Abstract
Objective
To investigate the association of serum anti-Jo-1 antibody levels with the disease activity and prognosis in anti-Jo-1-positive patients with antisynthetase syndrome (ASS).
Methods
This study included 115 anti-Jo-1-positive patients with ASS who were admitted to China-Japan Friendship Hospital between 2009 and 2019. Anti-Jo-1 antibody serum levels at initial admission and follow-up were determined by enzyme-linked immunosorbent assay (ELISA). Global and organ disease activity was assessed at baseline and follow-up according to the International Myositis Assessment and Clinical Studies guidelines.
Results
Among enrolled patients, 70 (60.9%) patients initially presented with interstitial lung disease (ILD), and 46 (40%) patients presented with with muscle weakness at initial admission. At baseline, patients with ILD had lower levels of anti-Jo-1 antibodies than those without ILD (p = 0.012). Baseline anti-Jo-1 antibody levels were higher in patients with muscle weakness, skin involvement, and arthritis (all p < 0.05) compared to those without these manifestations. Baseline anti-Jo-1 antibody levels were positively correlated with skin visual analogue scale (VAS) scores (r = 0.25, p = 0.006), but not with disease activity in other organs. However, changes in anti-Jo-1 antibody levels were significantly positively correlated with the changes in PGA (β = 0.002, p = 0.001), muscle (β = 0.003, p < 0.0001), and pulmonary (β = 0.002, p = 0.013) VAS scores, but not with skin and joint VAS scores. Older age of onset (hazard ratio [HR] 1.069, 95% confidence interval [CI]:1.010–1.133, p = 0.022) and higher C-reactive protein (CRP) levels (HR 1.333, 95% CI: 1.035–1.717, p = 0.026) were risk factors for death.
Conclusion
Anti-Jo-1 titers appear to correlate more with disease activity changes over time rather than with organ involvement at baseline, which provides better clinical guidance for assessing the disease course using anti-Jo-1 levels.
Similar content being viewed by others
Introduction
Antisynthetase syndrome (ASS), a subtype of idiopathic inflammatory myopathies (IIM), manifests as one or more clinical symptoms such as interstitial lung disease (ILD), arthritis, mechanic’s hand, myositis, fever, Raynaud’s phenomenon, and the prominent occurrence of circulating antisynthetase antibodies (ASA) [1,2,3,4]. To date, more than ten ASAs targeting aminoacyl-tRNA synthetases have been reported [5,6,7]. Among them, the first ASA reported in 1980 was anti-histidyl-tRNA synthetase (HisRS), also known as anti-Jo-1 antibody, which was closely associated with ILD and systemic symptoms in patients with ASS [8]. Anti-Jo-1 antibody is also the most common ASA, with a positivity rate of 60–70% in ASS patients [9]. ILD, one of the most common manifestations of ASS, may be the first and sometimes the only feature of ASS [10,11,12,13]. Approximately 79–90% of anti-Jo-1-positive patients with ASS will develop ILD during the course of the disease, which can adversely affect prognosis [14, 15].
Previous studies have demonstrated that HisRS, the target antigen of anti-Jo-1 antibodies, is overexpressed in lung and muscle tissue and that pro-inflammatory His-tRNA synthetase-specific CD4+ T cells are present in the lungs and circulation of these patients. Therefore, HisRS may be involved in the pathogenesis of lung and muscle involvement in ASS [16,17,18]. Furthermore, the levels of anti-Jo-1 antibody have been shown to be associated with the disease activity in ASS patients in cross-sectional and longitudinal analyses [19, 20]. Paradoxically, some studies have suggested that anti-Jo-1 antibody levels are associated with the activity of specific organs (i.e., lungs, muscles, and joints), while others have found no correlation between anti-Jo-1 antibody levels and disease activity [21]. However, the relationship between anti-Jo-1 antibody levels and disease and organ activity has not been fully elucidated, so the exact value of antibody detection levels in disease surveillance remains to be determined.
Therefore, this study aimed to investigate the association between serum levels of anti-Jo-1 antibodies and disease activity and to evaluate the impact of anti-Jo-1 antibody levels on the prognosis of ASS patients.
