Abstract
Background
While regular cigar smoking is believed to carry similar health risks as regular cigarette smoking, the impact of cigar use, alone or in combination with cigarettes, on obstructive pulmonary disease (COPD) has not been well characterized. The purpose of this study was to examine the prospective association between exclusive and dual cigar and cigarette use and incident self-reported diagnosed COPD.
Methods
This study used data from Waves 1–5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) Study, a nationally representative survey of U.S. adults. Longitudinal data from adults aged 40 to 79 at Wave 1, without a pre-existing COPD diagnosis who participated at follow-up interview were analyzed. A time-varying current tobacco exposure, lagged by one wave and categorized as: (a) never/non-current use; (b) exclusive cigar use; (c) exclusive cigarette use; and (d) dual cigar/cigarette use. Multivariable models adjusted for demographics (age, sex, race or ethnicity, education), clinical risk factors (asthma, obesity), and smoking-related confounders (second-hand smoke exposure, other combustible tobacco product use, e-cigarette use, time since quitting, cigarette pack-years). The incidence of self-reported diagnosed COPD was estimated using discrete-time survival models, using a general linear modeling (GLM) approach with a binomial distribution and a complementary log-log link function.
Results
The analytic sample consisted of 9,556 adults with a mean (SD) age of 56 (10.4), who were predominately female (52.8%) and Non-Hispanic White (70.8%). A total of 906 respondents reported a diagnosis of COPD at follow-up. In the fully adjusted model, exclusive cigar use (adjusted hazard ratio (aHR) = 1.57, 95% CI: 0.77, 3.21) was not associated with increased COPD risk compared to non-use, while exclusive cigarette use (aHR = 1.48, 95% CI: 1.13, 1.93) and dual cigar/cigarette use (aHR = 1.88, 95% CI: 1.24, 2.85) were.
Conclusions
Exclusive cigarette use and dual cigar/cigarette use were associated with diagnosed incident COPD. These results suggest that cigars, when used in combination with cigarettes, may be associated with poorer COPD health outcomes. Dual use may promote a higher likelihood of inhaling cigar smoke, and future research would benefit from examining whether inhalation of cigar smoke increases COPD risk.
Similar content being viewed by others
Introduction
While United States (US) cigarette smoking prevalence among adults has steadily declined over the past two decades, cigar use has remained relatively stable [1]. US cigar sales increased between 2009 and 2020 [2], demonstrating the increasingly important role of cigars in the US tobacco marketplace. With 3.5% of US adults reporting current cigar use in 2020 [3], cigars represent a key public health concern, highlighting the need to better understand the health effects of cigar smoking [4].
Cigars contain many of the same hazardous constituents as cigarette smoke [5], and regular cigar smoking is believed to carry similar health risks as regular cigarette smoking [4,5,6]. A few studies have associated cigar use with lung dysfunction [7, 8], chronic obstructive pulmonary disease (COPD) [9, 10], and COPD-related mortality risk [4, 11]. However, the respiratory impact of cigar use is not well characterized as most adults who use cigars also use cigarettes, which many studies overlook. Moreover, there is a dearth of research examining the association between cigar use and COPD using longitudinal and population-based data.
Establishing an association between cigar use and COPD is complicated by the fact that the majority of adults who smoke cigars also smoke cigarettes [12], and cigarette smoking is a major risk factor for COPD [13,14,15]. The age-adjusted COPD prevalence of 14.1% among adults who currently smoke cigarettes and 7.1% among adults who formerly smoked cigarettes [16] demonstrates that a large proportion of COPD’s health and economic burden can be directly attributed to cigarette smoking [15]. Therefore, studies documenting the association between cigar smoking and COPD risk must adjust for cigarette smoking histories, including smoking status, duration, and intensity.
In this study, we examined the prospective association between exclusive and dual cigar and cigarette use and incident self-reported diagnosis of COPD among a nationally representative cohort of US adults. We (1) examined the risk of COPD prospectively; (2) developed a one-wave lagged exposure variable combining current cigar use and cigarette use to examine the relative contribution of exclusive cigar use and cigarette use and dual cigar/cigarette use to COPD risk, compared to non-use; and (3) adjusted for the duration, intensity, and history of cigarette smoking by adjusting for cigarette pack-years.
