Abstract
Purpose
To investigate the prognostic value of quantitative analysis of CT among patients with idiopathic pulmonary fibrosis (IPF) by quantifying the fibrosis extent and to attempt to provide precise medium-long term prognostic predictions for individual patients.
Methods
This was a retrospective cohort study that included 95 IPF patients in Zhongshan Hospital, Fudan University. 64 patients firstly diagnosed with IPF from 2009 to 2015 was included as the derivation cohort. Information regarding sex, age, the Gender-Age-Physiology (GAP) index, high-resolution computed tomography (HRCT) images, survival status, and pulmonary function parameters including forced vital capacity (FVC), FVC percent predicted (FVC%pred), diffusing capacity of carbon monoxide (DLCO), DLCO percent predicted (DLCO%pred), carbon monoxide transfer coefficient (KCO), KCO percent predicted (KCO%pred) were collected. 31 patients were included in the validation cohort. The Synapse 3D software was used to quantify the fibrotic lung volume (FLV) and total lung volume (TLV). The ratio of FLV to TLV was calculated and labeled CTFLV/TLV%, reflecting the extent of fibrosis. All the physiological variants and CTFLV/TLV% were analyzed for the dimension of survival through both univariate analysis and multivariate analysis. Formulas for predicting the probability of death based on the baseline CTFLV/TLV% were calculated by logistic regression, and validated by the validation cohort.
Results
The univariate analysis indicated that CTFLV/TLV% along with DLCO%pred, KCO%pred and GAP index were significantly correlated with survival. However, only CTFLV/TLV% was meaningful in the multivariate analysis for prognostic prediction (HR 1.114, 95% CI 1.047–1.184, P = 0.0006), and the best cutoff was 11%, based on receiver operating characteristic (ROC) curve analysis. The survival times for the CTFLV/TLV% ≤ 11% and CTFLV/TLV% > 11% groups were significantly different. Given the CTFLV/TLV% data, the death probability of a patient at 1 year, 3 years and 5 years could be calculated by using a particular formula. The formulas were tested by the validation cohort, showed high sensitivity (88.2%), specificity (92.8%) and accuracy (90.3%).
Conclusion
Quantitative volume analysis of CT might be useful for evaluating the extent of fibrosis in the lung. The CTFLV/TLV% could be a valuable biomarker for precisely predicting the medium-long term prognosis of individual patients with IPF.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Idiopathic pulmonary fibrosis (IPF) is the most common type of idiopathic interstitial pneumonia and is defined as a spontaneously occurring (idiopathic) specific form of chronic fibrosing interstitial pneumonia limited to the lung according to an American Thoracic Society/European Respiratory Society (ATS/ERS) consensus statement [1]. IPF has a usual interstitial pneumonia (UIP) pattern on high-resolution computed tomography (HRCT) images or surgical lung biopsy. IPF is a deadly disease with poor prognosis. The median survival of IPF has been reported to range from 2 to 5 years [2, 3]. However, the prognosis varies among individual patients with IPF. The risk of death in individual IPF patients at the time of diagnosis ranges from < 1 year to > 10 years [2]. Accurate prediction of survival is critical for guiding clinical care.
The known predictors of reduced survival include older age, male sex, lower forced vital capacity (FVC) percent predicted (FVC%pred), lower diffusing capacity of carbon monoxide (DLCO) percent predicted (DLCO%pred), need for supplemental oxygen, greater severity of dyspnea, lower distance walked on the six-minute walk test (6MWT), more respiratory hospitalization and greater extent of fibrosis on HRCT images [3,4,5]. Several index models, including the Gender-Age-Physiology (GAP) index [3], the composite physiologic index (CPI) [6] and a risk stratification score (ROSE) [5], have been proposed. All these models include variables of FVC and DLCO. However, achieving consistent DLCO results between and within laboratories remains a difficult problem; even when tested in the same laboratory a few days apart, DLCO results from healthy subjects may vary as much as 8 mL/min per mmHg [7]. Furthermore, qualified pulmonary function tests (PFTs) are sometimes unavailable for elderly patients or those who cannot cooperate. HRCT is much easier to perform for these patients and more accurate. In previous studies, it was confirmed that the CT fibrosis score by visual assessment or computer-based algorithms could replace standard clinical and physiological variables [8,9,10,11,12,13,14]. Quantifying the severity of fibrosis with HRCT is a promising approach for predicting the prognosis of patients with IPF, especially the computer-based assessment, with more efficiency and accuracy as compared with artificial visual assessment.