Methods
Patient enrollment
All patients diagnosed with ASS according to the 2010 Conner’s criteria and also positive for anti-Jo-1 antibodies who were admitted to the Department of Rheumatology and Immunology of China-Japan Friendship Hospital from 2009 to 2019 were included in this study [3].
All patients completed informed consent forms, and the study was approved by the Research Review Committee and the Ethical Review Committee of the China-Japan Friendship Hospital (approval number 2019-SDZL-3). This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Data collection and clinical assessment
Clinical information, including patient demographic data, laboratory test results, and imaging findings, was retrospectively collected at baseline and during follow-up. The diagnosis of ILD was determined based on high-resolution chest computed tomography and abnormal pulmonary function tests [22]. Skin involvement included Mechanic’s hand, Gottron sign, heliotrope sign, and Raynaud’s phenomena. Patients disease activity was assessed at baseline and each follow-up visit. The global and organ disease activities were assessed using Core Set Measures conducted by the International Myositis Assessment and Clinical Studies Group, including the physician’s global assessment (PGA) on 10-cm visual analogue scale (VAS) and pulmonary, muscle, skin, and joint VAS, in all enrolled patients [23,24,25]. The survival status and cause of death were followed up by telephone and medical records, and the follow-up period was defined as the time from diagnosis to the date of death or last visit.
Detection of anti-Jo-1 antibodies
The patients’ sera from the first and follow-up visits were collected and stored at -80 °C. A human Jo-1 quantitative enzyme-linked immunosorbent assay (ELISA) kit (Inova Diagnostics, California, USA) was used to detect the levels of anti-Jo-1 antibodies according to the manufacturer’s instructions, and levels > 15 IU/L were considered positive. Line blot (Euroimmun, Lübeck, Germany) for myositis-specific and myositis-associated antibodies were used to confirm positive anti-Jo-1 antibodies.
Statistical analysis
All statistical analyses were performed using GraphPad Prism 7.0 (GraphPad, San Diego, CA, USA) and SPSS version 26 (IBM Corp., Armonk, NY, USA). Numerical variables are expressed as medians and interquartile ranges, and categorical variables are expressed as numbers and proportions. Differences in non-normally distributed groups of numerical variables were tested using the Mann–Whitney U test, and differences in categorical variables were analyzed using the chi-square or Fisher’s exact test, as appropriate. Spearman’s rank correlation was used to determine cross-sectional correlations. Generalized estimating equations (GEE) were used to analyze longitudinal data. Univariate and multivariate COX analyses were used to analyze risk factors affecting mortality. The area under the receiver operating characteristics (ROC) curve was used to determine the power of the univariate and multivariate Cox models to assess their reliability in predicting risk factors for mortality, and p < 0.05 was considered statistically significant.
Results
Clinical characteristics of anti-Jo-1 autoantibody-positive patients
The study included 115 patients who were positive for anti-Jo-1 on first admission. Anti-Jo-1 antibody positivity was determined by both ELISA and line blot. The enrolled patients were 85 women (73.9%) and 30 men (26.1%), with an age of onset of [52 (41,61; IQR)] years and a disease duration of [9(3,36); IQR] months. At baseline, 70 patients (60.8%) initially presented with ILD, 46 patients (40.0%) with muscle weakness, 46 (40%) with skin involvement, and 58 (50.4%) with arthritis. Based on lung and muscle involvement at baseline, 115 patients included 52 patients (45.2%) with isolated ILD, 28 (24.3%) patients with isolated myositis, 18 (15.7%) patients with both and 17 (14.8%) patients with neither. Anti-Jo-1 antibody levels were as 135 (98,185) U/ml at baseline for all patients. During the course of disease, 112 (97.4%) patients developed ILD, 52 (45.2%) with muscle weakness, 75 (65.2%) with skin involvement, and 64 (55.7%) with arthritis (Table 1).
