Abstract
Diabetic kidney disease (DKD) is the most common cause of end stage renal disease. The comprehensive management of DKD depends on combined target-therapies for hyperglycemia, hypertension, albuminuria, and hyperlipaemia, etc. Sodium–glucose co-transporter 2 (SGLT2) inhibitors, the most recently developed oral hypoglycemic agents acted on renal proximal tubules, suppress glucose reabsorption and increase urinary glucose excretion. Besides improvements in glycemic control, they presented excellent performances in direct renoprotective effects and the cardiovascular (CV) safety by decreasing albuminuria and the independent CV risk factors such as body weight and blood pressure, etc. Simultaneous use of SGLT-2 inhibitors and renin–angiotensin–aldosterone system (RAAS) blockers are novel strategies to slow the progression of DKD via reducing inflammatory and fibrotic markers induced by hyperglycaemia more than either drug alone. The available population and animal based studies have described SGLT2 inhibitors plus RAAS blockers. The present review was to systematically review the potential renal benefits of SGLT2 inhibitors combined with dipeptidyl peptidase-4 inhibitors, glucagon-like peptide-1 receptor agonists, mineralocorticoid receptor antagonists, and especially the angiotensin-converting enzyme inhibitors/angiotensin receptor blockers.
Similar content being viewed by others
Background
There are more than 350 million people suffering from type 2 diabetes mellitus (T2DM) worldwide, and its prevalence is increasing [1]. One of the most common complications in T2DM is diabetic kidney disease (DKD), which is characterized by prior diabetes mellitus, kidney damage, decreased glomerular filtration rate (GFR), and persistent albuminuria. Etiologies of DKD include environmental insults, genetic susceptibility, primarily metabolic and hemodynamic factors, etc. [2]. Thus the treatment for DKD is mainly aimed at controlling metabolic and hemodynamic abnormalities. The agents for treatment including the use of traditional anti-hyperglycemic agents (AHAs) such as metformin, insulin or pioglitazone, and renin–angiotensin–aldosterone system (RRAS) inhibitors like angiotensin-converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARBs).
Despite a large armamentarium already being available for the management of hyperglycemia in T2DM, current oral AHAs often do not provide adequately effective or continuing glycemic control with improved β-cell function. Although metformin provides modest weight loss, most AHAs may result in weight gain or may not substantively decrease body weight [1, 3]. And renal insufficiency is definitely correlated with body fat in patients with coronary artery disease [4]. Therefore, it is necessary to call for newer AHAs that can provide long-term glycemic control and additional benefits like weight loss and the renoprotection, etc.
Sodium–glucose co-transporter 2 (SGLT2) inhibitors are new AHAs with an original insulin-independent mode of action and well tolerance, as well as favorable safety profile in patients with DKD [5, 6]. The present review provided an overview of studies with SGLT2 inhibitors, and discussed the synergistic mechanisms of SGLT2 inhibitors combined with ACEI/ARBs, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 receptor agonists (GLP1-RAs) and mineralocorticoid receptor antagonists (MRAs) in the treatment for DKD.
The role of SGLT2 in glucose metabolism
The kidneys play a critical role in the management of glucose reabsorption and maintaining the overall metabolic balance in humans [7]. The SGLT2, a low-affinity, high-capacity glucose transporter, is located primarily in the brush border membrane of the S1 segment of the proximal renal tubule and is responsible for approximated 90% of the plasma glucose reabsorption in the kidney [8]. The action site of SGLT2 in normal situation showed in Fig. 1.
Expression and activity of the SGLT2 transporter genes are up-regulated and the renal threshold is increased in patients with T2DM. These lead to increased glucose reabsorption from glomerular filtrate and reduced urinary glucose excretion (UGE), and further worsen the hyperglycemic condition [7, 9]. SGLT2 inhibitors are specifically aimed to block the reabsorption of filtered glucose in the proximal renal tubule, and resulting in increased UGE and decreased glycated haemoglobin (HbA1c) and fasting plasma glucose (FPG), especially when hyperglycaemia is present, in the meantime, they are protecting kidney [10, 11].
However, SGLT2 inhibitors could lead to a substantial increase in endogenous (hepatic) glucose production (EGP, HGP) and was accompanied by an increase in FPG concentration [12]. An acute decline in blood glucose concentration could stimulate the release of glucagon and other counter-regulatory hormones [13]. Moreover, because of the removal of the inhibitory effect of hyperglycemia on HGP, a decrease in FPG concentration potentially could result in an increase in HGP [14, 15]. Glucagon was a powerful stimulator of HGP [14,15,16], so the increasing glucagon observed with SGLT2 inhibitors probably provided an obvious explanation for the increase in EGP.