In our study, we focused on the value of quantitative volume analysis of CT in the quantification of fibrosis, calculated the fibrotic lung volume (FLV), total lung volume (TLV) and FLV/TLV ratio (CTFLV/TLV%), and then used the CTFLV/TLV% to predict the precise death probability within 5 years for individual patients with IPF.
Methods
Study population
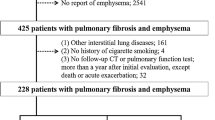
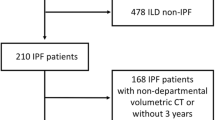
This was a retrospective cohort study of patients diagnosed with stable IPF at Zhongshan Hospital, Fudan University. Two cohorts were collected, including a derivation cohort firstly diagnosed as IPF between 1 January 2009 and 31 December 2015, as well as a validation cohort firstly diagnosed as IPF between 1 January 2009 and 31 December 2020. According to the diagnosis criteria from ATS/ERS/JRS/ALAT 2011, the inclusion criteria of the study included (1) definite features of UIP on HRCT images or (2) surgical lung biopsy results correlated with the HRCT findings. The exclusion criteria were as follows: (1) interstitial lung diseases of known cause, e.g., drug-induced, environmental, occupational or connective tissue diseases; (2) IPF combined with pulmonary infections and needed for anti-infective therapy; (3) other severe systemic diseases or organ dysfunction; or (4) malignant tumors.
The study was approved by the institutional ethics committees of Zhongshan Hospital, Fudan University (ethical number: ZS2013-31). The requirement for informed consent from the patients included in this study was waived due to the retrospective nature of the study, and any personal information from the data was removed beforehand.
Data collection
General information for the enrolled patients, including sex, age, date of diagnosis, symptoms and complications, as well as lung HRCT images and PFT were collected. PFT parameters included FVC, FVC%pred, DLCO, DLCO%pred, carbon monoxide transfer coefficient (KCO), KCO percent predicted (KCO%pred). The GAP index [3] was calculated based on the sex, age and PFT data.
The patients in the derivation cohort were followed up every 6 months or 1 year either face-to-face or by telephone. Patient enrollment started on 1 January 2009 and ended on 31 December 2015. The whole cohort was followed up until 31 January 2021. The longest observation time was 145 months (12 years and 1 month). This process ensured that the last participant’s observation time was greater than 5 years. For each individual, the observation was ended if the patient died; otherwise, the patient was observed until the end of the study. In the validation cohort, patients firstly diagnosed as IPF between 1 January 2009 and 31 December 2020 were searched from the Hospital Information System. The patients who had already been included in the derivation cohort were excluded from the validation cohort. The survival status was collected by telephone interview between 1 September 2022 to 31 October 2022. If a patient in the validation cohort is diagnosed with IPF for less than 5 years and survives, the patient will be excluded. This ensured that patients who survived were observed for more than 5 years.
HRCT and quantitative analysis of fibrotic lung volume
HRCT imaging was performed using a 64-detector row spiral CT machine (Lightspeed VCT, Ge Healthcare, Hamilton, USA) in the supine position at full inspiration breath hold. The diagnostic settings were as follows: tube voltage, 120 ~ 140 kV; tube current, 140 mAs; collimation, 64 × 0.625 mm; pitch, 0.9875; and reconstruction slice thickness, 1.25 mm. The original images in DICOM format were loaded into image analysis software (Synapse 3D, V4.4, Fuji Film, Japan). Total lung tissue and fibrotic lung tissue were manually delineated layer by layer. Fibrotic lung tissue was defined as honeycombing or reticular opacities on CT and was judged jointly by a respiratory physician (with no less than 10 years of professional experience in respiratory medicine) and a radiologist (with no less than 7 years of professional experience in chest radiology) who did not know any of the patients’ clinical information. If the raters disagreed, a third senior radiologist joined the discussion. The software automatically calculated the total lung tissue area and the fibrotic lung tissue area of each CT layer. According to the approximate cylindrical volume calculation formula, the volume of each lesion and total CT lung volume were computed automatically by the computer-aided diagnosis (CADx) system (Fig. 1). The FLV and TLV were expressed as absolute values, and the FLV/TLV ratio refers to the percentage of FLV relative to TLV (CTFLV/TLV%).
