Abstract
Background
Early glucose lowering intervention in subjects with type 2 diabetes mellitus was demonstrated to be beneficial in terms of micro- and macrovascular risk reduction. However, most of currently ongoing cardiovascular outcome trials are performed in subjects with manifest atherosclerosis and long-standing diabetes. Therefore, the aim of this study is to investigate the effects of the dipeptidylpeptidase-4 inhibitor linagliptin in subjects with coronary artery disease (CAD) but early type 2 diabetes mellitus (T2DM) on a set of cardiovascular surrogate measurements.
Methods
In this randomized, placebo-controlled, double-blind, single-center study, we included subjects with early diabetes (postchallenge diabetes (2 h glucose > 200 mg/dl) or T2DM treated with diet only or on a stable dose of metformin monotherapy and an HbA1c < 75 mmol/mol) and established CAD. Participants were randomized to receive either linagliptin (5 mg) once daily orally or placebo for 12 weeks. The primary outcome was the change in flow mediated dilatation (FMD). The secondary objective was to investigate the effect of linagliptin treatment on arginine bioavailability ratios [Global arginine bioavailability ratio (GABR) and arginine to ornithine ratio (AOR)]. Arginine, ornithine and citrulline were measured in serum samples with a conventional usual amino acid analysis technique, involving separation of amino acids by ion exchange chromatography followed by postcolumn continuous reaction with ninhydrin. GABR was calculated by l-arginine divided by the sum of (l-ornithine plus l-citrulline). The AOR was calculated by dividing l-arginine by l-ornithine levels. Group comparisons were calculated by using a two-sample t-test with Satterthwaite adjustment for unequal variances.
Results
We investigated 43 patients (21% female) with a mean age of 63.3 ± 8.2 years. FMD at baseline was 3.5 ± 3.1% in the linagliptin group vs. 4.0 ± 2.9% in the placebo group. The change in mean FMD in the linagliptin group was not significantly different compared to the change in the placebo group (0.43 ± 4.84% vs. − 0.45 ± 3.01%; p = 0.486). No significant improvements were seen in the arginine bioavailability ratios (GABR; p = 0.608 and AOR; p = 0.549).
Conclusion
Linagliptin treatment in subjects with CAD and early T2DM did not improve endothelial function or the arginine bioavailability ratios.
Trial registration ClinicalTrials.gov, NCT02350478 (https://clinicaltrials.gov/ct2/show/NCT02350478)
Similar content being viewed by others
Background
Patients with type 2 diabetes (T2DM) are at increased risk of macrovascular events as well as microvascular complications [1]. Endothelial dysfunction represents an early step in the process of atherosclerosis and moreover serves as a surrogate for future cardiovascular events. We and others have shown previously, that endothelial dysfunction is present in patients with coronary artery disease and early diabetes and can be improved by pharmacological intervention [2].
Dipeptidylpeptidase-4 (DPP-4) inhibitors increase endogenous glucagon like-peptide-1 (GLP-1) levels leading to an insulin release from pancreatic beta-cells and suppression of glucagon secretion from alpha cells in a glucose dependent manner [3]. Hence, this drug class was demonstrated to lower both, fasting and post-challenge or postmeal glucose levels and consequently glycosylated haemoglobin (HbA1c) and is well tolerated.
Three cardiovascular outcome trials with the DPP-4 inhibitors alogliptin, saxagliptin and sitagliptin were published and demonstrated cardiovascular safety of those molecules as compared to usual diabetes care without DPP-4 inhibitors [4,5,6]. Two outcome trials with linagliptin (CAROLINA [7] and CARMELINA—NCT01897532) are ongoing. All published studies included subjects with longstanding diabetes (median duration between 7.1 and 11.6 years) and it has been argued that results might be different in subjects with shorter diabetes duration.
A well-known and validated cardiovascular surrogate parameter for future cardiovascular events is the dysfunction of endothelium, characterized by impairment of relaxation of the arteries in response to increased shear stress [8]. Mechanistic animal and in vitro data demonstrated, that DPP-4 inhibitions leads to improved vascular stiffening, endothelial function, vascular remodelling, suggesting potential cardiac, renal and neurologic benefits of this drug class [9, 10]. Reduction in oxidative stress, inflammatory responses or apoptosis and beneficial effects on the AGE/RAGE axis were proposed as possible molecular mechanisms leading to the vascular and renal effects observed [11].