Association of anti-Jo-1 antibody levels with different organ involvement
When comparing the serum levels of anti-Jo-1 antibody levels at baseline between patients with different symptoms on admission, patients with ILD at baseline had lower levels of anti-Jo-1 antibodies than those without ILD at baseline [122 (94, 167) vs. 158 (113, 200) U/ml, p = 0.012] (Fig. 1A). When comparing anti-Jo-1 levels in the four groups of patients with both ILD and myositis, isolated ILD, isolated myositis, and neither, a statistically significant difference was found only in the isolated myositis and isolated ILD groups [177(124,200) vs. 121(95,155), p < 0.001] (Fig. 1B). Patients with isolated myositis had higher baseline anti-Jo-1 levels than those with isolated ILD [177 (124,200) vs. 121(95,155) U/ml, p = 0.004] (Fig. 1B). Baseline anti-Jo-1 antibody levels were higher in patients with muscle weakness [168(110, 200) vs. 122 (96, 165) U/ml, p = 0.018] (Fig. 1C), skin involvement [153(118, 200) vs. 122 (86, 168) U/ml, p = 0.009] (Fig. 1D), and arthritis [164 (111, 200) vs. 120 (85, 157) U/ml, p = 0.006] (Fig. 1E) compared to those without these manifestations. We also compared anti-Jo-1 levels in ASS with and without anti-Ro52, as well as in treated and treatment naïve patients. There was no difference in anti-Jo-1 antibody levels in patients with and without anti-Ro-52 [139(110,192) vs. 120(82,181), p = 0.112], and treated and treatment naive patients [129(96,182) vs. 136(105,199), p = 0.527] (Supplementary Tables 1 and 2).
The serum levels of anti-Jo-1 in patients with anti-synthetase syndrome. A Anti-Jo-1 levels in patients with and without ILD at baseline [122 (94, 167) vs. 158 (113, 200) U/ml, p = 0.012]; B Anti-Jo-1 levels in patients with isolated ILD [121(95,155)], both ILD and myositis [144(86,195)], isolated myositis [177(124,200)], and neither ILD nor myositis [143(109,180)]; C Anti-Jo-1 levels in patients with and without muscle weakness at baseline[168(110, 200) vs. 122 (96, 165) U/ml, p = 0.018]; D Anti-Jo-1 levels in patients with and without skin involvement on the first admission [153(118, 200) vs. 122 (86, 168) U/ml, p = 0.009]; E Anti-Jo-1 levels in patients with and without arthritis at baseline [164 (111, 200) vs. 120 (85, 157) U/ml, p = 0.006]. *p < 0.05; **p < 0.01
Anti-Jo-1 levels in patients with new development of organ involvement were also analyzed. Anti-Jo-1 levels were higher in patients with new development of skin involvement than those without new development of skin involvement [136 (101, 191) vs. 107 (66, 155) U/ml, p = 0.032], but no statistical difference was found in new development of other organ involvement (Supplementary Figure 1).
Correlation between anti-Jo-1 autoantibody levels and disease activity
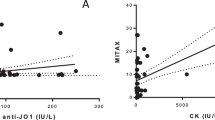
In the overall cohort, the anti-Jo-1 levels were negatively correlated with the age of onset (r =-0.30, p = 0.001). Baseline anti-Jo-1 antibody levels of patients were positively correlated with skin VAS score (r =0.25, p = 0.006), but were not correlated with PGA, muscle, pulmonary, or joint VAS scores. In addition, the baseline anti-Jo-1 antibody levels were positively associated with levels of CK (r = 0.24, p = 0.011), IgG (r = 0.25, p = 0.008), IgM (r = 0.22, p = 0.019), and erythrocyte sedimentation rate (ESR; r = 0.20, p = 0.035). No correlation was found between anti-Jo-1 antibody levels and lung function (Fig. 2).
Correlation matrix of baseline anti-Jo-1 levels, laboratory test results, and disease activity. Spearman’s correlation analysis was used to analyze the correlation between the variables. The numbers in the boxes represent the correlation coefficient between the two variables (red negative, blue positive) when p < 0.05. PGA, Physician’s Global Assessment; VAS, Visual Analog Scale; ALT, alanine aminotransferase; AST, aspartate aminotransferase; LDH, lactic dehydrogenase; CK, creatine kinase; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; %FVC, percent predicted forced vital capacity; %FEV1, percent predicted forced expiratory volume in one second; %DLco, percent predicted carbon monoxide diffusion capacity
The correlation between anti-Jo-1 levels and disease activity in different subgroups were shown in Supplementary Table 3 (with and without ILD and baseline), Supplementary Table 4 (with and without anti-Ro-52) and Supplementary Table 5 (treated and treatment naive), and no significant correlation was found.