Evaluation of the CTFLV/TLV% by Synapse 3D software. A and D Two adjacent HRCT images of a transverse axial scan of one IPF patient. B and E The total lung area and the total area of fibrosis were automatically captured and drawn by the Synapse 3D software. C and F Green shows the area of fibrosis after drawing by the Synapse 3D software. G The FLV and TLV were approximately calculated by the Cylinder volume formula
Statistical analysis
Baseline characteristics of the patient cohort were summarized according to survival status. All data are presented as the mean ± SD for continuous variables and as absolute numbers and percentages for categorical data. The differences between two groups were assessed by Student’s t-test or the Mann–Whitney U test for continuous data and the chi-square or Fisher’s exact test for categorical variables.
The correlation between the clinical parameters and survival time was analyzed by linear correlation analysis and was expressed by the Pearson correlation coefficient. The closer the area under the curve (AUC) value is to one, the better the discrimination capacity of the model. Youden's index was used to identify the optimal cutoff value for the CTFLV/TLV%, which was 11%. Kaplan–Meier survival curves were calculated in strata defined by the CTFLV/TLV% categories (CTFLV/TLV% ≤ 11%, > 11%). Two-sided log-rank tests defined significance.
To explore risk factors that could be associated with all-cause mortality, a univariate Cox proportional hazards model was initially applied using demographics, clinical variables, physiological indices and CT indices. Then, a multivariate binary logistic regression was performed by introducing the variables selected in the univariate regression model, and the statistically significant variables were eventually identified. Based on the results of the multivariate analysis, mortality predictive formulas were further constructed, and were validated in the validation cohort. The sensitivity, specificity and accuracy of the formulas were calculated.
All tests of hypotheses were two-tailed and conducted at a significance level of 0.05. Statistical analyses were conducted using SAS version 9.3.
Results
Patient characteristics
Eighty-one patients with IPF were included in the derivation cohort. Among them, 6 were excluded for malignant tumors (1 with nasopharyngeal cancer and 5 with lung cancer), 2 were excluded for connective tissue disease, and 9 were lost to follow-up. Therefore, 64 patients were included in the analyses of derivation cohort. The number of survivors or deaths was recorded at the timepoint of at least 5 years of observation since enrollment as well as at the end of the study. Forty-five patients completed the baseline PFT, while 19 failed (10 patients lost their initial PFT reports, 9 patients could not complete the PFT process). Among the 45 patients, 37 finished the diffusion function test, and 8 could not cooperate. All 64 patients completed baseline HRCT scans, and 21 patients were followed up with HRCT after 1 and 3 years.
Fifty-six patients were included in the validation cohort. Among them, 1 was excluded for liver cancer, 9 survivors were excluded because the time to first diagnosis of IPF was less than 5 years, and 15 were excluded since loss of communication by telephone. Therefore, 31 patients were finally included in the analyses of validation cohort. Baseline HRCT images were available in all patients, but the PFT reports were available in only 16 patients.
Correlation of patient characteristics and survival time
The patients in both derivation and validation cohorts were divided into two groups according to their 5-year survival. Table 1 shows the patient characteristics of the cohorts. In the derivation cohort, among 64 patients, 31 (48.4%) died, and 33 (51.6%) survived after 5 years of observation since enrollment. DLCO%pred (39.3 ± 14.4% vs. 57.6 ± 22.4%, P = 0.0033) and KCO%pred (57.6 ± 22.4% vs. 75 ± 21.9%, P = 0.0067) were significantly decreased in the death group compared with the survival group. The mean GAP index was higher in the death group (4.9 ± 1.5 vs. 3.8 ± 2, P = 0.0420). The baseline CTFLV/TLV% showed a significant difference between the two groups: 29.6% ± 11.6% in the death group and 10.7% ± 7.1% in the survival group (P < 0.0001). There were no significant differences between the two groups with regard to sex, age, FVC (absolute value), FVC%pred, DLCO (absolute value) or KCO (absolute value). In the validation cohort, only CTFLV/TLV% showed a significant difference between 5-year survival and death groups (P < 0.0001).
In the derivation cohort, the patients were then divided into three groups according to their survival time (< 2 years, 2–5 years and ≥ 5 years), and the patient characteristics, including sex, age, baseline FVC%pred, DLCO%pred, KCO%pred, GAP index and baseline CTFLV/TLV%, were compared among the groups (Table 2). A higher baseline DLCO%pred (P = 0.0048) and KCO%pred (P = 0.0224), a lower GAP index (P = 0.0066), and a lower baseline CTFLV/TLV% (P < 0.0001) were protective factors for patients with IPF when considering the survival time.
