Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease characterized by chronic bronchitis, emphysema and vascular remodelling. The disease is associated with hypoxia, inflammation and oxidative stress. Lung fibroblasts are important cells in remodelling processes in COPD, as main producers of extracellular matrix proteins but also in synthesis of growth factors and inflammatory mediators.
Methods
In this study we aimed to investigate if there are differences in how primary distal lung fibroblasts obtained from COPD patients and healthy subjects respond to hypoxia (1% O2) and pro-fibrotic stimuli with TGF-β1 (10 ng/mL). Genes and proteins associated with oxidative stress, endoplasmic reticulum stress, remodelling and inflammation were analysed with RT-qPCR and ELISA.
Results
Hypoxia induced differences in expression of genes involved in oxidative stress (SOD3 and HIF-1α), ER stress (IRE1, PARK and ATF6), apoptosis (c-Jun and Bcl2) and remodelling (5HTR2B, Collagen7 and VEGFR2) in lung fibroblasts from COPD subjects compared to control subjects, where COPD fibroblasts were in general less responsive. The release of VEGF-C was increased after hypoxia, whereas TGF-β significantly reduced the VEGF response to hypoxia and the release of HGF. COPD fibroblasts had a higher release of IL-6, IL-8, MCP-1 and PGE2 compared to lung fibroblasts from control subjects. The release of inflammatory mediators was less affected by hypoxia, whereas TGFβ1 induced differences in inflammatory profile between fibroblasts from COPD and control subjects.
Conclusion
These results suggest that there is an alteration of gene regulation of various stress responses and remodelling associated mediator release that is related to COPD and hypoxia, where fibroblasts from COPD patients have a deficient response.
Similar content being viewed by others
Background
COPD is a severe heterogeneous lung disease with no cures or effective treatments available. Causes of the disease are related to exposure to smoke and air pollutions [1]. The disease is characterised by airflow limitations linked to chronic inflammation, fibrosis around the small airways and emphysema. Lack of sufficient oxygen supply in the lung results in hypoxic milieus which trigger cellular activity and pathological remodelling processes [2]. These events contribute to a decline in effective oxygen exchange in the alveoli and to progression of the disease. Hypoxia has mostly been studied in different cancer diseases and less in detail in ongoing remodelling processes in chronic lung diseases, highlighting the need of more research into this area. The transcriptional activator hypoxia-inducible factor (HIF) is induced by hypoxia and a modulator of oxygen homeostasis. Activation of HIF induces expression of matrix metalloproteinases and vascular endothelial factor (VEGF) to increase oxygen delivery by promoting vascular remodelling and angiogenesis [3].
Pulmonary vascular remodelling is common in COPD [4] and comorbidities in cardiovascular disease have negative impacts on COPD prognosis [5]. Airflow obstructions and fibrosis in small airways and emphysema with destruction of alveolar capillaries and epithelial cells result in decreased oxygen transport and alveolar hypoxia [2]. We have previously shown that VEGF is synthesised by primary human lung fibroblasts and induced by transforming growth factor (TGF)-β1 and prostaglandins [6] and that COPD patients have an altered fibroblast phenotype [7]. Fibroblasts are key players in regulating the homeostasis of extracellular matrix (ECM) but also in pathological remodelling processes by constituting a rich source of cytokines and growth factors and responding to profibrotic stimuli [8]. Increased VEGF expression is associated with bronchial angiogenesis that inversely correlated with lung function in COPD patients [9]. Other important pathological changes appear in COPD, such as alterations in gene expressions related to ER stress and unfolded protein responses (UPR) [10], which have been linked to oxidative stress and mitochondrial dysfunction [2].
The aim of this project was to assess if exposure to a hypoxic milieu induces responses in distally derived lung fibroblasts that mimic pathological changes, involving oxidative stress and ER stress, inflammation and remodelling, as hypoxia is implicated to be a driver for COPD progression, and if there were differences in inflammatory response to hypoxia and profibrotic stimuli between the lung fibroblasts obtained from healthy subjects and COPD patients. Investigated genes were associated with ER stress and UPR (IRE1, PERK, ATF6 and CHOP, PSMA1, PSMB6 and PSMD11), oxidative stress (Nrf2, OXR1, SOD3), metabolic or mitochondrial stress responses (PINK1 and Parkin), inflammation (PTGS2) and hypoxia (HIF-1α). Other genes of interest were the VEGF receptors 2 and 3 linked to angiogenesis and vascular remodelling, basement membrane collagen VII linked to airway remodelling responses in COPD [11] and serotonin receptor 5-HTR2B associated with lung fibrosis [12]. We hypothesized that differences observed in gene and protein expression, related to cellular stress, inflammation and remodelling in COPD, are induced by hypoxia exposure in healthy fibroblasts which may give an increased understanding how hypoxia could be an initiator or driver of pathological alterations observed in COPD. Changes in measured markers related to hypoxia exposure may be useful as biomarkers of disease onset or progression. We also hypothesized that the response to hypoxia and profibrotic stimuli would be different between lung fibroblasts obtained from healthy subjects and COPD patients. Our findings indicate that hypoxia and profibrotic stimuli induced cellular responses and altered inflammatory profile with fibroblasts from COPD patients being less responsive compared to control subjects.
Materials & methods
Patient material
Primary distally derived human lung fibroblasts were obtained after isolation from the alveolar regions from either explants from healthy subjects intended to be used for lung transplantation (donor lungs), or patients with very severe COPD (GOLD IV) subjected to lung transplantation. In addition, lung resection tissue was obtained from distal areas of tumour sites from smokers and patients with well-characterised moderate COPD (GOLD II), see Table 1 for detailed info. There was no information available if the COPD patients were diagnosed with pulmonary hypertension. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Regional Ethical Review Board in Lund, Sweden (FEK 2015/891) and the Swedish Research Ethical Committee in Gothenburg (FEK675–12/2012) and performed in accordance with guidelines approved by the ethical committees. Written informed consent was obtained from the closest relatives of healthy lung donors and from patients included in the study.
Culture of primary human lung fibroblasts
Distally-derived lung fibroblasts were obtained from alveolar parenchymal specimens. The tissue was collected 2–3 cm from the pleura in the lower lobes, i.e. from the same location as where transbronchial biopsies were taken. Vessels and small airways were removed from the peripheral lung tissues and the remaining tissues were chopped into small pieces. Parenchymal pieces from explants were allowed to adhere to the plastic of cell culture flasks for 4 h before addition of Dulbecco’s modified eagle medium (DMEM) GlutaMAX™ (Gibco™, Thermo Scientific, Cat# 10,566,016, Waltham, MA, USA) supplemented with 10% FetalClone III serum (FCIII, HyClone Laboratories, Cat# SH30109.03, Marlborough, MA, USA), 1 mM sodium pyruvate (Stock 100 mM, Sigma-Aldrich, Cat# S8636, Darmstadt, Germany), 2.5 mg/mL Amphotericin B solution (AmpB, Stock 250 mg/mL, Sigma-Aldrich, Cat# A2942, Darmstadt, Germany) and 0.25 mg/mL Gentamycin (Stock 50 mg/mL, Thermo Fisher, Cat# 15,750,037, Waltham, MA, USA) (complete medium) in a humidified incubator at 37 °C and 10% CO2. The culture flasks were then kept in cell culture medium (DMEM) in 37 °C cell incubators until outgrowth of fibroblasts were observed. Parenchymal fibroblasts were then referred to as distal lung fibroblasts [13]. The primary human distally-derived lung fibroblasts were cultured in Dulbecco’s modified eagle medium (DMEM) GlutaMAX™ (Gibco™, Thermo Scientific, Cat# 10,566,016, Waltham, MA, USA) supplemented with 10% FetalClone III serum (FCIII, HyClone Laboratories, Cat# SH30109.03, Marlborough, MA, USA), 1 mM sodium pyruvate (Stock 100 mM, Sigma-Aldrich, Cat# S8636, Darmstadt, Germany), 2.5 mg/mL Amphotericin B solution (AmpB, Stock 250 mg/mL, Sigma-Aldrich, Cat# A2942, Darmstadt, Germany) and 0.25 mg/mL Gentamycin (Stock 50 mg/mL, Thermo Fisher, Cat# 15,750,037, Waltham, MA, USA) (complete medium) in a humidified incubator at 37 °C and 10% CO2. Cells were passaged upon confluency and cell culture medium was exchanged every 3 days.
