Abstract
Aim
Acute respiratory distress syndrome or ARDS is an acute, severe form of respiratory failure characterised by poor oxygenation and bilateral pulmonary infiltrates. Advancements in signal processing and machine learning have led to promising solutions for classification, event detection and predictive models in the management of ARDS.
Method
In this review, we provide systematic description of different studies in the application of Machine Learning (ML) and artificial intelligence for management, prediction, and classification of ARDS. We searched the following databases: Google Scholar, PubMed, and EBSCO from 2009 to 2023. A total of 243 studies was screened, in which, 52 studies were included for review and analysis. We integrated knowledge of previous work providing the state of art and overview of explainable decision models in machine learning and have identified areas for future research.
Results
Gradient boosting is the most common and successful method utilised in 12 (23.1%) of the studies. Due to limitation of data size available, neural network and its variation is used by only 8 (15.4%) studies. Whilst all studies used cross validating technique or separated database for validation, only 1 study validated the model with clinician input. Explainability methods were presented in 15 (28.8%) of studies with the most common method is feature importance which used 14 times.
Conclusion
For databases of 5000 or fewer samples, extreme gradient boosting has the highest probability of success. A large, multi-region, multi centre database is required to reduce bias and take advantage of neural network method. A framework for validating with and explaining ML model to clinicians involved in the management of ARDS would be very helpful for development and deployment of the ML model.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Acute respiratory distress syndrome (ARDS) is a common complication in adult general intensive care units (ICUs) [1]. In 2016 a survey conducted in 459 ICUs across 50 countries demonstrated that ARDS occurred in 10% of patients with a mortality rate exceeding 40% [1]. The management of ARDS in the US, UK and Europe is largely based on the individual country’s national guidelines. Although these guidelines are created based on nationwide surveys and research studies, the quality of evidence for recommendations for clinical practice is poor with absence of high-quality evidence [2]. This may explain why there is a poor uptake of the guidelines by clinicians. For example, the UK guidelines recommend a low tidal volume of less than 8ml/kg and a positive-end expository pressure (PEEP) of more than 12 cmH2O [2]. However, only about 60% of patients received 8ml/kg of tidal volume or less and more than 82% received less than 12cmH2O PEEP [1]. Huge practice variations are recognised and there is an urgent need for evidence-based and standardised management for ARDS in ICU.
Machine learning (ML) has been applied successfully into other areas including natural language processing, computer vision applications, and automatic speech recognition. As a result, advancement has been made in many areas from sports to robotic, from entertainment to industry. Applications of ML have shown enormous potential across several medical fields such as disease prediction, clinical outcome prediction, diagnosis and prognosis using various data modalities, including time signals and medical imaging [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18].
Although ML has the ability to recognise patterns within large amount of data, many of these patterns are imperceptible by human. These patterns can be used in different ways to categorise or predict events [3]. However, to be successfully integrated into the health care system, ML applications must aim to archive high performance metric such as accuracy and achieve trust from users towards clinical application. As a result, the demand for better transparency in ML models in medicine is essential for better understanding of the causality and relationship between input and output, and for legal and ethical purposes [19,20,21].
The concept of interpretation or explainability in machine learning is defined as the capability of the algorithm to present and/or produce knowledge contained inside the data so that it is perceptible and understandable by users [22]. Various explainability methods have been used in medical care in general [23] and for ARDS data in particular [24]. However, few studies have actually validated the effectiveness of these explainability methods with direct involvement of clinicians [23]. There is also lack of evidence on which method is most suitable for clinicians in terms of its explainability.
The main focus of this review is to identify studies that has used machine learning methods on the management, prognosis and diagnosis of patients with ARDS, reflect on usage of different database and data gathering method, algorithms and their effectiveness. The review also aims to highlight the state of explainability in term of methods and usages, and performance of different ML methods in ARDS.
Method
Inclusion and exclusion criteria
Articles employing machine learning or artificial intelligence addressed directly to the diagnosis, management, risk assessment, prognosis or outcome of ARDS were included in the review. The included articles can utilise existing ML algorithm or create new algorithm based on either classical ML method such as decision tree or more advanced ones like neural network or both. Protocol, commentaries, letters, abstract-only articles, conference proceedings, non-English and non-peer reviewed articles were excluded. Only studies using exclusively human data were selected. Research using paediatric patients was excluded.
Search strategy
An extensive literature search was performed in Pubmed, Google scholar and EBSCO on July 2023. The summary of the screening process is reported in the PRISMA diagram (Fig. 1) A random snowball search was also carried out using Google to identify any additional results. Keywords used for these searches include “acute respiratory distress syndrome”,”ARDS”, “acute lung injury”, “ALI”,”machine learning” and”artificial intelligence”. Boolean Operator “AND” and “OR” was used for Pubmed and EBSCO searches. The reference list of all results was also screened by title and abstract for potentially relevant citations. The list of author contributions to this paper is included.