The linear correlation analysis of survival time and patient characteristics showed similar results (Fig. 2). DLCO%pred (r2 = 0.1207, P = 0.0260) and KCO%pred (r2 = 0.1247, P = 0.0321) were positively correlated with survival time, while the GAP index had a negative correlation (r2 = 0.1092, P = 0.0267). The baseline CTFLV/TLV% had a strong negative correlation with the survival time (r2 = 0.5916, P < 0.0001). Age and FVC%pred showed no significant correlation with the survival time.
Correlation between the survival time and patient characteristics. Graphs show that age (A) and FVC%pred (B) do not correlate with the survival time. DLCO%pred (r2 = 0.1207, P = 0.0260) (C) and KCO%pred (r2 = 0.1247, P = 0.0321) (D) positively correlated with survival. The GAP index (E) negatively correlated with survival (r2 = 0.1092, P = 0.0267). The baseline CTFLV/TLV% (F) showed a strongly negative correlation with survival (r2 = 0.5916, P = < 0.0001)
Therefore, we suggest that the baseline DLCO%pred, KCO%pred, and GAP index, and especially the baseline CTFLV/TLV%, are predictors of the survival time for patients with IPF.
Prediction of mortality probability by CTFLV /TLV%
A univariate Cox proportional hazards model was applied in the derivation cohort to explore the risk factors associated with 5-year all-cause mortality. The variants included the baseline age, FVC, FVC%pred, DLCO, DLCO%pred, KCO, KCO%pred, GAP index, and baseline CTFLV/TLV%. Among these variants, the DLCO%pred, KCO%pred and CTFLV/TLV% were considered significant variants. Multivariate Cox analysis was further performed, covariates included sex, age, FVC%pred, DLCO%pred, KCO%pred, GAP index, and baseline CTFLV/TLV%, and only baseline CTFLV/TLV% was a significant predictor of 5-year mortality (HR 1.114, 95% CI 1.047–1.184, P = 0.0006). The Kaplan–Meier survival curve demonstrated a significant difference in mortality at 5 years, which was defined by a cutoff point of 11% for CTFLV/TLV% (Fig. 3A and B).
Kaplan–Meier analysis of the survival of patients. A The Kaplan–Meier curve of 64 patients in the derivation cohort. B The 64 patients in the derivation cohort were separated into two groups according to the baseline CTFLV/TLV%, with a cutoff of 11%. The two curves separate obviously at the beginning of the follow-up and become farther with the increase in follow-up months. C The Kaplan–Meier curve of 31patients in the validation cohort. D Patients in the validation cohort were divided into two groups by the cutoff point of 11% for baseline CTFLV/TLV%. The two survival curves separated apart significantly even at the beginning of the observation. No patient of the CT FLV/TLV% < 11% group died in the first 5 years. The graph only shows the survival in the first 5 years from the date of enrollment of every individual patient in our study
In the validation cohort, patients were divided into two groups by the cutoff point of 11% for baseline CTFLV/TLV%. The Kaplan–Meier survival curve also showed significant difference between groups (Fig. 3C and D).
Based on the survival data of the derivation cohort, a logistic model was applied to create a predictive formula of the probability of death. Figure 4 shows the logistic regression curve for the prediction of the 5-year death probability. The logistic equation was as follows:
where \(\hat{P}\) is the 5-year death probability. It is clear from the equation that the risk of death increased directly with the increase in the baseline CTFLV/TLV%.
For instance, the baseline CTFLV/TLV% of a patient with IPF was 19.99%, and that patient’s 5-year death probability \(\left( {\hat{P}} \right)\) was as follows:
Furthermore, we calculated the prediction formula for the 1-year and 3-year death probabilities based on the cohort data for the CTFLV/TLV%, 1-year death and 3-year death by logistic regression.
The prediction of the 1-year death probability was as follows:
The prediction of the 3-year death probability was as follows:
For clinical application, the formulas could be made into a mobile phone or computer applet. By inputting the baseline CTFLV/TLV%, the prediction of the 1-year, 3-year and 5-year death probability of the patient would be obtained immediately.