The pharmacological roles of SGLT2 inhibitors in experimental models
Blocking the activity of SGLT2 leads to amelioration of renin–angiotensin system (RAS) component activation, renal inflammation and decreased expressions of antioxidant enzymes in Otsuka Long-Evans Tokushima Fatty (OLETF) rats [17]. Hence, they are slowing the progression of DKD. Furthermore, enhanced reabsorption reduces the Na–Cl–K concentration at the macula densa and increases GFR through the physiology of tubuloglomerular feedback and a possible reduction in the hydrostatic pressure in Bowman space [18]. SGLT2 inhibitors reduce hyperfiltration through the above mentioned mechanism, and attenuate/prevent the molecular markers of kidney growth, fibrotic responses of proximal tubular cells and glomerular size, as well as gluconeogenesis in diabetic Akita rats [19, 20].
For example, empagliflozin reduced the expression of nuclear deoxyribonucleic acid binding for nuclear factor kappa B (NF-κB), activator protein 1, Toll-like receptor-4 and attenuated collagen IV expression as well as interleukin-6 secretion [21]. Dapagliflozin reduced renal expression of Bax, renal tubule injury and TUNEL-positive cells and increased renal expression of hypoxia-inducible factor 1 to protect kidney [22].
SGLT2 inhibitors in clinical trials
Currently, SGLT2 inhibitors like canagliflozin, dapagliflozin and empagliflozin have now been approved for clinical use in patients with T2DM in the United States, Europe and other countries [23]. As new AHAs, SGLT2 inhibitors have renoprotection including the following two aspects.
On one hand, SGLT2 inhibitors exert indirect renoprotection through suppressing renal glucose reabsorption to reduce blood glucose and body weight. One the other hand, SGLT2 inhibitors specifically alter renal hemodynamics and then reduce intraglomerular pressure [21, 24,25,26], and attenuate diabetes-associated hyperfiltration and tubular hypertrophy, as well as reduce the tubular toxicity of glucose to directly protect kidney [27]. Moreover, SGLT2 inhibitors reduce albuminuria, serum uric acid without potassium abnormalities [28], as well as BP especially systolic blood pressure (SBP) by mild natriuresis, afferent arteriole vasoconstriction, osmotic diuresis and weight loss [29]. The last but not least, diuresis can induce the increasing of hematocrit and erythropoietin. SGLT2 inhibitors reduce the workload of the proximal tubules to improve tubulointerstitial hypoxia, and then allow fibroblasts to resume normal erythropoietin production, and thereby protect the kidney [30]. Above all, SGLT2 inhibitors can be expected to translate into improved long-term kidney outcomes in patients with DKD.
A study of stage 3 DKD patients showed that canagliflozin 100 and 300 mg were associated with greater decreases in urine albumin–creatinine ratio (UACR) compared with placebo [31]. In addition, Yale et al. [31] found that the increased blood urea nitrogen (BUN) with canagliflozin occurred early and then had tendency towards baseline over the remaining treatment period. Two studies performed in T2DM patients with moderate renal impairment demonstrated that treatment with SGLT2 inhibitors led to an initial fall in estimated glomerular filtration rate (eGFR) with a trend toward an increase over time [28, 31].
Actually, sodium delivery to the macula densa could be increased by SGLT2 inhibitors, the increased sodium delivery is sensed as an increase in circulating volume at the level of the juxtaglomerular apparatus, resulting in a constriction of afferent renal arterioles, a decrease in intraglomerular pressure and a reversible decrease in single nephron GFR [18, 32]. These above mentioned investigations suggested that initial changes in renal function were associated with haemodynamic responses to SGLT2 inhibitors treatment.
The markers such as body weight (including abdominal adiposity), BP, reduced eGFR, poor control of diabetes and serum uric acid are considered as independent CV risk factors, effective management of CV risk factors and careful monitoring of eGFR may represent opportunities to reduce the risks of CV events [33]. Moreover, the reduction in CV mortality is primarily through enhancing diuresis and reducing BP [34]. SGLT2 inhibitors can efficiently normalize the above mentioned factors. The EMPA-REG OUTCOME trial and the LEADER trial have shown superiority of the SGLT2 inhibitors on the 3-point major adverse cardiovascular events (MACE) outcome and CV, as well as all-cause mortality [35].
In another several EMPA-REG OUTCOME trials, patients with T2DM at high risk for CV events who used SGLT2 inhibitors against placebo had a lower rate of the primary composite CV outcome, reduced heart failure (HF) hospitalization and CV death. Moreover, they were associated with lower rates of clinical renal events and slower progression of kidney disease. There exist consistent benefits in patients with and without baseline HF when the study drugs were added to standard care [36,37,38,39]. Although potentially atherogenic low density lipoprotein-cholesterol (LDL-C) concentrations increased by approximately 5%, this might be counterbalanced by corresponding increases in high density lipoprotein-cholesterol (HDL-C) and more significant decreases in triglyceride levels [40].