Longitudinal correlation between anti-Jo-1 autoantibody levels and disease activity
Ninety-eight of the 115 patients were followed up to survival status, with 1–9 visits. The follow-up disease activity and anti-Jo-1 antibody levels were examined in 43 patients with two or more follow-up visits. The longitudinal correlation between anti-Jo-1 antibody levels and disease activity was further estimated using GEE models. Overall, changes in anti-Jo-1 antibody levels were significantly positively correlated with the changes in PGA (β = 0.002, p = 0.001), muscle (β = 0.003, p < 0.0001), and pulmonary (β = 0.002, p = 0.013) VAS scores, but not with skin and joint VAS scores. Meanwhile, changes in anti-Jo-1 antibody levels were also positively correlated with changes in the levels of AST, CK, IgG, IgM (all p < 0.05) and negatively correlated with changes in the percent predicted forced vital capacity (%FVC; β = -0.025, p < 0.0001), percent predicted forced expiratory volume in one second (%FEV1; β = -0.021, p < 0.0001) (Fig. 3 and Supplemental Table 6).
In patients with ILD at baseline, changes in anti-Jo-1 antibody levels were correlated with changes in PGA, pulmonary, and joint VAS scores; IgG, IgA, IgM, and CRP levels; %FVC; %FEV1; and percent predicted carbon monoxide diffusion capacity (%DLco) (all p < 0.05). Variations in anti-Jo-1 antibody levels were significantly correlated with changes in PGA, muscle, and pulmonary VAS scores; ALT, CK, IgG, and IgA levels; %FVC, and %FEV1 in patients without ILD at baseline (all p < 0.05) (Table 2).
Among 43 patients with two or more follow-up visits, 8 who were anti-Jo-1-positive had more than 3 visits. The variability of anti-Jo-1 antibody and serum CK levels, %FVC, and %DLco over time in these patients showed comparable trends over time in the majority of patients (Fig. 4).
Longitudinal changes of anti-Jo-1 levels in and serum CK levels, %FVC pred, and %DLco pred over time in 8 anti-Jo-1-positive patients with more than 3 times visits. The black dashed line indicates the cut-off line for the normal level of anti-Jo-1 antibodies(15U/ml). Abbreviation: ILD, interstitial lung diseases; CK, creatine kinase; %FVC, percent predicted forced vital capacity; %DLco, percent predicted carbon monoxide diffusion capacity; GCs, corticosteroids steroids; DMARDS, disease-modifying anti-rheumatic drugs; CsA, ciclosporin A; CTX, cyclophosphamide; MMF, mycophenolate mofetil; IVIG, intravenous. immunoglobulin; tac, tacrolimus
Association between anti-Jo-1 antibody levels and prognosis in patients with ASS
A total of 98 anti-Jo-1 positive patients were followed up for 1 month to 118.87 months, and the median follow-up time was 41.89 months. Eleven deaths were observed, including nine from respiratory failure, one from endometrial cancer, and one from malignancies.
Risk factors for mortality in anti-Jo-1 positive patients were analyzed. Univariate analyses showed that older age of onset (HR 1.074, 95% CI: 1.021–1.129, p = 0.006), arthritis at baseline(HR 0.184, 95% CI: 0.039–0.855, p = 0.031), and higher levels of IgA (HR 1.006, 95% CI: 1.001–1.010, p = 0.018) and CRP (HR 1.338, 95% CI: 1.037–1.726, p = 0.025) were risk factors for death in anti-Jo-1-positive patients. Further multivariate Cox regression analysis showed that a higher age of onset (HR 1.069, 95% CI: 1.010–1.133, p = 0.022), and higher CRP levels (HR 1.333, 95% CI: 1.035–1.717, p = 0.026) were risk factors for death in anti-Jo-1-positive patients. Patients who died had an older age of onset [61 (48, 79) vs. 50 (39, 61) years old, p = 0.009] and higher CRP levels [1.55 (0.41, 2.90) vs. 0.43 (0.21, 1.30) mg/dl, p = 0.039] than those who survived. Baseline anti-Jo-1 levels were not risk factors for death in anti-Jo-1-positive patients (p = 0.997) (Table 2). The multivariate cox model, which included age of onset and CRP, showed the best efficacy for predicting death, with the largest area under the ROC curve [0.770(0.625–0.915)] (Supplementary Table 6).