These formulas were validated in the validation cohort with high accuracy. As shown in the Table 3, 15 of the 16 patients with 5-year death probability > 50% was actually died, and 13 of the 15 patients with 5-year death probability ≤ 50% was actually alive. The sensitivity, specificity and accuracy were 88.2%, 92.8% and 90.3%. Similar results were observed for 1-year death probability and 3-year death probability.
Correlation of dynamic changes in the CT FLV/TLV% and survival
In the derivation cohort, dynamic CT FLV/TLV% data were available for 21 patients. At the end of the follow-up, 9 survived, and 12 died. The CTFLV/TLV% at baseline and at 1 year and 3 years after diagnosis between the two groups (survival and death) were compared (Table 4 and Fig. 5). The CTFLV/TLV% increased with time in both groups (P = 0.0005), and the value of the CTFLV/TLV% was higher in the death group (P = 0.0531), indicating that the baseline CTFLV/TLV% correlated with survival. Although only a small number of patients had dynamic HRCT images, the slopes of the two lines were almost parallel (P = 0.1641), which indicates that fibrotic lesions of the lung develop, regardless of the patients’ group. The results are consistent with the theory that once IPF is diagnosed, the progression of the disease is irreversible.
Dynamic CTFLV/TLV% within 3 years. The CTFLV/TLV% of individual patients as well as the mean CTFLV/TLV% at baseline and 1 year and 3 years after enrollment are shown in the graph. The patients were divided into two groups according to their 5-year survival status at the end of the follow-up. The two lines are far apart from each other, indicating that the baseline CTFLV/TLV% correlated with survival (P = 0.0531). The CTFLV/TLV% increases with time (P = 0.0005). The two lines are nearly parallel, and there is no interaction for the CTFLV/TLV% within 3 years (P = 0.1641)
Discussion
The general prognosis of IPF is poor but varies widely among individuals. Accurate and precise prognosis prediction of IPF will guide the clinical strategy, such as the best time to start drug therapy, lung transplantation, or palliative care.
Physiological variants of the PFT, especially the FVC%pred and DLCO%pred, have been reported as predictors for the prognosis of IPF in past studies [1, 15,16,17,18,19]. Therefore, we identified the FVC%pred and DLCO%pred as candidate variants in our study to validate their prediction value in IPF prognosis. In our cohort, the baseline DLCO%pred was correlated with survival according to the univariate analysis, which was consistent with the results of past studies. However, the predictive value of the baseline FVC%pred failed to be validated. Although many studies have considered the FVC%pred as a predictor for prognosis [15,16,17], few studies have reported that the baseline FVC%pred has no dependent correlation with survival [18, 20]. Instead, the decline rate of FVC is a commonly validated predictor [17, 21, 22]. A decline in the FVC ≥ 10% is associated with an increased risk of death [17]. DLCO changes over time are also valuable in prognosis prediction and have been shown to be a better predictor of mortality than FVC changes [23]. In our study, the baseline FVC%pred showed no significant difference between the survival and death groups, but the decline rate of FVC between the groups might be different, which would influence the prognosis. However, limited by the retrospective nature of the study, we did not obtain follow-up PFT reports from the patients. Another possible reason might be the bias due to incomplete PFT data since 10 patients lost their initial PFT reports and 9 patients could not complete the PFT process. KCO, which is often written as DLCO/alveolar volume (VA), is an index of the efficiency of alveolar transfer of carbon monoxide. DLCO is often decreased in interstitial lung diseases because of diffuse alveolar capillary damage. VA is decreased due to loss of aerated alveoli. Therefore, the extent of KCO reduction is often less than that of DLCO [24]. Few studies have identified KCO as a prognostic predictor. Corte et al. reported that a decline in KCO in six months predicted early mortality in patients with idiopathic interstitial pneumonia [25]. In our study, we found that the baseline KCO%pred along with the DLCO%pred were correlated with survival. However, we did not further compare the prediction value of the two variants.
The GAP model is the most widely validated clinical prediction model for IPF. It incorporates age, sex, FVC, and DLCO into a simple point-score index and staging system, predicting 1-, 2-, and 3-year mortality [3]. The correlation between the baseline GAP and survival was confirmed in our study.
