Abstract
Background
Long-term outcomes of lung transplantation (LTx) remain hampered by chronic lung allograft dysfunction (CLAD). Matrix metalloproteinase 9 (MMP-9) is a secretory endopeptidase identified as a key mediator in fibrosis processes associated with CLAD. The objective of this study was to investigate whether plasma MMP9 levels may be prognostic of CLAD development.
Methods
Participants were selected from the Cohort in Lung Transplantation (COLT) for which a biocollection was associated. We considered two time points, year 1 (Y1) and year 2 (Y2) post-transplantation, for plasma MMP-9 measurements. We analysed stable recipients at those time points, comparing those who would develop a CLAD within the 2 years following the measurement to those who would remain stable 2 years after.
Results
MMP-9 levels at Y1 were not significantly different between the CLAD and stable groups (230 ng/ml vs. 160 ng/ml, p = 0.4). For the Y2 analysis, 129 recipients were included, of whom 50 developed CLAD within 2 years and 79 remained stable within 2 years. MMP-9 plasma median concentrations were higher in recipients who then developed CLAD than in the stable group (230 ng/ml vs. 118 ng/ml, p = 0.003). In the multivariate analysis, the Y2 MMP-9 level was independently associated with CLAD, with an average increase of 150 ng/ml (95% CI [0–253], p = 0.05) compared to that in the stable group. The Y2 ROC curve revealed a discriminating capacity of blood MMP-9 with an area under the curve of 66%.
Conclusion
Plasmatic MMP-9 levels measured 2 years after lung transplantation have prognostic value for CLAD.
Similar content being viewed by others
Introduction
Lung transplantation (LTx) has the potential to bring survival benefits and improve quality of life in selected candidates [1, 2]. However, long-term outcomes remain low, with an overall survival of 63% at 5 years post-transplantation [3]. The main long-term limitation is chronic lung allograft dysfunction (CLAD), which is responsible for most deaths after the first posttransplant years [4]. A large part of CLAD physiopathology remains unclear, but significant advances have been made to better understand the two clinically and functionally well-defined phenotypes of CLAD: bronchiolitis obliterans syndrome (BOS) and restrictive allograft syndrome (RAS). Briefly, repeated injuries of the airway epithelium, alveoli or lung endothelial cells result in chronic inflammation, wound healing, recruitment and proliferation of fibroblasts and aberrant deposition of extracellular matrix, leading to small airway fibrotic obliteration in BOS and alveolar fibroelastosis in RAS [5]. CLAD risk stratification of LTx recipients is presently an unmet need. A multisystemic approach is certainly the way forward in a highly complex situation in which immunology, medications, environment and patient’s behaviours have an important impact on outcomes. Matrix metalloproteinases (MMPs) are a family of zinc-dependent endopeptidases involved in the degradation of various proteins of the extracellular matrix. MMPs play a role in tissue remodelling during various physiological processes, such as angiogenesis, embryogenesis, morphogenesis and wound repair, as well as in pathological conditions, such as fibrotic disorders and cancer. Matrix metalloproteinase 9 (MMP-9) is part of the gelatinase subfamily, which has a distinct collagen-binding domain. It can be secreted by a variety of cells, including epithelial cells, fibroblasts, macrophages and T cells [6]. MMP-9 has been identified as a key mediator in processes associated with CLAD, such as extracellular matrix reorganization, cell migration, epithelial to mesenchymal transition and immune response [7]. Interestingly, MMP-9 is an old suspect in BOS, and several works have found increased gelatinolytic activity and/or MMP-9 concentrations in bronchoalveolar lavage (BAL) from recipients with BOS [8,9,10,11]. Two studies reported that almost 6 months before the diagnosis of BOS, increased BAL MMP-9 activity was observed [12, 13]. However, the relevance of MMP-9 in peripheral blood remains debated, whereas the clinical need for minimally invasive biomarkers of CLAD is high [14]. Previous data from our group showed that blood MMP-9 levels may be higher in CLAD recipients [15]. To evaluate CLAD risk factors that could enable preventive intervention, we considered the following time points of analysis: 1 and 2 years post-transplantation. Our objective in this study was to validate whether plasma MMP-9 levels at 1 year and 2 years post-transplantation can predict future CLAD onset.
Materials and methods
Participants
Lung transplant recipients (LTRs) were recruited within the multicentre cohort in lung transplantation [COLT], NCT00980967) study (Comité de Protection des Personnes Ouest 1-Tours, 2009-A00036-51). The study was approved by the local ethical committee, and all participants provided written informed consent. The COLT study protocol has been previously described (Additional file 1: S1) [16]. Briefly, participants were included in the cohort before transplantation. Planned visits were at the time of transplantation and then every 6 months up to 5 years post-transplantation. Blood samples were taken at each visit. This study was conducted in accordance with the Declaration of Helsinki and complies with the International Society for Heart and Lung Transplantation statement on Transplant Ethics.