Methods
Study design and population
We used restricted-access data on adults from Waves 1–5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) Study, a nationally representative longitudinal study of the non-institutionalized civilian US population [17]. Details on the PATH Study are described elsewhere [18]. Information on accessing the restricted use data is described in the PATH Study Restricted Use Files User Guide at: https://doi.org/10.3886/Series606.21.
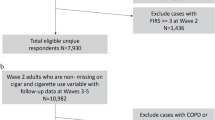
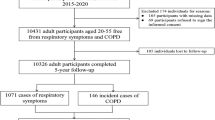
Consistent with the inclusion criteria from other national COPD cohort studies, we restricted the analytic sample to adult respondents aged 40 to 79 at Wave 1 (baseline) [19, 20] without a pre-existing COPD diagnosis (i.e., COPD, chronic bronchitis, or emphysema) who participated in at least one follow-up interview (Supplemental Fig. 1) [21]. We also excluded adults who exclusively smoked premium cigars for three reasons: compared to other types of cigar use, exclusive premium cigar use is (1) less likely to represent true established use [5], (2) less frequent (defined by the number of days used in the past 30 days) [22, 23], and (3) less likely to be used by adults who smoke cigarettes [22, 23]. These different usage patterns result in lower levels of toxicant exposure, potentially confounding the association between other types of cigar use and COPD [5].
Measures
Self-reported diagnosed COPD incidence at each follow-up interview was based on the question: “In the past 12 months, has a doctor, nurse, or other health professional told you that you had…(1) COPD, (2) chronic bronchitis, or (3) emphysema?” Consistent with the clinical definition of COPD [24], respondents who reported being diagnosed with any of these conditions were considered to have COPD at follow-up.
Current cigar use was defined as established (ever used cigars fairly regularly) every day or someday use of traditional cigars, filtered cigars, or cigarillos in the past 30 days. Current cigarette use was defined as established (smoked 100 or more cigarettes in their lifetime) every day or someday use in the past 30 days. These two variables were then used to construct a four-category, time-varying cigar/cigarette exposure: (1) non-current use of either product (including never use and former use), (2) exclusive cigar use, (3) exclusive cigarette use, and (4) dual use of cigars and cigarettes. To ensure the cigar/cigarette exposure preceded the outcome, we lagged the time-varying exposure variable by one wave (t-1) and evaluated its association with the COPD outcome at wave (t).
Several baseline sociodemographic and health factors were included as covariates, including age (continuous), sex (male, female), race and ethnicity (Hispanic, non-Hispanic (NH) White, NH Black, another race and ethnicity), and education (high school or less, some college, bachelor’s degree/graduate degree). Obesity (body mass index (BMI) ≥ 30 vs. < 30), based on self-reported height and weight, and ever self-reported diagnosis of asthma were included as baseline COPD risk factors. Exposure to second-hand smoke (number of hours of ‘close’ exposure during the past seven days (range 0-100)) was included as a time-varying and lagged (t-1) COPD risk factor.
Several additional covariates were included to account for potential tobacco-related confounding. First, electronic nicotine delivery systems (ENDS) and ‘other’ combustible tobacco product use (pipes, hookah) were included as covariates. Both variables were based on current established use (ever use fairly regularly), and both variables were included as time-varying exposures, lagged by one wave (t-1). Second, using former established smoking (smoked at least 100 cigarettes in lifetime, but no current use) and years since quitting, a categorical time since quitting variable was constructed (non-former smoking, short-term quitting, long-term quitting). Non-former smoking includes never established and current smoking, while short-term quitting refers to former smokers who quit less than two years ago, and long-term smoking refers to former smokers who quit two or more years ago. Finally, cigarette pack-years were included to measure lifetime cigarette smoking at baseline. Cigarette pack-years were calculated by multiplying the reported years of cigarette smoking by the average number of packs per day while individuals smoked. Respondents who reported smoking more than 200 cigarettes daily (10 packs per day) were considered implausible and were set to missing (n = 99).