All the search results were collected using their title and abstract. The full-text version of these results was used for screening using criteria in 2.1. Non-full-text paper was excluded at this stage. This process was carried out independently by TT and MT to eliminate bias and disagreements were resolved with consensus from all authors.
Results
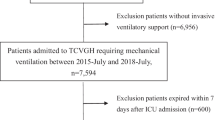
Search results and selection process
Google Scholar search yielded 54 results after preliminary screening. Three non-English articles were excluded along with 2 not yet peer-reviewed results, 1 duplication and 27 irrelevant articles. One duplicated paper was also excluded.
The search was repeated with the EBSCO and Pubmed database, resulting in 88 articles and 85 articles respectively. Finally, 52 articles were selected for review matching all criteria listed in Inclusion and exclusion criteria section (Table 1).
Characteristics of the reviewed studies
Fifty-two articles between 2009 and 2023 were selected. 18 (34.6%) of these focused on prediction of ARDS development in patients during hospitalisation. 14 (26.9%) publications articles were related to diagnostic accuracy. 11 (21.2%) articles were focused on categorizing patients with ARDS into groups or subgroups based on severity or mortality. Five articles were related to the use of ML to predict patient mortality or create more suitable management for patients. There is a single (1.9%) article on the prognosis or health trajectory of ARDS and 1 (1.9%) article on using ML to model the condition of patients with ARDS. This can be seen in (Fig. 2).
In summary, there are 49 different ML systems deployed. The most common algorithm is the random forest with 17 (32.7%) usages. A different variation of gradient boosting algorithms is also very common with 13 (25%) XGBoost, 4 (7.7%) adaboost, and 7 (13.5%) others. Neural networks methods and its variances were also albeit less frequent with 8 (15.4%) neural network (NN), 1 (1.9%) deep neural network (DNN), 2 (3.8%) recurrent neural network (RNN) and 3 (5.8%) convolutional neural network (CNN) for 14 (26.9%) in total. Existed ML-based models were also tested for example ALI sniffer, Dense-Ynet and ResNet-50 (Fig. 3).
The definition and phenotypes of ARDS were defined recently using the Berlin definition and updated in 2023 [76]. Therefore, there were various attempts to establish a more rigorous subphenotype using the ML algorithm over the years. Unsupervised algorithms were used with some success. Sinha [31] used latent class analysis to separate patients into hyper and hypo-inflammatory states. Zhang et al.[38] in 2019 and Liu et al. [53] in 2021 both tried to categorise ARDS patients into 3 subphenotypes using tree-based gradient boosting and k-mean method respectively. Although the ML algorithm has shown great potential to define ARDS subphenotypes, only 6 (50%) out of 12 studies in severity and subphenotype topics used this method.
There has been a surge in ARDS research since 2019 most likely in response to the COVID-19 pandemic. 44 (84.6%) studies were published between 2019 and June 2023 of which 5 are directly used data from Covid patients (Fig. 4).
Supervised ML algorithms are widely used for many applications such as verifying subphenotypes, improving diagnoses, predicting the development of ARDS, potential outcomes and providing insights into the management of ARDS. Across these applications, the gradient boosting method and its variations proved to be very popular, being used in 24 of the studies. 12 (23.1%) articles employed multiple ML algorithms including gradient boosting-type algorithms: gradient boosting and its variations. Among those, Gradient boosting-type algorithms had the best performance in 8 studies (66.7%), for example, Yang [40], Reamaroon [57] and Lazzarini [58]. The most common supervised ML algorithm is random forest used in 17 studies, followed by logistic regression and extreme gradient boosting (XGBoost) in 13 studies.
In term of data used, the most popular data source is from private data collections, which was used in 30 studies (57.7%). Public and large data collections composed the rest of data usage. The most popular public data collection is The Medical Information Mart for Intensive Care (MIMIC) and was used 12 times in two versions 3 [34] and 4 [67] (23.1%). The eICU database [51] is also popular and was used in 9 studies (17.3%). Others notable data sources include the Secure Anonymised Data Linking (SAILS) Databank [42] with 4 appearances and the National Lung, Heart, and Blood Institute ARDS Network (ARMA, ALVEOLI, and FACTT) [46] which was used 10 times across all versions. Even with large data collection like MIMIC and eICU, only 12 (23.1%) studies included more than 5000 samples (Fig. 5). The largest data collection is from the National Trauma Data Bank from the US used by Pearl, et al., [26] with 1,438,035 patients. Barakat, et al., [72] used 1 million simulated patients based on MIMIC 3 database for their study. The simulation method was developed by Sharafutdinov [77]. This approach circumvents the need of cleaning the data, data protection and deidentification and handling missing and inconsistent data. It also allows limitless database in term of data size.
