Abstract
Background
The complement component C1q triggers activation of the classical immune pathway and can bind to adiponectin (APN). Recently, some studies have been reported that serum C1q-APN/total APN ratio correlates with atherosclerosis and coronary artery disease (CAD). We assessed the relationships between C1q related variables and the severity of CAD, and investigated the localization of the C1q–APN complex.
Methods
The sample included 153 subjects comprising healthy controls and patients with subclinical or overt CAD. We measured the serum concentrations of C1q, total APN, and high-molecular weight (HMW)-APN, and the amount of C1q–APN complex. We identified the sites of C1q–APN complex deposition in various adipose tissues and blood vessels.
Results
Serum concentrations of C1q and HMW-APN and the C1q/HMW-APN ratio were independently associated with the severity of coronary stenosis. The amount of C1q–APN complex was significantly higher in patients with CAD compared with controls. C1q and APN co-localized in perivascular areas of subcutaneous, visceral, and pericardial fat tissues, and the internal mammary artery of patients with severe CAD.
Conclusions
Serum C1q concentration and the C1q/HMW-APN ratio were independent markers of coronary artery stenosis. The amount of C1q–APN complex was significantly greater in serum from CAD patients. C1q and APN co-localized to perivascular areas in adipose tissue and blood vessels. The association between the increased amount of the C1q–APN complex and CAD should be investigated further.
Similar content being viewed by others
Background
The incidence of cardiovascular diseases has increased markedly in recent years, and atherosclerotic coronary artery disease (CAD) is now the most common cause of death in the world. The process of atherosclerosis is mediated by chronic inflammation in which dyslipidemia, hypertension, and diabetes play important pathogenic roles [1,2]. Considering the potentially fatal consequences of CAD, it is important to find biomarkers that can predict CAD early and precisely. To date, a number of adipokines and inflammatory cytokines have been investigated in the search for reliable predictors of CAD [3,4].
Adiponectin (APN) is a well-known adipokine secreted almost exclusively by adipocytes and circulates at a high concentration [5]. It has beneficial effects on insulin sensitivity and glucose homeostasis [6,7]. APN also inhibits inflammation and plays a role in the prevention of atherosclerosis. Thus, it is considered to be a protective adipokine and is therefore a potential therapeutic agent to prevent or treat atherosclerosis [8,9]. APN has a adhesive property and exists as large homo-oligomers in trimer, hexamer, and high-molecular weight (HMW) forms [10]. Some studies have suggested that the HMW form (HMW-APN) is the most biologically active form [11] and is a more accurate, independent risk factor for CAD than is the total APN amount or concentration [12,13].
Complement is a major system involved in host innate immunity [14]. Complement 1q (C1q), a subcomponent of complement C1, plays a key role in triggering activation of the classical pathway by recognition of immune complexes [15]. Like APN, C1q is abundant in the circulation and is structurally similar to APN; both have a collagen-like domain and a globular heads domain [16]. C1q is important in the immune response involving complement activation, but little is known about its role in chronic, low-grade systemic inflammation, which plays an important role in metabolic diseases such as atherosclerosis. One study has demonstrated that recombinant and native human APN binds to purified C1q under physiological conditions [17]. Recent studies have reported that the C1q–APN protein complex exists in human blood [18,19] and that the serum C1q–APN/total APN ratio may serve as a biomarker of CAD [20]. However, the clinical significance and physiological function of the C1q–APN complex and the tissue sites of C1q–APN complex deposition are not well known.
We measured the amount of serum APN parameters including C1q, total APN, HMW-APN, and C1q–APN complex to determine whether any of these variables correlates with the severity of coronary artery stenosis and could thus serve as a biomarker of CAD. We identified the deposition sites of C1q and APN in various adipose tissues and blood vessel to provide a better understanding of the C1q–APN complex in CAD patients.