Compared with the PFT, CT is a promising examination for prognosis prediction for IPF, with the advantages of convenience and objectivity. Lynch et al. confirmed the correlation between DLCO and HRCT findings and suggested that the extent of reticulation and honeycombing on HRCT images is an important independent predictor of mortality in patients with IPF [10]. Ley et al. used the CT fibrosis score to replace DLCO and constructed a modified GAP model [8]. Salisbury et al. reported that postbaseline changes in ground glass-reticular densities correlated with changes in the FVC [9]. These findings support CT as an alternative when the PFT is unavailable or unreliable.
Although the CT images were objective, the repeatability and homogeneity of the visual assessment of CT were limited by the experience of the radiologists, and it was difficult to quantify the lesion volume precisely by artificial assessment [8, 12, 26]. Jacob et al. [13] reported that computer-derived CT variants are superior predictors of mortality than any visually scored CT parameter in patients with IPF. Therefore, computer-assisted CT evaluation is a future assessment direction, which could provide more precise and comprehensive evaluation.
Several studies have reported computer-assisted segmentation, quantification, and characterization of pulmonary fibrosis. Maldonado et al. [11] explored the application of the computer-aided lung informatics for pathology evaluation and rating (CALIPER) software to quantify parenchymal lung abnormalities on HRCT images and found that short-term volumetric longitudinal changes in serial HRCT images correlated with IPF mortality in a retrospective cohort of patients with IPF. Salisbury et al. [9] used adaptive multiple features method (AMFM) lung texture analysis software to recognize and quantify the volume of lung occupied by ground glass, ground glass-reticular, honeycombing, emphysema, and normal lung in HRCT images of patients with IPF and found that a greater volume occupied by AMFM-measured fibrosis was independently associated with an increased hazard of disease progression. A recent study compared different software programs [27] and found that the shape model-based segmentation software tool was superior to the threshold-based tool since the density of (severe) fibrosis was similar to that of the surrounding soft tissues. These studies have proven the value of computer software in quantitative analysis of CT in IPF and have revealed the close correlation of quantified severity in CT with disease severity, progression and prognosis of IPF, showed advantage of volumetric analysis of total lung as compared with visual scoring based on a few CT images. But these studies had not provided detailed prognosis prediction for an individual patient.
We used Synapse 3D, a software to quantify the volume of fibrotic lung and total lung and obtain the ratio of FLV/TLV, defined as the CTFLV/TLV%. We aimed to verify the correlation between the CTFLV/TLV% and physiological variants and the prognosis of IPF in a retrospective cohort from our hospital and tried to provide a precise and detailed formula for the prediction of prognosis for a certain patient. The univariate Cox proportional hazards model analysis showed that the baseline CTFLV/TLV% as well as physiological variants, including DLCO%pred, KCO%pred and GAP index, correlated with the survival time, but the multivariate analysis showed that the CTFLV/TLV% was the only factor correlated with survival. The cutoff point at 11% CTFLV/TLV% was chosen from the ROC curve, and there was a significant difference in the survival time between the CTFLV/TLV% ≤ 11% and > 11% groups. Formulas to predict the probability of death at 1 year, 3 years and 5 years since the diagnosis of IPF were calculated through logistic regression based on the baseline CTFLV/TLV%. These formulas were validated as with high sensitivity and specificity by a validation cohort, and might provide precise predictions of prognosis for individual patients and provide a reference for clinical strategies. Patients firstly diagnosed as IPF would be evaluated by their baseline HRCT. We could get the baseline CTFLV/TLV% by using the computer software, then calculate the 1-year, 3-year and 5-year death probability by using the formulas. For those patients with high risk of death, we could give them more active interventions, starting anti-fibrotic drugs as early as possible, and applying for lung transplantation.
There are still some limitations to our study. Firstly, this study was retrospective, which may have limited the sample number and data quality. The treatments given to the patients were not identical, which may also influence the assessments of prognosis. Secondly, although the formulas were confirmed to be with high sensitivity and specificity in the validation cohort from our hospital, a larger external validation cohort from multiple centers to validate the suitability of the formulas would be look forward. Thirdly, the assistance of experienced radiologists and respiratory physicians in the quantification of fibrosis or total lung volume from CT images was still required because of the lack of fully automated artificial intelligence computer software for the analysis. With the development of machine learning and artificial intelligence [28, 29], these problems might be resolved in the near future. Fourthly, since dynamic CT FLV/TLV% data were available in only 32.8% (n = 21) of the total cohort (n = 64), the analysis of the correlation of the CTFLV/TLV% changes with disease progression and prognosis failed to obtain a certain result. A larger sample number is needed for future research.