Pharmacological synergistic effects of SGLT2 inhibitors in DKD therapy
Monotherapy with metformin, insulin or pioglitazone alone is poorly effective in maintaining long-term glycemic control and renoprotection in a majority of patients with DKD [41]. Various pharmacological approaches may be added to them as dual therapies or combined together as triple therapies. The concept of combining SGLT2 inhibitors with ACEI/ARBs, DPP-4 inhibitors and GLP1-RAs has got much attention [42]. Because the mechanisms of they complement SGLT2 inhibitors may include two aspects. On one hand, they are counteracting the SGLT2 inhibitors associated rise in EGP and glucagon, on the other hand, they are potentially applying an additive or synergistic effect on RAAS blocked and glucose-lowering to delay the progression of DKD [17].
SGLT2 inhibitors combined with ACEI/ARBs therapy
In view of T2DM and RAS activation, it results in renal and systemic vascular dysfunction that promotes end-organ injury and significant morbidity. Guidelines recommend that inhibition of the RAS with ACEI/ARBs constitutes the therapeutic mainstay in DKD patients with albuminuria and glomerular diseases at present. It had been reported that ACEI/ARBs were associated with a lower incidence of the progression to end stage renal disease in DKD patients and reduced the incidence of composite MACE outcome [43].
The systemic RAAS would activated by natriuresis paralleled which was caused by volume depletion. Classical RAAS cascade gives rise to the production of angiotensin II (Ang II) which binds to the Ang II type 1 receptor leads to vasoconstriction, cell proliferation, inflammation, increased oxidative stress and cell apoptosis [44]. SGLT2 inhibitors would contribute to increased sodium levels delivered to the macula densa and secondary autoregulatory vasoconstriction of afferent glomerular arteriolae to neutralize the vascular imbalance driven by local Ang II characterized by glomerular hypertension in T2DM [45].
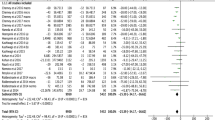
SGLT2 inhibitors and ACEI/ARBs clearly play different roles in different places on the kidney. Figure 1 shows the action sites of SGLT2 and RASS inhibitors and the potential synergistic mechanism of their combined therapy in T2DM. Figure 2 shows the synergistic effects of SGLT2 inhibitors and ACEI/ARBs in DKD therapy.
Illustration of potential synergistic effects of SGLT2 inhibitor with ACEI/ARB in DKD therapy. ACEI/ARB angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, SGLT2i Sodium–glucose co-transporter 2 inhibitor, RAAS renin–angiotensin–aldosterone system, UGE urinary glucose excretion, BP blood pressure, SBP systolic blood pressure, HDL-C high density lipoprotein-cholesterol, eGFR estimated glomerular filtration rate, DKD diabetic kidney disease
In an experimental model study, Bautista et al. [46] found that a higher expression of SGLT2 in hypertensive rats than in normotensive rats. And the levels of protein and mRNA were decreased in rats treated with either ramipril or losartan. Therefore, they suggested that in renovascular hypertension, Ang II induced SGLT2 via the Ang II type 1 receptor possibly contributing to increased absorption of Na and thereby to the development or maintenance of hypertension.
Although SGLT2 inhibitors or ACEI/ARBs have effects on albuminuria- and BP-lowering in patients with DKD, the effects of monotherapy are always unsatisfactory. Considering their complementary mechanisms on the kidneys, theoretically, SGLT2 inhibitors and ACEI/ARBs should have synergistic action. Recently several studies indicated that the combination of SGLT2 inhibitors with ACEI/ARBs satisfactorily afforded greater renoprotection than administration of either drug alone. These results demonstrated a long-term control of hyperglycemia and BP, reduction of hyperfiltration and proteinuria, and attenuation of the development of renal injury in Dahl-STZ rat model and patients of DKD [46,47,48].
In a phase III clinical trial, ACEI/ARBs added-on to dapagliflozin resulted in the albuminuria and SBP decreased by −33.2% [95% confidence interval (CI) −45.4, −18.2] and −3.5 mmHg (95% CI −5.9, −1.0) compared with placebo respectively in patients with DKD. Patients had corresponding changes in HbA1c and body weight. Furthermore, trial suggested that reduction of albuminuria was to a large extent independent of glucose-lowering effects, and some other mechanisms were also involved in albuminuria-lowering effect of dapagliflozin [49]. Moreover, serum uric acid was decreased and serum potassium levels remained at normal levels by the patients in SGLT2 inhibitors treatment groups during double-blind treatment [50,51,52]. Table 1 reveals the benefits of SGLT2 inhibitors combined with ACEI/ARBs.
However, other measures of volume status such as BUN, serum creatinine remained modestly increased and eGFR mildly decreased with SGLT2 inhibitors [50, 52]. Heerspink et al. [49] showed that the initial fall in eGFR was completely reversible only 1 week after SGLT2 inhibitors discontinuation and this reversibility indicated that the initial fall in eGFR did not reflect a decrease in the number of functioning nephrons. Besides improvements in glycemic control and lower in the above mentioned CV risks, combination therapy of SGLT2 inhibitors and ACEI/ARBs coupled with other potentially favorable renal effects may lead to a reduced long-term renal risk and CV event.