Hypoxia exposure of primary human lung fibroblasts
Cells were seeded at a density of 15–30 × 104 cells/well in 2 mL complete medium in 6-well plates (Nunclon Delta Surface, Thermo Scientific Waltham, MA, United States) and cultured at 37 °C with 10% CO2 until approximately 70–80% confluency. Cells were then starved with supplemented DMEM GlutaMAX™ medium containing 0.4% FC III in a humidified incubator at 37 °C and 10% CO2 for 2 h. Medium was then changed to new starvation medium with or without addition of 10 ng/mL of profibrotic TGF-β1 (R&D Systems, Cat# 240-B, Minneapolis, MN) 10 min before hypoxia or normoxia exposure. Plates for hypoxia exposure were placed in a hypoxic chamber [model CO2-O2 UNIT-BL (0–20, 1–95), Okolab, Ottaviano, NA, Italy] set to 37 °C, 90% humidity, 1% O2 and 10% CO2 and the other plates were placed in a humidified incubator with normoxic standard culture conditions (37 °C, 21% O2, 10% CO2) for either 4–24 h, as previously described in Berggren-Nylund et al [14]. After the exposure, the supernatant was immediately collected for further analysis and the cell layer was collected to either mRNA analysis or protein analysis and stored at -80 °C. All the exposure studies were performed in passage 3–6.
Total protein amount in cell cultures
To collect cells for protein analysis, 100 mL NP-40 lysis buffer (Thermo Fisher, Cat# FNN0021, Waltham, MA, USA) containing 1% protease inhibitor (Sigma-Aldrich, Cat# P8340, Darmstadt, Germany) was added to the cells. The cells were scraped off and the samples were centrifuged at 10.000 rcf at 4 °C for 10 min. The supernatant was collected and stored at -80 °C. Protein concentrations were determined with Pierce™ BCA Protein Assay Kit (Thermo Fisher Scientific, Cat# 23,225, Waltham, MA, USA) following manufacturer’s instructions.
Gene expression analysis
Ice-cold RLT buffer (0.3 mL) with 1% β-mercaptoethanol was added to the cell layer and total RNA was purified using RNeasy Mini Kit (Qiagen, Cat# 74,106, Hilden, Germany). Cells were then scraped off and a syringe was used to homogenise the sample. Samples were stored at -80 °C until purification. To increase yield of RNA purification using RNeasy Mini Kit, the centrifugation times were increased to 60 s for all washing steps and 3 min for the last washing step. Briefly, RNA samples of the same conditions (normoxia versus hypoxia) were pooled. DNA was removed with RNase-free DNase Set (Qiagen, Cat#79,256, Hilden, Germany). RNA concentration was measured with a NanoDrop. cDNA was synthesised using iScript™cDNA Synthesis Kit (Bio-Rad, Cat# 170–8890, Hercules, CA, USA). The reaction mix was prepared as described in the manufacturer’s instructions and scaled for RNA amounts > 1000 ng. qPCR reaction mixes were prepared using iTaq™ Universal SYBR® Green Supermix (Bio-Rad, Cat# 1,725,124, Hercules, CA, USA) following the manufacturer’s instructions. 25 ng cDNA was added into each well containing 300 nM of each primer. Genes analysed were: DNA damage-inducible transcript 3 protein (CHOP), Nuclear factor erythroid 2-related factor 2 (NRF2), Serine/threonine-protein kinase/endoribonuclease (IRE1), Eukaryotic translation initiation factor 2-alpha kinase 3 (PERK), Cyclic AMP-dependent transcription factor ATF-6 alpha (ATF6), Proteasome subunit alpha type-1 (PSMA1) and beta type-6 (PSMAB6), 26 S proteasome non-ATPase regulatory subunit 11 (PSMD11), Oxidation resistance protein 1 (OXR1), Apoptosis regulator Bcl-2, VEGFR1, VEGFR2, VEGFR3, 5-HTR2B, Collagen 7, HIF-1α, E3 ubiquitin-protein ligase parkin (PARK), Serine/threonine-protein kinase (PINK1), Extracellular superoxide dismutase (SOD3), Transcription factor AP-1 oncogene (c-Jun), Prostaglandin G/H synthase 2 (PTGS2). The housekeeping genes GAPDH, 18 S, β-actin were analysed. Data indicated that GADPH was unstable in the hypoxia experiments and was therefore excluded as housekeeping gene. β-actin and 18 S were both stable during the experimental settings and a geometric mean of these two housekeeping genes was used for all the gene expression analysis. Data is presented as 2^dCT (Ct housekeeping gene – Ct gene of interest). The primer sequences are shown in Additional data 1 Table S1. Ct values of 38 or higher were excluded from the data.
Measurements of cell viability
Cells were cultured in 24-well cell culturing plates and incubated for 4 h, 24–72 h at 37⁰C, 10% CO2 in either hypoxia or normoxia. Cell medium was collected and analysed for cytotoxicity using Lactate Dehydrogenase Activity Assay Kit (Roche, Cat. No. 11 644 739 001, Basel, Switzerland) and the manufacturer’s instructions were followed. Cells treated with 1% Triton-X100 were used as a positive control for cell death. The cell culture plates with cells prepared for the LDH assay were further analysed for metabolic activity using a Water-soluble tetrazolium salt 1 (WST-1) test (Roche, 11 644 807 001). Remnants of cell medium were removed and 10% WST-1 medium/well were added. Plates continued exposure to hypoxic or normoxic conditions for 1 h. Absorbance of cell culture medium was measured in a microplate reader at 440 nm and 620 nm (as reference).
Measurements of growth factors and inflammatory mediators
The release of several cytokines and growth factors were analysed in cell culture medium from cells exposed to 24 h normoxic or hypoxic conditions with Bio-Plex Pro Human Cytokine assay according to the manufacturer’s instructions (Bio-Rad, Cat# 12,007,283, Hercules, CA, USA). The following cytokines were analysed: monocyte chemotactic protein-1 (MCP-1), interleukin (IL)-6, IL-8, fibroblast growth factor-basic (FGF-basic, also known as FGF-2), hepatocyte growth factor (HGF), Regulated upon Activation, Normal T Cell Expressed and Secreted (RANTES) and tumour necrosis factor (TNF)-alpha. The calibration curves were fitted using a five-point regression model and the results were evaluated in the Bio-Plex Manager Software 6.0 (Bio-Rad). The lower limit of quantification was 1.4 (IL-6), 3.0 (IL-8), 2.6 (MCP-1), 0.12 (RANTES), 1.9 (FGF basic) and 7.6 (HGF) pg/mL, respectively.