In 14 studies there was an attempt to develop algorithms based on neural network architectures. The developed models based on neural network architecture such as ResNet-50 (CNN) and Dense-Ynet (DNN) were also tested with promising results such as with Jabbour in 2022 [63] and Yahyataba [71] in 2023. However, when competing with non-neural network models in Yang [40] in 2019, Izadi [62] in 2022, Xu [47] in 2021 and Wang [67] in 2023, neural networks showed no advantage in terms of ROC area under the curve (AUC) or accuracy. This might be due to the amount of data available for use in the neural network (Fig. 5), showcased clearly in Lam [66] 2022 study, developing XGBoost and RNN model on the relatively large database of 40,703 patients with RNN came out on top with AUC = 0.842.
There are 15 (28.8%) studies which employed explainability in ML in some way (Fig. 6). The most popular explainability method was feature importance used in 13 (87%) studies. Most of these studies did not specify how the feature importances were obtained. 6 studies used feature extraction tools: Shapley additive explanations (SHAP) and Local interpretable model-agnostic explanations (LIME) to obtain the importance of all the features that contributed to the results [49, 58, 65,66,67, 73]. In 2020, Sinha et al. [46] used feature importance on 3 different ML methods to determine the 6 most impactful parameters which can be fed into the final ML algorithms. The white-box approach of explainability was used by Wu et al. in 2022 [69] via an interpretable random forest algorithm. Wang et al. in 2023 [68] used 3 different feature attraction methods SHAP, LIME and DALEX for their best-performing algorithm. They were also the only group that actively pursue explainability as the core feature of the final algorithm.
Discussion
This review aimed to highlight the usage of ML methods on ARDS and ARDS-related issues such as diagnosis and management. The vast majority of research showed good results within their performing metric, for example, all studies used AUC as a performing gauge and archived the AUC values of between 0.7 and 1. However, while most studies employed the k-fold validating technique and/or used separated cohorts for validation, only one study by Lazzarini et al.[58] compared and validated the prediction capability of the ML algorithm through clinicians.
XGBoost seems to be the most popular and successful algorithm. This may be due to the size of the database used in these studies [24, 33, 40, 42, 48, 51, 57,58,59, 65, 66, 69, 73]. While large public databases such as MIMIC and eICU were commonly used, the vast majority of research used less than 5000 samples. This may limit the viability of more advanced ML algorithm such as neural network and its variances. Additionally, ML algorithms especially non-neural network models, can perform well with limited data, having a large database can potentially provide a more stable and reliable final algorithm. The most advanced ML algorithm, neural network, also requires a larger database to increase its potential. However, collecting patient data is meet with many difficulties in term of ethic and administrative control such as identifiability or patient consent. An interesting way to avoid this is by using virtual/simulated patients pioneered by Barakat [72]. However, whilst this method provided arbitrarily large, cleaned and complete database, the realistic of the virtual patients must be thoroughly tested and justified before being used for ML model development. It is another layer of complexity added on top of the developed ML model which must be independently validated.
With the rise of applications of ML and AI in real life, medical law, regulations, and demand for transparency will require a larger degree of explainability on ML algorithms. However, the use of explainability methods in the reviewed articles seems to be an afterthought with only one research actively trying to create an explainable ML algorithm as one of their main goals [67]. Furthermore, there was no attempt to validate those explainable features with actual physicians and clinicians. With the growing impetus and demand for digital healthcare, more research in this area is required. For example, there is currently no method to quantify the effectiveness of explainability methods to clinicians that was utilised in the included papers. Future work also should verify the resulting ML algorithm and is explainability methods with actual physician and clinician as a key component of the research. Although a rigorous validating method was proposed by Amarasinghe et al. [78], there are currently few studies that fully utilise this method [78].
To bridge the gap between research and real-life application, future research should focus on not only the performing metric of the ML algorithm such as AUC or accuracy but also on finding a clear explanation for the algorithm outcome. These should not be limited to graphical outputs such as those provided by SHAP or LIME but should other outputs (textual or numerical). Validating these explanations with clinicians and physicians should also be prioritised. We propose another validation step by seeking consensus with clinicians to validate the usability of future models.
The risk of bias was not formally reported in this review due to bias assessment tool such as Prediction model Risk of Bias Assessment Tool (PROBAST) is for prediction model alone. However, in general, the characteristic of data used such as ethnicity or sex were unreported in all studies. Therefore, the risk of bias is high in all studies if PROBAST was used.