SGLT2 inhibitors combined with DPP-4 inhibitors therapy
As previously mentioned, SGLT2 inhibitors could increase EGP (HGP) and plasma glucagon concentrations. However, DPP-4 inhibitors exert their hypoglycemic effects by preventing the degradation of endogenously released incretin hormones such as glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide to enhance postprandial insulin secretion and suppress glucagon secretion, likewise, decrease endogenous (hepatic) glucose [53]. In addition, a study indicated that DPP-4 inhibitors could improve endothelial function and reduce renal and vascular oxidative stress, which was independent of albuminuria-lowering or improvement in glucose control, in patients with T2DM and chronic kidney disease [54].
Merovci et al. [12] indicated that AHAs that worked specifically on the kidney improved muscle insulin sensitivity. Since more than 80% of insulin-mediated glucose disposal during the euglycemic insulin clamp took place in skeletal muscle [55], these results indicated that the lowering plasma glucose concentration in T2DM significantly improved muscle insulin resistance. A characteristic of T2DM was that the progressive deterioration of β-cell functions. By promoting glucosuria and reducing hyperglycaemia, SGLT2 inhibitors dampened glucotoxicity, which indirectly resulted in an improvement of β-cell function and peripheral insulin sensitivity [12].
As mentioned above, DPP-4 inhibitor add-on to SGLT2 inhibitor meets a need for pharmacological agents with complementary mechanisms that can be applied to effectively improve glycemic control and thereby protect kidney and have potential CV safety in patients with DKD (Fig. 3).
Illustration of potential synergistic effects of SGLT2 inhibitor with DPP-4 inhibitor in DKD therapy. SGLT2i Sodium–glucose co-transporter 2 inhibitor, DPP-4i dipeptidyl peptidase-4 inhibitor, UGE urinary glucose excretion, GLP-1 glucagon-like peptide-1, GIP glucose-dependent insulinotropic polypeptide, SBP systolic blood pressure, DKD diabetic kidney disease
A phase III, randomized, double-blind, parallel-group study showed that the combination of SGLT2 inhibitors and DPP-4 inhibitors resulted in the reductions of HbA1c (mean baseline 7.90–8.02% [62.8–64.1 mmol/mol]), FPG, serum uric acid, SBP, and hypoglycemic risk were superior to those with the individual components in patients with T2DM. As for, the SBP-lowering mechanisms of DPP-4 inhibitor may complement or augment SGLT2 inhibitor-induced plasma volume reduction and other mechanism. Of note, a higher proportion of subjects with microalbuminuria at baseline decreased to no albuminuria at the end of combination treatment [56]. Mean changes from baseline in UACR and eGFR were small and similar across treatment groups [57]. Furthermore, the combined therapy had CV safety and did not induce weight gain in several large prospective CV outcome studies, as well as potential renoprotection [53, 56]. Pharmacokinetics and pharmacodynamic (PK–PD) study investigated in healthy individuals found no drug–drug interaction in combination therapy of SGLT2 inhibitors and DPP-4 inhibitors [58].
SGLT2 inhibitors combined with GLP1-RAs therapy
It had been reported that GLP1-RAs could inhibit the potent inflammatory mediator NF-κB and decrease monocyte chemoattractant protein-1, intracellular cell adhesion molecule-1 and vascular cell adhesion molecule-1, which had been associated with abnormalities in vascular function and progression of DKD [59, 60]. Moreover, GLP1-RAs could induce significant diuretic and natriuretic responses and might have beneficial effects on renal sodium and water handling [61].
GLP1-RAs stimulated the GLP-1 receptor to increase insulin secretion and inhibited glucagon secretion in a glucose-dependent manner. Elevated glucagon levels induced by SGLT2 inhibitors could be counteracted by GLP1-RAs. SGLT2 inhibitors decreased calorie availability through the urine to reduce body weight, otherwise, weight loss might be attributed to visceral fat tissue lipolysis and enhanced lipid metabolism. But this calorie loss could lead to a compensatory appetite increase [24, 62]. However, GLP1-RAs lost body weight via reduced appetite and delayed gastric emptying [63]. The mechanisms of two combined drugs may have complemented each other and have potential renoprotection and CV safety (Fig. 4).
Illustration of potential synergistic effects of SGLT2 inhibitor with GLP-1 receptor agonists in DKD therapy. SGLT2i Sodium–glucose co-transporter 2 inhibitor, GLP1-RA glucagon-like peptide-1 receptor agonist, UGE urinary glucose excretion, NF-κB nuclear factor kappa B, MCP-1 monocyte chemoattractant protein-1, GLP-1 glucagon-like peptide-1, SBP systolic blood pressure, eGFR estimated glomerular filtration rate, HDL-C high density lipoprotein-cholesterol, LDL-C low density lipoprotein-cholesterol, DKD diabetic kidney disease
Several studies indicated that reduction of HbA1c, SBP and body weight was observably lower in patients with combination therapy than without. No significant changes in eGFR, HDLC or LDL-C were found in both groups [64, 65]. Especially, adverse effects of hypotension or dehydration in dapagliflozin/exenatide-treated participants were not reported. The study showed that combined therapy was superior to monotherapy.
