Abstract
Background
Mechanical thrombectomy has been shown to reduce thrombus burden and pulmonary artery pressure (PAP) and to improve right ventricular (RV) function in patients with high-risk or intermediate-high-risk pulmonary embolism (PE). As hemodynamic data after mechanical thrombectomy for PE are scarce, we aimed to assess the hemodynamic effects of mechanical thrombectomy in acute PE with right heart overload.
Methods
In this prospective, open-label study, patients with acute symptomatic, computed tomography-documented PE with signs of right heart overload underwent mechanical thrombectomy using the FlowTriever System. Right heart catheterization was performed immediately before and after thrombectomy and after three months. Transthoracic echocardiography was performed before thrombectomy, discharge, and at three months. This analysis was done after 20 patients completed three months of follow-up.
Results
Twenty-nine patients (34% female) underwent mechanical thrombectomy, of which 20 completed three months follow-up with right heart catheterization. Most patients were at high (17%) or intermediate-high (76%) risk and had bilateral PE (79%). Before thrombectomy, systolic PAP (sPAP) was severely elevated (mean 51.3 ± 11.6 mmHg). Mean sPAP dropped by -15.0 mmHg (95% confidence interval [CI]: -18.9 to -11.0; p < 0.001) immediately after the procedure and continued to decrease from post-thrombectomy to three months (-6.4 mmHg, 95% CI: -10-0 to -2.9; p = 0.002). RV/left ventricular (LV) ratio immediately reduced within two days by -0.37 (95% CI: -0.47 to -0.27; p < 0.001). The proportion of patients with a tricuspid annular plane systolic excursion (TAPSE)/sPAP ratio < 0.31 mm/mmHg decreased from 28% at baseline to 0% before discharge and at three months (p = 0.007). There were no procedure-related major adverse events.
Conclusions
Mechanical thrombectomy for acute PE was safe and immediately reduced PAP and improved right heart function. The reduction in PAP was maintained at three months follow-up.
Similar content being viewed by others
Background
Pulmonary embolism (PE) remains the leading cause of preventable death in hospitalised patients [1, 2]. The 2019 European Society of Cardiology (ESC) Guidelines recommend a risk-adjusted approach for the management of acute PE by stratifying the risk of early death based on clinical and hemodynamic parameters [3]. In low- and intermediate-low-risk patients, treatment consists of therapeutic anticoagulation [3]. Patients with high-risk PE appear to benefit from reperfusion therapy, i.e. systemic thrombolysis [3]. However, systemic thrombolysis is underused, associated with bleeding complications, occasionally fails, [4,5,6] and is contraindicated in a subset of patients [5]. Additionally, patients with intermediate-high-risk PE do not benefit from systemic thrombolysis as bleeding complications often outweigh potential hemodynamic improvements [4, 7].
Whenever systemic lysis fails or is contraindicated, catheter-directed reperfusion treatment should be considered in patients with high-risk PE [3, 8,9,10]. In the FlowTriever Pulmonary Embolectomy (FLASH) study [11] and a large registry, [12] transcatheter thrombus aspiration using the FlowTriever System (Inari Medical, Irvine, CA) was shown to be feasible and safe in intermediate and high-risk PE. Moreover, mechanical thrombectomy reduced pulmonary artery pressures (PAP) and right ventricle (RV)/left ventricle (LV) ratio acutely after the procedure. However, whether the observed hemodynamic improvements following thrombectomy are maintained through longer-term follow-up is unknown.
Herein, we assessed the safety and the hemodynamic effects of mechanical thrombectomy in acute PE with right heart overload through three months of follow-up.
Methods
Study design and patient selection
This prospective, open-label, single-arm, single-center study assessed the hemodynamic effects of transcatheter mechanical thrombectomy using the FlowTriever System in acute symptomatic PE with right heart overload. This analysis was done after the first 20 patients completed their three months follow-up. Adults (≥ 18 years) with symptoms and clinical signs of acute (symptom duration < 30 days) PE, computed tomography-documented proximal filling defects in at least one main or lobar pulmonary artery, and signs of right heart overload in transthoracic echocardiography or computed tomography were included. Exclusion criteria were inability to receive anticoagulation and life expectancy < 30 days (as determined by the investigator). All patients provided written informed consent. The trial was approved by the local ethics committee (ethic committee of the Ärztekammer des Saarlandes) and complied with the Declaration of Helsinki.
Procedures
All patients had computed tomography to confirm the diagnosis of pulmonary embolism. Transthoracic echocardiography was performed before the thrombectomy.