Clinical phenotype
All patients within the COLT study underwent individual phenotyping by an adjudication committee that gathered at least 5 investigator physicians from the different participating centres. Pulmonary function tests, relevant chest computed tomography and medical history, especially potential confounding factors, were reviewed for a collegial decision on phenotype initially based on the 2014 proposed classification and then on the 2019 ISHLT consensus report on CLAD [17, 18]. Recipients were classified as follows: BOS, RAS, azithromycin responsive allograft dysfunction (ARAD), stable and other (death within 3 months post-transplantation, death without CLAD, insufficient data to conclude or confounding factors).
Design of the study and recipient selection
The objective of this study was to evaluate the ability of MMP-9 blood levels to predict CLAD. We designed a comparative analysis of plasma MMP-9 concentrations at year 1 post-transplantation (Y1) between stable recipients at this time point who will develop CLAD within 2 years (i.e., by 3 years post-transplantation) and those who remained without CLAD for the same 2-year follow-up (Stable). Similarly, we designed a comparative analysis of plasma MMP-9 concentrations at year 2 post-transplantation (Y2) from stable recipients at this time point, comparing those who will develop CLAD within 2 years of sampling (i.e., by 4 years post-transplantation) and those who remained stable (Additional file 1: Figure S1).
For this purpose, we identified every COLT participant with stable lung function at Y1 for whom we had a plasma sample available, and we then selected those who presented a CLAD phenotype by year 3. Then, we matched up to 2 stable controls for each CLAD recipient on age at transplantation and gender (variable ratio matching) (Fig. 1). We excluded COLT participants who were not transplanted, recipients with the phenotype “Other” and those with no phenotype. We also excluded recipients who were included in our previous MMP-9 analysis (n = 94) [15]. According to the study design, recipients who developed CLAD before 1 year post-transplantation were not included in the Y1 analysis (n = 35), and similarly, recipients who developed CLAD before 2 years post-transplantation were not included in the Y2 analysis (n = 124). Flowcharts are represented in Fig. 1 for the Y1 analysis and Fig. 2 for the Y2 analysis. Overall, the median follow-up time from LTx was 45 months, and 63 patients were included in both the Y1 and Y2 analyses (recipients for whom a sample was available at Y1 and Y2).
Year 1 sample analysis flowchart. Selection of COLT lung transplant recipients with CLAD or a stable phenotype. Other phenotypes included death before 3 months, death without CLAD and an inconclusive phenotype (insufficient data or cofounding factors affecting adjudication). “No phenotype” refers to recipients awaiting adjudication
Year 2 sample flowchart. Selection of COLT lung transplant recipients with CLAD or a stable phenotype. Other phenotypes included death before 3 months, death without CLAD and an inconclusive phenotype (insufficient data or cofounding factors affecting the adjudication). “No phenotypes” refer to recipients awaiting adjudication.* One recipient was initially classified as having azithromycin-responsive allograft dysfunction and was not included in the stable group for the year 1 sample analysis but later developed CLAD and was included in the CLAD group for the year 2 sample analysis
MMP-9 detection
All plasma samples were obtained in heparinized tubes, stored at − 80 °C in Nantes University Hospital Biological Resource Center and never thawed before use. MMP-9 concentrations were determined with the quantitative MMP-9 Human ELISA Kit (Thermo Fisher Scientific, BMS2016-2) according to the manufacturer’s instructions.
Statistical analysis
For descriptive analysis, normally distributed continuous variables are summarized herein by the mean plus standard deviation, whereas nonnormally distributed continuous variables are summarized using the median and interquartile range (IQR). Categorical variables are presented as the effectiveness and percentage of modalities. We used usual statistical tests to compare distributions between two groups (Student’s t test, Mann‒Whitney-Wilcoxon test and Fisher exact test). Missing values are systematically presented. No imputation was performed.
To assess whether MMP-9 could be prognostic of CLAD, we only considered measures that had been made before the diagnosis. In addition, we drew ROC and precision-recall (PR) curves to investigate with appropriate metrics whether MMP-9 concentrations could be relevant in predicting CLAD in these patients. The confidence interval of the ROC area under the curve (AUC) and PR-AUC was computed using 3000 bootstrap iterations of the corresponding study sample. Finally, a multivariate linear regression model was fit to explain MMP-9 concentrations at Y1 by the status regarding CLAD 2 years later, plus susceptible confounders identified by a group of clinicians. Additional descriptions of the variables of interest are provided in Additional file 1: S2. We also fitted a model for MMP-9 concentrations at Y2 explained by the status regarding CLAD 2 years after, plus the same confounders. Due to a lack of data, we were unable to split our dataset into a training set and a test set. Analyses were performed using R package version 4.2.2, especially using the tidyverse package for data manipulation and visualization and tidymodels for predictive modelling.
