kuno T, So M, Iwagami M, Takahashi M, Egorova NN. The association of statins use with survival of patients with COVID-19. J Cardiol. 2021;S0914–5087(21):00367–71.
Acknowledgements
We thank the participants of the Korean Health Insurance Cohort study as well as the National Health Insurance Service, which developed the NHIS-HEALS (2002–2015) database (NHIS-2017-2-592).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JYK, SGK, and NHK contributed to the study idea and design. JC analyzed the data. JYK and NHK wrote the manuscript. All authors contributed to manuscript review and revision. NHK is the guarantor of this work and, as such, had full access to all study data and takes responsibility for its integrity and analytical accuracy. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Korea University Anam Hospital (IRB number: ED17181). All data were anonymised; thus, the NHIS approved the study without requiring informed consent from each person.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Pre- and post-treatment lipid profiles with statin therapy. Table S2. Relative importance of predictors for MACE by estimating the log-likelihood explained by each predictor. Figure S1. Flow diagram of the study subject selection process. Figure S2. Cumulative incidence of major cardiovascular events by statin intensity.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, J.Y., Choi, J., Kim, S.G. et al. Relative contributions of statin intensity, achieved low-density lipoprotein cholesterol level, and statin therapy duration to cardiovascular risk reduction in patients with type 2 diabetes: population based cohort study. Cardiovasc Diabetol 21, 28 (2022). https://doi.org/10.1186/s12933-022-01466-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01466-z