Data on the effect of DPP-4 inhibitors on endothelial function are conflicting. While Nakamura et al. [12] demonstrated an improvement of endothelial function with Sitagliptin, Ayaori and contributors [13] showed a worsening of endothelial function using the same drug. However, Jax et al. demonstrated a neutral effect on macrovascular function [14]. However, not all these trials were performed in a placebo-controlled fashion.
Therefore, we performed a randomized, placebo-controlled, double-blind trial investigating the effect of the DPP-4 inhibitor linagliptin on endothelial function and further biochemical markers of vascular function and effects on postprandial lipids of the DPP-4 inhibitor linagliptin in early stages of T2DM.
Methods
We conducted a prospective, single-center, double-blind, randomized placebo-controlled trial at the Medical University of Graz, Austria (ClinicalTrials.gov, NCT02350478). The study was approved by the local Ethics Committee of the Medical University of Graz (25–295 ex 12/13) and was performed in accordance with the principles of the Declaration of Helsinki, good clinical practice guidelines, and the standard operating procedures of the sponsor. Written informed consent was obtained from all participants prior to enrolment.
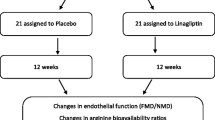
Detailed information regarding the design and methods of this study were described previously [15]. Briefly, patients with early T2DM and manifest coronary atherosclerosis (diagnosed either by coronary angiography or coronary computer tomography), aged between 40 and 80 years, with either a 2 h-glucose value above 200 mg/dl after 75 g glucose load or a glycated haemoglobin (HbA1c) level between 42 and 75 mmol/mol while on diet only or metformin monotherapy, were included in the trial. Participants were randomized to receive either linagliptin [linagliptin group (LG)] or matched placebo drug [placebo group (PG)] administered orally for a duration of 12 weeks. Randomization was performed by using the web-based randomization tool “Randomizer for Clinical Trials: http://www.randomizer.at/” (Accessed 29 Jan 2018) provided by the Institute of Medical Informatics, Statistics and Documentation, Medical University of Graz. Patients were randomly assigned to one of the two arms (LG or PG, ratio 1:1). Permuted block randomization with block size 10 was used.
Mobilization of hematopoietic stem/progenitor cells (HSPC) endothelial progenitor cells (EPC) and mesenchymal stromal cells (MSC) was analysed by multi-parameter flow cytometry as described previously using heparinised peripheral blood samples [16]. Briefly, at least one million mononuclear cells per sample were analysed to determine mature cell lineage marker-negative (LinNEG) CD34+/CD45+/CD90+/CD271− HSPC, CD34+/CD45−/CD90−/CD271− EPC and CD34−/CD45−/CD90+/CD271+ MSC based on previously published procedures [17, 18]. HSPC subpopulations were measured as LinNEG/CD34+/CD38−/CD45RA+ lymphoid multipotent progenitors (LMPP), LinNEG/CD34+/CD38+/CD10−/CD123−/CD45RA− megakaryocyte-erythroid progenitors (MEP), LinNEG/CD34+/CD38+/CD10+/CD45RA+ common lymphoid progenitors (CLP) and LinNEG/CD34+/CD38−/CD45RA− multipotent progenitors (MPP) [19].
Statistical analysis
For sample size calculation a relative improvement of the FMD of 30% in the linagliptin group and no changes from baseline to week 12 in the placebo group were assumed. For a total sample size of 42 subjects and based on an absolute difference between the two groups in the FMD change from baseline to week 12 of 1.5% with a SD of 1.5%, a power of approximately 90% could be achieved (two-sided test with alpha 5%). All statistical analyses were performed with SAS® software version 9.4 (SAS Institute, Cary, NC, USA). Data are expressed as mean (± standard deviation), unless otherwise specified.
Net incremental area (net area above baseline) was calculated for c-peptide, glucose and insulin, and net decremental area (net area below baseline) for the free fatty acids based on the trapezoidal rule with baseline value as mean of the values at time points − 5 and 0 min. For the primary and secondary endpoints, group differences were analysed using analysis of covariance with the follow-up value at week 12 as dependent variable, and the baseline value and treatment group as covariates. If the assumptions of the ANCOVA were not fulfilled, parameter changes between the groups were compared by t-test or Mann–Whitney-U-test. Laboratory parameters having a skewed distribution were log-transformed. As post hoc sensitivity analysis, multiple linear regression analysis for change in FMD including age, gender, eGFR, NT-proBNP, LDL-cholesterol and systolic blood pressure at baseline was conducted. All analyses were performed on intention-to-treat (ITT) basis. Statistical significance was defined as p < 0.05.