Results
Prognostic value of MMP-9 at Y1
A total of 190 stable recipients were included for the analysis of MMP-9 at Y1 post-transplantation of whom 86 developed CLAD (68 BOS, 9 RAS and 9 mixed) and 104 remained stable within the next 2 years (Fig. 2). Pretransplant characteristics and early posttransplantation outcomes (within the first year post-Tx) are presented in Table 1. The distribution of underlying disease was significantly different between the stable and CLAD groups, with fewer patients with chronic obstructive pulmonary disease (COPD)/emphysema and more with interstitial lung disease (ILD) and other diagnoses in the CLAD group (p = 0.01). The median height was lower in the CLAD group (165 cm vs. 168 cm, p = 0.05), and more patients in the stable group had pre-Tx pulmonary colonization to Candida albicans (37% vs. 18%, p = 0.04). There were also fewer recipients in the CLAD group who benefited from induction treatment after transplantation (70% vs. 84%, p = 0.03). Finally, there was a tendency for an increased number of experienced acute cellular rejections in the CLAD group (43% vs. 30%, p = 0.08). The 2 groups were comparable in terms of sex, age, type of procedure, donor and graft characteristics and infection post-transplantation outcomes.
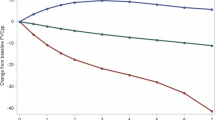
Before transplantation, the MMP-9 levels were statistically similar in both the CLAD and stable groups (386 ng/ml IQR[174–757] vs. 349 ng/m IQR[162–822], p = 0.8). The MMP-9 plasma median concentration at Y1 was 237 ng/ml IQR[72–551] for recipients who developed CLAD within the next 2 years and 165 ng/ml IQR[75–317] for those who remained stable (Fig. 3). The difference was not significant (p = 0.2). Additionally, there was no significant difference according to CLAD phenotype (Additional file 1: Figure S2). In this analysis, we also distinguished those who developed CLAD within the year that followed the Y1 measurement (sample close to CLAD) and those who developed CLAD at least 1 year later (sample distant from CLAD). In this setting, the MMP-9 blood concentration was slightly higher when the sample was close to CLAD than when the sample was distant from CLAD diagnosis (248 ng/ml vs. 225 ng/ml, p = 0.9) (Fig. 3). The multivariate analysis revealed that the CLAD phenotype was associated with an increase in MMP-9 plasma levels, but the difference did not reach statistical significance (average increase of 126, 95% CI [− 32–284], p = 0.1) (Table 2). To test the discriminating capacity of Y2 MMP-9 blood measurement for CLAD prediction, we performed a PR curve, which showed an AUC of 53% (95% CI [43–65]). For the ROC curve, we found an AUC of 55% (95% CI [47–63]) (Additional file 1: Figure S3).
Blood MMP-9 value at Y1. A Comparison of the MMP-9 plasmatic concentration at Y1 between recipients who then developed CLAD and those who remained stable in the next 2 years (p = 0.2). B Comparison of samples close to CLAD and distant from CLAD. Comparison of the MMP-9 plasmatic concentration at Y1 between recipients who developed CLAD within 1 year of measurement, those who developed CLAD at least 1 year after measurement and those who remained stable at least 2 years after measurement. No significant difference was observed. Boxplot interpretation: thick horizontal bars correspond to the median, notches to the upper and lower limits of the confidence interval and top and bottom of the box to the first and third interquartile of MMP-9 values
Prognostic value of MMP-9 at Y2
For this analysis, 129 LTx recipients were included, of whom 50 developed CLAD and 79 remained stable within the next 2 years (i.e., up to 4 years post-transplantation) (Fig. 2). Notably, one patient was initially diagnosed with ARAD (and thus not included in the stable group) but later developed CLAD and was included in the CLAD Y2 group. Pretransplantation characteristics, per transplantation data and early post-transplantation outcomes are presented in Table 3. Few differences can be noted compared to the Y1 analysis. Underlying diseases were not differently distributed between the CLAD and stable groups, and there was no difference in recipient height. Interestingly, there were more CLAD patients with pre-Tx colonization with Pseudomonas aeruginosa (46% vs. 27%, p = 0.04) and fewer with Candida albicans (16% vs. 37%, p = 0.02). The 2 groups were comparable in terms of sex, age, type of procedure, donor and graft characteristics, infection and acute rejection outcomes post-transplantation.