SGLT2 inhibitors combined with MRAs therapy
It has been reported that Aldosterone contributes to renal injury. MRAs have effect on renoprotection by reducing the concentration of aldosterone in DKD patients. But MRAs are limited by notable side effect hyperkalaemia. An experimental model study demonstrated that spironolactone prevented the STZ-induced increase in the renal aldosterone synthase CYP11B2 mRNA content and did not influence glycemic level or BP in STZ-induced diabetic rats. Moreover, controlling blood glucose with AHAs also attenuated the renal expression of mRNA for CYP11B2. These results indicated that spironolactone exerted renoprotective effects and inhibited local angiotensin-converting enzyme expression and the hyperglycemia-induced overexpression of CYP11B2 in the kidney [66].
The novel drug finerenone of MRAs is more selective for the mineralocorticoid receptor than spironolactone and has greater affinity for the mineralocorticoid receptor than eplerenone, and shows less incidence of hyperkalemia as compared to spironolactone. Hence, it can efficiently reduce the concentration of aldosterone and play a role in renoprotection [67]. Furthermore, a large randomized controlled trial (RCT) on the renoprotective effect of finerenone in DKD is currently ongoing (FIDELIO-DKD).
As previously mentioned, SGLT2 inhibitors played roles in lowering glucose, renoprotection and CV safety [24]. It was worth noting that SGLT2 inhibitors were not increasing the risks of hyperkalemia or severe hypokalemia [28, 68]. The apparent mechanism of action in SGLT2 inhibitors and MRAs suggests that there exists a potential synergistic renoprotective effect of combination therapy to slow the progression of DKD. Large RCTs are imperative to investigate if this combination therapy can provide effective renoprotection in DKD.
The safety of combined therapy with SGLT2 inhibitors
Although the combined therapy have potential renoprotection and CV safety, receiving SGLT2 inhibitors may lead to adverse effects like genital mycotic and urinary tract infections even it combined with other drugs [29, 69]. This may be attributed to the increased and prolonged glucosuria induced by SGLT2 inhibitors. And then, adverse effect of SGLT2 inhibitors therapy reported by a study is osmotic diuresis which leads to dehydration, hypotension and renal impairment. Intravascular volume depletion, a dose-dependent increase in serum creatinine and a known marker of renal damage are also discovered in SGLT2 inhibitors treatment in patients with T2DM [70]. In addition, efficacy in lowering glucose levels of SGLT2 inhibitors depends in the filtration rate in the kidneys, so it has shown no efficacy in reducing HbA1c levels in patients with severe renal impairment, ESRD and patients on dialysis, as well as some moderate renal impairment [28].
Above all, although these side effects are in most cases not of serious nature, patients and the health care providers should be aware of them, in any case. In addition, SGLT2 inhibitors should be prescribed with caution in T2DM patients with significant renal impairment. Maybe health care providers should limit the capacity of this drug class in treating severe DKD patients.
Conclusions
All the researches, mentioned above, demonstrating the SGLT2 inhibitors with their novel mechanism and associated benefits on glucose-lowering, renoprotection, body weight, CV safety, etc. have proved to be promising choices either as monotherapy or as combination therapy for patients with DKD. Moreover, large RCTs are necessary to investigate the combination therapy of SGLT2 inhibitors with the above mentioned drugs and thereby provide the direct evidences of renoprotection and CV safety in DKD patients.
Change history
09 March 2018
Following publication of the original article [1] the authors reported that the first affiliation (“Medical Center of the Graduate School, Nanchang University, China”) had been added in error, and that the correct author information is as given in this erratum.
Abbreviations
- ACEI:
-
angiotensin-converting enzyme inhibitors
- AHAs:
-
anti-hyperglycemic agents
- Ang II:
-
angiotensin II
- ARBs:
-
angiotensin receptor blockers
- BP:
-
blood pressure
- BUN:
-
blood urea nitrogen
- CI:
-
confidence interval
- CV:
-
cardiovascular
- DKD:
-
diabetic kidney disease
- DPP-4:
-
dipeptidyl peptidase-4
- eGFR:
-
estimated glomerular filtration rate
- EGP:
-
endogenous glucose production
- FPG:
-
fasting plasma glucose
- GFR:
-
glomerular filtration rate
- GLP-1:
-
glucagon-like peptide-1
- GLP1-RAs:
-
glucagon-like peptide-1 receptor agonists
- HbA1c:
-
glycated haemoglobin
- HDL-C:
-
high density lipoprotein-cholesterol
- HF:
-
heart failure
- HGP:
-
hepatic glucose production
- LDL-C:
-
low density lipoprotein-cholesterol
- MACE:
-
major adverse cardiovascular events
- MRAs:
-
mineralocorticoid receptor antagonists
- NF-kB:
-
nuclear factor kappa B
- OLETF:
-
Otsuka Long-Evans Tokushima Fatty
- PK-PD:
-
pharmokinetics and pharmacodynamic
- RAAS:
-
renin–angiotensin–aldosterone system
- RAS:
-
renin–angiotensin system
- RCT:
-
randomized controlled trial
- SBP:
-
systolic blood pressure
- SGLT2:
-
sodium–glucose co-transporter 2
- STZ:
-
streptozocin
- T2DM:
-
type 2 diabetes mellitus
- UACR:
-
urine albumin–creatinine ratio
- UGE:
-
urinary glucose excretion
References
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the study of diabetes (EASD). Diabetologia. 2012;55:1577–96.