Discussion
This study demonstrated the clinical associations and the prognostic significance of anti-Jo-1 antibodies in patients with ASS. We found that baseline anti-Jo-1 levels were lower in patients with ILD at baseline, but higher in patients with extrapulmonary involvement at baseline. Anti-Jo-1 antibody levels were weakly correlated with disease activity in the cross-sectional analysis and were not related with the final outcome. In addition, a smaller longitudinal subset follow-up analysis showed that anti-Jo-1 levels reflected the disease activity to some extent.
Myositis, ILD, and arthritis are common manifestations of ASS, and the spectrum of symptoms in different patients can be distinct. Previous studies have shown that 51-55.2% of Jo-1-positive patients have ILD at onset, and 82-84% of patients will eventually develop ILD during their clinical course [10, 11, 26]. In this study, we found that anti-Jo-1 levels were higher in patients with muscle weakness, skin involvement, and arthritis, but lower in patients with ILD. A previous study found that patients with dermatomyositis had lower levels of anti-Jo-1 antibody than those with polymyositis (127 vs. 178 IU/l). Although differences in anti-Jo-1 antibody levels in different subgroups were not analyzed, the results seem to suggest that anti-Jo-1-positive patients with different phenotypes have different anti-Jo-1 antibody levels [21].
We found no statistically difference in the proportion of receiving treatment in patients with and without ILD (60% vs. 66.7%, p = 0.471). Thus, ILD patients with lower baseline anti-Jo-1 levels may not be related to whether they receive treatment, which may be related to the differences in antigen levels and antibody types in different tissues. The antigen recognized by the anti-Jo-1 antibody is HisRS, which consists of 509 amino acids and can be divided into three domains: WHEP, internal catalytic domain (CD), and anticodon binding domain (ABD) [27]. Additionally, splice variants of HisRS that skip CD and link the noncatalytic domain, HisRS∆CD, also exist in serum and tissues, with particularly enriched expression in human lung tissue. Recent studies discovered that the serum from anti-Jo-1-positive patients had different affinities for different antigen fragments of HisRS [27]. The anti-Jo-1 antibody ELISA kit we used in this study was a commercial kit coated with a recombinant HisRS full-length (HisRS-FL), which could detect the levels of anti-Jo-1 antibody that react with HisRS-FL. Research by Zhou et al. found that the tissue distribution of HisRS-FL and HisRSWHEP was different, with HisRSWHEP having higher expression in the lung than HisRS-FL, while HisRS-FL was predominantly expressed in muscle, which had very low levels of HisRSWHEP [28]. This may explain the differences in baseline anti-Jo-1 antibody levels in subgroups involving different organs. In patients with muscle damage, exposure to HisRS-FL in muscle tissue induced the production of anti-Jo-1 antibodies, resulting in higher levels of anti-Jo-1 antibodies in patients with muscle weakness. However, anti-Jo-1 antibodies mainly against HisRSWHEP may not be detected by this kit in patients with ILD, and the higher percentage of muscle weakness in the non-ILD subgroup (60% vs. 25.7%, P < 0.0001) may also contribute to the higher levels of anti-Jo-1 antibodies in patients without ILD.