Before transplantation, the MMP-9 levels were 419 ng/ml IQR[242–675] in the CLAD group and 345 ng/ml IQR[162–861] in the stable group (p = 0.6). Interestingly, the MMP-9 plasma median concentration at Y2 was significantly higher for recipients who developed CLAD within the next 2 years than for those who remained stable (230 ng/ml IQR[105–376] vs. 118 ng/ml IQR[64–218], p = 0.003) (Fig. 4). BOS, RAS and mixed MMP-9 values were all above the stable group, but the difference was significant only for recipients with RAS (265 ng/ml vs. 119 ng/ml, p = 0.02) (Additional file 1: Figure S4). In the CLAD group, patients with a sample close to the CLAD diagnostic date (within 1 year of measurement) had a higher blood MMP-9 level than those with a sample distant from the CLAD (at least 1 year after measurement) (224 ng/ml vs. 182 ng/ml, Fig. 4). In the multivariate analysis, higher MMP-9 levels at Y2 were independently and significantly associated with future CLAD diagnosis (estimated increase of 151 ng/ml, 95% CI [20–281], p = 0.02) (Table 2). The only other factor for which a significant difference was observed was pretransplantation colonization with Candida albicans, which resulted in an average increase in MMP-9 concentration at Y1 of 129 ng/mL (95% CI [2–257, (p = 0.04) (Table 3). To test the discriminating capacity of Y2 MMP-9 blood measurement for CLAD prediction, we performed a PR curve, which showed an AUC of 53% (95% CI [43–65]). For the ROC curve, we found an AUC of 66% (95% CI [56–75]) (Fig. 5). The prognostic power of blood MMP-9 was demonstrated at higher values. For example, an MMP-9 blood level higher than 314 ng/ml in our cohort enabled the identification of 40% of CLAD cases (recall or sensitivity) with a precision (positive predictive value) of 65%. Finally, to determine the prognostic effect of plasma MMP9 kinetics, we calculated the individual difference between MMP9 at Y1 and MMP9 at Y2 (MMP9 Y1–MMP9 Y2). We had 63 recipients in the CLAD group and 32 recipients in the stable group for which we had a sample available at Y1 and Y2. Interestingly, we observed an average individual decrease of 100 ng/ml in the stable group, whereas it remained almost similar in the CLAD group, with a calculated difference of 1 ng/ml. The difference between the two groups was, however, not significant (p = 0.9). The longitudinal analysis of MMP9 levels before transplantation, at Y1 and Y2 for participants with available samples at those 3 time points is presented in Additional file 1: Figure S5.
Blood MMP-9 value at Y2. A Comparison of the MMP-9 plasmatic concentration at Y2 between recipients who then developed CLAD and those who remained stable in the next 2 years (p = 0.003). B Blood MMP-9 value at Y2 with comparison of samples close to the CLAD and distant from the CLAD. Comparison of the MMP-9 plasmatic concentration at Y2 between recipients who developed CLAD within 1 year of measurement, those who developed CLAD at least 1 year after measurement and those who remained stable at least 2 years after measurement with a significant difference between the stable and CLAD groups within 1 year (p = 0.003). Boxplot interpretation: thick horizontal bars correspond to the median, notches to the upper and lower limits of the confidence interval and top and bottom of the box to the first and third interquartile of MMP-9 values. * corresponds to p value < 0.05
Discussion
In this study, we report a potential prognostic value of MMP-9 plasma concentrations at 2 years post-transplantation for CLAD diagnosis. In a smaller set of patients, our team, with a different methodology in which the reference time point was CLAD diagnosis, found increased levels of plasma MMP-9 1 year before CLAD diagnosis compared to the levels in recipients without CLAD [15]. It was, however, essential to validate the prognostic potential of blood MMP-9 in a setting that could enable risk stratification and thus therapeutic intervention. To this aim, we chose two posttransplantation time points, Y1 and Y2, that have clinical relevance because they are sufficiently distant from the lung transplantation surgery, early infection and immune complications that could strongly interfere with inflammatory or wound-healing-related biomarkers but also early enough regarding the CLAD onset time to allow early intervention in the lung transplant population.
The reason MMP-9 levels predict Y2 but not Y1 CLAD risk is unclear. However, it could be related to the fact that MMP-9 plasma levels seem to be higher when CLAD appears within 1 year from the date of sampling because we also observed that the average time between the sample and CLAD diagnosis was longer in the Y1 analysis than in the Y2 analysis (643 days vs. 489 days, respectively). The Louven group indeed described a median time of CLAD onset of 3.2 years post-transplantation, and in a North American population, Kulkarni et al. reported a median BOS-free survival of 3.6 years for double lung transplant recipients [19, 20]. The only study that prospectively evaluated MMP-9 levels after transplantation was performed by Kastelijn et al. on 10 LTx recipients who developed BOS and 10 matched control recipients without BOS. They found that the median MMP-9 concentrations in all serial samples were significantly higher in BOS patients [190 ng/ml (163–238) versus 128 ng/ml (106–162), p < 0.0001], but a longitudinal analysis of MMP-9 serum levels from the time of transplantation onwards did not reveal a significant difference in serum levels in the period preceding BOS [21]. More recently, a study using a high-component multiplex immunoassay identified MMP-9, among other proteins, as a diagnostic biomarker of BOS in a set of patients (n = 46). This finding was confirmed in another set of patients from different centres by ELISA [8]. In the different context of BOS related to chronic graftversus-host disease after allogeneic haematopoietic cell transplantation, plasma MMP-9 was also found at a higher concentration in 33 patients with BOS at the time of diagnosis than in 60 recipients without BOS, and elevated MMP-9 was thought to be associated with treatment failure and worse prognosis [22].