Statistical analysis
Descriptive statistics were calculated for all variables at baseline. Tobacco-related variables were then examined according to respondent’s baseline cigar and cigarette use. Chi-square tests or Fisher’s exact tests were used to test for statistical differences between these groups. Lifetables were then generated to describe the distribution of self-reported diagnosed COPD.
Discrete-time survival models were used to examine the prospective association between exclusive and dual use of cigars and cigarettes and incident self-reported diagnosis of COPD at follow-up (Wave 2-Wave 5). These models provide the discrete-time equivalent to continuous time survival models [25], and we have used this methodological framework in previous health effects research [21, 26, 27]. Hazard ratios (HRs) and 95% confidence intervals (CIs) were fit using a general linear modeling (GLM) approach with a binomial distribution and a complementary log-log link function. All data were weighted using Wave 1 weights, including full-sample and 100 replicate weights, to ensure respondents represented the non-institutionalized US adult population at baseline. For all analyses, variances were computed using the balanced repeated replication methods with Fay’s adjustment set to 0.3, as recommended by the PATH study [28, 29]. All analyses were conducted using Stata 17.1 [30].
Sensitivity tests
Several sensitivity analyses were conducted. First, to better understand how cigarette and cigar smoking histories impact COPD, we constructed a nine-category mutually exclusive cigarette/cigar exposure that disaggregated non-use into never and former use: (1) never cigarette or cigar use, (2) never cigarette use, former cigar use, (3) never cigarette use, current cigar use, (4) former cigarette use, never cigar use, (5) current cigarette use, never cigar use, (6) former cigarette use, former cigar use, (7) former cigarette use, current cigar use, (8) current cigarette use, former cigar use, (9) current cigarette use, current cigar use. Second, to assess sensitivity to the choice of PATH survey weights, ‘wave 2 weights,’ which restricted the analysis to respondents who participated in the first follow-up interview, and the ‘all waves weights,’ which restricted the analysis to the longitudinal cohort of respondents who participated in all waves of the PATH study were both considered. To test the impact of our decision to remove adults who used exclusive premium cigars from the analytic sample, discrete-time models were estimated, including these respondents. Finally, because research suggests that COPD may be prevalent among younger adults [31], we expanded our analytic sample to include adult respondents aged 25–39.
Results
At baseline, sample respondents (\(n\)=9,559) had a mean age of 56 years (SD = 10.4) and were predominately female (52.8%), NH White (70.8%), and with some postsecondary education (61.4%) (Table 1). Approximately one-third of respondents had a BMI of 30 kg/m2 or more (34.3%), and 8.9% reported a lifetime diagnosis of asthma at baseline. Most respondents did not have current cigar or cigarette use at baseline (85%). Of those, 2.2% had short-term former cigarette use, and 20.6% had long-term former cigarette use. Among respondents with current or former established cigarette smoking, the average cigarette pack-years at baseline was 25.9 (SD = 26.3). Regarding exposure to second-hand smoke, 42.4% reported past 7-day exposure to second-hand smoke, with an average 10.2 h (SD = 22.1) of exposure. At baseline, 13.6% of respondents (n = 3,173) reported exclusive cigarette use, while exclusive cigar use and dual cigar/cigarette use was reported by 0.6% (n = 134) and 0.8% (n = 184) of respondents, respectively.
Compared to adults who exclusively smoked cigars, adults who smoked cigarettes exclusively or in combination with cigars had higher levels of second-hand smoke exposure (Table 2). Among adults who smoke cigars, traditional cigars were more likely to be used (54.7%) and were used on more days during the past month (x = 9.6) by those who exclusively smoke cigars than by those who smoke cigars and cigarettes (36.4%; x = 5.2). In contrast, filtered cigars were more likely to be used by adults who smoke cigars and cigarettes (55.9%) and were used on more days during the past month (x = 11.0) than those who smoke cigars exclusively (27.4%; x = 5.9). Cigarillos (48.5% vs. 44.8%) and poly cigar types (27.3% vs. 29.7%) were not statistically different between the two groups of cigar use.
A total of 906 of the 9,559 respondents in the analytic sample reported a COPD diagnosis at follow-up (Table 3). The weighted conditional probability of a COPD diagnosis ranged between 1.4% and 2.4%, with an average incidence of 2% during the five years of follow-up.