VEGF-A and VEGF-C were analysed in the cell culture medium using Human VEGF-A Quantikine ELISA kit and Human VEGF-C Quantikine ELISA kit DVC00 (both from R&D Systems, Minneapolis, MN, United States), according to manufacturer’s instructions. The absorption was measured at 450 and 570 nm (as reference). The lower detection limit of quantification was 7.8 pg/mL for VEGF-A and 55 pg/mL for VEGF-C. Prostacyclin and prostaglandin E2 (PGE2) were analysed using 6-keto Prostaglandin F1α (a stable metabolite of prostacyclin) ELISA Kit (Cayman Chemical, Cat# 515,211, Ann Arbor, MI, USA) and PGE2 ELISA Kit – Monoclonal (Cayman Chemical, Cat# 514,010, Ann Arbor, MI, USA) following the manufacturer’s instructions. The absorbance was measured at 415 nm with a microplate reader. The assay detection limit for PGF1α was 1.6 pg/mL and PGE2 was 7.8 pg/mL. Total amount of released mediator was normalized to total protein amount for each individual sample.
Immunocytochemistry staining
Fibroblasts were cultured (10 000 cells/well) in chamber slides (ThermoFisher Scientific, 177,399) with four wells /slide. The slides were cultured for 24 h in either hypoxia or normoxia. The cells were fixed in 4% formaldehyde solution for 15 min at room temperature. Cells were washed in D-PBS and stored at 4⁰C. For HIF-1α staining, cells were permeabilized for 5 min with Triton-X100 0.2% in PBS. The following primary antibodies were used: HIF-1α (dilution 1:50, Biotin, ab81633), HIF-2α (dilution 1:100 Novus Biologicals, Bio-Techne, #NB100-132), 5HTR2B (dilution 1:300, Aviva System Biology, OAAF02801), VEGFR2 (dilution 1:200, Bio-rad, AHP-1327), VEGFR3 (dilution 1:200, Abcam, GR3217142-6) and negative control (Dako, X0903), all diluted in 1% BSA in TBS. Slides were incubated without light exposure at room temperature for 90 min. Slides were washed in TBS for 2 × 5 min and thereafter incubated for 45 min with the secondary antibody (dilution 1:200, anti-rabbit, Cy3 conjugated, Life technologies, A21428) supplemented (separately) with 4′,6-diamidino-2-phenylindole (DAPI; 1:500) for nuclear staining. Slides were washed for 2 × 5 min in TBS and mounted with fluorescence mounting medium (Dako). Slides were stored at 4⁰C until microscopy analysis. Fluorescence images were obtained with an automated slide scanner (Olympus VS-120 S, Olympus, VS120-L100-FL080, Hamburg, Germany) in the DAPI, Cy5 and FITC or Cy3 channel. The HIF-2α stainings were quantified with QuPath v0.4.4 [15] with which a threshold of 3000 maximum pixel intensity within the whole cell body (both cytoplasm and nucleus) was set to determine number of positive cells. The percentages of positive cells were then compared, and statistics were run with Graphpad Prism (repeated measures ANOVA for paired comparisons and two-way ANOVA for unpaired comparisons). Images were processed in OlyVia 2.9.1 (Olympus, Hamburg, Germany), by adjusting the signal intensity through gating to remove autofluorescence and background, and to allow for comparisons between slides. The same gating for the signal was applied to correlated images.
Statistical analysis
All statistical analyses were performed using the software GraphPad Prism 9.3.1 (San Diego, USA). Data are presented as individual values with median. Statistical analyses were performed with one-way or two-way repeated measurements (RM) ANOVA followed by post-hoc test (Fisher’s LSD) using the software GraphPad Prism 9.1.2 (San Diego, USA). A p-value below 0.05 (p < 0.05) was statistically significant.
Results
Experimental settings of hypoxic conditions in healthy primary lung fibroblasts
A pilot study was first conducted in primary healthy distally-derived lung fibroblasts. Different oxygen concentrations (1%, 2% or 5% O2), serum concentrations (0.4%, 1% or 2%) in the culture medium and time points (4 h, 24 h, 48 h and 72 h) were evaluated for the settings for hypoxia exposures in primary healthy lung fibroblasts (Additional data file 2, Figure Supplement 1a-l). Based on these experiments, we set hypoxia exposure to 1% oxygen, exposure time to 4 h and 24 h and cell medium containing 0.4% serum for following experiments with primary lung fibroblasts.
Effects of hypoxia on gene expression in distal lung fibroblasts from COPD and healthy
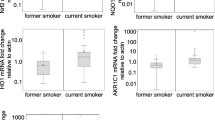
Alterations in gene expression after hypoxia exposure (1% O2) was investigated using RT-qPCR. As we could not detect any significant differences in gene expression between fibroblasts from non-smokers and former smokers or fibroblasts from COPD patients with GOLD II and GOLD IV, the gene expression results were grouped as healthy vs. COPD. After 4 h of hypoxia exposure there were increased expression of 5-HTR2B (p = 0.023, Fig. 1b), Collagen7 (p = 0.027, Fig. 1c), IRE1 (p = 0.019, Fig. 1d), SOD3 (p = 0.021, Fig. 1g), and c-Jun (p = 0.005, Fig. 1h) and a decrease in expression of HIF-1α (p = 0.036, Fig. 1f) in fibroblasts from control subjects, whereas there was an increase in expression of VEGFR2 (p = 0.035, Fig. 1a) in fibroblasts from COPD patients. We also investigated if there was a difference in gene expression between fibroblasts from control subjects and COPD patients at normoxic conditions and after 4 h of hypoxia exposure. We found that at hypoxia, the mRNA expression of 5-HTR2B (p = 0.043, Fig. 1b) and IRE1 (p = 0.062, Fig. 1d) was expressed at lower levels in COPD patients compared to control subjects. There was a tendency for increased VEGFR2 expression (p = 0.084, Fig. 1a) in fibroblasts from COPD patients compared to control subjects at hypoxic conditions and a tendency for decreased HIF1α (p = 0.066, Fig. 1f) in fibroblasts from COPD patients at normoxic conditions compared to control subjects. Several other genes were investigated but the differences were not significantly altered (Additional data 3, Figure Supplement 2).
Effect of 4 h of hypoxia exposure on gene expression levels. Genes related to remodelling: VEGFR2 (a), 5-HTR2B (b) and Collagen7 (c); cellular stress: IRE1 (d) and c-Jun (h), oxidative stress: Nrf2 (e), HIF-1α (f) and SOD3 (g) were measured by RT-qPCR in primary distal lung fibroblasts obtained from healthy subjects (n = 7) and COPD patients (n = 7) after 4 h of exposure to normoxic (21% O2) or hypoxic (1% O2) conditions. Beta-actin and 18 S were used as housekeeping genes. The data is presented as median with interquartile range. Ordinary two-way ANOVA or RM two-way ANOVA were used for unpaired and paired comparisons and the post-hoc test Fisher’s LSD was used for statistical analysis *p < 0.05, **p < 0.01
Hypoxia exposure during 24 h induced an increased expression of Bcl2 (p = 0.007, Fig. 2a) and a decreased expression of Parkin (PARK) (p = 0.023, Fig. 2b) in fibroblasts from healthy subjects. When comparing the expression in lung fibroblasts from healthy subjects and COPD patients there was a higher expression of ATF6 (p = 0.037, Fig. 2c) and a lower expression of SOD3 (p = 0.016, Fig. 2d) and c-Jun (p = 0.039, Fig. 2e) in COPD patients at hypoxic conditions. There were also tendencies for lower expression of SOD3 (p = 0.077, Fig. 2d) and c-Jun (p = 0.068, Fig. 2e) in lung fibroblasts from COPD patients compared to controls at normoxic conditions. Several other genes were investigated but the differences were not significantly altered (Additional data 4, Figure Supplement 3).