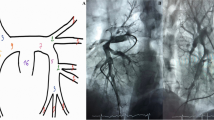
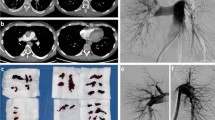
Mechanical thrombectomy was achieved using the FlowTriever System via large-bore transfemoral venous access. Full details of the procedure have been reported previously [11]. In brief, the Triever Catheter (16, 20, or 24 Fr) was advanced over an 0.035” guidewire into the pulmonary arteries for thrombus aspiration. If needed, the FlowTriever Catheter was advanced through the Triever Catheter over the guidewire for mechanical thrombus dislodgment and removal. Pulmonary angiography and right heart catheterization were performed immediately before and after the thrombectomy. A suture-based closure device was used. Procedure time was defined as the time from gaining venous access until sheath removal.
Right heart catheterization and transthoracic echocardiography were repeated at three months of follow-up.
Outcomes
The primary safety outcomes were the number of patients with major adverse events, including major bleeding and periprocedural device- or procedure-related adverse events, between baseline to 48 h and survival at 30 days of follow-up. The efficacy outcomes were changes in sPAP between baseline and three months and changes in RV/LV ratio determined by transthoracic echocardiography from baseline to 48 h. Other outcomes included changes in echocardiographic parameters (tricuspid annular plane systolic excursion (TAPSE), TAPSE/sPAP ratio, and LV ejection fraction), and biomarkers, such as high-sensitivity (hs) troponin T and N-terminal B-type natriuretic peptide (NT-proBNP), as well as lengths of in-hospital stay, and time spent at intensive care unit (ICU).
Statistical analysis
Statistical analyses were done using Stata 16.1 (StataCorp, College Station, TX, USA). Categorical variables are summarized as counts (percentages). Continuous variables are presented as means (standard deviations [SD]) or median (interquartile range [IQR]). The paired t-test or the Wilcoxon signed-ranks test was used to analyze matched pairs. Before-after changes are summarized as means (95% confidence intervals [CI]). McNemar’s (two paired samples) or Cochran’s Q test (more than two paired samples) were used to compare the proportion of patients with mean PAP (mPAP) > 20 mmHg within groups. Pearson’s correlation coefficient was calculated for systolic PAP before thrombectomy and its change during follow-up. All tests were two-sided, and p-values < 0.05 were considered significant.
Results
From April 2021 to August 2022, 29 patients (34% female) were included. The patients’ baseline characteristics are summarized in Table 1. Most patients were at high (17%) or intermediate-high (76%) risk, according to the 2019 ESC acute PE Guidelines [3]. The mean PE severity index (PESI) [13] was 121 ± 38. Bilateral PE occurred in 79% of the patients. The median time from the symptom onset to the procedure was 21 h (IQR: 4–24). The median procedural time was 68 min (IQR: 60–90). The procedural characteristics are summarized in Table 2. The median ICU and in-hospital length of stay were 2 days (IQR: 1–4) and 7 days (IQR: 6–11), respectively. At discharge, 83% of the patients were prescribed direct oral anticoagulants, 3% vitamin K antagonists, and 14% low-molecular-weight heparin (Table 2).
Hemodynamic data
Table 3 summarizes the invasive and non-invasive hemodynamic data. Before thrombectomy, mean sPAP (51.3 ± 11.6 mmHg) and mPAP (29.8 ± 9.1 mmHg) were severely elevated. On table, mean sPAP, diastolic PAP (dPAP), and mPAP dropped by -15.0 mmHg (95%: -18.9 to -11.0; p < 0.001) (Fig. 1), -3.8 mmHg (95% CI: -6.6 to -1.1; p = 0.008), and − 8.4 mmHg (95% CI: -11.0 to -5.8; p < 0.001), respectively. While 2 (7%) patients had an sPAP > 70 mmHg before thrombectomy, none of the patients had an sPAP > 70 mmHg post-thrombectomy.
From post-thrombectomy to three months, mean sPAP (p = 0.002) continued to decrease (Table 3). Compared with before thrombectomy, sPAP (-23.2 mmHg, 95% CI: -28.5 to -17.8; p < 0.001), dPAP (-6.7 mmHg, 95% CI: -11.6 to -1.8; p = 0.010), and mPAP (-12.0 mmHg, 95% CI: -16.8 to -7.2; p < 0.001) were significantly lower at three months. The change in sPAP from pre-thrombectomy to post-thrombectomy (r=-0.76; p < 0.001) and three months (r=-0.80; p < 0.001) strongly correlated with the pre-thrombectomy sPAP (Fig. 2). The proportion of patients with mPAP ≤ 20 mmHg increased on table and continued to increase until three months (Cochran’s Q p = 0.001) (Fig. 3).