The results from discrete-time models examining the association between the cigar/cigarette exposure and incident COPD outcome are presented in Table 4. When compared to non-current use in the unadjusted model (Model 1), exclusive cigarette use (hazard ratio (HR) = 2.91, 95% CI: 2.45, 3.33), and dual cigar/cigarette use (HR = 3.73, 95% CI: 2.61, 5.30) were both associated with an increased risk of incident COPD risk, while exclusive cigar use was not (HR = 1.29, 95% CI: 0.65, 5.30). After adjusting for sociodemographic risk factors, baseline risk factors, and tobacco-related variables, the point estimates were reduced for exclusive cigarette and cigarette/cigar use, but the substantive interpretation remained the same. In the multivariable model (Model 4), both exclusive cigarette use (adjusted hazard ratio (aHR) = 1.48, 95% CI: 1.13, 1.93), and dual cigar/cigarette use (aHR = 1.88, 95% CI: 1.24, 2.85) were associated with increased COPD risk compared to non-current use, while exclusive cigar use was not (aHR 1.57, 95% CI: 0.77, 3.21).
Sensitivity analyses
Compared to never established use of cigars or cigarettes, current cigarette use/never cigar use (aHR 1.61, 95% CI 1.17, 2.23) and dual cigar/cigarette use (aHR 2.06, 95% CI 1.31, 3.24) were associated with increased risk of incident COPD in the multivariable model (Table S1, Model 3). Discrete-time models were also estimated using PATH Wave 2 weights (Table S2) and PATH “all-waves weights” (Table S3); with exclusive premium cigar use included in the analytic sample (Table S4) and with the analytic sample extended to include adult respondents aged 25 to 79 at baseline (Table S5). Across all sensitivity analyses, the substantive results remained consistent: exclusive cigar use was not associated with incident COPD risk, while exclusive cigarette and dual cigar/cigarette use were.
Discussion
Using nationally representative data from the PATH cohort study, we examined the prospective association between cigars, cigarettes, and incident COPD among US adults aged 40 to 79. We found that time-varying exclusive cigarette use and baseline cigarette pack-years were both associated with increased incident COPD, which was expected since current cigarette smoking [32] and cumulative smoking [14, 33, 34] are major COPD risk factors. Consistent with other cigar research [1, 12], most adults with established cigar use had established histories of cigarette smoking, time-varying dual use of cigars and cigarettes was associated with an increased risk of incident COPD compared to non-current use in models accounting for current cigarette use and cigarette pack-years. However, we did not find an association between time-varying exclusive cigar use and incident COPD risk compared to non-current use.
Adults with dual cigar/cigarette use had different tobacco-related use profiles than adults who used cigars or cigarettes exclusively. Compared to the exclusive use of either product, people who used cigars and cigarettes had higher levels of second-hand smoke exposure and higher cigarette pack-years. While these risk factors are important for determining whether tobacco use will lead to COPD [33, 35], adjusting for these tobacco-related differences did not attenuate the association between dual cigar/cigarette use and incident COPD in multivariable models. This suggests that factors other than cigarette smoking histories may be salient. For instance, while the small number of adults with current established cigar use in our study limited our ability to disaggregate cigar use by cigar type in models, filtered cigar use was more prevalent and smoked more frequently by adults with dual cigar/cigarette use. By contrast, traditional cigar use was more prevalent and smoked more frequently by adults with exclusive cigar use. Filtered cigars have been marketed as an inexpensive cigarette substitute [36], and associated with higher levels of cigar smoking frequency and intensity [22]. It is possible that the dual cigar/cigarette association is driven by higher levels of exposure based on differences in cigar type use, and examining the health effects separately by cigar type should be considered in future research. Conversely, inhalation of cigar smoke is known to be a key determinant of cigar-related health outcomes [4], and adults who smoke cigarettes are more likely than cigarette naïve cigar smokers to inhale cigar smoke [4, 37]. It is also possible that the dual cigar/cigarette association may be driven by the inhalation of cigar smoke by adults who smoke cigarettes; cigar inhalation behavior should also be considered in future research on the health effects of cigar use.