Results
Study population
In total 49 randomizations were performed. After randomization, two subjects were excluded due to screening failures without receiving the study medication. Therefore 47 subjects were enrolled in the study and received the study medication. Of those, 3 subjects were lost to follow up without available follow-up data and 1 subject was excluded due to a major protocol violation prior to unblinding (Fig. 1).
In the final analysis we included 43 patients (9 females/34 males) with a mean age of 63.3 ± 8.2 years and a mean diabetes duration of 4.3 ± 5.5 years. Mean HbA1c at baseline was 52.3 ± 8.2 mmol/mol in the LG and 51.0 ± 8.3 mmol/mol in the PG, respectively. Overall, 16 (8 in the LG vs. 8 in the PG) subjects were treated with diet only, while 27 (12 in the LG vs. 15 in the PG) participants were on metformin monotherapy. No differences with respect to any of the baseline parameters were seen between PG and LG at the time of enrolment (Table 1).
Endothelial function
At baseline FMD measurement was 3.5 ± 3.1% in the LG and 4.0 ± 2.9% in the PG, respectively (Table 2). The increase in mean FMD in the LG (0.4 ± 4.8%) was not significantly different compared to the change in the PG (− 0.5 ± 3.0%; p = 0.486). The sensitivity analysis for change in FMD including age, gender, eGFR, NT-proBNP, LDL-cholesterol and systolic blood pressure at baseline did not change the results (data not shown). No significant improvements were observed in the change of other endothelial function parameters such as Global Arginine Bioavailability Ratio (GABR) (change − 0.11 ± 0.35 in the LG vs. − 0.06 ± 0.39 in the PG; p = 0.608), the change of the arginine-to-ornithine-ratio (AOR) (− 0.13 ± 0.45 in the LG vs. − 0.05 ± 0.53 in the PG; p = 0.549), change in asymmetric dimethylarginine (ADMA) (0.15 ± 0.22 µmol/L in the LG vs. 0.10 ± 0.14 µmol/L in the PG; p = 0.28), change of serum soluble intercellular adhesion molecule-1 ([sICAM-1]-15 (− 272 to 103) vs. − 21 (− 134 to 310) ng/ml; p = 0.903) or change of serum soluble vascular cell adhesion molecule-1 ([sVCAM-1]-34 ± 84 vs. 5 ± 130 ng/ml; p = 0.431), respectively.
Glucose and lipid metabolism
HbA1c was significantly reduced with linagliptin treatment − 2 (− 8 to 27) mmol/mol in the LG vs. 0.5 (− 28 to 18) mmol/mol in the PG; p = 0.029). Compared with the placebo group, subjects receiving linagliptin showed a numerical, but not statistically significant reduction of the area under curve (AUC) for glucose (Table 2). AUC for insulin, C-peptide and free fatty acids were comparable between both treatment groups (Table 2).
Ancillary study for hematopoietic stem cells
In a subset of randomly selected 8 subjects (5 in the linagliptin and 3 in the placebo group) endothelial progenitor cells (EPC) and mesenchymal stromal cells (MSC) were investigated. Neither increased nor reduced mobilization of EPCs and MSC were observed in this small subgroup (see Additional file 1: Table S1).
Serious adverse events occurred in 3 subjects in the LG vs. in 1 subject in the PG (p = 0.323), none of the events were related to the study medication.
Discussion
We investigated the impact of the DPP-4 inhibitor linagliptin on markers of endothelial function and postprandial lipid excursions in subjects with established coronary artery disease and early diabetes treated either with diet alone or metformin monotherapy. We observed, that linagliptin neither improves flow mediated dilation or other biochemical markers of endothelial function nor postprandial lipid levels.
Animal studies suggested beneficial effects of DPP-4 inhibitors on atherosclerosis [20]. Although first human studies suggested a beneficial effect on endothelial function [12] there were others showing even a worsening of endothelial function [13], while others turned out to be neutral [14, 21].