The scatter plot shows the correlation and the simple linear regression line (95% confidence interval) between systolic pulmonary artery pressure (PAP) before thrombectomy and its change on table (A) and at from before thrombectomy to 3 months (B). Pearson’s correlation coefficient was calculated for systolic PAP before thrombectomy and its change during follow-up
Heart rate decreased significantly by -27 b.p.m. (95% CI: -35 to -20; p < 0.001) during the procedure, while systolic and diastolic blood pressure (BP) remained unchanged. Of note, patients in the lowest quartile of systolic BP before thrombectomy (mean systolic BP 104 ± 11 mmHg; range: 80 to 115) had an increase in systolic BP by 23 mmHg (95% CI: 14 to 31; p < 0.001) on table, whereas in those in the upper quartile (mean systolic BP 160 ± 5 mmHg; range: 155 to 177), systolic BP decreased by -18 mmHg (95% CI: -30 to -6; p = 0.008). Patients in the second and third quartiles did not have a change in systolic BP (both p > 0.189).
Echocardiographic data
Before thrombectomy, the RV/LV ratio was increased (Table 4) and immediately reduced within two days by -0.37 (95% CI: -0.47 to -0.27; p < 0.001). TAPSE increased from 17.3 ± 6.4 mm pre-procedurally to 20.4 ± 4.0 mm before discharge (+ 3.0 mm; 95% CI: 0.5 to 5.5; p = 0.022). Improvements in right ventricular function were maintained at three months of follow-up. In line, the TAPSE/sPAP ratio, a parameter of RV arterial coupling, [14] tended to increase on table and significantly improved from discharge to three months (Table 4). The proportion of patients with impaired RV-arterial coupling, defined as TAPSE/sPAP ratio < 0.31 mm/mmHg, [14] decreased from 28% (5/18) at baseline to 0% before discharge and at three months (Cochran’s Q p = 0.007).
Clinical outcomes
The peripheral oxygen saturation increased from 93 ± 7% to 97 ± 2% (p = 0.006) from pre- to post-procedure, whereas the supplemental oxygen was reduced from 7 ± 5 l/min to 2 ± 2 l/min (p < 0.001). The arterial lactate level decreased (-1.8 mmol/l; 95% CI: -2.9 to -0.7; p = 0.003) on table. The perceived exertion, as measured using the original Borg CR10 scale, [15] improved on table (from a rating of 7 ± 2 to 3 ± 2; p < 0.001).
Median hs-troponin T decreased from 80 pg/ml (IQR: 55–128) to 25.5 pg/ml (IQR: 18–42) before discharge (median change: -37.5 pg/ml; 95% CI: -89 to -13; p < 0.001) and to 11 pg/ml (IQR: 8–27) at three months (median change from pre-thrombectomy: -58 pg/ml; 95% CI: -131 to -42; p = 0.002). Before thrombectomy, hs-troponin T was increased (> 14 pg/ml) in 97% (28/29) of the patients. Following thrombectomy, the proportion of patients with increased hs-troponin T decreased from 90% (20/22) before discharge to 38% (5/13) at three months (Cochran’s Q for change from baseline to three months p = 0.006).
Likewise, NT-proBNP substantially decreased from 2327 pg/ml (IQR: 1341–4167) to 344 pg/ml (IQR: 140–716) before discharge (median change: -2172 pg/ml; 95% CI: -3661 to -1328; p < 0.001) and to 166 pg/ml (IQR: 82–260) at three months (median change from pre-thrombectomy: -2226.5 pg/ml; 95% CI: -3904 to -1693; p < 0.001).
Safety outcomes
There were no procedure-related major adverse events between baseline to 48 h and survival from baseline to 30 days of follow-up. Importantly, no patient died during 30 days of follow-up.
Discussion
This study assessed whether the hemodynamic effects of mechanical thrombectomy using the FlowTriever System are maintained through three months post-procedure in acute PE with right heart overload. The key findings are: (i) mechanical thrombectomy for acute PE was safe, (ii) immediately reduced PAP, improved right heart function and clinical symptoms, and (iii) mean sPAP continued to decrease through three months of follow-up.