In the literature, more data are available for MMP-9 in BAL. In a cohort of 45 recipients, Vandemeulen et al. found that MMP9 levels were increased in RAS and BOS at the time of diagnosis [23]. Similarly, Heijink et al. found increased levels of MMP-2, MMP-3, MMP-7, MMP-8, MMP-9 and the MMP endogenous inhibitor TIMP1 at the time of diagnosis [11]. Older works have shown the predictive potential of MMP-9 in BAL in a relatively smaller cohort of less than 25 patients and not at a prespecified time point that could apply in real-life surveillance [12, 13].
Thus, regarding all these data, we are the first to describe blood MMP-9 levels in a large cohort of LTx recipients as prognostic of CLAD onset with a 66% AUC in the ROC analysis and 53% in the PR analysis. These figures may appear as low, likely due to the high variability of MMP-9 blood levels within each group of patients. While remaining a limitation, if considered alone for a given patient, no parameter currently used can actually enable a prognostic assessment of CLAD. Additionally, one important point is that given the time points chosen, i.e., 1 and 2 years for MMP-9 measurement, early CLAD (before 1-year post-transplantation) were not in the spectrum of this study. To answer these limitations, first, we did not consider MMP-9 alone as a predictive biomarker of CLAD, but this work clearly demonstrates its potential to increase the efficiency of a CLAD multidimensional score. Our group previously reported a blood gene expression analysis in which we identified three genes, POU class 2 associating factor 1, T-cell leukaemia/lymphoma protein 1A and B-cell lymphocyte kinase, which were validated as predictive biomarkers of BOS more than 6 months before diagnosis [24]. We also found differential T and B lymphocyte phenotyping between CLAD and stable recipients, again upstream of CLAD diagnosis [25, 26]. Analysis of those potential biomarkers with blood MMP-9 at this specific Y2 time point in particular will be of interest in the ongoing new prospective multicentric study to build a multidimensional risk stratification for CLAD, along with demographic, clinical and environmental data (PRELUD study, NCT03967340).
Conclusion
We described here in a large cohort the interesting prognostic potential of blood MMP-9 levels measured at 1 and 2 years post-transplantation. The implementation of these mini-invasive biomarkers into a multidimensional score, along with transcriptomic and immune phenotyping, has the potential to provide an efficient risk stratification tool to patients and clinicians.
Availability of data and materials
Any datasets used can be accessed after request to the corresponding author via e-mail.
Abbreviations
- ARAD:
-
Azithromycin-responsive allograft dysfunction
- AUC:
-
Area under the curve
- BAL:
-
Bronchoalveolar lavage
- BOS:
-
Bronchiolitis obliterans syndrome
- CLAD:
-
Chronic lung allograft dysfunction
- COLT:
-
Cohort in lung transplantation
- COPD:
-
Chronic obstructive pulmonary disease
- ILD:
-
Interstitial lung disease
- LTx:
-
Lung transplantation
- MMP-9:
-
Matrix metalloproteinase 9
- PR:
-
Precision-recall
- RAS:
-
Restrictive allograft syndrome
References
Vock DM, Durheim MT, Tsuang WM, et al. Survival benefit of lung transplantation in the modern era of lung allocation. Ann Am Thorac Soc. 2017;14(2):172–81.
Timofte I, Wijesinha M, Vesselinov R, et al. Survival benefit of lung transplantation compared with medical management and pulmonary rehabilitation for patients with end-stage COPD. ERJ Open Res. 2020;6(2):00177–2019.
Agence de la biomédecine. https://rams.agence-biomedecine.fr/greffe-cardio-pulmonaire-et-pulmonaire-0. Accessed March 14, 2022.
Chambers DC, Zuckermann A, Cherikh WS, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: 37th adult lung transplantation report—2020; focus on deceased donor characteristics. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2020;39(10):1016–27.
Verleden SE, Von der Thüsen J, Roux A, et al. When tissue is the issue: a histological review of chronic lung allograft dysfunction. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2020;20(10):2644–51.
Cui N, Hu M, Khalil RA. Biochemical and biological attributes of matrix metalloproteinases. Prog Mol Biol Transl Sci. 2017;147:1–73.
Augoff K, Hryniewicz-Jankowska A, Tabola R, Stach K. MMP9: a tough target for targeted therapy for cancer. Cancers. 2022;14(7):1847.
Niroomand A, Ghaidan H, Hallgren O, et al. Corticotropin releasing hormone as an identifier of bronchiolitis obliterans syndrome. Sci Rep. 2022;12(1):8413.
Vandermeulen E, Verleden SE, Ruttens D, et al. BAL neutrophilia in azithromycin-treated lung transplant recipients: clinical significance. Transpl Immunol. 2015;33(1):37–44.