Effects of 24 h of hypoxia on gene expression levels. Genes related to cell death: Bcl2 (a), metabolic or mitochondrial stress responses: Park (b), cellular stress: IRE1 (c) and c-Jun (e) and oxidative stress: SOD3 (d) were measured by RT-qPCR in primary distal lung fibroblasts obtained from healthy subjects (n = 7) and COPD patients (n = 7) after 24 h of exposure to normoxic (21% O2) or hypoxic (1% O2) conditions. Beta-actin and 18 S were used as housekeeping genes. The data is presented as median with interquartile range. Ordinary two-way ANOVA or RM two-way ANOVA were used for unpaired and paired comparisons and the post-hoc test Fisher’s LSD was used for statistical analysis. *p < 0.05, **p < 0.01
Effects of hypoxia and TGF-β exposure linked to remodelling
The levels of several growth factors and inflammatory mediators were investigated after exposure to hypoxia with and without profibrotic stimuli with TGF-β1. The levels of VEGF-A were significantly increased after TGF-β exposure in lung fibroblasts from healthy subjects both at normoxic (p = 0.0087) and hypoxic (p = 0.015) conditions and COPD patients at normoxic (p = 0.015) and hypoxic conditions (p = 0.0047) (Fig. 3a). There was a tendency for increased VEGF-A in hypoxic condition compared to normoxic conditions after TGF-β stimulation (p = 0.076) (Fig. 3a). The levels of VEGF-C were significantly increased after hypoxia in lung fibroblasts from both healthy subjects (p = 0.046) and COPD patients (p = 0.041) (Fig. 3b), whereas stimuli with TGF-β significantly reduced the response to hypoxia in lung fibroblasts from both healthy subjects (p = 0.0323) and COPD patients (p = 0.0064) (Fig. 3b). There were decreased levels of HGF in response to TGF-β stimulation in lung fibroblasts from healthy subjects at normoxic (p = 0.011) and hypoxic conditions (p = 0.0027), and in COPD patients at normoxic (p = 0.0027) and hypoxic (p = 0.009) conditions (Fig. 3c). Additionally, there was a tendency for decreased levels of FGF-basic after TGF-β stimulation in healthy subjects at normoxic (p = 0.088) and hypoxic (p = 0.053) conditions (Fig. 3d).
Effects of hypoxia and profibrotic stimuli on mediators linked to remodelling. Release of the following growth factors vascular endothelial growth factors (VEGF)-A (a), VEGF-C (b), hepatocyte growth factor (HGF), (c) and fibroblast growth factor (FGF)-basic (d) from lung fibroblasts from healthy subjects (n = 6) and COPD patients (n = 6) at normoxic (21% O2) and hypoxic (1% O2) conditions with and without stimuli with transforming growth factor TGF-β1 (10 ng/mL). Total protein levels were used to normalize each sample. The data is presented as median with interquartile range. Ordinary two-way ANOVA or RM two-way ANOVA were used for unpaired and paired comparisons and the post-hoc test Fisher’s LSD was used for statistical analysis. *p < 0.05, **p < 0.01
Effects of hypoxia and TGF-β stimuli linked to inflammation
Lung fibroblasts from COPD patients had significantly higher release of MCP-1 (p = 0.007, Fig. 4c), and tendency towards lower release of RANTES (p = 0.062, Fig. 4d) compared to lung fibroblasts from control subjects at basal conditions (normoxia) (Fig. 4). Stimuli with TGF-β induced higher release of IL-8 (p = 0.023, Fig. 4b) and PGE2 (p = 0.036, Fig. 4f) in lung fibroblasts from COPD patients compared to control subjects at normoxia (Fig. 4). The levels of IL-6 increased after TGF-β stimulation in lung fibroblasts from control subjects at both normoxic (p = 0.018) and hypoxic (p = 0.0008) conditions, and in lung fibroblasts from COPD patients at both normoxic (p = 0.049) and hypoxic (p = 0.013) conditions (Fig. 4a). There was a significant higher level of IL-6 in COPD patients compared to healthy subjects at hypoxic conditions after TGF-β stimuli (p = 0.039) (Fig. 4a). The levels of MCP-1 were decreased after TGF-β stimulation of lung fibroblasts from control subjects at normoxic conditions (p = 0.023) and hypoxic conditions (p = 0.030) in fibroblasts from control subjects, and in fibroblasts from COPD patients at normoxic (p = 0.048) and hypoxic (p = 0.022) conditions (Fig. 4c). The levels of MCP-1 were higher in fibroblasts from COPD patients compared to control subjects at normoxic (p = 0.007) and hypoxic (p = 0.022) conditions (Fig. 4c). Neither hypoxia nor TGF-β induced any significant alterations in RANTES (Fig. 4d). TNF-α levels were decreased after TGF-β stimulation in lung fibroblasts from healthy subjects at normoxic conditions (p = 0.034) and a tendency at hypoxic conditions (p = 0.076), whereas there were no effects of either hypoxia or TGF-β stimuli in lung fibroblasts from COPD patients (Fig. 4e). There was a tendency to reduced release of PGE2 (p = 0.061; Fig. 4f) and a significant decrease in PGF1α levels (p = 0.039; Fig. 4g) after hypoxia exposure in TGF-β stimulated fibroblasts from control subjects.
Effects of hypoxia and profibrotic stimuli on inflammatory mediators. Release of inflammatory mediator interleukin (IL)-6 (a), IL-8 (b), monocyte chemoattractant protein (MCP)-1 (c), Regulated upon Activation, Normal T Cell Expressed and Secreted (RANTES) (d), Tumor necrosis factor (TNF)-α (e), prostaglandin (PG) E2 (f) and PGF1α (g) from lung fibroblasts from healthy subjects (n = 6) and COPD patients (n = 6) at normoxic (21% O2) and hypoxic (1% O2) conditions with and without stimuli with transforming growth factor TGF-β1 (10 ng/mL). Total protein levels were used to normalize each sample. The data is presented as mean with min to max. Ordinary two-way ANOVA or RM two-way ANOVA were used for unpaired and paired comparisons and the post-hoc test Fisher’s LSD was used for statistical analysis. *p < 0.05, **:p < 0.01, ***:p < 0.001
Expression of HIF2α in lung fibroblasts
To investigate the effect of 24 h of hypoxia exposure on the expression of HIF2α, the protein expression was analysed using immunocytochemistry (Fig. 5a-e). The HIF2α positive cells were quantified and comparisons were made between healthy (Fig. 5a and b) versus COPD subjects (Fig. 5c and d) at normoxia versus hypoxia. No differences were found between fibroblasts from control and COPD subjects, but when comparing normoxic and hypoxic conditions a downregulation was found at hypoxic conditions both in healthy (p = 0.0086) and COPD (p = 0.0003) subjects (Fig. 5e).
Immunocytochemistry staining and quantification of HIF-2α. Immunofluorescent staining of HIF-2α in distal lung fibroblasts from healthy (a and b) and COPD (c and d) subjects at normoxic (a and c) and hypoxic (b and d) conditions. The blue stain indicates DAPI and the red stain indicates HIF-2α. Scale bar indicates 200 μm. Quantification of the % positive cells (e). Repeated measures ANOVA was used for paired samples and 2-way ANOVA was used for unpaired samples. **p < 0.01, ***p < 0.001
Discussion
The overall aims of this study were to investigate if distally-derived lung fibroblasts respond to hypoxic conditions and if there were differences in the response between fibroblasts obtained from healthy subjects and COPD patients. Analyses were performed on mRNA and protein levels. We could detect some differences in RNA expression and secretion of mediators due to hypoxia exposure, although hypoxia did not seem to have profound effects on the fibroblasts. We did also show some differences related to disease pathology, such as differential gene expression profiles and inflammatory pathways between healthy subjects and COPD, and varying responses of fibroblasts to hypoxia between healthy subjects and COPD patients. In general, the present study imply that lung fibroblasts are less responsive to hypoxia exposure compared to epithelial cells, as hypoxia exposure in our previous study on bronchial and alveolar epithelial cells induced several alterations in stress related genes and release of inflammatory mediators and growth factors [14]. These observed differences in response to hypoxia are probably related to the localisation in the lung tissue as mesenchymal cells are not exposed to oxygen in the same degree as the epithelial cells.