The 2019 ESC Guidelines for the Diagnosis and Management of Acute PE recommend catheter-directed treatment for reperfusion in patients with high-risk PE, in case systemic thrombolysis fails or is contraindicated [3, 7]. The feasibility and safety of mechanical thrombectomy using the FlowTriever System in patients with intermediate and high-risk PE were recently investigated in the multicenter, single-arm FLARE study (n = 104 patients) and the prospective FlowTriever All-Comer Registry for Patient Safety and Hemodynamics (FLASH) (n = 1000 patients). In line with the findings presented herein, in FLARE study [11] and FLASH, the mean RV/LV ratio was immediately reduced by 0.38 and 0.25, respectively [12]. Thrombectomy was also associated with reductions in sPAP and mPAP [11, 12] but the degree of mPAP changes varied across studies (-7.6 mmHg in FLASH [12] versus − 2.0 mmHg in FLARE) [11]. In the present study, mPAP was reduced by -8.4 mmHg. Interestingly, a progressive decline in sPAP was observed through three months of follow-up. This sustained reduction in sPAP could help to prevent the development of post-PE syndrome (PPES), which is defined as new or progressive dyspnea, exercise intolerance, and/or impaired functional or mental status after at least three months of adequate anticoagulation following acute PE, reported in up to 40–60% of PE survivors [16].
Compared with baseline, where 90% of the patients had pulmonary hypertension as defined by mPAP > 20 mmHg, about 35% had sustained mPAP > 20 mmHg at three months. This is of relevance since mPAP elevations > 20 mmHg predict mortality [17,18,19,20]. Therefore, mechanical thrombectomy may improve acute outcomes by disrupting the shock spiral and mortality by reducing pulmonary arterial pressures in the long term. This is supported by the observation that immediately following the procedure (i) oxygen saturation increased while oxygen supply was reduced (-5 l O2 l /min), (ii) arterial lactate level decreased, (iii) heart rate was lowered by 27 bpm, and (iv) hs-troponin T levels normalised. However, mPAP remains elevated in about a third of the patients. This group may include patients with previously undiagnosed pulmonary hypertension and those at increased risk for chronic thromboembolic pulmonary hypertension (CTEPH), requiring further follow-up.
Further, mechanical thrombectomy improved RV function and RV-arterial coupling, assessed using the TAPSE/sPAP ratio. The ratio of TAPSE/sPAP, where TAPSE estimates contractility and sPAP reflects afterload, represents a non-invasive surrogate of end-systolic/arterial elastance (Ees/Ea) ratio and associates with functional class and prognosis in pulmonary hypertension [14, 21, 22].
None of the patients included in this study died within 30 days post-thrombectomy. In FLASH, all-cause mortality at 30 days was 0.8%, [12] which is lower than the historical 30-day mortality rate for intermediate-risk PE patients receiving anticoagulation only (up to 10%) [23]. In the absence of evidence from prospective, randomised, controlled trials assessing cardiovascular outcomes, a retrospective analysis comparing patients with intermediate-high and high-risk PE who received mechanical thrombectomy (n = 28) or routine care (n = 30) suggested that mechanical thrombectomy might indeed improve in-hospital mortality (3.6% vs. 23.3%, p < 0.05) [24].
In contrast to systemic thrombolysis, recommended in high-risk PE but associated with increased bleeding risk, particularly in elderly patients, [4] we observed no major adverse events. There were also no major procedure- or device-related adverse events documented.
This study adds to previous single-arm studies and registries showing that mechanical thrombectomy using large-bore thrombus aspiration is feasible and safe, reduces thrombus burden, and immediately improves hemodynamics in intermediate and high-risk PE [11, 12]. Moreover, this is the first study indicating that the improvement in invasive hemodynamic parameters was maintained at three months of follow-up. Therefore, if mechanical thrombectomy improves cardiovascular outcomes and reduced morbidity and mortality in randomized controlled trials, the procedure offers an alternative approach to systemic thrombolysis for treating acute PE with right heart overload, especially in patients with contraindications for or hemodynamically stable patients who do not benefit from systemic thrombolysis.
Limitations
Several limitations of this analysis need to be acknowledged. Because of the non-randomized study design and the lack of a comparator treatment group, we cannot exclude selection bias and unspecific treatment effects. Therefore, the data should be interpreted with caution and as hypothesis-generating. This feasibility study’s size was small and not based on an a priori power calculation to assess hemodynamic effects. All procedures herein were performed using the FlowTriever System, so the findings cannot be extrapolated to other catheter systems. The procedures were performed by only two experienced operators trained in structural interventions, which may explain the low rate of adverse events observed herein.