Verleden SE, Vandooren J, Vos R, et al. Azithromycin decreases MMP-9 expression in the airways of lung transplant recipients. Transpl Immunol. 2011;25(2–3):159–62.
Heijink IH, Rozeveld D, van der Heide S, et al. Metalloproteinase profiling in lung transplant recipients with good outcome and bronchiolitis obliterans syndrome. Transplantation. 2015;99(9):1946.
Ramirez AM, Nunley DR, Rojas M, Roman J. Activation of tissue remodeling precedes obliterative bronchiolitis in lung transplant recipients. Biomark Insights. 2008;3:351–9.
Smith GN Jr, Mickler EA, Payne KK, et al. Lung transplant metalloproteinase levels are elevated prior to bronchiolitis obliterans syndrome. Am J Transplant. 2007;7(7):1856–61.
Kennedy VE, Todd JL, Palmer SM. Bronchoalveolar lavage as a tool to predict, diagnose and understand bronchiolitis obliterans syndrome. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2013;13(3):552–61.
Pain M, Royer PJ, Loy J, et al. T cells promote bronchial epithelial cell secretion of matrix metalloproteinase-9 via a C-C chemokine receptor type 2 pathway: implications for chronic lung allograft dysfunction. Am J Transplant. 2017;17:1502–14 (Published online January 1).
Koutsokera A, Royer PJ, Antonietti JP, et al. Development of a multivariate prediction model for early-onset bronchiolitis obliterans syndrome and restrictive allograft syndrome in lung transplantation. Front Med. 2017;4:109.
Verleden GM, Glanville AR, Lease ED, et al. Chronic lung allograft dysfunction: definition, diagnostic criteria, and approaches to treatment-a consensus report from the pulmonary council of the ISHLT. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2019;38(5):493–503.
Verleden GM, Raghu G, Meyer KC, Glanville AR, Corris P. A new classification system for chronic lung allograft dysfunction. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2014;33(2):127–33.
Kulkarni HS, Cherikh WS, Chambers DC, et al. Bronchiolitis obliterans syndrome-free survival after lung transplantation: an international society for heart and lung transplantation thoracic transplant registry analysis. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2018;38:5–16 (Published online September 25).
Van Herck A, Verleden SE, Sacreas A, et al. Validation of a post-transplant chronic lung allograft dysfunction classification system. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2019;38(2):166–73.
Kastelijn EA, van Moorsel CHM, Ruven HJT, et al. YKL-40 and matrix metalloproteinases as potential biomarkers of inflammation and fibrosis in the development of bronchiolitis obliterans syndrome. Sarcoidosis Vasc Diffuse Lung Dis Off J WASOG. 2013;30(1):28–35.
Inamoto Y, Martin PJ, Onstad LE, et al. Relevance of plasma matrix metalloproteinase-9 for bronchiolitis obliterans syndrome after allogeneic hematopoietic cell transplantation. Transplant Cell Ther. 2021;27(9):759.e1-759.e8.
Vandermeulen E, Verleden SE, Bellon H, et al. Humoral immunity in phenotypes of chronic lung allograft dysfunction: a broncho-alveolar lavage fluid analysis. Transpl Immunol. 2016;38:27–32.
Danger R, Royer PJ, Reboulleau D, et al. Blood gene expression predicts bronchiolitis obliterans syndrome. Front Immunol. 2017;8:1841.
Durand M, Lacoste P, Danger R, et al. High circulating CD4+CD25hiFOXP3+ T-cell sub-population early after lung transplantation is associated with development of bronchiolitis obliterans syndrome. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2018;37(6):770–81.
Brosseau C, Danger R, Durand M, et al. Blood CD9+ B cell, a biomarker of bronchiolitis obliterans syndrome after lung transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2019;19(11):3162–75.
Acknowledgements
The authors are grateful to the participating patients and their families, whose trust, support, and cooperation were essential for the collection of the data used in this study. We also thank the COLT Consortium for their organizational assistance Moreover, we acknowledge the Centre de Ressources Biologiques du CHU De Nantes, the cluster LUNG innOvatiOn (LUNG O2).