To develop more robust ML model, there is a need for a large, multinational, multi centres database. This database will help to reduce bias, increase representation in different ethnic and gender groups. Collaboration between clinician and data scientist is also vital to cross validate and evaluate the viability of developed model. One of the most important purposes of the reviewed studies is to further the knowledge about ARDS and thus provide a tool for clinician to improve patient’s condition and survivability. Therefore, a rigorous framework for assessing the effectiveness of explainability of ML model on end-user is needed. The framework may contain series of surveys and tests to evaluate clinicians’ performances with and without ML support and explanations. Such framework would narrow the gap between academic study and real-world applications.
Conclusion
This systematic review captures the usage of ML in ARDS research. This is the most extensive review on this topic thus far with 52 articles included. However, due to the amount of area of research included, spanning 7 categories (Fig. 2), meta-analysis was not considered for this paper. This can be done in future review focusing on each category of ML application.
Machine learning has been proven to be useful in many aspects of ARDS including diagnosis, risk assessment, mortality prediction and prognosis. To fully utilise the advantages of neural network algorithm, a database of more than 5000, ideally more than 10,000 patient records is required. With small databases of fewer than 5000 records, extreme gradient boosting has the highest probability of success. Public databases such as MIMIC are ideal if used in conjunction with handpicked data to either provide a broader spectrum, or to validate the resulting algorithm emerged from such data. With such database, more advanced and powerful ML algorithm such as neural network, reinforcement learning and deep learning and be utilised and show their full potential.
In term of area of research, not a lot of research focused on how ARDS is currently managed (Fig. 2). More research could be done in this category such as in drug admission and ventilator setting as improvement in this area can vastly improve the mortality rate of patients. As the nature of this kind of the outcome of management research is more complex than prediction of ARDS or mortality research, this category of research would also benefit from lager database and more advanced algorithm mentioned above.
In terms of explainability, while SHAP and LIME are popular choices, there is still a gap between understanding and utilising the results from such instruments by data scientists compared to real clinicians. Therefore, to develop a machine learning model to truly support clinicians to tackle ARDS, there is still a lack of research on transparent and explainable models. Due to the complexity of ARDS in definition, recognition, and management, this is challenging. Future research and studies on machine learning applications in ARDS should focus more on the explainability and robustness of the model rather than the accuracy and sensitivity of the models.
Amarasinghe et al. [78] proposed a framework to quantify the effectiveness of explainability method to clinician. This method involves a series of survey on how clinician’s opinion changed with and without explainability. Future research can ultilised this method to evaluate the resulting algorithm and explainability method. This can accelerate the acceptance and integration of ML into real life application. However, this method is time consuming due to the number of clinicians required and the number of surveys needed for this method to be statistically significant. Therefore, a more approachable framework that requires fewer resources, would be hugely beneficial for future researches and can be integrated into more researches.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Bellani G, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. https://doi.org/10.1001/jama.2016.0291.
“Guidelines on the management of acute respiratory distress syndrome,” 2018.
Shamout F, Zhu T, Clifton DA. Machine learning for clinical outcome prediction. IEEE Rev Biomed Eng. 2021;14:116–26. https://doi.org/10.1109/RBME.2020.3007816.
B. Rush, L. A. Celi, and D. J. Stone, “Applying machine learning to continuously monitored physiological data,” Journal of Clinical Monitoring and Computing, 2019;33(5):887–893. Springer Netherlands, https://doi.org/10.1007/s10877-018-0219-z.
D. A. Clifton, J. Gibbons, J. Davies, and L. Tarassenko, “Machine learning and software engineering in health informatics,” in 2012 1st International Workshop on Realizing AI Synergies in Software Engineering, RAISE 2012 - Proceedings, 2012, pp. 37–41. https://doi.org/10.1109/RAISE.2012.6227968.
Z. C. Lipton, J. Berkowitz, and C. Elkan, “A Critical Review of Recurrent Neural Networks for Sequence Learning,” May 2015, [Online]. Available: http://arxiv.org/abs/1506.00019
A. M. Alaa and M. van der Schaar, “AutoPrognosis: Automated Clinical Prognostic Modeling via Bayesian Optimization with Structured Kernel Learning,” 2018.
Jha D, et al. Real-time polyp detection, localization and segmentation in colonoscopy using deep learning. IEEE Access. 2021;9:40496–510. https://doi.org/10.1109/ACCESS.2021.3063716.