Changes related to oxidative stress and ER stress
We evaluated if hypoxia could affect downstream signalling related to oxidative stress as oxidative stress is linked to COPD pathology [16]. The results show that several genes have a changed expression after exposure to hypoxia primarily in fibroblasts from healthy subjects. After 4 h of hypoxia exposure, fibroblast from healthy subjects showed significantly upregulated expression of IRE1 (UPR), SOD3 (oxidative stress) and c-Jun (cellular stress, apoptosis), while HIF-1α was downregulated. There was a tendency to lower levels of IRE1 after hypoxia exposure in fibroblasts from COPD patients. After 24 h of hypoxia exposure there was a significant higher expression of ATF6 (UPR) and lower expression of SOD3 and c-Jun in fibroblasts from COPD patients compared to healthy subjects. The gene expression data suggests a difference in how lung fibroblasts from healthy compared to COPD patients respond to hypoxia. SOD3 is an extracellular antioxidant and functions as a superoxide anion scavenger limiting inflammation and attenuating oxidative stress by directly binding to and preventing oxidative fragmentation of numerous ECM components, such as type I collagen, heparan sulphate, and hyaluronan [17]. Our obtained results on SOD expression are in line with previous findings in COPD pathology, as a decrease of SOD3 has been related to emphysema. SOD3 attenuated pulmonary emphysema in an in vivo emphysematic mouse models [18] and SOD3 protected against hypoxia-induced pulmonary hypertension in a mouse model with chronic hypoxia [19]. Taken together it has been shown that SOD3 has a protective role both against hypoxia and hallmarks of COPD. We also observed differences in c-Jun which is important for cell proliferation and has anti-apoptotic activity [20]. The gene is regulated by stress stimuli, such as oxidative stress, and it is positively regulated by its own expression [21]. Additionally, c-Jun has been shown to have a role in remodelling and phenotypic shifting in the form of epithelial to mesenchymal transitioning [22]. The reduced expression of SOD3 and c-jun in fibroblasts from COPD subjects after 24 h of hypoxia could indicate that COPD fibroblasts do not proliferate to the same extent and be in a senescent state due to reduced anti-apoptotic signalling, as hypoxia increased Bcl2 gene expression in healthy fibroblasts. It is also possible that there is reduced abilities of phenotypic shifting in COPD fibroblasts which could contribute to the remodelling present in COPD [22].
Transcription factor Nrf2 regulates expression of antioxidant genes, and reduced levels were present in COPD lungs [23]. Nrf2 showed protective effects by inducing antioxidant and antiprotease gene transcription in macrophages, but again, a decreased expression of Nrf2 was present in smokers with COPD [24]. However, we could not detect any significant differences in Nrf2 gene expression in lung fibroblasts. Hypoxia has been shown to increase proteostasis in COPD patients [25, 26] and induce related stress pathways [27]. PINK1 is a kinase that phosphorylates proteins and regulates activity of Parkin (PARK) [28]. In the present study fibroblasts from healthy subjects showed a significant decrease of PARK. Parkin is a ubiquitin ligase involved in protection from mitochondrial dysfunction (mitophagy) by labelling proteins for proteasomal degradation in cellular stress responses such as unfolded proteins [29], but the function of its gene is not completely understood. ER stress results in un- and misfolded proteins often caused by oxidative stress. Lungs of smokers and COPD patients experience enhanced oxidative stress [2]. Our obtained data indicates that there is a difference in the hypoxic ER stress response (IRE1 and ATF6) between lung fibroblasts from healthy subjects and COPD patients. In a previous study in mouse fibroblasts, hypoxia induced an unfolded protein response by PERK activation, independent on HIF-1α activation [30]. Weidner et al. showed disrupted ER, Golgi and lysosomal structures in fibroblasts derived from COPD patients compared to healthy individuals [10]. Altogether, our current findings on changes in gene expression related to oxidative stress and ER stress need further investigations.
Changes related to remodelling
Airway and pulmonary vascular remodelling are processes associated with COPD pathogenesis and severity where hypoxia and hypoxaemia has been shown to play an important role in these remodelling processes [4, 31]. Pulmonary hypertension (PH) is very common in endstage COPD) [31, 32]. PH is suggested to be the result of hypoxia associated with COPD and vascular alterations have been shown to often appear before emphysema is even detectable [33]. In the current study, differences related to remodelling as alterations in collagen7, 5HTR2B and VEGF were seen between healthy and COPD fibroblasts. Collagen VII is a crucial basal membrane protein that forms anchoring fibrils and turnover rate of type VII collagen was significantly increased in serum samples from COPD patients [11]. Our results show that levels of Collagen7 mRNA were affected by hypoxia in lung fibroblasts from healthy subjects, where an increase was seen after 4 h and a decrease in 24 h exposure to hypoxia, however, no changes were seen in fibroblasts from COPD patients. 5-HTR2B mRNA levels were significantly increased after 4 h hypoxia exposure in lung fibroblasts from healthy subjects and the expression levels of 5-HTR2B mRNA were lower in COPD patients compared to healthy subjects. 5-HTR2B has previously been shown to be upregulated in pulmonary fibrosis [12, 34], suggesting that the opposite may occur in COPD. Our results showed very low expression of VEGFRs on protein and mRNA level in fibroblasts, which seemed to be differently affected by hypoxia in disease. Basal VEGFR2 mRNA levels appeared to be higher in COPD patients compared to healthy. Previous immunocytochemistry staining has shown that distally derived lung fibroblasts from healthy individuals and patients with GOLD IV express all three VEGFRs [6]. VEGFR1 and VEGFR2 have predominantly been reported to be expressed by endothelial cells, while VEGFR3 is expressed on lymph vessels. In these cell types, all receptors were shown to be upregulated after hypoxia [35]. Studies also reported an increase of VEGF and VEGFR2 expression in COPD that was positively correlated with HIF-1α and associated with disease severity [3]. Another study showed that the response to hypoxia relating HIF-1 and subsequent VEGF expression was lower in COPD patients compared to healthy controls (non-smokers and smokers) [36]. However, our obtained data show that VEGF-C, but not VEGF-A, is increased by hypoxia in the fibroblasts (both in healthy and diseased). Our data show an increase of VEGF-A, but not VEGF-C, in fibroblasts in response to TGF-β1, whereas the hypoxia-induced release of VEGF-C was decreased by TGF-β, indicating that the VEGF isoforms are regulated in different ways in the fibroblasts. Upregulation of both VEGF-A and VEGF-C expression has been detected in lung donor grafts [37]. VEGF-C is important for lymphangiogenesis but also involved in vascular remodelling and could be a potential biomarker as VEGF can be measured in serum samples. The role of VEGF-C in different stages and phenotypes of COPD is however less described and remains to be further explored. Morfoisse et al. has previously shown in a tumour model that VEGF-C expression was increased during hypoxic conditions, however the transcription was not induced via HIF-1α [38]. In our current study profibrotic stimuli with TGF-β decreased response to hypoxia in both VEGF-C and HGF levels in lung fibroblasts from both COPD patients and healthy subjects. HGF have shown anti-apoptotic effects on epithelial and endothelial cells [39] and that HGF induces apoptosis and prevents accumulation of myofibroblasts in experimental lung fibrosis, while in vitro studies have shown that HGF is involved in the regulation of TGF-β and inhibits epithelial-mesenchymal transitions [40]. Both VEGF and HGF levels have been shown to be reduced in COPD patients, which may further contribute to emphysema in the lung parenchyma [41].