Methods
Study subjects
A total of 153 subjects were enrolled in this study. This included 113 asymptomatic patients who had undergone a cardiac evaluation with 64-slice multidetector computed tomography (MDCT) either as a health check or for cardiac evaluation of high-risk patients with prediabetes or drug-naïve patients with type 2 diabetes at the Seoul National University Bundang Hospital [SNUBH] from March 2005 to May 2010.
The other 40 subjects were symptomatic patients with coronary artery stenosis ≥50% in three major coronary arteries. Elective coronary artery bypass surgery was performed and samples of whole adipose tissue (subcutaneous, visceral (preperitoneal), and/or pericardial fat), internal mammary artery, and blood were obtained as a part of a study to identify candidate biomarkers of atherosclerosis.
We identified their risk factors from medical history, demographics, baseline clinical profile, and concomitant medications. This study was conducted according to the Declaration of Helsinki and was approved by ethics committees of SNUBH (SNUBH IRB#B-1203/147-006, #A111218-CP02) and all subjects provided their written informed consent.
Measurement of anthropometric and biochemical parameters
Body weight, height, and blood pressure were measured at enrollment in the study. Body mass index was calculated as the weight in kilograms divided by the square of the height in meters (kg/m2). Serum concentrations of total cholesterol, triglycerides, high-density lipoprotein-cholesterol, low-density lipoprotein (LDL)-cholesterol, aspartate aminotransferase, alanine aminotransferase, creatinine, glycated hemoglobin (HbA1c), high-sensitivity C-reactive protein (hs-CRP), and plasma glucose were measured after a ≥12-hour fast. We defined diabetes mellitus as a fasting plasma glucose concentration of ≥126 mg/dL, an HbA1c level ≥6.5%, or taking antidiabetic medicine. Hypertension was defined as systolic blood pressure >140 mmHg, or diastolic blood pressure >90 mmHg, or taking antihypertensive medicine. Dyslipidemia was defined as an LDL-C concentration of ≥130 mg/dL, or hypertriglyceridemia (triglyceride concentration ≥200 mg/dL), or taking lipid-lowering medicine. Serum C1q concentration was measured using an enzyme-linked immunosorbent assay (ELISA) kit (HK356, Hycult Biotech, Uden, The Netherlands) using samples that had been frozen at −80°C until analyzed. ELISA kits were used to measure serum total APN concentration (EZHADP-61 K, Millipore, Billerica, MA, USA) and HMW-APN (EZHMWA-64 K, Millipore) in the same samples.
MDCT protocol
CAD was detected using 64-slice MDCT during a routine health examination. Subjects with a heart rate >70 beats per min received 10–30 mg of intravenous esmolol (Jeil Pharm, Seoul, Korea) before MDCT imaging. CT angiography was performed with a 64-slice MDCT scanner (Brilliance 64, Philips Medical Systems, Best, The Netherlands) using the standard scanning protocol described previously [21].
Definition of coronary artery stenosis
Coronary artery stenosis was identified as percent of luminal narrowing of at least 1 major coronary artery and was evaluated with MDCT or coronary angiography. Coronary artery stenosis was categorized into three classifications: normal (any coronary artery stenosis <25%), mild to moderate (any coronary artery stenosis ≥25%), and severe (three coronary artery stenosis ≥50%; coronary artery bypass surgery). The presence of CAD was defined as any coronary artery stenosis ≥50% regardless of number of involved coronary artery.
Blood and tissue samples
Serum was obtained from peripheral blood at the time of patient enrollment. Fat tissues from subcutaneous, visceral, and pericardial areas, and samples of the internal mammary artery were obtained from 40 patients during coronary artery bypass surgery and were irrigated with saline. All of the samples were stored at −80°C until analyzed.