S. Ali et al., “Deep learning for detection and segmentation of artefact and disease instances in gastrointestinal endoscopy,” Med Image Anal, vol. 70, May 2021, doi: https://doi.org/10.1016/j.media.2021.102002.
H. Phan, F. Andreotti, N. Cooray, O. Y. Chen, and M. de Vos, “Automatic Sleep Stage Classification Using Single-Channel EEG: Learning Sequential Features with Attention-Based Recurrent Neural Networks,” in Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Institute of Electrical and Electronics Engineers Inc., 2018:1452–1455. https://doi.org/10.1109/EMBC.2018.8512480.
D. Suo et al., “Machine Learning for Mechanical Ventilation Control,” Feb. 2021, [Online]. Available: http://arxiv.org/abs/2102.06779
L. Yu et al., “Machine learning methods to predict mechanical ventilation and mortality in patients with COVID-19,” PLoS One. 2021;16(4). https://doi.org/10.1371/journal.pone.0249285.
M. Y. Lin et al., “Explainable machine learning to predict successful weaning among patients requiring prolonged mechanical ventilation: a retrospective cohort study in central Taiwan,” Front Med (Lausanne), 2021;8. https://doi.org/10.3389/fmed.2021.663739.
Kulkarni AR, et al. Deep learning model to predict the need for mechanical ventilation using chest X-ray images in hospitalised patients with COVID-19. BMJ Innov. 2021;7(2):261–70. https://doi.org/10.1136/bmjinnov-2020-000593.
A. Peine et al., “Development and validation of a reinforcement learning algorithm to dynamically optimize mechanical ventilation in critical care,” NPJ Digit Med. 2021;4(1). https://doi.org/10.1038/s41746-021-00388-6.
B. Mamandipoor et al., “Machine learning predicts mortality based on analysis of ventilation parameters of critically ill patients: multi-centre validation,” BMC Med Inform Decis Mak. 2021;21(1). https://doi.org/10.1186/s12911-021-01506-w.
Chatrian A, et al. Artificial intelligence for advance requesting of immunohistochemistry in diagnostically uncertain prostate biopsies. Mod Pathol. 2021;34(9):1780–94. https://doi.org/10.1038/s41379-021-00826-6.
Colopy GW, Roberts SJ, Clifton DA. Gaussian Processes for personalized interpretable volatility metrics in the step-down ward. IEEE J Biomed Health Inform. 2019;23(3):949–59. https://doi.org/10.1109/JBHI.2019.2890823.
Lipton ZC. The mythos of model interpretability. Queue. 2018;16(3):31–57. https://doi.org/10.1145/3236386.3241340.
A. Holzinger, G. Langs, H. Denk, K. Zatloukal, and H. Müller, “Causability and explainability of artificial intelligence in medicine,” Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery, 2019;9(4). Wiley-Blackwell. https://doi.org/10.1002/widm.1312.
J. Amann, A. Blasimme, E. Vayena, D. Frey, and V. I. Madai, “Explainability for artificial intelligence in healthcare: a multidisciplinary perspective,” BMC Med Inform Decis Mak. 2020;20(1). https://doi.org/10.1186/s12911-020-01332-6.
Murdoch WJ, Singh C, Kumbier K, Abbasi-Asl R, Yu B. Definitions, methods, and applications in interpretable machine learning. Proc Natl Acad Sci U S A. 2019;116(44):22071–80. https://doi.org/10.1073/pnas.1900654116.
Y. Zhang, Y. Weng, and J. Lund, “Applications of Explainable Artificial Intelligence in Diagnosis and Surgery,” Diagnostics, 2022;12(2). https://doi.org/10.3390/diagnostics12020237. MDPI.
M. Sayed, D. Riaño, and J. Villar, “Predicting duration of mechanical ventilation in acute respiratory distress syndrome using supervised machine learning,” J Clin Med, 2021;10(17). https://doi.org/10.3390/jcm10173824.
Herasevich V, Yilmaz M, Khan H, Hubmayr RD, Gajic O. Validation of an electronic surveillance system for acute lung injury. Intensive Care Med. 2009;35(6):1018–23. https://doi.org/10.1007/s00134-009-1460-1.
A. Pearl and D. Bar-Or, “Using Artificial Neural Networks to predict potential complications during Trauma patients’ hospitalization period,” in Studies in Health Technology and Informatics, IOS Press, 2009, pp. 610–614. doi: https://doi.org/10.3233/978-1-60750-044-5-610.
Brown LM, Calfee CS, Matthay MA, Brower RG, Thompson BT, Checkley W. A simple classification model for hospital mortality in patients with acute lung injury managed with lung protective ventilation. Crit Care Med. 2011;39(12):2645–51. https://doi.org/10.1097/CCM.0b013e3182266779.