We did not observe an association between exclusive cigar use and incident COPD over the 5-year follow-up period. This finding is consistent with the results from another recently published study using PATH data [38]. In this study, Paulin et al. examined the association between 12 categories of current tobacco product use and COPD, and found that exclusive past 30-day cigar use (n = 391) was not associated with incident COPD risk compared to adults who never used tobacco [38]. However, in our study, while exclusive cigar use was not statistically associated with COPD risk, we observed an elevated hazard ratio compared to non-current use (aHR = 1.57) that was similar in magnitude to the hazard ratio for exclusive cigarette use (aHR = 1.48), albeit not statistically significant. The wide confidence intervals associated with the exclusive cigar use hazard ratio (95% CI 0.77, 3.21) suggests a lack of power, which is important to note given our exclusive cigar use sample was small (n = 130 at baseline). The main reason our sample of exclusive cigar users was smaller than the sample in the Paulin et al. study was because we excluded respondents who exclusively smoked premium cigars from our analytic sample because they are used less frequently than other cigar types and are less likely to represent true established use [5]. In a sensitivity analysis where exclusive premium cigar users were included in the analytic sample (Table S5), the number of respondents in the exclusive cigar use group increased, but the hazard ratios were lower (unadjusted HR = 0.97; fully adjusted HR = 1.29). Since exclusive premium cigar use is likely to have a different COPD risk profile compared to other types of cigar use, it is important to distinguish premium use from non-premium use.
Cigars and cigarettes are known to emit similarly harmful chemical constituents [5], and there is strong biological plausibility that exposure to regular cigar use, particularly if the smoke is inhaled, will be associated with increased risk of deleterious health outcomes [5], including increased COPD risk [9, 10]. In this study, the lower levels of COPD risk observed among people with exclusive cigar use compared to dual use is likely due to the lower frequency of use among exclusive cigar users, which results in less regular exposure to the harmful constituents of cigar smoke compared to dual use. It remains likely that frequent cigar use, especially when the cigar smoke is inhaled, will increase COPD risk independent of cigarette smoke. With the expansion of the cigar market in the US, future studies with greater statistical power are needed to evaluate the COPD risk associated with exclusive cigar use.
There are several important limitations to note. First, the results from this study are based on self-reported incident diagnosed COPD rather than on results from a spirometry test. This is a limitation of the PATH data. Still, the COPD prevalence estimates in PATH are generally consistent with those from the National Health and Nutritional Examination Survey [38]. Prior research has also demonstrated concurrent validity with other self-reported PATH health outcomes [39]. Second, PATH does not collect information on the level of cigar use inhalation, which has been strongly associated with negative health outcomes [5]. Future iterations of PATH would benefit from including inhalation questions for adults who smoke cigars. Third, the current research included cigarette pack-years as a measure of lifetime cigarette use but did not include an analogous measure of lifetime cigar use. Developing a standardized measure of lifetime cigar use is an important task for future research as it would allow for an estimate of lifetime frequency and intensity of cigar use on respiratory health. Fourth, the few respondents using cigars at each wave may have limited power to detect an association between exclusive cigar use and COPD. Moreover, the relatively small sample of adults with established cigar use meant it was not possible to disaggregate traditional cigars from cigarillos and filtered cigars. Given the important differences across cigar types [22, 23], future research would benefit from looking at the respiratory health effects of filtered cigar use separately from cigarillos and traditional cigars. Larger, more diverse cohorts that oversample adults who use cigars may be able to build on our analyses and further examine the complexities of cigar use behavior.
Conclusions
In summary, our longitudinal analysis of the prospective association between cigar and cigarette use and incident diagnosed COPD provides evidence that exclusive cigarette use and dual cigar/cigarette use were associated with increased COPD risk. These findings remained statistically significant after controlling for confounders, including cigarette pack-years, providing evidence that cigar use, especially combined with cigarettes, is an independent risk factor for COPD. As cigars continue to play an increasingly important role in the US tobacco marketplace, our results demonstrate the need to implement policies designed to reduce the prevalence of cigar use.
Data availability
The current study used restricted use data from the PATH Study because the analysis included cigarette pack-years and continuous age. Information on accessing the restricted use data is described in the PATH Study Restricted Use Files User Guide at: https://doi.org/10.3886/Series606.21.