Giunti S, Barit D, Cooper ME. Mechanisms of diabetic nephropathy: role of hypertension. Hypertension. 2006;48:519–26.
Bennett WL, Maruthur NM, Singh S, Segal JB, Wilson LM, Chatterjee R, et al. Comparative effectiveness and safety of medications for type 2 diabetes: an update including new drugs and 2-drug combinations. Ann Int Med. 2011;154:602–13.
Gnudi L, Coward RJ, Long DA. Diabetic nephropathy: perspective on novel molecular mechanisms. Trends Endocrinol Metab. 2016;27:820–30.
Elisaf M, Tzavela E, Karanatsis N, Tsimichodimos V. Antidiabetic drugs and the kidney. Curr Pharm Des. 2017. doi:10.2174/1381612823666170307103222.
Yang W, Ji L, Zhou Z, Cain VA, Johnsson KM, Sjostrom CD. Efficacy and safety of dapagliflozin in Asian patients: a pooled analysis. J Diabetes. 2016. doi:10.1111/1753-0407.12484.
Gerich JE. Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabet Med. 2010;27:136–42.
Wright EM, Turk E. The sodium/glucose cotransport family SLC5. Pflugers Arch. 2004;447:510–8.
DeFronzo RA, Davidson JA, Del PS. The role of the kidneys in glucose homeostasis: a new path towards normalizing glycaemia. Diabetes Obes Metab. 2012;14:5–14.
Bailey CJ. Renal glucose reabsorption inhibitors to treat diabetes. Trends Pharmacol Sci. 2011;32:63–71.
Abdul-Ghani MA, Norton L, Defronzo RA. Role of Sodium–glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetes. Endocr Rev. 2011;32:515–31.
Merovci A, Solis-Herrera C, Daniele G, Eldor R, Fiorentino TV, Tripathy D, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124:509–14.
DeFronzo RA, Andres R, Bedsoe TA, Boden G, Faloona GA, Tobin JD. A test of the hypothesis that the rate of fall in glucose concentration triggers counterregulatory hormonal responses in man. Diabetes. 1977;26:445–52.
DeFronzo RA, Ferrannini E. Regulation of hepatic glucose metabolism in humans. Diabetes Metab Rev. 1987;3:415–59.
Cherrington AD, Lecture B. Control of glucose uptake and release by the liver in vivo. Diabetes. 1997;1999(48):1198–214.
Matsuda M, Defronzo RA, Glass L, Consoli A, Giordano M, Bressler P, et al. Glucagon dose-response curve for hepatic glucose production and glucose disposal in type 2 diabetic patients and normal individuals. Metabolism. 2002;51:1111–9.
Shin SJ, Chung S, Kim SJ, Lee EM, Yoo YH, Kim JW, et al. Effect of Sodium–glucose co-transporter 2 inhibitor, dapagliflozin, on renal renin–angiotensin system in an animal model of type 2 diabetes. PLoS ONE. 2016;11:e165703.
Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of Sodium–glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587–97.
Vallon V, Gerasimova M, Rose MA, Masuda T, Satriano J, Mayoux E, et al. SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice. Am J Physiol Renal Physiol. 2014;306:F194–204.
Vallon V. The proximal tubule in the pathophysiology of the diabetic kidney. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1009–22.
Panchapakesan U, Pegg K, Gross S, Komala MG, Mudaliar H, Forbes J, et al. Effects of SGLT2 inhibition in human kidney proximal tubular cells–renoprotection in diabetic nephropathy? PLoS ONE. 2013;8:e54442.
Chang YK, Choi H, Jeong JY, Na KR, Lee KW, Lim BJ, et al. Dapagliflozin, SGLT2 inhibitor, attenuates renal ischemia–reperfusion injury. PLoS ONE. 2016;11:e158810.
Neumiller JJ. Empagliflozin: a new Sodium–glucose co-transporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes. Drugs Context. 2014;3:212262.
Andrianesis V, Glykofridi S, Doupis J. The renal effects of SGLT2 inhibitors and a mini-review of the literature. Ther Adv Endocrinol Metab. 2016;7:212–28.