In a recent trial, Ott et al. investigated the impact of linagliptin on renal endothelial dysfunction and their data of a 4 week trial suggest the prevention of hyperglycaemia induced impaired renal endothelial function by linagliptin [22]. In contrast to our study, they focused on renal endothelial function, while we used flow mediated vasodilation as an assessment of vascular function and the major difference is, that our cohort had established coronary atherosclerosis as an inclusion criterion. Effects of linagliptin on endothelial function in subjects without manifest atherosclerosis might be different than the neutral effects observed in our cohort.
Shigiyama and colleagues investigated changes in endothelial function by linagliptin treatment compared to placebo and metformin treatment in subjects with type 2 diabetes and without macrovascular disease. While there was a significant improvement within the linagliptin group from baseline to study end, they were not able to demonstrate a significant improvement in the change of endothelial function compared to the other two groups [23]. The recent EFFORT trial is very similar to our trial in design, investigating subjects with early type 2 diabetes and coronary artery disease. They demonstrate an improvement in endothelial function measured by reactive hyperaemia-peripheral arterial tonometry by a 3 months linagliptin treatment compared to a voglibose group [24]. The major limitation of this small trial (in total 16 subjects) is the open label design without providing details on a prespecified sample size calculation in the publication.
The neutral effect shown by our study fits well into the framework of the neutral cardiovascular outcome trials seen with compounds of this group [4,5,6]. It is also in line with the neutral results of the recently published MARLINA-T2D trial, which did not confirm previous suggestions of an improvement in acute glomerular damage measured by the urinary albumin-creatinine ratio in subjects with type 2 diabetes [25]. The novelty of our study is that compared to in particular cardiovascular outcome trials, where usually subjects with longer diabetes duration are included, we performed our study solely in subjects with earlier stages of very well controlled diabetes and established coronary artery disease, given that previous analyses were suggesting that with increasing diabetes duration interventions are less likely to have an impact on endothelial function [26]. However, our data suggest, that also in this patient group linagliptin has a neutral effect on endothelial function. Future analyses using novel-omics techniques such as metabolomics might help in finding biomarker patterns to select patient subgroups still benefiting of a particular treatment despite neutral outcome in the overall population [27].
Data from a small ancillary study performed within the main trial did not show any changes in stem cell counts by linagliptin supporting a safe drug profile.
One limitation of our study is that we compared linagliptin against placebo and not an active control drug. However, given that the mean HbA1c at baseline was below 53 mmol/mol, the impact of linagliptin on glucose lowering was statistically significant, but very limited in the extent, as one would expect. Therefore, the glucose lowering effect observed in the linagliptin group is very unlikely to have an influence on endothelial function. Another limitation is the trial duration of 3 months. One could argue that a longer treatment period might be necessary to demonstrate a benefit on endothelial function in a cohort already having coronary atherosclerosis. However, our neutral results fit well in the overall neutral cardiovascular effects observed for DPP-4 inhibitors in recent cardiovascular outcome trials [4,5,6]. Further, the overall number of subjects included, being 43, could be considered small, however, the trial was powered to demonstrate a potential relative 30% improvement in FMD, which is deemed a clinically meaningful improvement.
Conclusion
Our study in subjects with early diabetes and established coronary artery disease demonstrates a neutral effect of linagliptin on various measurements of endothelial function. Whether this finding is also true for subjects with newly diagnosed diabetes without established cardiovascular disease, needs further investigation.
Abbreviations
- AOR:
-
arginine-to-ornithine-ratio
- AUC:
-
area under curve
- CAD:
-
coronary artery disease
- DPP-4:
-
dipeptidylpeptidase-4
- EPC:
-
endothelial progenitor cells
- FMD:
-
flow mediated dilatation
- GABR:
-
global arginine bioavailability ratio
- GLP-1:
-
glucagon like-peptide-1
- HbA1c:
-
glycated haemoglobin
- ITT:
-
intention-to-treat
- LG:
-
linagliptin
- MSC:
-
mesenchymal stromal cells
- MTT:
-
meal tolerance test
- PG:
-
placebo group
- sVCAM-1:
-
soluble vascular cell adhesion molecule-1
- sICAM-1:
-
soluble intercellular adhesion molecule-1
- T2DM:
-
type 2 diabetes mellitus
References
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12.
Sourij H, Zweiker R, Wascher TC. Effects of pioglitazone on endothelial function, insulin sensitivity, and glucose control in subjects with coronary artery disease and new-onset type 2 diabetes. Diab Care. 2006;29(5):1039–45.