Changes related to inflammation
The inflammatory markers IL-6, IL-8 and MCP-1 are recognised as drivers in pulmonary fibrosis but also in COPD pathology [42]. In the present study, MCP-1 was the only cytokine that was significantly increased in fibroblasts from COPD patients, whereas there was a tendency towards lower release of RANTES at normoxia (basal conditions). Hypoxia had in general no effect on the release of inflammatory mediators. Stimuli with TGF-β induced a significantly increased release of IL-8 and PGE2 in COPD fibroblasts compared to healthy fibroblasts, whereas increased IL-6 and decreased MCP-1 levels were observed in both COPD and healthy fibroblasts. Hypoxia exposure alone without TGFβ stimuli had in general no significant effect on the release of inflammatory cytokines. The combination of hypoxia and TGF-β induced significantly higher release of IL-6 in COPD fibroblasts compared to healthy fibroblasts. In our previous study on epithelial cells, hypoxia and TGF-β1 stimuli increased the release of IL-6 and MCP-1 in bronchial epithelial cells and IL-6 in alveolar epithelial cells [14]. MCP-1 plays a role in antiviral immune response and regulates infiltration and migration of innate immune cells. MCP-1 has been found to be increased in sputum [43] and blood from COPD subjects [44]. This matches the increased levels of MCP-1 found in our study in lung fibroblasts from COPD subjects and is logical since one of the characteristics of COPD is inflammation. Previous studies in endothelial cells have seen an increased release of IL-6 and IL-8 in response to hypoxia [45]. Both IL-6 and IL-8 have been shown to be increased in fibroblasts from COPD patients [46]. These findings overlap partly with our obtained data where we found higher levels in COPD fibroblasts, but only after profibrotic stimuli. Both IL-6 and IL-8 are cytokines with multiple proinflammatory functions and an increased level of these are expected in inflammatory diseases such as COPD. The response to profibrotic stimuli was however similar in lung fibroblasts from control and COPD subjects., indicating that the response to TGF-β is not impaired in COPD, though the profibrotic stimuli had the potential to induce or exasperate differences both between healthy and COPD (as seen in IL-6, IL-8, and PGE2), and between normoxia and hypoxia (as seen in PGF1α). As hypoxia had limited effects on the release of inflammatory markers there is a possibility that some of these markers need more than one kind of stimuli to be induced in lung fibroblasts. RANTES is a chemokine that attracts several different kinds of immune cells. There is only limited literature on RANTES in COPD, but it has been shown to be increased during viral induced exacerbations [47]. In this study we have seen a tendency for lower levels of RANTES in lung fibroblasts from COPD patients, which is in contrast to what has been found in sputum, where no difference could be found [48]. The difference between the results could be explained by the different cell types investigated and in vitro versus in vivo conditions. Altogether, this data indicate that hypoxia may aggravate inflammatory responses that are already present in COPD patients.
Expression of HIF-2α
Immunocytochemistry staining of lung fibroblasts have revealed the presence of HIF-2α both at normoxia and hypoxia in lung fibroblasts from both healthy and COPD subjects. This is, to our knowledge, the first time HIF-2α expression has been investigated in hypoxia stimulated distal lung fibroblasts from human subjects. In this study we have found the expression of HIF-2α to be decreased after 24 h hypoxia (1% O2). This is in contrast to human lung and pulmonary artery adventitial fibroblasts which have been shown to have an upregulation of HIF-2α under similar conditions [49, 50]. This disparity could be due to differences between central vs. distally derived fibroblasts [13]. In a previous study in human alveolar epithelial cells we also detected an upregulation of HIF-2α after exposure to hypoxia (1% O2) [14]. It has been shown that the expression levels of HIF-2α is different in different cell types and different organs in rats [51] which also may be the case in the human lung. The same study also found a downregulation of HIF-2α protein in the lung after 12 h. This is in line with what we have found in this study and indicates that the HIF-2α response in the lung probably occurs at an earlier timepoint than in other tissues. This could be due to the lung being the main organ for oxygen exchange and thereby more sensitive to hypoxia. Additionally, HIF-2α has been shown to regulate genes that are also regulated by HIF-1α [52]. Mizuno et al. have shown lower levels of HIF-1α and VEGF in patients with severe COPD, classified by the Global Initiative for COPD [53], indicating impairment of lung maintenance programs. In our study we did not found statistical differences in the expression of HIF-2α between lung fibroblasts from healthy and COPD subjects, which could indicate that this pathway is not impaired in fibroblasts from COPD subjects, but further research in the area is warranted.
Strengths and limitations of the study
Fibroblasts have often been studied in association to disease pathogenesis related to remodelling, however not much is known about these cells in COPD patients. As there is limited data published on hypoxia and fibroblasts and especially distally derived lung fibroblasts from COPD patients, we were intrigued how this cell type would respond to hypoxia exposure, mimicking on episode which could occur during an exacerbation with increased airflow limitations, and if there would be differences in response between healthy and COPD. This study used primary human material, which is more representative of real disease than cell lines, as it includes heterogeneity between patient groups and individuals. However, this study investigated a limited number of patients with moderate or very severe COPD to compare potential differences between disease stages of COPD. As this study provided some interesting findings, future studies should include more individuals within the different GOLD stages. In the current study we analysed gene expression after 4 h and both gene expression and protein levels after 24 h. Alterations in gene expression could have appeared at other time points that we were not able to detect due to unstable or degraded mRNA. Furthermore, it would be interesting to investigate whether some anti-fibrotic or anti-angiogenic drugs that act on VEGF signalling pathways could induce responses of healthy fibroblasts in COPD patients upon treatment, or vice versa, to model COPD.
Conclusions
Our obtained data in this study provide insights into different expression profiles associated with stress responses and remodelling processes during hypoxic and normoxic conditions, as alterations in gene expression of c-jun, SOD3, IRE, 5HTR2B, VEGFR2 and collagen7 in fibroblasts from control subjects and COPD patients. Our primary findings indicate decreased response to hypoxia in regulation of 5-HTR2B and IRE1 gene expression, increased release of MCP-1 and VEGF-C in COPD fibroblasts and that profibrotic stimuli resulted in higher IL-8 and PGE2 release in COPD fibroblasts. These results give information about altered responses in lung fibroblasts from COPD patients and may contribute towards improved understanding of the heterogeneity of COPD pathology. Our findings indicate that hypoxia and profibrotic stimuli induced cellular responses with altered inflammatory profile with fibroblasts from COPD patients being less responsive to hypoxia compared to control subjects. Since both hypoxia and inflammation are common in the disease this constant environment of stress could desensitize the lung fibroblasts to external stimuli.
Data availability
The data will be supplied upon request to corresponding authors.