Koenig HC, et al. Performance of an automated electronic acute lung injury screening system in intensive care unit patients. Crit Care Med. 2011;39(1):98–104. https://doi.org/10.1097/CCM.0b013e3181feb4a0.
Chbat NW, et al. Clinical knowledge-based inference model for early detection of acute lung injury. Ann Biomed Eng. 2012;40(5):1131–41. https://doi.org/10.1007/s10439-011-0475-2.
Bernstein DB, Nguyen B, Allen GB, Bates JHT. Elucidating the fuzziness in physician decision making in ARDS. J Clin Monit Comput. 2013;27(3):357–63. https://doi.org/10.1007/s10877-013-9449-2.
Sinha P, Delucchi KL, Thompson BT, McAuley DF, Matthay MA, Calfee CS. Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Intens Care Med. 2018;44(11):1859–69. https://doi.org/10.1007/s00134-018-5378-3.
M. Afshar et al., “A Computable Phenotype for Acute Respiratory Distress Syndrome Using Natural Language Processing and Machine Learning.” [Online]. Available: http://ctakes.apache.org
D. Zeiberg, T. Prahlad, B. K. Nallamothu, T. J. Iwashyna, J. Wiens, and M. W. Sjoding, “Machine learning for patient risk stratification for acute respiratory distress syndrome,” PLoS One, 2019; 14(3). https://doi.org/10.1371/journal.pone.0214465.
X.-S. Yu et al., “Lung-heart pressure index is a risk factor for acute respiratory distress syndrome (ARDS): A machine learning and propensity score-matching study,” 2019. https://doi.org/10.21203/rs.2.19093/v1.
Zampieri FG, et al. Heterogeneous effects of alveolar recruitment in acute respiratory distress syndrome: a machine learning reanalysis of the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial. Br J Anaesth. 2019;123(1):88–95. https://doi.org/10.1016/j.bja.2019.02.026.
Zhang Z, Zheng B, Liu N, Ge H, Hong Y. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45(6):856–64. https://doi.org/10.1007/s00134-019-05627-9.
X. F. Ding et al., “Predictive model for acute respiratory distress syndrome events in ICU patients in China using machine learning algorithms: A secondary analysis of a cohort study,” J Transl Med, 2019; 17(1). https://doi.org/10.1186/s12967-019-2075-0.
Zhang Z. Prediction model for patients with acute respiratory distress syndrome: Use of a genetic algorithm to develop a neural network model. PeerJ. 2019;9:2019. https://doi.org/10.7717/peerj.7719.
Zhou M, et al. Rapid breath analysis for acute respiratory distress syndrome diagnostics using a portable two-dimensional gas chromatography device. Anal Bioanal Chem. 2019;411(24):6435–47. https://doi.org/10.1007/s00216-019-02024-5.
P. Yang et al., “A new method for identifying the acute respiratory distress syndrome disease based on noninvasive physiological parameters,” PLoS One. 2020; 15(2). https://doi.org/10.1371/journal.pone.0226962.
Reamaroon N, Sjoding MW, Lin K, Iwashyna TJ, Najarian K. Accounting for label uncertainty in machine learning for detection of acute respiratory distress syndrome. IEEE J Biomed Health Inform. 2019;23(1):407–15. https://doi.org/10.1109/JBHI.2018.2810820.
Sinha P, Churpek MM, Calfee CS. Machine learning classifier models can identify acute respiratory distress syndrome phenotypes using readily available clinical data. Am J Respir Crit Care Med. 2020;202(7):996–1004. https://doi.org/10.1164/rccm.202002-0347OC.
Le S, et al. Supervised machine learning for the early prediction of acute respiratory distress syndrome (ARDS). J Crit Care. 2020;60:96–102. https://doi.org/10.1016/j.jcrc.2020.07.019.
J. Hu, Y. Fei, and W. qin Li, “Predicting the mortality risk of acute respiratory distress syndrome: radial basis function artificial neural network model versus logistic regression model,” J Clin Monit Comput, vol. 36, no. 3, pp. 839–848, Jun. 2022, doi: https://doi.org/10.1007/s10877-021-00716-x.
Chen Y, et al. A quantitative and radiomics approach to monitoring ards in COVID-19 patients based on chest CT: A retrospective cohort study. Int J Med Sci. 2020;17(12):1773–82. https://doi.org/10.7150/ijms.48432.
Sinha P, Delucchi KL, McAuley DF, O’Kane CM, Matthay MA, Calfee CS. Development and validation of parsimonious algorithms to classify acute respiratory distress syndrome phenotypes: a secondary analysis of randomised controlled trials. Lancet Respir Med. 2020;8(3):247–57. https://doi.org/10.1016/S2213-2600(19)30369-8.