Change history
23 February 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12931-024-02728-y
References
Rostron BL, Corey CG, Gindi RM. Cigar Smoking prevalence and morbidity among US adults, 2000–2015. Prev Med Rep. 2019;14:100821.
Delnevo CD, Lo EM, Giovenco DP, Ross JC, Hrywna M, Strasser AA. Cigar sales in convenience stores in the US, 2009–2020. JAMA. 2021;326(23):2429–32.
Cornelius ME, Loretan CG, Wang TW, Jamal A, Homa DM. Tobacco product use among adults—United States, 2020. Morb Mortal Wkly Rep. 2022;71(11):397.
Chang CM, Corey CG, Rostron BL, Apelberg BJ. Systematic review of cigar Smoking and all cause and Smoking related mortality. BMC Public Health. 2015;15(1):1–20.
National Academies of Sciences E., Medicine. Premium Cigars: Patterns of Use, Marketing, and Health Effects. 2022.
Baker F, Ainsworth SR, Dye JT, et al. Health risks associated with cigar Smoking. JAMA. 2000;284(6):735–40.
Jiménez-Ruiz C, Sobradillo V, Gabriel R, et al. Respiratory symptoms and diagnosis of COPD in smokers of various types to Tobacco. Results from the IBERPOC study. Arch Bronconeumol. 2002;38(11):530–5.
Rodriguez J, Jiang R, Johnson WC, MacKenzie BA, Smith LJ, Barr RG. The association of pipe and cigar use with cotinine levels, lung function, and airflow obstruction: a cross-sectional study. Ann Intern Med. 2010;152(4):201–10.
Iribarren C, Tekawa IS, Sidney S, Friedman GD. Effect of cigar Smoking on the risk of Cardiovascular Disease, Chronic Obstructive Pulmonary Disease, and cancer in men. N Engl J Med. 1999;340(23):1773–80.
Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung Disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160(11):1683–9.
Christensen CH, Rostron B, Cosgrove C, et al. Association of cigarette, cigar, and pipe use with mortality risk in the US population. JAMA Intern Med. 2018;178(4):469–76.
Edwards KC, Sharma E, Halenar MJ, et al. Longitudinal pathways of exclusive and polytobacco cigar use among youth, young adults and adults in the USA: findings from the PATH study waves 1–3 (2013–2016). Tob Control. 2020;29(Suppl 3):163–s169.
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung Disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–82.
Løkke A, Lange P, Scharling H, Fabricius P, Vestbo J. Developing COPD: a 25 year follow up study of the general population. Thorax. 2006;61(11):935–9.
Zafari Z, Li S, Eakin MN, Bellanger M, Reed RM. Projecting Long-Term Health and Economic Burden of COPD in the United States. Chest. 2021;159(4):1400–10.
Cunningham TJ, Ford ES, Rolle IV, Wheaton AG, Croft JB. Associations of self-reported cigarette Smoking with Chronic Obstructive Pulmonary Disease and co-morbid chronic conditions in the United States. COPD: J Chronic Obstr Pulmonary Disease. 2015;12(3):281–91.
United States Department of H, Human Services. National Institutes of Health. National Institute on Drug A, United States Department of H, Human Services F, Drug Administration. Center for Tobacco P. Population Assessment of Tobacco and Health (PATH) study [United States] restricted-use files. Inter-university Consortium for Political and Social Research [distributor]; 2021.
Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob Control. 2017;26(4):371–8.
Couper D, LaVange LM, Han M, et al. Design of the subpopulations and intermediate outcomes in COPD study (SPIROMICS). Thorax. 2014;69(5):492–5.
Tilert T, Paulose-Ram R, Howard D, Butler J, Lee S, Wang MQ. Prevalence and factors associated with self-reported Chronic Obstructive Pulmonary Disease among adults aged 40–79: the National Health and Nutrition Examination Survey (NHANES) 2007–2012. EC Pulmonol Respiratory Med. 2018;7(9):650–62.
Cook SF, Hirschtick JL, Fleischer NL et al. Cigarettes, ENDS Use, and Chronic Obstructive Pulmonary Disease incidence: a prospective longitudinal study. Am J Prev Med. 2023.