In conclusion, we quantified the volume of fibrotic lungs and total lungs through Synapse 3D and obtained the CTFLV/TLV%, analyzed factors that might influence the prognosis of patients with IPF in a retrospective cohort, and confirmed that the baseline CT FLV/TLV% was significantly correlated with the survival time. Formulas to predict the probability of one to five years death of IPF patients were calculated and might serve as a reference in clinical decision-making for individual patients.
Availability of data and materials
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Abbreviations
- IPF:
-
Idiopathic pulmonary fibrosis
- GAP:
-
Gender-age-physiology
- HRCT:
-
High-resolution computed tomography
- FVC:
-
Forced vital capacity
- FVC%pred:
-
FVC percent predicted
- DLCO:
-
Diffusing capacity of carbon monoxide
- DLCO%pred:
-
DLCO percent predicted
- KCO:
-
Carbon monoxide transfer coefficient
- KCO%pred:
-
KCO percent predicted
- FLV:
-
Fibrotic lung volume
- TLV:
-
Total lung volume
- ROC:
-
Receiver operating characteristic
- CTFLV/TLV% :
-
FLV/TLV ratio
- ATS:
-
American Thoracic Society
- ERS:
-
European Respiratory Society
- UIP:
-
Usual interstitial pneumonia
- 6MWT:
-
Six-minute walk test
- CPI:
-
Composite Physiologic Index
- ROSE:
-
Risk Stratification Score
- PFT:
-
Pulmonary Function Test
- CADx:
-
Computer-aided diagnosis
- AUC:
-
Area under the curve
- CALIPER:
-
Computer-aided lung informatics for pathology evaluation and rating
- AMFM:
-
Adaptive multiple features method
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824.
Nathan SD, Shlobin OA, Weir N, Ahmad S, Kaldjob JM, Battle E, et al. Long-term course and prognosis of idiopathic pulmonary fibrosis in the new millennium. Chest. 2011;140(1):221–9.
Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156(10):684–91.
Ley B, Bradford WZ, Weycker D, Vittinghoff E, du Bois RM, Collard HR. Unified baseline and longitudinal mortality prediction in idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1374–81.
du Bois RM, Weycker D, Albera C, Bradford WZ, Costabel U, Kartashov A, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(4):459–66.
Wells AU, Desai SR, Rubens MB, Goh NS, Cramer D, Nicholson AG, et al. Idiopathic pulmonary fibrosis: a composite physiologic index derived from disease extent observed by computed tomography. Am J Respir Crit Care Med. 2003;167(7):962–9.
Hathaway EH, Tashkin DP, Simmons MS. Intraindividual variability in serial measurements of DLCO and alveolar volume over one year in eight healthy subjects using three independent measuring systems. Am Rev Respir Dis. 1989;140(6):1818–22.
Ley B, Elicker BM, Hartman TE, Ryerson CJ, Vittinghoff E, Ryu JH, et al. Idiopathic pulmonary fibrosis: CT and risk of death. Radiology. 2014;273(2):570–9.
Salisbury ML, Lynch DA, van Beek EJ, Kazerooni EA, Guo J, Xia M, et al. Idiopathic pulmonary fibrosis: the association between the adaptive multiple features method and fibrosis outcomes. Am J Respir Crit Care Med. 2017;195(7):921–9.
Lynch DA, Godwin JD, Safrin S, Starko KM, Hormel P, Brown KK, et al. High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med. 2005;172(4):488–93.
Maldonado F, Moua T, Rajagopalan S, Karwoski RA, Raghunath S, Decker PA, et al. Automated quantification of radiological patterns predicts survival in idiopathic pulmonary fibrosis. Eur Respir J. 2014;43(1):204–12.
Oda K, Ishimoto H, Yatera K, Naito K, Ogoshi T, Yamasaki K, et al. High-resolution CT scoring system-based grading scale predicts the clinical outcomes in patients with idiopathic pulmonary fibrosis. Respir Res. 2014;15(1):10.
Jacob J, Bartholmai BJ, Rajagopalan S, Kokosi M, Nair A, Karwoski R, et al. Mortality prediction in idiopathic pulmonary fibrosis: evaluation of computer-based CT analysis with conventional severity measures. Eur Respir J. 2017. https://doi.org/10.1183/13993003.01011-2016.