W. Xu et al., “Risk factors analysis of COVID-19 patients with ARDS and prediction based on machine learning,” Sci Rep, 2021;11(1). https://doi.org/10.1038/s41598-021-82492-x.
M. Sayed, D. Riaño, and J. Villar, “Novel criteria to classify ARDS severity using a machine learning approach,” Crit Care, 2021;25(1). https://doi.org/10.1186/s13054-021-03566-w.
L. Singhal et al., “eARDS: A multi-center validation of an interpretable machine learning algorithm of early onset Acute Respiratory Distress Syndrome (ARDS) among critically ill adults with COVID-19,” PLoS One, 2021;16(9). https://doi.org/10.1371/journal.pone.0257056.
P. Sinha, A. Spicer, K. L. Delucchi, D. F. McAuley, C. S. Calfee, and M. M. Churpek, “Comparison of machine learning clustering algorithms for detecting heterogeneity of treatment effect in acute respiratory distress syndrome: A secondary analysis of three randomised controlled trials,” EBioMedicine. 2021;74. https://doi.org/10.1016/j.ebiom.2021.103697.
E. Schwager et al., “Utilizing machine learning to improve clinical trial design for acute respiratory distress syndrome,” NPJ Digit Med. 2021;4(1). https://doi.org/10.1038/s41746-021-00505-5.
B. Afshin-Pour et al., “Discriminating Acute Respiratory Distress Syndrome from other forms of respiratory failure via iterative machine learning,” Intell Based Med. 2023;7. https://doi.org/10.1016/j.ibmed.2023.100087.
X. Liu et al., “Identification of distinct clinical phenotypes of acute respiratory distress syndrome with differential responses to treatment,” Crit Care. 2021;25(1). https://doi.org/10.1186/s13054-021-03734-y.
C. Lam et al., “Semisupervised deep learning techniques for predicting acute respiratory distress syndrome from time-series clinical data: Model development and validation study,” JMIR Form Res, 2021;5(9). https://doi.org/10.2196/28028.
Huang B, et al. Mortality prediction for patients with acute respiratory distress syndrome based on machine learning: a population-based study. Ann Transl Med. 2021;9(9):794–794. https://doi.org/10.21037/atm-20-6624.
Sabeti E, et al. Learning using partially available privileged information and label uncertainty: application in detection of acute respiratory distress syndrome. IEEE J Biomed Health Inform. 2021;25(3):784–96. https://doi.org/10.1109/JBHI.2020.3008601.
N. Reamaroon, M. W. Sjoding, J. Gryak, B. D. Athey, K. Najarian, and H. Derksen, “Automated detection of acute respiratory distress syndrome from chest X-Rays using Directionality Measure and deep learning features,” Comput Biol Med, 2021;134. https://doi.org/10.1016/j.compbiomed.2021.104463.
N. Lazzarini, A. Filippoupolitis, P. Manzione, and H. Eleftherohorinou, “A machine learning model on Real World Data for predicting progression to Acute Respiratory Distress Syndrome (ARDS) among COVID-19 patients,” PLoS One. 2022;17(7). https://doi.org/10.1371/journal.pone.0271227.
Y. Bai, J. Xia, X. Huang, S. Chen, and Q. Zhan, “Using machine learning for the early prediction of sepsis-associated ARDS in the ICU and identification of clinical phenotypes with differential responses to treatment,” Front Physiol, 2022;13. https://doi.org/10.3389/fphys.2022.1050849.
T. McKerahan, “A Machine Learning Algorithm to Predict Hypoxic Respiratory Failure and risk of Acute Respiratory Distress Syndrome (ARDS) by Utilizing Features Derived from Electrocardiogram (ECG) and Routinely Clinical Data”. https://doi.org/10.1101/2022.11.14.22282274.
Maddali MV, et al. Validation and utility of ARDS subphenotypes identified by machine-learning models using clinical data: an observational, multicohort, retrospective analysis. Lancet Respir Med. 2022;10(4):367–77. https://doi.org/10.1016/S2213-2600(21)00461-6.
Izadi Z, et al. Development of a prediction model for COVID-19 acute respiratory distress syndrome in patients with rheumatic diseases: results from the global rheumatology alliance registry. ACR Open Rheumatol. 2022;4(10):872–82. https://doi.org/10.1002/acr2.11481.
Jabbour S, Fouhey D, Kazerooni E, Wiens J, Sjoding MW. Combining chest X-rays and electronic health record (EHR) data using machine learning to diagnose acute respiratory failure. J Am Med Inform Assoc. 2022;29(6):1060–8. https://doi.org/10.1093/jamia/ocac030.