Corey CG, Holder-Hayes E, Nguyen AB, et al. US adult cigar Smoking patterns, purchasing behaviors, and reasons for use according to cigar type: findings from the Population Assessment of Tobacco and Health (PATH) study, 2013–2014. Nicotine and Tobacco Research. 2018;20(12):1457–66.
Corey CG, King BA, Coleman BN, et al. Little filtered cigar, cigarillo, and premium cigar Smoking among adults—United States, 2012–2013. Morb Mortal Wkly Rep. 2014;63(30):650.
Phan L, McNeel TS, Choi K. Prevalence of current large cigar versus little cigar/cigarillo Smoking among US adults, 2018–2019. Prev Med Rep. 2021;24:101534.
Singer JD, Willett JB, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford university press; 2003.
Cook S, Hirschtick JL, Barnes G, et al. Time-varying association between cigarette and ENDS use on incident Hypertension among US adults: a prospective longitudinal study. BMJ open. 2023;13(4):e062297.
Hirschtick JL, Cook S, Patel A, et al. Longitudinal associations between exclusive and dual use of electronic nicotine delivery systems and cigarettes and self-reported incident diagnosed Cardiovascular Disease among adults. Nicotine and Tobacco Research. 2023;25(3):386–94.
Judkins DR. Fay’s method for variance estimation. J Official Stat. 1990;6(3):223–39.
Piesse A, Opsomer J, Dohrmann S, et al. Longitudinal uses of the Population Assessment of Tobacco and Health Study. Tob Regul Sci. 2021;7(1):3–16.
StataCorp. Stata Statistical Software: Release 17. In. College Station. TX: Stata Corp LLC; 2021.
Akinbami OJ, Liu X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. US Department of Health and Human Services, Centers for Disease Control and … 2011.
Kamal R, Srivastava AK, Kesavachandran CN. Meta-analysis approach to study the prevalence of Chronic Obstructive Pulmonary Disease among current, former and non-smokers. Toxicol Rep. 2015;2:1064–74.
Chang JT, Meza R, Levy DT, Arenberg D, Jeon J. Prediction of COPD risk accounting for time-varying Smoking exposures. PLoS ONE. 2021;16(3):e0248535.
Gotts JE, Jordt S-E, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? bmj 2019;366.
Fischer F, Kraemer A. Meta-analysis of the association between second-hand smoke exposure and ischaemic Heart Diseases, COPD and Stroke. BMC Public Health. 2015;15(1):1–18.
Delnevo CD, Hrywna M, Giovenco DP, Lo EJM, O’Connor RJ. Close, but no cigar: certain cigars are pseudo-cigarettes designed to evade regulation. Tob Control. 2017;26(3):349–54.
Benowitz NL, Liakoni E. Tobacco use disorder and cardiovascular health. Addiction. 2022;117(4):1128–38.
Paulin LM, Halenar MJ, Edwards KC, et al. Association of Tobacco product use with Chronic Obstructive Pulmonary Disease (COPD) prevalence and incidence in waves 1 through 5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) study. Respir Res. 2022;23(1):1–13.
Mahoney MC, Rivard C, Hammad HT, et al. Cardiovascular risk factor and Disease measures from the Population Assessment of Tobacco and Health (PATH) study. Int J Environ Res Public Health. 2021;18(14):7692.
Funding
Supported by NIH/FDA grant U54CA229974. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Author information
Authors and Affiliations
Contributions
Conceptualization, SC, JB; Methodology, SC, JB; formal analysis, SC, RM, Resources, NF, DL, RM; Writing-review and editing, SC, JB, DL, RM, NF; Supervision: RM, NF. All authors have read and agreed to publish this version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted by Westat and approved by the Westat institutional review board. Deidentified data were used and no personal identifying information was included in the manuscript. This study was approved by the ethics committee at the University of Michigan (HUM00153979). The participants gave informed consent to participate in the study before taking part.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of the article was revised: The author James H. Buszkiewicz has been corrected.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cook, S., Buszkiewicz, J.H., Levy, D.T. et al. Association between cigar use, with and without cigarettes, and incident diagnosed COPD: a longitudinal cohort study. Respir Res 25, 13 (2024). https://doi.org/10.1186/s12931-023-02649-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-023-02649-2