Immunoblotting assay to detect the C1q–APN complex
Human serum was mixed with C1q antibody (SC-53544, Santa Cruz Biotechnology, Dallas, TX, USA) in 1× kinase buffer (20 mM HEPES pH 7.4, 5 mM MgCl2, 1 mM dithiothreitol) and agitated overnight at 4°C. Protein G (17-0618-01, GE Healthcare, Buckinghamshire, UK) was added to the mixture, and the mixture was rotated for 4 h at 4°C. After three washes, the C1q-immunocomplexes were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis and western blotting using anti-APN antibody (ab18851, Abcam, Cambridge, UK).
Histological analysis
Deparaffinized adipose tissue sections and blood vessels were fixed in 4% paraformaldehyde in phosphate-buffered saline. The sections of fat tissues and vessels were stained with hematoxylin–eosin. Immunostaining was performed overnight at 4°C with mouse anti-C1q (ab71089, Abcam,) or with rabbit anti-APN (NB100-65810, Novus Biologicals, Littleton, CO, USA) antibodies. The sections were then washed and incubated in Alexa Fluor 488 goat anti-rabbit IgG (Moleaulr Probes, Eugene, OR) and Alexa Fluor 594 goat anti-mouse IgG (Molecular Probes, Eugene, OR) as the secondary antibody for 1 h at 37°C. The slides were examined under a Zeiss Axio Imager A1 fluorescent microscope (Carl Zeiss, Cambridge, UK).
Statistical analysis
All values are expressed as mean and standard deviation (SD) or number (percent). Clinical parameters that were not normally distributed were log-transformed to reduce the skewness; we present the results as the anti-logarithm for ease of interpretation. Differences in parameters between groups were analyzed using χ 2-test, Student’s t-test, or one-way analysis of variance (ANOVA). When significantly different values were observed in an ANOVA, Bonferroni post hoc analysis was applied to identify the significantly different values. Simple and multivariate logistic regression analysis was used to determine the associations between parameters and CAD. A p-value <0.05 was considered significant. All analyses were performed using SPSS 17.0 for Windows.
Results
Baseline characteristics of subjects
The characteristics of the study subjects are summarized in Table 1. Serum C1q and HMW-APN concentrations were significantly lower in patients with severe coronary artery stenosis compared with those with no stenosis or mild to moderate stenosis. There was a trend toward a stepwise decrease in these concentrations with severity of stenosis. However, serum total APN concentration did not differ significantly between the groups. The C1q/HMW-APN ratio was significantly higher in patients with severe stenosis compared with those with no stenosis or with mild to moderate stenosis (Table 1).
Men had significantly lower serum concentrations of both total APN and HMW-APN than women: 5.40 ± 3.71 and 9.51 ± 4.17 μg/mL (P <0.001) for total APN and 2.91 ± 2.33 and 5.34 ± 3.75 μg/mL for HMW-APN (P <0.001), respectively. Serum C1q concentration did not differ significantly between men and women (5.19 ± 1.50 and 5.32 ± 1.64 μg/mL, respectively; P = 0.656).
Simple and multivariate logistic regression analyses of the associations between APN parameters and CAD
Logistic regression analysis was performed to evaluate the relationship between CAD and various APN parameters (Table 2). Simple logistic regression analysis showed that the presence of CAD correlated significantly with the concentrations of C1q, HMW-APN, and the C1q/HMW-APN ratio. Following adjustment for age and sex, the associations between CAD and the concentration of C1q, HMW-APN, and the C1q/HMW-APN ratio were significant. After adjusting for age, sex, body mass index, diabetes mellitus, hypertension, and dyslipidemia, the concentrations of C1q total APN, HMW-APN, and the C1q/HMW-APN ratio were independently associated with CAD (odds ratio, OR 0.01 [confidence interval, CI 0.001 – 0.091]; OR 0.88 [CI 0.77 0– 0.996]; OR 0.25 [CI 0.121 – 0.517]; and OR 2.09 [CI 1.122 – 3.907], respectively).