In this study, anti-Jo-1 antibody levels were only weakly correlated with skin VAS scores in the cross-sectional analysis, but no correlation with anti-Jo-1 antibody levels or other organ VAS scores was found. Stone et al. found a modest correlation between the anti-Jo-1 antibody and CK levels and muscle and joint disease activity in a cross-sectional assessment of a cohort of 94 anti-Jo-1-positive patients [13, 21], which is not entirely consistent with the findings of this study. There was also a correlation between anti-Jo-1 antibody levels and some laboratory parameters (CK, IgG, IgM, and ESR). Kryštůfková et al. also found a correlation between the anti-Jo-1 antibody level and levels of CK, AST, and CRP [21]. These findings indicate that cross-sectional anti-Jo-1 antibody levels may not have good correlation with disease activity.
In the follow-up study, changes in anti-Jo-1 levels were correlated with changes in most parameters (PGA, pulmonary, and skin VAS scores; AST, CK, IgG, and IgM levels; and %FVC), and previous studies have shown similar findings. We also found that the spectrum of variables associated with changes in anti-Jo-1 antibody levels differed in different subgroups. Changes in anti-Jo-1 antibody levels were not associated with changes in muscle enzymes but were associated with changes in parameters related to lung disease severity (pulmonary VAS score, %FVC, and %DLco) in patients with ILD at baseline. In addition, changes in anti-Jo-1 antibody levels were correlated with changes in indicators of the severity of muscle damage (muscle VAS score, ALT level, and CK level) in patients without ILD at baseline. This suggests that longitudinal anti-Jo-1 antibody levels may better reflect disease activity in the damaged target organs. The anti-Jo-1 antibody recruits T lymphocytes and damages target organs (lung and muscle), which is one of the reasons for the pathogenicity of Jo-1 antibody-positive ASS [16, 29]. This may explain the correlation between anti-Jo-1 levels and disease activity in the target organs.
Subsequently, we analyzed the risk factors affecting the outcome of anti-Jo-1-positive patients and found that baseline anti-Jo-1 antibody levels were not a risk factor for death. In cross-sectional analyses, we were also unable to find an association between the level of anti-Jo-1 antibodies and the activity of the disease. This suggests that pre-post changes in anti-Jo-1 antibody levels may be more indicative of disease activity than their absolute levels. Therefore, focusing on longitudinal changes in anti-Jo-1 antibody levels may be more important in clinical practice. In addition, an older age of onset and high CRP levels were risk factors for death. In contrast, the main cause of death was ILD-related respiratory failure (9/11, 81.8%). Patients who died had a higher pulmonary VAS score at baseline than those who survived (2.53 ± 0.76 vs. 2.01 ± 0.21, P = 0.043), and pulmonary VAS scores at baseline were positively associated with the age of onset and CRP levels, which may explain why patients with an older age of onset and higher CRP levels had a lower survival rate. Consistent with our results, Wei Jiang et al. also reported that ASS patients over 60 years of age had a lower survival rate [30].
This study had some limitations. First, we determined anti-Jo-1 antibody positivity by ELISA and immunoblotting, but we did not use immunoprecipitation for confirmation. Although it is possible that some individual patients may have had false positives, especially those with low titers, this may not have affected the main conclusions of this study. Second, some patients were treated at enrolment, and the treatment may affect antibody levels and disease status. Finally, our longitudinal association analysis was performed in only a small subset of patients due to data availability, which may have introduced bias.
In conclusion, this study revealed that levels of anti-Jo-1 antibodies were weakly associated with disease activity at the cross-sectional level and with final outcome. However, longitudinal changes of anti-Jo-1 antibody levels reflect the disease activity and may be more strongly associated with disease activity in the major affected organs, which may provide clinicians with more effective guidance in assessing disease progression based on anti-Jo-1 antibody levels.
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Lundberg IE, Fujimoto M, Vencovsky J, Aggarwal R, Holmqvist M, Christopher-Stine L, et al. Idiopathic inflammatory myopathies. Nat Rev Dis Prim. 2021;7:1–22.
Marco JL, Collins BF. Clinical manifestations and treatment of antisynthetase syndrome. Best Pract Res Clin Rheumatol. 2020;34:101503.
Connors GR, Christopher-Stine L, Oddis CV, Danoff SK. Interstitial lung disease associated with the idiopathic inflammatory myopathies: what progress has been made in the past 35. Years? Chest. 2010;138:1464–74.