COLT consortium: Maria Ruiz-Patino, Maarten Vander Kuylen, Youri Sokolow, Constantin Stefanidis, Isabelle Huybrechts, Laurent Perrin, Fabio Taccone, Isabelle Etienne, Christiane Knoop, Anna Roussoulières, Maya Hites, Agnes Lambert, Axelle Hemelsoet—Département médico-chirurgical des pathologies thoraciques, Hôpital Universitaire de Bruxelles, Bruxelles, Belgium; Renaud Grima, Gabrielle Drevet, Jean-Michel Maury, François Tronc, Philippe Portan, Jean-François Mornex, Claire Merveilleux Du Vignaud, Eva Chatron, Jean Charles Glérant, Ségolène Turquier, Salim Si Mohamed, Vincent Cottin, Lara Chalabresse, Chantal Dubois, Aurélie Rea, Médéric Reignier, Julia Canterini—Université Claude Bernard Lyon 1, EPHE, INRAE, IVPC, Lyon F-69007, Hospices civils de Lyon, Lyon F-69007, Inserm, Hospices civils de Lyon, CIC1407, Lyon F-69007; Elie Fabre, Olaf Mercier, Delphine Mitilian, Justin Issard, Dominique Fabre—Service de Chirurgie thoracique et Transplantation Pulmonaire, Groupe hospitalier Marie-Lannelongue -Saint Joseph, Le Plessis-Robinson, Université Paris-Saclay, Le Kremlin Bicêtre, UMR_S 999, Université Paris–Sud, INSERM France; Anne Bergeron, Gregory Berra, Angela Koutsokera–Service de Pneumologie, Hôpitaux Universitaires de Genève, Rue Gabrielle-Perret-Gentil 4, 1211 Genève 14
Elodie Blanchard8, Xavier Demant8, Virginie Hulo8, Maria Ruiz-Patino, Maarten Vander Kuylen, Youri Sokolow, Constantin Stefanidis, Isabelle Huybrechts, Laurent Perrin, Fabio Taccone, Isabelle Etienne, Christiane Knoop, Anna Roussoulières, Maya Hites, Agnes Lambert, Axelle Hemelsoet, Pierrick Bedouch10, Amandine Briault10, Loic Falque10, Quentin Perrier10, Christel Saint Raymond10, Samarmar Chacaroun10, Yoann Gioria10, Joane Quentin10, Renaud Grima, Gabrielle Drevet, Jean-Michel Maury, François Tronc, Philippe Portan, Jean-François Mornex, Claire Merveilleux Du Vignaud, Eva Chatron, Jean Charles Glérant, Ségolène Turquier, Salim Si Mohamed, Vincent Cottin, Lara Chalabresse, Chantal Dubois, Aurélie Rea, Médéric Reignier, Julia Canterini, Nicolas Carlier14, Véronique Boussaud14, Romain Guillemain14, Xavier-Benoit D’Journo4, Pascale-Alexandre Thomas4, Delphine Trousse4, Geoffrey Brioude4, David Boulate4, Alex Fourdrain4, Fabienne Bregeon4, Stéphane Delliaux4, Martine Reynaud-Gaubert4, Bérengère Coltey4, Nadine Dufeu4, Benjamin Coiffard4, Julien Bermudez4, Ana Nieves4, Hervé Dutau4, Julie Tronchetti4, Jean-Yves Gaubert4, Paul Habert4, Mathieu Di Biscéglie4, Agnes Basire4, Pascal Pedini4, Florence Daviet4, Christophe Guervilly4, Sami Hraiech4, Jean Marie Forel4, Louis Delamarre4, Aude Charvet4, Ines Gragueb-Chatti4, Pierre Mora4, Daniel Laurent4, Sophie Giusiano4, Jean-Philippe Dales4, Mélanie Gaubert4, Marc Laine4, Philippe Lacoste1, Christian Perigaud1, Jean-Christian Roussel1, Thomas Senage1, Antoine Mugniot1, Isabelle Danner1, Adrien Tissot1, Charlotte Bry1, Morgane Penhouet1, Emmanuelle Eschapasse1, Delphine Horeau-Langlard1, François-Xavier Blanc1, Thierry Lepoivre1, Mickael Vourch1, Sophie Brouard1, Richard Danger1, Megguy Bernard1, Elodie Godard1, Régine Valéro1, Karine Maugendre1, Eugénie Durand1, Nataliya Yeremenko1, Aurore Foureau1, David Lair1, Géraldine Gallot1, Mathilde Berthome1, Jérôme Le Pavec12, Gaëlle Dauriat12, Pauline Pradere12, Séverine Feuillet12, Samuel Dolidon12, Chahine Medraoui12, Pierre Gazengel12, Adrian Crutu12, Amir Hanna12, Elie Fabre, Olaf Mercier, Delphine Mitilian, Justin Issard, Dominique Fabre, Yves Castier11, Pierre Mordant11, Pierre Cerceau11, Antoine Girault11, Arnaud Roussel11, Enora Atchade-Thierry11, Sylvain Jean-Baptiste11, Sandrine Boudinet11, Sébastien Tanaka11, Aurélie Gouel11, Philippe Montravers11, Nathalie Zappella11, Aurélie Snauwaert11, Parvine Tashk11, Brice Lortat-Jacob11, Tiphaine Goletto11, Domitille Mouren11, Lise Morer11, Mathilde Salpin11, Hervé Mal11, Armelle Marceau11, Gaëlle Weisenburger11, Vincent Bunel11, Adèle Sandot11, Kinan El Husseini11, Pierre Halitim11, Lucie Genet11, Sabrina Trigueiros11, Alice Savary11, Hakima Rabia11, Pierre-Emmanuel Falcoz5,6, Anne Olland5,6, Charlotte Ponte5,6, Charles Tacquard5,6, Garib Ajob5,6, Olivier Collange5,6, Antoine Pons5,6, Xavier Delabranche5,6, Olivier Helms5,6, Anne Roche5,6, Benjamin Renaud-Picard5,6, Romain Kessler5,6, Tristan Degot5,6, Sandrine Hirschi5,6, Armelle Schuller5,6, Anne Dory5,6, Florence Toti5,6, Nadia Benkirane-Jessel5,6, Laurence Kessler5,6, Julien Stauder5,6, Edouard Sage7, Francois Parquin7, Sandra De Miranda7, Clément Picard7, Antoine Roux7, Olivier Brugière7, Béatrice D’Urso7, Marc Stern7, Akounach Mbarka7, Antoine Magnan7, Quentin Marquant7, Isabelle Schwartz7, Helene Salvator7, Tiffany Pascreau7, Thomas Villeneuve13, Marion Dupuis13, Marlène Murris-Espin13, Pierre Rabinel13, Laurent Brouchet13, Laure Crognier13, Olivier Mathe13, Frédérique Legenne13, Myriam Barthes13, Blandine Vilquin13, Anne-Laure Costes13, Isabelle Recoche13, Anne Bergeron, Gregory Berra, Angela Koutsokera