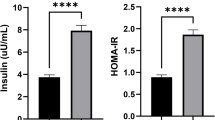
Detection of C1q-APN complex in human serum
To confirm whether C1q and APN form complexes in human serum, we performed immunoprecipitation and an immunoblotting assay. Serum samples from normal controls without CAD (n = 8) and from patients with CAD (n = 8) were subjected to immunoprecipitation with antibody against C1q, followed by immunoblotting with antibody against APN. APN was detected in C1q immunoprecipitates (Figure 1A). The serum C1q–APN complex was detected, and the relative amount of serum C1q–APN complex in the serum was about twofold higher in patients with CAD compared with the controls (P = 0.026) (Figure 1B).
Immunofluorescence of C1q and APN in adipose tissue and blood vessels
We selected samples of adipose tissue (visceral, pericardial, and subcutaneous fat) and the internal mammary artery taken during coronary artery bypass surgery from four patients with CAD. The samples were stained for C1q and total APN using immunofluorescent antibodies. Positive staining for C1q and total APN by immunofluorescence was shown along the perivascular areas in all fat tissues and in the intimal–medial layer of blood vessels. C1q and APN were almost completely co-localized in the same areas. Because the results were similar among 4 subjects, we showed the results of 1 subject, representatively (Figure 2).
Co-localization of C1q and APN deposited in adipose tissue and blood vessels (×100). Positive staining of C1q (red) and APN (green) is shown along the perivascular areas of fat tissues and intimal–medial layer of the blood vessel. C1q and APN co-localized almost completely in the same areas. H&E, hematoxylin and eosin.
Discussion
The major findings of the present study are as follows. First, serum C1q concentration was significantly lower and the serum C1q/HMW-APN ratio significantly higher in subjects with severe coronary artery stenosis compared with subjects with no stenosis or mild to moderate stenosis. By contrast, APN concentration did not differ according to the presence or absence of stenosis. Second, the amount of the C1q–APN complex in serum was significantly higher in subjects with CAD than in subjects without CAD. Third, the C1q and APN co-localized to the perivascular areas of adipose tissues and intimal–medial layer of blood vessels of CAD patients.
C1q is the first component of the serum complement system. It comprises six globular “heads” linked via six collagen-like “stalks” to a fibril-like central region and possesses significant homology to APN [16]. The traditionally accepted role of C1q is the recognition of immune complexes and activation of the classical pathway. Binding of Fc regions of immunoglobulin to the globular head portion of C1q induces further activation of the cascade of proteins comprising the classical pathway [22]. C1q is produced by and deposits around macrophages and dendritic cells, and promotes phagocytosis [23]. However, the role of C1q is not restricted to recognition of immune complexes or other molecules. Nontraditional roles of C1q are rapidly emerging and include autoimmune diseases and carcinogenesis [24], but little is known about its possible role in chronic metabolic diseases such as atherosclerosis, obesity, and diabetes.
C1q has recently been suggested to play a role in atherosclerosis when complexed with APN. Previously, it has reported that the C1q–APN complex exists in the blood and has suggested that the C1q–APN/total APN ratio is a useful predictive marker of the metabolic syndrome and CAD in Japanese people [18,20,25]. A high serum C1q–APN/total APN ratio was associated with CAD prevalence, independent of other CAD risk factors in a previous study [20]. We measured the serum concentrations of C1q, total APN, and HMW-APN, and their associations with the severity of CAD. Previous studies have reported nonsignificant correlations between C1q, HMW-APN, and atherosclerotic disease [20,25]. However, in contrast to the previous results, we found that the serum concentrations of C1q and HMW-APN were independently associated with CAD and decreased significantly with increasing severity of coronary artery stenosis. The total APN concentration and the C1q/total APN ratio were not associated with the presence or severity of CAD. We could not measure the absolute concentration of the C1q–APN complex in the blood because no commercial ELISA kit is available for the direct measurement of the complex. Instead, we measured the quantity of C1q–APN complex in coimmunoprecipitation experiments. The amount of C1q–APN complex was significantly higher in the blood of patients with CAD than in the controls with no CAD. Our result is concordant with the other study that serum C1q-APN levels were significantly higher in the acute coronary syndrome than in the normal coronary group [26]. Recently, the protein family C1q/TNF-related protein (CTRP) has been discovered as adiponectin paralog. Some CTRP family members have metabolic regulatory function in glucose and/or fat homeostasis [27]. CTRP-3 is an anti-inflammatory adipokine and serum CTRP-3 concentrations are significantly decreased in patients with acute coronary syndrome [28]. Serum CTRP-1 and CTRP-3 levels were positively associated with atherosclerosis [29,30]. These results suggest that APN parameters including C1q, C1q-APN complex and CTRPs might be important in the regulation of atherosclerosis and development of acute coronary syndrome.