J. Wu et al., “Early prediction of moderate-to-severe condition of inhalation-induced acute respiratory distress syndrome via interpretable machine learning,” BMC Pulm Med, 2022;22(1). https://doi.org/10.1186/s12890-022-01963-7.
K. C. Pai et al., “Artificial intelligence–aided diagnosis model for acute respiratory distress syndrome combining clinical data and chest radiographs,” Digit Health. 2022;8. https://doi.org/10.1177/20552076221120317.
C. Lam et al., “Multitask Learning with Recurrent Neural Networks for Acute Respiratory Distress Syndrome Prediction Using Only Electronic Health Record Data: Model Development and Validation Study,” JMIR Med Inform, 2022;10(6). https://doi.org/10.2196/36202.
Wang Z, et al. Developing an explainable machine learning model to predict the mechanical ventilation duration of patients with ARDS in intensive care units. Heart Lung. 2023;58:74–81. https://doi.org/10.1016/j.hrtlng.2022.11.005.
M. Zhang and M. Pang, “Early prediction of acute respiratory distress syndrome complicated by acute pancreatitis based on four machine learning models,” Clinics. 2023;78. https://doi.org/10.1016/j.clinsp.2023.100215.
W. Wu, Y. Wang, J. Tang, M. Yu, J. Yuan, and G. Zhang, “Developing and evaluating a machine-learning-based algorithm to predict the incidence and severity of ARDS with continuous non-invasive parameters from ordinary monitors and ventilators,” Comput Methods Programs Biomed. 2023;230. https://doi.org/10.1016/j.cmpb.2022.107328.
S. Fonck, S. Fritsch, G. Nottenkämper, and A. Stollenwerk, “Implementation of ResNet-50 for the Detection of ARDS in Chest X-Rays using transfer-learning,” 2023. [Online]. Available: www.journals.infinite-science.de/automed/article/view/742
M. Yahyatabar et al., “A Web-Based Platform for the Automatic Stratification of ARDS Severity,” Diagnostics. 2023;13(5). https://doi.org/10.3390/diagnostics13050933.
Barakat CS, et al. Developing an artificial intelligence-based representation of a virtual patient model for real-time diagnosis of acute respiratory distress syndrome. Diagnostics. 2023;13(12):2098. https://doi.org/10.3390/diagnostics13122098.
W. Zhang, Y. Chang, Y. Ding, Y. Zhu, Y. Zhao, and R. Shi, “To Establish an Early Prediction Model for Acute Respiratory Distress Syndrome in Severe Acute Pancreatitis Using Machine Learning Algorithm,” J Clin Med. 2023;12(5). https://doi.org/10.3390/jcm12051718.
R. Wang, L. Cai, J. Zhang, M. He, and J. Xu, “Prediction of acute respiratory distress syndrome in traumatic brain injury patients based on machine learning algorithms,” Medicina (Lithuania). 2023;59(1). https://doi.org/10.3390/medicina59010171.
N. Farzaneh, S. Ansari, E. Lee, K. R. Ward, and M. W. Sjoding, “Collaborative strategies for deploying artificial intelligence to complement physician diagnoses of acute respiratory distress syndrome,” NPJ Digit Med. 2023;6(1). https://doi.org/10.1038/s41746-023-00797-9.
Matthay MA, et al. A new global definition of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2023. https://doi.org/10.1164/rccm.202303-0558ws.
K. Sharafutdinov et al., “Computational simulation of virtual patients reduces dataset bias and improves machine learning-based detection of ARDS from noisy heterogeneous ICU datasets,” IEEE Open J Eng Med Biol. 2023:1–11. https://doi.org/10.1109/OJEMB.2023.3243190.
K. Amarasinghe, K. T. Rodolfa, H. Lamba, and R. Ghani, “Explainable machine learning for public policy: Use cases, gaps, and research directions,” Data Policy. 2023;5. https://doi.org/10.1017/dap.2023.2.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial or non-profit sector.
Author information
Authors and Affiliations
Contributions
Original ideal T.T and M.T. Searching T.T. Screening and reviewing T.T and M.T. First drafting T.T. PRISMA Check list T.T and M.T. Critical review these paper T.T, M.T, A.J, P.P, V.G, and A.F. Oversee process V.G and A.F
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical committee approval was not required in this systematic review.
Consent for publication
The authors consent for this work to be published by the publisher.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tran, T.K., Tran, M.C., Joseph, A. et al. A systematic review of machine learning models for management, prediction and classification of ARDS. Respir Res 25, 232 (2024). https://doi.org/10.1186/s12931-024-02834-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02834-x