Nauck M. Incretin therapies: highlighting common features and differences in the modes of action of glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Diab Obes Metab. 2016;18(3):203–16.
White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369(14):1327–35.
Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–26.
Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, Josse R, Kaufman KD, Koglin J, Korn S, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–42.
Marx N, Rosenstock J, Kahn SE, Zinman B, Kastelein JJ, Lachin JM, Espeland MA, Bluhmki E, Mattheus M, Ryckaert B, et al. Design and baseline characteristics of the CARdiovascular Outcome Trial of LINAgliptin vs. glimepiride in type 2 diabetes [CAROLINA(R)]. Diab Vasc Dis Res. 2015;12(3):164–74.
Moens AL, Goovaerts I, Claeys MJ, Vrints CJ. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest. 2005;127(6):2254–63.
Manrique C, Habibi J, Aroor AR, Sowers JR, Jia G, Hayden MR, Garro M, Martinez-Lemus LA, Ramirez-Perez FI, Klein T, et al. Dipeptidyl peptidase-4 inhibition with linagliptin prevents western diet-induced vascular abnormalities in female mice. Cardiovasc Diabetol. 2016;15:94.
Aroor AR, Manrique-Acevedo C, DeMarco VG. The role of dipeptidylpeptidase-4 inhibitors in management of cardiovascular disease in diabetes; focus on linagliptin. Cardiovasc Diabetol. 2018;17(1):59.
Hasan AA, Hocher B. Role of soluble and membrane-bound dipeptidyl peptidase-4 in diabetic nephropathy. J Mol Endocrinol. 2017;59(1):R1–10.
Nakamura K, Oe H, Kihara H, Shimada K, Fukuda S, Watanabe K, Takagi T, Yunoki K, Miyoshi T, Hirata K, et al. DPP-4 inhibitor and alpha-glucosidase inhibitor equally improve endothelial function in patients with type 2 diabetes: EDGE study. Cardiovasc Diabetol. 2014;13:110.
Ayaori M, Iwakami N, Uto-Kondo H, Sato H, Sasaki M, Komatsu T, Iizuka M, Takiguchi S, Yakushiji E, Nakaya K, et al. Dipeptidyl peptidase-4 inhibitors attenuate endothelial function as evaluated by flow-mediated vasodilatation in type 2 diabetic patients. J Am Heart Assoc. 2013;2(1):e003277.
Jax T, Stirban A, Terjung A, Esmaeili H, Berk A, Thiemann S, Chilton R, von Eynatten M, Marx N. A randomised, active- and placebo-controlled, three-period crossover trial to investigate short-term effects of the dipeptidyl peptidase-4 inhibitor linagliptin on macro- and microvascular endothelial function in type 2 diabetes. Cardiovasc Diabetol. 2017;16(1):13.
Tripolt NJ, Aberer F, Riedl R, Hutz B, Url J, Dimsity G, Meinitzer A, Stojakovic T, Hodl R, Brodmann M, et al. The effects of linagliptin on endothelial function and global arginine bioavailability ratio in coronary artery disease patients with early diabetes: study protocol for a randomized controlled trial. Trials. 2016;17(1):495.
Strunk D, Rohde E, Lanzer G, Linkesch W. Phenotypic characterization and preclinical production of human lineage-negative cells for regenerative stem cell therapy. Transfusion. 2005;45(3):315–26.
Reinisch A, Etchart N, Thomas D, Hofmann NA, Fruehwirth M, Sinha S, Chan CK, Senarath-Yapa K, Seo EY, Wearda T, et al. Epigenetic and in vivo comparison of diverse MSC sources reveals an endochondral signature for human hematopoietic niche formation. Blood. 2015;125(2):249–60.
Strunk D. Endothelial progenitor cells: quod erat demonstrandum? Curr Pharm Des. 2011;17(30):3245–51.
Seita J, Weissman IL. Hematopoietic stem cell: self-renewal vs. differentiation. Wiley Interdiscip Rev Syst Biol Med. 2010;2(6):640–53.
Salim HM, Fukuda D, Higashikuni Y, Tanaka K, Hirata Y, Yagi S, Soeki T, Shimabukuro M, Sata M. Dipeptidyl peptidase-4 inhibitor, linagliptin, ameliorates endothelial dysfunction and atherogenesis in normoglycemic apolipoprotein-E deficient mice. Vascul Pharmacol. 2016;79:16–23.