Interestingly, we confirmed the deposition of the C1q and APN in human white adipose tissues and blood vessels. Immunofluorescence showed that C1q and APN co-localized in the perivascular areas of fat tissues and in the intimal–medial area of the artery. APN is known to bind to collagen types I, II, and V, which are present in the vascular intima. APN is detected in the walls of injured arteries and in atherosclerotic lesions [31]. Our study is the first to show the co-localization of C1q and APN in human tissues. However, it remains unclear which forms of circulating APN forms protein complex with C1q. The precise physiological role of the complex is also unknown, but we speculate that APN may play a protective role in the C1q-induced activation of the complement pathway, which is known as a cause of vascular damage in autoimmune disease or other types of inflammation that contribute to systemic atherosclerosis. APN is thought to prevent inflammation and to play a beneficial role in preventing atherosclerosis and metabolic syndrome [32,33]. One study reported that adiponectin protects against activation of C1q-induced inflammation in injured tissues of mice [34], which is similar evidence as our result of C1q-APN co-localization in perivascular tissues. Further research is needed to clarify the role of the C1q–APN complex in protecting against the development of atherosclerosis in humans.
The present study has several limitations. First, it was a cross-sectional study, making it difficult to interpret whether there is a causal relationship between the markers measured in this study and CAD. Further prospective studies are needed to confirm this relationship. Second, we could not directly measure the serum concentration and tissue deposit of C1q-APN complex because of the lack of a commercially available method. Third, the number of serum and tissue samples used in the tests for detection of C1q and APN was small. Although we repeated the tests, there could be a selection bias. Forth, we could not get tissue and blood vessel samples of normal healthy control.
Conclusion
In conclusion, the present study demonstrated that serum C1q concentration and the C1q/HMW-APN ratio were independent markers of coronary artery stenosis. The co-localization of the C1q and APN was observed in the perivascular areas of fat tissues and in the intimal–medial area of the internal mammary artery in conjunction with a higher serum amount of the C1q–APN complex in patients with CAD. These results suggest that the C1q–APN complex may play a role in the development of atherosclerosis. Further human studies are needed to clarify whether the C1q–APN complex is a potential target for new treatments to protect against atherosclerosis.
Abbreviations
- CAD:
-
Coronary artery disease
- APN:
-
Adiponectin
- HMW:
-
High-molecular weight
- C1q:
-
Complement 1q
- MDCT:
-
Multidetector computed tomography
- LDL:
-
Low-density lipoprotein
- HbA1c:
-
Glycated hemoglobin
- hs-CRP:
-
High-sensitivity C-reactive protein
- ELISA:
-
Enzyme-linked immunosorbent assay
- SD:
-
Standard deviation
- ANOVA:
-
Analysis of variance
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- CTRP:
-
C1q/TNF-related protein
References
Williams KJ, Tabas I. The response-to-retention hypothesis of early atherogenesis. Arterioscler Thromb Vasc Biol. 1995;15(5):551–61.
Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999;340(2):115–26.