Funding
This work was supported by the ANR project PRELUD (ANR-18-CE17-0019), The Institut de Recherche en Santé Respiratoire des Pays de Loire, the Fondation du Souffle and the Fonds de Recherche en Santé Respiratoire according the fundings Cohorte en Pneumologie 2017 and Plates-Formes et Recherche en Santé Respiratoire 2020. The Cohort in Lung Transplantation was funded by Vaincre La Mucoviscidose and l'Association Grégory Lemarchal, the French Research Ministry (Agence Nationale de la Recherche grant), the French Government (Programme Hospitalier de Recherche Clinique—DGOS 20-11), the European Union (FP7 collaborative project HEALTH.2012.2.1.2-1—grant agreement number: 305457) and Nantes Metropole.
The study sponsor(s) or funder(s) had no role in the study design, the collection, analysis, and interpretation of data, in the writing of the report or in the decision to submit the article for publication. Researchers were independent to funders, and all authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Contributions
AT, RD and SB developed the concept and designed the experiments. ED processed the samples and performed the experiments. AT and TG analysed the data. AT wrote the manuscript. RD, SB, LB and DL performed a critical review of the manuscript. BRP, BC, AR, JL, TV, LF, and XD revised the manuscript. AR, BRP, BC, JL, MS, JFM, LF, VB, CK, TV, and AT enrolled the participants and collected samples.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted in accordance with the Declaration of Helsinki and complies with:
• Articles L. 1121-1 to L. 1126-12 of the French Public Health Code concerning research involving the human body.
• the French Data Protection Act of January 6, 1978, as amended, and Act no. 2018–493 of June 20, 2018 on the protection of personal data.
• Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of individuals with regard to the processing of personal data and on the free movement of such data (RGPD).
The protocol has received the approval of the Ethic Committee on 24th February 2009, and the authorization from the French regulatory authority (AFSSASP/ANSM) on 5th February 2009. The protocol is also registered to the CNIL (national committee for data processing and liberties) and approved on 16th September 2011. The University Hospital Ethical Committee of Nantes and the Committee for the Protection of Patients from Biologic Risks approved this study.
Lung transplant recipients (LTRs) were recruited within the multicentre COhort in Lung Transplantation [COLT], NCT00980967) study (Comité de Protection des Personnes Ouest 1-Tours, 2009-A00036-51). The study was approved by the local ethical committee, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
AT and BC declare competing interests with Biotest. tSB and RD have ownership interests in the BioMAdvanced Diagnostics company. TV declares competing interests with Boeringer Ingelheim and Mauna Kea. The other authors declare no competing interests. All authors have completed the ICMJE uniform disclosure form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: S1.
COLT study protocol. S2. Description of variables of interest. Figure S1. Study protocol. Figure S2. Comparison of MMP-9 blood levels of Y2 analysis according to CLAD phenotypes. Figure S3. Precision-Recall (A) and ROC (B) curves for the Y1 MMP-9 analysis. Figure S4. Comparison of MMP-9 blood levels of Y2 analysis according to CLAD phenotypes. Figure S5. Longitudinal analysis of MMP-9 blood levels for recipients with available samples before transplantation, at Y1 and Y2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tissot, A., Durand, E., Goronflot, T. et al. Blood MMP-9 measured at 2 years after lung transplantation as a prognostic biomarker of chronic lung allograft dysfunction. Respir Res 25, 88 (2024). https://doi.org/10.1186/s12931-024-02707-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02707-3