Best AC, Meng J, Lynch AM, Bozic CM, Miller D, Grunwald GK, et al. Idiopathic pulmonary fibrosis: physiologic tests, quantitative CT indexes, and CT visual scores as predictors of mortality. Radiology. 2008;246(3):935–40.
Schwartz DA, Helmers RA, Galvin JR, Van Fossen DS, Frees KL, Dayton CS, et al. Determinants of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1994;149(2 Pt 1):450–4.
King TE Jr, Safrin S, Starko KM, Brown KK, Noble PW, Raghu G, et al. Analyses of efficacy end points in a controlled trial of interferon-gamma1b for idiopathic pulmonary fibrosis. Chest. 2005;127(1):171–7.
Paterniti MO, Bi Y, Rekić D, Wang Y, Karimi-Shah BA, Chowdhury BA. Acute exacerbation and decline in forced vital capacity are associated with increased mortality in idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2017;14(9):1395–402.
Hallstrand TS, Boitano LJ, Johnson WC, Spada CA, Hayes JG, Raghu G. The timed walk test as a measure of severity and survival in idiopathic pulmonary fibrosis. Eur Respir J. 2005;25(1):96–103.
Hamada K, Nagai S, Tanaka S, Handa T, Shigematsu M, Nagao T, et al. Significance of pulmonary arterial pressure and diffusion capacity of the lung as prognosticator in patients with idiopathic pulmonary fibrosis. Chest. 2007;131(3):650–6.
King TE Jr, Tooze JA, Schwarz MI, Brown KR, Cherniack RM. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 2001;164(7):1171–81.
Jegal Y, Kim DS, Shim TS, Lim CM, Do Lee S, Koh Y, et al. Physiology is a stronger predictor of survival than pathology in fibrotic interstitial pneumonia. Am J Respir Crit Care Med. 2005;171(6):639–44.
Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168(5):538–42.
EMPIRE Registry, Czech Part: Impact of demographics, pulmonary function and HRCT on survival and clinical course in idiopathic pulmonary fibrosis. Clinical Respiratory Journal. 2018.
Kanengiser LC, Rapoport DM, Epstein H, Goldring RM. Volume adjustment of mechanics and diffusion in interstitial lung disease. Lack of clinical relevance. Chest. 1989;96(5):1036–42.
Corte TJ, Wort SJ, Wells AU. Decline in KCO at six months predicts early mortality and pulmonary hypertension in patients with idiopathic interstitial pneumonia.
Fraser E, St Noble V, Hoyles RK, Benamore R, Ho LP. Readily accessible CT scoring method to quantify fibrosis in IPF. BMJ Open Respir Res. 2020;7(1):e000584.
Ley-Zaporozhan J, Giannakis A, Norajitra T, Weinheimer O, Kehler L, Dinkel J, et al. Fully automated segmentation of pulmonary fibrosis using different software tools. Respiration. 2021;100(7):580–7.
Walsh SLF, Humphries SM, Wells AU, Brown KK. Imaging research in fibrotic lung disease; applying deep learning to unsolved problems. Lancet Respir Med. 2020;8(11):1144–53.
Handa T, Tanizawa K, Oguma T, Uozumi R, Watanabe K, Tanabe N, et al. Novel artificial intelligence-based technology for chest computed tomography analysis of idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2022;19(3):399–406.
Acknowledgements
We appreciate the instruction work on data analysis by Xuejuan Jin from Evidence Based Medicine Center of Fudan University.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81970023 by ZHC), the Shanghai Health Committee (Grant No. 201840288), the Shanghai Top-Priority Clinical Key Disciplines Construction Project (Grant No. 2017ZZ02013), and the Shanghai Municipal Key Clinical Specialty (Grant No. shslczdzk02201).
Author information
Authors and Affiliations
Contributions
ZC, XZ conceived and designed the study; KD, RM enrolled the patients and collected the raw data. KD and YZ analyzed the data statistically. YQ, BC and YM searched the references. YZ, KD and ZC wrote and modified the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional ethics committees of Zhongshan Hospital, Fudan University (ethical number: ZS2013-31). The requirement for informed consent from the patients included in this study was waived due to the retrospective nature of the study, and any personal information from the data was removed beforehand.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Du, K., Zhu, Y., Mao, R. et al. Medium-long term prognosis prediction for idiopathic pulmonary fibrosis patients based on quantitative analysis of fibrotic lung volume. Respir Res 23, 372 (2022). https://doi.org/10.1186/s12931-022-02276-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02276-3