Maruhashi T, Higashi Y, Kihara Y, Yamada H, Sata M, Ueda S, Odawara M, Terauchi Y, Dai K, Ohno J, et al. Long-term effect of sitagliptin on endothelial function in type 2 diabetes: a sub-analysis of the PROLOGUE study. Cardiovasc Diabetol. 2016;15(1):134.
Ott C, Kistner I, Keller M, Friedrich S, Willam C, Bramlage P, Schmieder RE. Effects of linagliptin on renal endothelial function in patients with type 2 diabetes: a randomised clinical trial. Diabetologia. 2016;59(12):2579–87.
Shigiyama F, Kumashiro N, Miyagi M, Iga R, Kobayashi Y, Kanda E, Uchino H, Hirose T. Linagliptin improves endothelial function in patients with type 2 diabetes: a randomized study of linagliptin effectiveness on endothelial function. J Diab Investig. 2017;8(3):330–40.
Koyama T, Tanaka A, Yoshida H, Oyama JI, Toyoda S, Sakuma M, Inoue T, Otsuka Y, Node K. Comparison of the effects of linagliptin and voglibose on endothelial function in patients with type 2 diabetes and coronary artery disease: a prospective, randomized, pilot study (EFFORT). Heart Vessels. 2018. https://doi.org/10.1007/s00380-018-1136-2.
Groop PH, Cooper ME, Perkovic V, Hocher B, Kanasaki K, Haneda M, Schernthaner G, Sharma K, Stanton RC, Toto R, et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial. Diab Obes Metab. 2017;19(11):1610–9.
Tripolt NJ, Meinitzer A, Eder M, Wascher TC, Pieber TR, Sourij H. Multifactorial risk factor intervention in patients with type 2 diabetes improves arginine bioavailability ratios. Diab Med. 2012;29(10):e365–8.
Hocher B, Adamski J. Metabolomics for clinical use and research in chronic kidney disease. Nat Rev Nephrol. 2017;13(5):269–84.
Authors’ contributions
HS and NJT conceived and designed the study, planned the analysis and implemented the study. JU and GD organized and performed the study visits. DS designed the study protocol of the ancillary hematopoietic stem cells study. GB performed the flow cytometry analysis and helped with data analyses. NJT, FA and HS wrote the first draft of the manuscript. HS, FH, MB, NJT designed the study protocol; NJT and HS wrote the clinical protocol and obtained authorization from the Ethics Committee and wrote the manuscript. RH supported the recruitment of study participants. HS calculated the sample size for this trial and RR planned and performed the statistical analyses. FAz performed statistical analyses in relation to the hematopoietic stem cells. TS and AM were responsible for the laboratory analyses. HS is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Acknowledgements
This study is funded as an investigator initiated study by Boehringer Ingelheim RCV, Vienna, Austria. We thank Nutricia Austria for the provision of the Fortimel compact drinks used in the Mixed Meal Tolerance Test, Dr. Ulrike Leb-Stöger for her editing support and Dr. Leonhard Harpf for his recruitment support.
The flow cytometry analyses were funded by the Anniversary Fund of the Oesterreichische Nationalbank (OeNB, Grant 15941, DS). We thank Anna Hochreiter for performing flow cytometry. Finally, we thank Prof. Willibald Wonisch for performing the supplementary analysis of ADMA.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This protocol study was approved by the Ethics Committee of the Medical University of Graz and all patients gave their written informed consent to participate in the study, as well as for sampling and banking of the biological material. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and written informed consent was obtained from all patients.
Funding
This work was supported by Boehringer Ingelheim.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Change in cell counts from baseline in linagliptin vs. Placebo groups. FMD: flow mediated dilatation; MTT: meal tolerance test; sVCAM-1: soluble vascular cell adhesion molecule-1; sICAM-1: soluble intercellular adhesion molecule-1.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tripolt, N.J., Aberer, F., Riedl, R. et al. Effects of linagliptin on endothelial function and postprandial lipids in coronary artery disease patients with early diabetes: a randomized, placebo-controlled, double-blind trial. Cardiovasc Diabetol 17, 71 (2018). https://doi.org/10.1186/s12933-018-0716-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-018-0716-x