Muro Y, Yamashita Y, Koizumi H, Ogawa-Momohara M, Takeichi T, Mitsuma T, et al. Two novel anti-aminoacyl tRNA synthetase antibodies: autoantibodies against cysteinyl-tRNA synthetase and valyl-tRNA synthetase. Autoimmun Rev. 2022;21:103204.
McHugh NJ, Tansley SL. Autoantibodies in myositis. Nat Rev Rheumatol. 2018;14:290–302.
Hengstman GJD, Engelen BGM, Van V, Egberts WTM, Van Venrooij WJ. Myositis-specific autoantibodies: overview and recent developments. Curr Opin Rheumatol. 2001;13:476–82.
Vulsteke J-B, Derua R, Dubucquoi S, Coutant F, Sanges S, Goncalves D, et al. Mass spectrometry based identification of new anti Ly and known antisynthetase autoantibodies. Ann Rheum Dis. 2023;82:546–55.
Nishikai M, Reichlin M. Heterogeneity of precipitating ntibodies characterization of the Jo- 1 antibody system. Arthritis Rheum. 1980;23:881–8.
Notarnicola A, Preger C, Lundström SL, Renard N, Wigren E, Gompel E, Van, et al. Longitudinal assessment of reactivity and affinity profile of anti-Jo1 autoantibodies to distinct HisRS domains and a splice variant in a cohort of patients with myositis and anti-synthetase syndrome. Arthritis Res Ther. 2022;24:1–16.
Huang K, Aggarwal R. Antisynthetase syndrome: a distinct disease spectrum. J Scleroderma Relat Disord. 2020;5(3):178–91.
Grau-junyent Trallero-araguásE, Monteagudo-jiménez JM, Fraile-rodriguez M. Clinical manifestations and long-term outcome of anti-Jo1 antisynthetase patients in a large cohort of Spanish patients Study Group and Autoimmune Diseases Study Group (GEAS) of the Spanish Society of. Semin Arthritis Rheum. 2016;46:225–31.
Gallay L, Gayed C, Hervier B. Antisynthetase syndrome pathogenesis: knowledge and uncertainties. Curr Opin Rheumatol. 2018;30:664–73.
Gasparotto M, Gatto M, Saccon F, Ghirardello A, Iaccarino L, Doria A. Pulmonary involvement in antisynthetase syndrome. Curr Opin Rheumatol. 2019;31:603–10.
Marie I, Josse S, Hatron PY, Dominique S, Hachulla E, Janvresse A, et al. Interstitial lung disease in anti – Jo-1 patients with antisynthetase syndrome. Arthritis Care Res (Hoboken). 2013;65:800–8.
Zamora AC, Hoskote SS, Abascal-bolado B, White D, Cox CW, Ryu JH, et al. Clinical features and outcomes of interstitial lung disease in anti-Jo-1 positive antisynthetase syndrome. Respir Med. 2016;118:39–45.
Galindo-Feria AS, Albrecht I, Fernandes-Cerqueira C, Notarnicola A, James EA, Herrath J, et al. Proinflammatory histidyl-transfer RNA synthetase-specific CD4 + T cells in the blood and lungs of patients with idiopathic inflammatory myopathies. Arthritis Rheumatol. 2020;72(1):179–91.
Zack Howard OM, Dong HF, Yang De, Raben N, Nagaraju K, Rosen A, et al. Histidyl-tRNA synthetase and asparaginyl-tRNA synthetase, autoantigens in myositis, activate chemokine receptors on T lymphocytes and immature dendritic cells. J Exp Med. 2002;196:781–91.
Ascherman DP, Oriss TB, Oddis CV, Wright TM. Critical requirement for Professional APCs in eliciting T cell responses to novel fragments of Histidyl-tRNA synthetase (Jo-1) in Jo-1 antibody-positive polymyositis. J Immunol. 2002;169:7127–34.
Miller FW, Twitty SA, Biswas T, Plotz PH. Origin and regulation of a disease-specific autoantibody response. Antigenic epitopes, spectrotype stability, and isotype restriction of anti-jo-1 autoantibodies. J Clin Invest. 1990;85:468–75.