Abbreviations
- ATF6:
-
Cyclic AMP-dependent transcription factor ATF-6 alpha
- c-Jun:
-
Transcription factor AP-1 oncogene
- CHOP:
-
DNA damage-inducible transcript 3 protein
- COPD:
-
Chronic obstructive pulmonary disease
- ECM:
-
Extracellular matrix
- FGF-2:
-
Fibroblast growth factor-basic
- HGF:
-
Hepatocyte growth factor
- HIF:
-
Hypoxia-inducible factor
- IL:
-
Interleukin
- IRE1:
-
Serine/threonine-protein kinase/endoribonuclease
- MCP-1:
-
Monocyte chemotactic protein-1
- NRF2:
-
Nuclear factor erythroid 2-related factor 2
- OXR1:
-
Oxidation resistance protein 1
- PERK:
-
Eukaryotic translation initiation factor 2-alpha kinase 3
- PGE2:
-
Prostaglandin E2
- PINK1:
-
Serine/threonine-protein kinase
- PSMA1:
-
Proteasome subunit alpha type-1
- PSMB6:
-
Proteasome subunit beta type-6
- PSMD11:
-
26 S proteasome non-ATPase regulatory subunit 11
- PTGS2:
-
Prostaglandin G/H synthase 2
- RANTES:
-
Regulated upon Activation, Normal T Cell Expressed and Secreted
- SOD3:
-
Extracellular superoxide dismutase
- TGF-β1:
-
Transforming growth factor-beta 1
- TNF:
-
Tumour necrosis factor
- UPR:
-
Unfolded protein response
- VEGF:
-
Vascular endothelial factor
- WST-1:
-
Water-soluble tetrazolium salt 1
References
Yang IA, Jenkins CR, Salvi SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. 2022;10(5):497–511.
Barnes PJ. Oxidative stress-based therapeutics in COPD. Redox Biol. 2020;33:101544.
Fu X, Zhang F. Role of the HIF-1 signaling pathway in chronic obstructive pulmonary disease. Exp Ther Med. 2018;16(6):4553–61.
Harkness LM, Kanabar V, Sharma HS, Westergren-Thorsson G, Larsson-Callerfelt AK. Pulmonary vascular changes in asthma and COPD. Pulm Pharmacol Ther. 2014;29(2):144–55.
Eapen MS, Hansbro PM, Larsson-Callerfelt AK, Jolly MK, Myers S, Sharma P, et al. Chronic obstructive Pulmonary Disease and Lung Cancer: underlying pathophysiology and New Therapeutic modalities. Drugs. 2018;78(16):1717–40.
Westergren-Thorsson G, Bagher M, Andersson-Sjoland A, Thiman L, Lofdahl CG, Hallgren O, et al. VEGF synthesis is induced by prostacyclin and TGF-beta in distal lung fibroblasts from COPD patients and control subjects: implications for pulmonary vascular remodelling. Respirology. 2018;23(1):68–75.
Larsson-Callerfelt AK, Hallgren O, Andersson-Sjoland A, Thiman L, Bjorklund J, Kron J, et al. Defective alterations in the collagen network to prostacyclin in COPD lung fibroblasts. Respir Res. 2013;14:21.
Burgess JK, Mauad T, Tjin G, Karlsson JC, Westergren-Thorsson G. The extracellular matrix - the under-recognized element in lung disease? J Pathol. 2016;240(4):397–409.
Kranenburg AR, de Boer WI, Alagappan VK, Sterk PJ, Sharma HS. Enhanced bronchial expression of vascular endothelial growth factor and receptors (Flk-1 and Flt-1) in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(2):106–13.
Weidner J, Jarenbäck L, Åberg I, Westergren-Thorsson G, Ankerst J, Bjermer L et al. Endoplasmic reticulum, Golgi, and lysosomes are disorganized in lung fibroblasts from chronic obstructive pulmonary disease patients. Physiol Rep. 2018;6(5).
Sand JMB, Lamy P, Juhl P, Siebuhr AS, Iversen LV, Nawrocki A, et al. Development of a Neo-epitope Specific Assay for Serological Assessment of Type VII collagen turnover and its relevance in Fibroproliferative disorders. Assay Drug Dev Technol. 2018;16(2):123–31.
Lofdahl A, Wenglen C, Rydell-Tormanen K, Westergren-Thorsson G, Larsson-Callerfelt AK. Effects of 5-Hydroxytryptamine class 2 receptor antagonists on Bronchoconstriction and Pulmonary remodeling processes. Am J Pathol. 2018;188(5):1113–9.
Hallgren O, Nihlberg K, Dahlback M, Bjermer L, Eriksson LT, Erjefalt JS, et al. Altered fibroblast proteoglycan production in COPD. Respir Res. 2010;11(1):55.
Berggren-Nylund R, Ryde M, Lofdahl A, Ibanez-Fonseca A, Karedal M, Westergren-Thorsson G, et al. Effects of hypoxia on bronchial and alveolar epithelial cells linked to pathogenesis in chronic lung disorders. Front Physiol. 2023;14:1094245.
Bankhead P, Loughrey MB, Fernandez JA, Dombrowski Y, McArt DG, Dunne PD, et al. QuPath: open source software for digital pathology image analysis. Sci Rep. 2017;7(1):16878.
Kirkham PA, Barnes PJ. Oxidative stress in COPD. Chest. 2013;144(1):266–73.
Manni ML, Oury TD. Significance of polymorphisms in the superoxide dismutase-3 gene in COPD: it’s all about location! COPD. 2010;7(4):237–9.
Yao H, Arunachalam G, Hwang JW, Chung S, Sundar IK, Kinnula VL, et al. Extracellular superoxide dismutase protects against pulmonary emphysema by attenuating oxidative fragmentation of ECM. Proc Natl Acad Sci U S A. 2010;107(35):15571–6.
Tseng V, Ni K, Allawzi A, Prohaska C, Hernandez-Lagunas L, Elajaili H, et al. Extracellular superoxide dismutase regulates early vascular Hyaluronan Remodeling in Hypoxic Pulmonary Hypertension. Sci Rep. 2020;10(1):280.
Wisdom R, Johnson RS, Moore C. c-Jun regulates cell cycle progression and apoptosis by distinct mechanisms. EMBO J. 1999;18(1):188–97.
Angel P, Hattori K, Smeal T, Karin M. The Jun proto-oncogene is positively autoregulated by its product, Jun/AP-1. Cell. 1988;55(5):875–85.
Eurlings IM, Reynaert NL, van de Wetering C, Aesif SW, Mercken EM, de Cabo R, et al. Involvement of c-Jun N-Terminal kinase in TNF-alpha-driven remodeling. Am J Respir Cell Mol Biol. 2017;56(3):393–401.
Hwang JW, Rajendrasozhan S, Yao H, Chung S, Sundar IK, Huyck HL, et al. FOXO3 deficiency leads to increased susceptibility to cigarette smoke-induced inflammation, airspace enlargement, and chronic obstructive pulmonary disease. J Immunol. 2011;187(2):987–98.
Suzuki M, Betsuyaku T, Ito Y, Nagai K, Nasuhara Y, Kaga K, et al. Down-regulated NF-E2-related factor 2 in pulmonary macrophages of aged smokers and patients with chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2008;39(6):673–82.
Balch WE, Sznajder JI, Budinger S, Finley D, Laposky AD, Cuervo AM, et al. Malfolded protein structure and proteostasis in lung diseases. Am J Respir Crit Care Med. 2014;189(1):96–103.
Attaway AH, Bellar A, Mishra S, Karthikeyan M, Sekar J, Welch N, et al. Adaptive exhaustion during prolonged intermittent hypoxia causes dysregulated skeletal muscle protein homeostasis. J Physiol. 2023;601(3):567–606.
Fawcett EM, Hoyt JM, Johnson JK, Miller DL. Hypoxia disrupts proteostasis in Caenorhabditis elegans. Aging Cell. 2015;14(1):92–101.
Kim Y, Park J, Kim S, Song S, Kwon SK, Lee SH, et al. PINK1 controls mitochondrial localization of Parkin through direct phosphorylation. Biochem Biophys Res Commun. 2008;377(3):975–80.
Imai Y, Soda M, Takahashi R. Parkin suppresses unfolded protein stress-induced cell death through its E3 ubiquitin-protein ligase activity. J Biol Chem. 2000;275(46):35661–4.