Conclusion
Mechanical thrombectomy for acute intermediate and high-risk PE with RV overload was safe and immediately reduced PAP, improved right heart function and RV-arterial coupling. Moreover, the reduction in PAP was maintained for three months. Randomized, controlled trials are required to finally assess the role of mechanical thrombectomy in the management of acute PE.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- dPAP:
-
diastolic pulmonary artery pressure
- ESC:
-
European Society of Cardiology
- Hs:
-
high sensitivity
- ICU:
-
intensive care unit
- LV:
-
left ventricle
- mPAP:
-
mean pulmonary artery pressure
- NT-proBNP:
-
N-terminal B-type natriuretic peptide
- PAP:
-
pulmonary artery pressure
- PE:
-
pulmonary embolism
- RV:
-
right ventricle
- sPAP:
-
systolic pulmonary artery pressure
- TAPSE:
-
tricuspid annular plane systolic excursion
References
Jimenez D, de Miguel-Diez J, Guijarro R, Trujillo-Santos J, Otero R, Barba R, et al. Trends in the management and outcomes of Acute Pulmonary Embolism: analysis from the RIETE Registry. J Am Coll Cardiol. 2016;67(2):162–70.
Jimenez D, Bikdeli B, Barrios D, Quezada A, Del Toro J, Vidal G, et al. Epidemiology, patterns of care and mortality for patients with hemodynamically unstable acute symptomatic pulmonary embolism. Int J Cardiol. 2018;269:327–33.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the european respiratory society (ERS). Eur Heart J. 2020;41(4):543–603.
Marti C, John G, Konstantinides S, Combescure C, Sanchez O, Lankeit M, et al. Systemic thrombolytic therapy for acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J. 2015;36(10):605–14.
Konstantinides SV, Barco S. Systemic thrombolytic therapy for Acute Pulmonary Embolism: who is a candidate? Semin Respir Crit Care Med. 2017;38(1):56–65.
Keller K, Hobohm L, Ebner M, Kresoja KP, Munzel T, Konstantinides SV, et al. Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur Heart J. 2020;41(4):522–9.
Gotzinger F, Lauder L, Sharp ASP, Lang IM, Rosenkranz S, Konstantinides S et al. Interventional therapies for pulmonary embolism. Nat Rev Cardiol. 2023:1–15.
Giri J, Sista AK, Weinberg I, Kearon C, Kumbhani DJ, Desai ND, et al. Interventional therapies for Acute Pulmonary Embolism: current status and principles for the development of Novel evidence: a Scientific Statement from the American Heart Association. Circulation. 2019;140(20):e774–e801.
Stevens SM, Woller SC, Baumann Kreuziger L, Bounameaux H, Doerschug K, Geersing GJ, et al. Executive Summary: antithrombotic therapy for VTE Disease: second update of the CHEST Guideline and Expert Panel Report. Chest. 2021;160(6):2247–59.
Pruszczyk P, Klok FA, Kucher N, Roik M, Meneveau N, Sharp ASP, et al. Percutaneous treatment options for acute pulmonary embolism: a clinical consensus statement by the ESC Working Group on Pulmonary circulation and right ventricular function and the European Association of Percutaneous Cardiovascular Interventions. EuroIntervention. 2022;18(8):e623–e38.
Tu T, Toma C, Tapson VF, Adams C, Jaber WA, Silver M, et al. A prospective, Single-Arm, Multicenter Trial of Catheter-Directed Mechanical Thrombectomy for Intermediate-Risk Acute Pulmonary Embolism: the FLARE Study. JACC Cardiovasc Interv. 2019;12(9):859–69.
Toma C, Jaber WA, Weinberg MD, Bunte MC, Khandhar S, Stegman B et al. Acute outcomes for the full US cohort of the FLASH mechanical thrombectomy registry in pulmonary embolism. EuroIntervention. 2022.
Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005;172(8):1041–6.
Tello K, Wan J, Dalmer A, Vanderpool R, Ghofrani HA, Naeije R, et al. Validation of the tricuspid annular plane systolic Excursion/Systolic pulmonary artery pressure ratio for the Assessment of right ventricular-arterial coupling in severe pulmonary hypertension. Circ Cardiovasc Imaging. 2019;12(9):e009047.
Hareendran A, Leidy NK, Monz BU, Winnette R, Becker K, Mahler DA. Proposing a standardized method for evaluating patient report of the intensity of dyspnea during exercise testing in COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:345–55.