Stone KB, Oddis CV, Fertig N, Katsumata Y, Lucas M, Vogt M, et al. Anti – Jo-1 antibody levels correlate with Disease Activity in Idiopathic Inflammatory Myopathy. Arthritis Rheum. 2007;56:3125–31.
Kryštufková O, Hulejová H, Mann HF, Pecha O, Putová I, Ekholm L, et al. Serum levels of B-cell activating factor of the TNF family (BAFF) correlate with anti-jo-1 autoantibodies levels and disease activity in patients with anti-Jo-1 positive polymyositis and dermatomyositis. Arthritis Res Ther. 2018;20:1–13.
Travis WD, Costabel U, Hansell DM, King TE, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
Sultan SM, Allen E, Oddis CV, Kiely P, Cooper RG, Lundberg IE, et al. Reliability and validity of the myositis disease activity assessment tool. Arthritis Rheum. 2008;58:3593–9.
Rider LG, Werth VP, Huber AM, Alexanderson H, Rao AP, Ruperto N, et al. Measures of adult and juvenile dermatomyositis, polymyositis, and inclusion body myositis. Arthritis Care Res. 2011;63:118–57.
Miller FW. New approaches to the assessment and treatment of the idiopathic inflammatory myopathies. Ann Rheum Dis 2012;71(Supp II):i82–5.
Bartoloni E, Gonzalez-Gay MA, Scirè C, Castaneda S, Gerli R, Lopez-Longo FJ, et al. Clinical follow-up predictors of disease pattern change in anti-Jo1 positive anti-synthetase syndrome: results from a multicenter, international and retrospective study. Autoimmun Rev. 2017;16:253–7.
Xu Z, Wei Z, Zhou JJ, Ye F, Lo WS, Wang F, et al. Internally deleted human tRNA synthetase suggests evolutionary pressure for repurposing. Structure. 2012;20:1470–7.
Zhou JJ, Wang F, Xu Z, Lo WS, Lau CF, Chiang KP, et al. Secreted histidyl-tRNA synthetase splice variants elaborate major epitopes for autoantibodies in inflammatory myositis. J Biol Chem. 2014;289:19269–75.
Levine SM, Raben N, Xie D, Askin FB, Tuder R, Mullins M, et al. Novel conformation of histidyl-transfer RNA synthetase in the lung: the target tissue in Jo-1 autoantibody-associated myositis. Arthritis Rheum. 2007;56:2729–39.
Jiang W, Shi J, Yang H, Tian X, Yang H, Chen Q, et al. Long-term outcomes and prognosis factors in patients with idiopathic inflammatory myopathies based on myositis-specific autoantibodies: a single cohort study. Arthritis Care Res. 2023;75:1175–82.
Acknowledgements
We would like to thank the National High Level Hospital Clinical Research Funding and Natural Science Foundation of Beijing Municipality for their support of our research. We also thank all members of the Department of Rheumatology at China-Japan Friendship Hospital for their help and assistance. We also thank to our patients for their trust in our department and their cooperation in research.
Funding
This work was supported by the National High Level Hospital Clinical Research Funding (2022-NHLHCRF-YS-02), and Natural Science Foundation of Beijing Municipality (No. 7232145).
Author information
Authors and Affiliations
Contributions
HX. Yang, QN. Chen, and C. Sun collected the data, performed the statistical analyses, and drafted the manuscript. QW. Jin and LN. Zhang helped with the collection of the data. QY. Liu helped with the performance of the ELISA. GC. Wang and QL. Peng reviewed the manuscript. X. Lu designed the study, supervised all data analyses, and revised the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients completed informed consent forms, and the study was approved by the Research Review Committee and the Ethical Review Committee of the China-Japan Friendship Hospital (approval number 2019-SDZL-3). And this study was conducted in accordance with the Declaration of Helsinki guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, H., Chen, Q., Sun, C. et al. Clinical and prognostic associations of anti-Jo-1 antibody levels in patients with antisynthetase syndrome. Respir Res 25, 222 (2024). https://doi.org/10.1186/s12931-024-02851-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02851-w