Syed Ikmal SI, Zaman Huri H, Vethakkan SR, Wan Ahmad WA. Potential biomarkers of insulin resistance and atherosclerosis in type 2 diabetes mellitus patients with coronary artery disease. Int J Endocrinol. 2013;2013:698567.
Choi SH, Hong ES, Lim S. Clinical implications of adipocytokines and newly emerging metabolic factors with relation to insulin resistance and cardiovascular health. Front Endocrinol (Lausanne). 2013;4:97.
Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257(1):79–83.
Hu E, Liang P, Spiegelman BM. AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem. 1996;271(18):10697–703.
Hotta K, Funahashi T, Arita Y, Takahashi M, Matsuda M, Okamoto Y, et al. Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol. 2000;20(6):1595–9.
Motoshima H, Wu X, Mahadev K, Goldstein BJ. Adiponectin suppresses proliferation and superoxide generation and enhances eNOS activity in endothelial cells treated with oxidized LDL. Biochem Biophys Res Commun. 2004;315(2):264–71.
Zhu W, Cheng KK, Vanhoutte PM, Lam KS, Xu A. Vascular effects of adiponectin: molecular mechanisms and potential therapeutic intervention. Clin Sci (Lond). 2008;114(5):361–74.
Schraw T, Wang ZV, Halberg N, Hawkins M, Scherer PE. Plasma adiponectin complexes have distinct biochemical characteristics. Endocrinology. 2008;149(5):2270–82.
Hara K, Horikoshi M, Yamauchi T, Yago H, Miyazaki O, Ebinuma H. Measurement of the high-molecular weight form of adiponectin in plasma is useful for the prediction of insulin resistance and metabolic syndrome. Diabetes Care. 2006;29(6):1357–62.
Koenig W, Khuseyinova N, Baumert J, Meisinger C, Lowel H. Serum concentrations of adiponectin and risk of type 2 diabetes mellitus and coronary heart disease in apparently healthy middle-aged men: results from the 18-year follow-up of a large cohort from southern Germany. J Am Coll Cardiol. 2006;48(7):1369–77.
Lim S, Koo BK, Cho SW, Kihara S, Funahashi T, Cho YM, et al. Association of adiponectin and resistin with cardiovascular events in Korean patients with type 2 diabetes: the Korean atherosclerosis study (KAS): a 42-month prospective study. Atherosclerosis. 2008;196(1):398–404.
Reid KB. Activation and control of the complement system. Essays Biochem. 1986;22:27–68.
Schumaker VN, Zavodszky P, Poon PH. Activation of the first component of complement. Annu Rev Immunol. 1987;5:21–42.
Arlaud GJ, Gaboriaud C, Thielens NM, Rossi V, Bersch B, Hernandez JF, et al. Structural biology of C1: dissection of a complex molecular machinery. Immunol Rev. 2001;180:136–45.
Peake PW, Shen Y, Walther A, Charlesworth JA. Adiponectin binds C1q and activates the classical pathway of complement. Biochem Biophys Res Commun. 2008;367(3):560–5.
Nakatsuji H, Kobayashi H, Kishida K, Nakagawa T, Takahashi S, Tanaka H, et al. Binding of adiponectin and C1q in human serum, and clinical significance of the measurement of C1q-adiponectin / total adiponectin ratio. Metabolism. 2013;62(1):109–20.
Kishida K, Kishida N, Arima M, Nakatsuji H, Kobayashi H, Funahashi T, et al. Serum C1q- binding adiponectin in maintenance hemodialysis patients. BMC Nephrol. 2013;14:50.
Hirata A, Kishida K, Nakatsuji H, Kobayashi H, Funahashi T, Shimomura I. High serum C1q-adiponectin/total adiponectin ratio correlates with coronary artery disease in Japanese type 2 diabetics. Metabolism. 2013;62(4):578–85.
Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol. 2008;52(5):357–65.