Klok FA, Ageno W, Ay C, Back M, Barco S, Bertoletti L, et al. Optimal follow-up after acute pulmonary embolism: a position paper of the European Society of Cardiology Working Group on Pulmonary circulation and right ventricular function, in collaboration with the European Society of Cardiology Working Group on Atherosclerosis and Vascular Biology, endorsed by the european respiratory society. Eur Heart J. 2022;43(3):183–9.
Cooper R, Ghali J, Simmons BE, Castaner A. Elevated pulmonary artery pressure. An independent predictor of mortality. Chest. 1991;99(1):112–20.
Heresi GA, Minai OA, Tonelli AR, Hammel JP, Farha S, Parambil JG, et al. Clinical characterization and survival of patients with borderline elevation in pulmonary artery pressure. Pulm Circ. 2013;3(4):916–25.
Douschan P, Kovacs G, Avian A, Foris V, Gruber F, Olschewski A, et al. Mild elevation of pulmonary arterial pressure as a predictor of Mortality. Am J Respir Crit Care Med. 2018;197(4):509–16.
Maron BA, Hess E, Maddox TM, Opotowsky AR, Tedford RJ, Lahm T, et al. Association of Borderline Pulmonary Hypertension with Mortality and hospitalization in a large patient cohort: insights from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. Circulation. 2016;133(13):1240–8.
Fauvel C, Raitiere O, Boucly A, De Groote P, Renard S, Bertona J, et al. Interest of TAPSE/sPAP ratio for noninvasive pulmonary arterial hypertension risk assessment. J Heart Lung Transplant. 2022;41(12):1761–72.
Tello K, Axmann J, Ghofrani HA, Naeije R, Narcin N, Rieth A, et al. Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension. Int J Cardiol. 2018;266:229–35.
Ismayl M, Machanahalli Balakrishna A, Aboeata A, Gupta T, Young MN, Altin SE, et al. Meta-analysis comparing Catheter-Directed Thrombolysis Versus systemic anticoagulation alone for Submassive Pulmonary Embolism. Am J Cardiol. 2022;178:154–62.
Buckley JR, Wible BC. In-Hospital mortality and related outcomes for elevated risk Acute Pulmonary Embolism treated with mechanical Thrombectomy Versus Routine Care. J Intensive Care Med. 2022;37(7):877–82.
Acknowledgements
None.
Funding
None.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
LL and FM created the first draft of the manuscript. LL, PPN, FG, HAG, SE, MB, and FM participated in the design of the study. All authors participated in patient data collection LL performed the statistical analyses and prepared the figures. All authors were involved in interpretation of the data. All authors agreed on the content of the manuscript, reviewed drafts, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
LL received speaker honoraria from AstraZeneca, ReCor Medical and Medtronic. FG is supported by the German Foundation of Heart Research and has received speaker honoraria from Astra-Zeneca. SE received speaker honoraria and/or travel support from Akcea Therapeutics, AstraZeneca, Bayer, Berlin Chemie, Bristol-Myers Squibb, Pfizer, Böhringer Ingelheim, Daiichi Sankyo, Edwards Lifesciences, Inari medical, Kaneka Pharma, Medtronic, Novartis and Recor. MB is supported by the Deutsche Forschungsgemeinschaft (German Research Foundation; TTR 219, project number 322900939) and reports personal fees from Abbott, Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, Cytokinetics, Edwards, Medtronic, Novartis, Recor, Servier and Vifor during the conduct of the study. FM is supported by Deutsche Gesellschaft für Kardiologie (DGK), Deutsche Forschungsgemeinschaft (SFB TRR219), and Deutsche Herzstiftung. He has received scientific support from Ablative Solutions, Medtronic and ReCor Medical and speaker honoraria/consulting fees from Ablative Solutions, Amgen, Astra-Zeneca, Bayer, Boehringer Ingelheim, Inari, Medtronic, Merck, ReCor Medical, Servier, and Terumo. PPN, HAG, BH, PL, SK, AL, and BS report no conflict of interest related to this study.
Ethics approval
The trial was approved by the local ethics committee (ethic committee of the Ärztekammer des Saarlandes) and complied with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lauder, L., Pérez Navarro, P., Götzinger, F. et al. Mechanical thrombectomy in intermediate- and high-risk acute pulmonary embolism: hemodynamic outcomes at three months. Respir Res 24, 257 (2023). https://doi.org/10.1186/s12931-023-02552-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-023-02552-w