Koumenis C, Naczki C, Koritzinsky M, Rastani S, Diehl A, Sonenberg N, et al. Regulation of protein synthesis by hypoxia via activation of the endoplasmic reticulum kinase PERK and phosphorylation of the translation initiation factor eIF2alpha. Mol Cell Biol. 2002;22(21):7405–16.
Nathan SD, Barbera JA, Gaine SP, Harari S, Martinez FJ, Olschewski H et al. Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J. 2019;53(1).
Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149).
Karnati S, Seimetz M, Kleefeldt F, Sonawane A, Madhusudhan T, Bachhuka A, et al. Chronic obstructive Pulmonary Disease and the Cardiovascular System: vascular repair and regeneration as a therapeutic target. Front Cardiovasc Med. 2021;8:649512.
Konigshoff M, Dumitrascu R, Udalov S, Amarie OV, Reiter R, Grimminger F, et al. Increased expression of 5-hydroxytryptamine2A/B receptors in idiopathic pulmonary fibrosis: a rationale for therapeutic intervention. Thorax. 2010;65(11):949–55.
Neufeld G, Cohen T, Gengrinovitch S, Poltorak Z. Vascular endothelial growth factor (VEGF) and its receptors. FASEB J. 1999;13(1):9–22.
To M, Yamamura S, Akashi K, Charron CE, Haruki K, Barnes PJ, et al. Defect of adaptation to hypoxia in patients with COPD due to reduction of histone deacetylase 7. Chest. 2012;141(5):1233–42.
Abraham D, Taghavi S, Riml P, Paulus P, Hofmann M, Baumann C, et al. VEGF-A and -C but not -B mediate increased vascular permeability in preserved lung grafts. Transplantation. 2002;73(11):1703–6.
Morfoisse F, Kuchnio A, Frainay C, Gomez-Brouchet A, Delisle MB, Marzi S, et al. Hypoxia induces VEGF-C expression in metastatic tumor cells via a HIF-1alpha-independent translation-mediated mechanism. Cell Rep. 2014;6(1):155–67.
Calvi C, Podowski M, Lopez-Mercado A, Metzger S, Misono K, Malinina A, et al. Hepatocyte growth factor, a determinant of airspace homeostasis in the murine lung. PLoS Genet. 2013;9(2):e1003228.
Crestani B, Marchand-Adam S, Quesnel C, Plantier L, Borensztajn K, Marchal J, et al. Hepatocyte growth factor and lung fibrosis. Proc Am Thorac Soc. 2012;9(3):158–63.
Kanazawa H, Tochino Y, Asai K, Hirata K. Simultaneous assessment of hepatocyte growth factor and vascular endothelial growth factor in epithelial lining fluid from patients with COPD. Chest. 2014;146(5):1159–65.
Burgoyne RA, Fisher AJ, Borthwick LA. The role of epithelial damage in the Pulmonary Immune Response. Cells. 2021;10(10).
Traves SL, Culpitt SV, Russell RE, Barnes PJ, Donnelly LE. Increased levels of the chemokines GROalpha and MCP-1 in sputum samples from patients with COPD. Thorax. 2002;57(7):590–5.
Di Stefano A, Coccini T, Roda E, Signorini C, Balbi B, Brunetti G, et al. Blood MCP-1 levels are increased in chronic obstructive pulmonary disease patients with prevalent emphysema. Int J Chron Obstruct Pulmon Dis. 2018;13:1691–700.
Tamm M, Bihl M, Eickelberg O, Stulz P, Perruchoud AP, Roth M. Hypoxia-induced interleukin-6 and interleukin-8 production is mediated by platelet-activating factor and platelet-derived growth factor in primary human lung cells. Am J Respir Cell Mol Biol. 1998;19(4):653–61.
Zhang J, Wu L, Qu JM, Bai CX, Merrilees MJ, Black PN. Pro-inflammatory phenotype of COPD fibroblasts not compatible with repair in COPD lung. J Cell Mol Med. 2012;16(7):1522–32.
Zhu J, Qiu YS, Majumdar S, Gamble E, Matin D, Turato G, et al. Exacerbations of Bronchitis: bronchial eosinophilia and gene expression for interleukin-4, interleukin-5, and eosinophil chemoattractants. Am J Respir Crit Care Med. 2001;164(1):109–16.
Queiroz CF, Lemos AC, Bastos ML, Neves MC, Camelier AA, Carvalho NB, et al. Inflammatory and immunological profiles in patients with COPD: relationship with FEV 1 reversibility. J Bras Pneumol. 2016;42(4):241–7.
Eul B, Rose F, Krick S, Savai R, Goyal P, Klepetko W, et al. Impact of HIF-1alpha and HIF-2alpha on proliferation and migration of human pulmonary artery fibroblasts in hypoxia. FASEB J. 2006;20(1):163–5.
Rose F, Grimminger F, Appel J, Heller M, Pies V, Weissmann N, et al. Hypoxic pulmonary artery fibroblasts trigger proliferation of vascular smooth muscle cells: role of hypoxia-inducible transcription factors. FASEB J. 2002;16(12):1660–1.
Wiesener MS, Jurgensen JS, Rosenberger C, Scholze CK, Horstrup JH, Warnecke C, et al. Widespread hypoxia-inducible expression of HIF-2alpha in distinct cell populations of different organs. FASEB J. 2003;17(2):271–3.
Hu CJ, Wang LY, Chodosh LA, Keith B, Simon MC. Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation. Mol Cell Biol. 2003;23(24):9361–74.
Mizuno S, Bogaard HJ, Gomez-Arroyo J, Alhussaini A, Kraskauskas D, Cool CD, et al. MicroRNA-199a-5p is associated with hypoxia-inducible factor-1alpha expression in lungs from patients with COPD. Chest. 2012;142(3):663–72.
Acknowledgements
This work was supported by the Swedish Heart-Lung foundation [2020/084, 2021/0382, 2021/0289, 2022/0322, 2022/0847, 2023/0453]; the Swedish Research Council [2020/01375], Lund University Medical Faculty, Region Skane (ALF) 2022-0130, Birgit and Sven Håkan Ohlsson Foundation, the Crafoord foundation and Alfred Österlund foundation.
Funding
This study was funded by the Swedish Heart-Lung foundation [2020/084, 2021/0382, 2021/0289, 2022/0322, 2022/0847, 2023/0453]; the Swedish Research Council [2020/01375], Lund University Medical Faculty, Region Skane (ALF) 2022 − 0130, Birgit and Sven Håkan Ohlsson Foundation, the Crafoord foundation and Alfred Österlund foundation.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
MGR performed experimental work, analyzed and interpreted data, and wrote and revised the manuscript. NM performed experimental work, analyzed data, and wrote the outline of the manuscript. AL contributed to conception, experimental work and analyzed data. OP contributed to experimental work and analyzed data. LB contributed resources and collection of patient material. GWT contributed to resources, interpretation of data, revised the manuscript, responsible for ethical applications and patient material. ET contributed to conception, resources, interpretation of data and revised the manuscript. AKLC made substantial contributions to conception, design, and materials to the work, experiments and acquisition of data, analyses and interpretation of the data, resources and drafted and revised the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Regional Ethical Review Board in Lund, Sweden (FEK 2015/891) and the Swedish Research Ethical Committee in Gothenburg (FEK675–12/2012) and performed in accordance with guidelines approved by the ethical committees. Written informed consent was obtained from the closest relatives of healthy lung donors and from patients included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martin, R., Nora, M., Anna, L. et al. Altered hypoxia-induced cellular responses and inflammatory profile in lung fibroblasts from COPD patients compared to control subjects. Respir Res 25, 282 (2024). https://doi.org/10.1186/s12931-024-02907-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02907-x