Siegert CE, Kazatchkine MD, Sjoholm A, Wurzner R, Loos M, Daha MR. Autoantibodies against C1q: view on clinical relevance and pathogenic role. Clin Exp Immunol. 1999;116(1):4–8.
Lu JH, Teh BK, Wang L, Wang YN, Tan YS, Lai MC, et al. The classical and regulatory functions of C1q in immunity and autoimmunity. Cell Mol Immunol. 2008;5(1):9–21.
Ghebrehiwet B, Hosszu KK, Valentino A, Peerschke EI. The C1q family of proteins: insights into the emerging non-traditional functions. Front Immunol. 2012;3:52.
Hirata A, Kishida K, Kobayashi H, Nakatsuji H, Funahashi T, Shimomura I. Correlation between serum C1q-adiponectin/total adiponectin ratio and polyvascular lesions detected by vascular ultrasonography in Japanese type 2 diabetics. Metabolism. 2013;62(3):376–85.
Kishida K, Nakagawa Y, Kobayashi H, Mazaki T, Yokoi H, Yanagi K, et al. High serum C1q-binding adiponectin levels in male patients with acute coronary syndrome. Cardiovasc Diabetol. 2014;13:9.
Seldin MM, Tan SY, Wong GW. Metabolic function of the CTRP family of hormones. Rev Endocr Metab Disord. 2014;15(2):111–23.
Choi KM, Hwang SY, Hong HC, Choi HY, Yoo HJ, Youn BS, et al. Implications of C1q/TNF-related protein-3 (CTRP-3) and progranulin in patients with acute coronary syndrome and stable angina pectoris. Cardiovasc Diabetol. 2014;13:14.
Yuasa D, Ohashi K, Shibata R, Takeshita K, Kikuchi R, Takahashi R, et al. Association of circulating C1q/TNF-related protein 1 levels with coronary artery disease in men. PLoS One. 2014;9(6):e99846.
Jung CH, Lee MJ, Kang YM, Jang JE, Leem J, Lee YL, et al. Association of serum C1q/TNF-related protein-9 concentration with arterial stiffness in subjects with type 2 diabetes. J Clin Endocrinol Metab. 2014;99(12):E2477–2484.
Okamoto Y, Arita Y, Nishida M, Muraguchi M, Ouchi N, Takahashi M, et al. An adipocyte-derived plasma protein, adiponectin, adheres to injured vascular walls. Horm Metab Res. 2000;32(2):47–50.
Duncan BB, Schmidt MI, Pankow JS, Bang H, Couper D, Ballantyne CM, et al. Adiponectin and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes. 2004;53(9):2473–8.
Luo N, Liu J, Chung BH, Yang Q, Klein RL, Garvey WT, et al. Macrophage adiponectin expression improves insulin sensitivity and protects against inflammation and atherosclerosis. Diabetes. 2010;59(4):791–9.
Ebina K, Oshima K, Matsuda M, Fukuhara A, Maeda K, Kihara S, et al. Adenovirus-mediated gene transfer of adiponectin reduces the severity of collagen-induced arthritis in mice. Biochem Biophys Res Commun. 2009;378(2):186–91.
Acknowledgements
This study was supported by the grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (grant number HI14C0074).
This work was supported by a grant (E.S.H., 2013) from the Korean Diabetes Association.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ESH analyzed the data and wrote the manuscript. CL contributed materials. HYC performed the experiments. EJK, KMK, JHM, SL, KSP, and HCJ contributed to the discussion and reviewed the manuscript. SHC conceived and designed the experiments. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hong, E.S., Lim, C., Choi, H.Y. et al. The amount of C1q–adiponectin complex is higher in the serum and the complex localizes to perivascular areas of fat tissues and the intimal–medial layer of blood vessels of coronary artery disease patients. Cardiovasc Diabetol 14, 50 (2015). https://doi.org/10.1186/s12933-015-0209-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0209-0