Lovshin JA, Gilbert RE. Are SGLT2 inhibitors reasonable antihypertensive drugs and renoprotective? Curr Hypertens Rep. 2015;17:551.
De Nicola L, Gabbai FB, Liberti ME, Sagliocca A, Conte G, Minutolo R. Sodium/glucose cotransporter 2 inhibitors and prevention of diabetic nephropathy: targeting the renal tubule in diabetes. Am J Kidney Dis. 2014;64:16–24.
Thomas MC. Renal effects of dapagliflozin in patients with type 2 diabetes. Ther Adv Endocrinol Metab. 2014;5:53–61.
Kohan DE, Fioretto P, Tang W, List JF. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int. 2014;85:962–71.
Stenlof K, Cefalu WT, Kim KA, Alba M, Usiskin K, Tong C, et al. Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetes Obes Metab. 2013;15:372–82.
Sano M, Takei M, Shiraishi Y, Suzuki Y. Increased hematocrit during Sodium–glucose cotransporter 2 inhibitor therapy indicates recovery of tubulointerstitial function in diabetic kidneys. J Clin Med Res. 2016;8:844–7.
Yale JF, Bakris G, Cariou B, Yue D, David-Neto E, Xi L, et al. Efficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes Metab. 2013;15:463–73.
Vallon V, Blantz RC, Thomson S. Glomerular hyperfiltration and the salt paradox in early [corrected] type 1 diabetes mellitus: a tubulo-centric view. J Am Soc Nephrol. 2003;14:530–7.
Cea SL, Johansson S, Stefansson B, Rodriguez LA. Cardiovascular events and all-cause mortality in a cohort of 57,946 patients with type 2 diabetes: associations with renal function and cardiovascular risk factors. Cardiovasc Diabetol. 2015;14:38.
Ferrannini E, DeFronzo RA. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J. 2015;36:2288–96.
Avogaro A, Fadini GP, Sesti G, Bonora E, Del PS. Continued efforts to translate diabetes cardiovascular outcome trials into clinical practice. Cardiovasc Diabetol. 2016;15:111.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME(R) trial. Eur Heart J. 2016;37:1526–34.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–34.
Sonesson C, Johansson PA, Johnsson E, Gause-Nilsson I. Cardiovascular effects of dapagliflozin in patients with type 2 diabetes and different risk categories: a meta-analysis. Cardiovasc Diabetol. 2016;15:37.
Inagaki N, Kondo K, Yoshinari T, Kuki H. Efficacy and safety of canagliflozin alone or as add-on to other oral antihyperglycemic drugs in Japanese patients with type 2 diabetes: a 52-week open-label study. J Diabetes Investig. 2015;6:210–8.
Hershon KS. Options for empagliflozin in combination therapy in type 2 diabetes mellitus. Int J Gen Med. 2016;9:155–72.
de Boer IH, Kahn SE. SGLT2 inhibitors-sweet success for diabetic kidney disease? J Am Soc Nephrol. 2017;28:7–10.
Wu LS, Chang SH, Chang GJ, Liu JR, Chan YH, Lee HF, et al. A comparison between angiotensin converting enzyme inhibitors and angiotensin receptor blockers on end stage renal disease and major adverse cardiovascular events in diabetic patients: a population-based dynamic cohort study in Taiwan. Cardiovasc Diabetol. 2016;15:56.
Burrell LM, Johnston CI, Tikellis C, Cooper ME. ACE2, a new regulator of the renin–angiotensin system. Trends Endocrinol Metab. 2004;15:166–9.
Stanton RC. Sodium glucose transport 2 (SGLT2) inhibition decreases glomerular hyperfiltration: is there a role for SGLT2 inhibitors in diabetic kidney disease? Circulation. 2014;129:542–4.
Bautista R, Manning R, Martinez F, Avila-Casado MC, Soto V, Medina A, et al. Angiotensin II-dependent increased expression of Na+-glucose cotransporter in hypertension. Am J Physiol Renal Physiol. 2004;286:F127–33.
Kojima N, Williams JM, Takahashi T, Miyata N, Roman RJ. Effects of a new SGLT2 inhibitor, luseogliflozin, on diabetic nephropathy in T2DN rats. J Pharmacol Exp Ther. 2013;345:464–72.
Kojima N, Williams JM, Slaughter TN, Kato S, Takahashi T, Miyata N, et al. Renoprotective effects of combined SGLT2 and ACE inhibitor therapy in diabetic Dahl S rats. Physiol Rep. 2015;3:E12436.
Heerspink HJ, Johnsson E, Gause-Nilsson I, Cain VA, Sjostrom CD. Dapagliflozin reduces albuminuria in patients with diabetes and hypertension receiving renin–angiotensin blockers. Diabetes Obes Metab. 2016;18:590–7.
Weber MA, Mansfield TA, Alessi F, Iqbal N, Parikh S, Ptaszynska A. Effects of dapagliflozin on blood pressure in hypertensive diabetic patients on renin–angiotensin system blockade. Blood Press. 2016;25:93–103.
Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, Ptaszynska A. Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Diabetes Endocrinol. 2016;4:211–20.
Sha S, Polidori D, Heise T, Natarajan J, Farrell K, Wang SS, et al. Effect of the sodium glucose co-transporter 2 inhibitor canagliflozin on plasma volume in patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2014;16:1087–95.
Scheen AJ. Safety of dipeptidyl peptidase-4 inhibitors for treating type 2 diabetes. Expert Opin Drug Saf. 2015;14:505–24.
Sagara M, Suzuki K, Aoki C, Tanaka S, Taguchi I, Inoue T, et al. Impact of teneligliptin on oxidative stress and endothelial function in type 2 diabetes patients with chronic kidney disease: a case-control study. Cardiovasc Diabetol. 2016;15:76.
DeFronzo RA, Jacot E, Jequier E, Maeder E, Wahren J, Felber JP. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes. 1981;30:1000–7.
DeFronzo RA, Lewin A, Patel S, Liu D, Kaste R, Woerle HJ, et al. Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care. 2015;38:384–93.
Hansen L, Iqbal N, Ekholm E, Cook W, Hirshberg B. Postprandial dynamics of plasma glucose, insulin, and glucagon in patients with type 2 diabetes treated with saxagliptin plus dapagliflozin add-on to metformin therapy. Endocr Pract. 2014;20:1187–97.
Brand T, Macha S, Mattheus M, Pinnetti S, Woerle HJ. Pharmacokinetics of empagliflozin, a sodium glucose cotransporter-2 (SGLT-2) inhibitor, coadministered with sitagliptin in healthy volunteers. Adv Ther. 2012;29:889–99.
Chaudhuri A, Ghanim H, Vora M, Sia CL, Korzeniewski K, Dhindsa S, et al. Exenatide exerts a potent antiinflammatory effect. J Clin Endocrinol Metab. 2012;97:198–207.
Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab. 2009;94:3171–82.
Zhou X, Huang CH, Lao J, Pocai A, Forrest G, Price O, et al. Acute hemodynamic and renal effects of glucagon-like peptide 1 analog and dipeptidyl peptidase-4 inhibitor in rats. Cardiovasc Diabetol. 2015;14:29.
Ferrannini G, Hach T, Crowe S, Sanghvi A, Hall KD, Ferrannini E. Energy balance after Sodium–glucose cotransporter 2 inhibition. Diabetes Care. 2015;38:1730–5.
Bhavsar S, Mudaliar S, Cherrington A. Evolution of exenatide as a diabetes therapeutic. Curr Diabetes Rev. 2013;9:161–93.
Lundkvist P, Sjostrom CD, Amini S, Pereira MJ, Johnsson E, Eriksson JW. Dapagliflozin once-daily and exenatide once-weekly dual therapy: a 24-week randomized, placebo-controlled, phase II study examining effects on body weight and prediabetes in obese adults without diabetes. Diabetes Obes Metab. 2017;19:49–60.
Gorgojo-Martinez JJ, Serrano-Moreno C, Sanz-Velasco A, Feo-Ortega G, Almodovar-Ruiz F. Real-world effectiveness and safety of dapagliflozin therapy added to a GLP1 receptor agonist in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2017;27:129–37.
Taira M, Toba H, Murakami M, Iga I, Serizawa R, Murata S, et al. Spironolactone exhibits direct renoprotective effects and inhibits renal renin–angiotensin–aldosterone system in diabetic rats. Eur J Pharmacol. 2008;589:264–71.
Yang P, Huang T, Xu G. The novel mineralocorticoid receptor antagonist finerenone in diabetic kidney disease: progress and challenges. Metabolism. 2016;65:1342–9.
Yavin Y, Mansfield TA, Ptaszynska A, Johnsson K, Parikh S, Johnsson E. Effect of the SGLT2 inhibitor dapagliflozin on potassium levels in patients with type 2 diabetes mellitus: a pooled analysis. Diabetes Ther. 2016;7:125–37.
Wilding JP, Charpentier G, Hollander P, Gonzalez-Galvez G, Mathieu C, Vercruysse F, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract. 2013;67:1267–82.
Nauck MA. Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Des Devel Ther. 2014;8:1335–80.
Authors’ contributions
HZ performed the literature searching, reviewed articles and wrote the manuscript. BZ revised the manuscript and provided the second views during the manuscript revision. GX reviewed the included articles and revised the manuscript. All authors read and approved the final the manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of supporting data
The data is available for review on request.
Funding
This work was supported by the National Natural Science Foundation of China (No. H0517/81560132).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional information
A correction to this article is available online at https://doi.org/10.1186/s12933-018-0676-1.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zou, H., Zhou, B. & Xu, G. SGLT2 inhibitors: a novel choice for the combination therapy in diabetic kidney disease. Cardiovasc Diabetol 16, 65 (2017). https://doi.org/10.1186/s12933-017-0547-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-017-0547-1