Abstract
Background
COVID-19 related acute respiratory distress syndrome (ARDS) has specific characteristics compared to ARDS in other populations. Proning is recommended by analogy with other forms of ARDS, but few data are available regarding its physiological effects in this population. This study aimed to assess the effects of proning on oxygenation parameters (PaO2/FiO2 and alveolo-arterial gradient (Aa-gradient)), blood gas analysis, ventilatory ratio (VR), respiratory system compliance (CRS) and estimated dead space fraction (VD/VT HB). We also looked for variables associated with treatment failure.
Methods
Retrospective monocentric study of intubated COVID-19 ARDS patients managed with an early intubation, low to moderate positive end-expiratory pressure and early proning strategy hospitalized from March 6 to April 30 2020. Blood gas analysis, PaO2/FiO2, Aa-gradient, VR, CRS and VD/VT HB were compared before and at the end of each proning session with paired t-tests or Wilcoxon tests (p < 0.05 considered as significant). Proportions were assessed using Fischer exact test or Chi square test.
Results
Forty-two patients were included for a total of 191 proning sessions, median duration of 16 (5–36) hours. Considering all sessions, PaO2/FiO2 increased (180 [148–210] vs 107 [90–129] mmHg, p < 0.001) and Aa-gradient decreased (127 [92–176] vs 275 [211–334] mmHg, p < 0.001) with proning. CRS (36.2 [30.0–41.8] vs 32.2 [27.5–40.9] ml/cmH2O, p = 0.003), VR (2.4 [2.0–2.9] vs 2.3 [1.9–2.8], p = 0.028) and VD/VT HB (0.72 [0.67–0.76] vs 0.71 [0.65–0.76], p = 0.022) slightly increased. Considering the first proning session, PaO2/FiO2 increased (186 [165–215] vs 104 [94–126] mmHg, p < 0.001) and Aa-gradient decreased (121 [89–160] vs 276 [238–321] mmHg, p < 0.001), while CRS, VR and VD/VT HB were unchanged. Similar variations were observed during the subsequent proning sessions. Among the patients who experienced treatment failure (defined as ICU death or need for extracorporeal membrane oxygenation), fewer expressed a positive response in terms of oxygenation (defined as increase of more than 20% in PaO2/FiO2) to the first proning (67 vs 97%, p = 0.020).
Conclusion
Proning in COVID-19 ARDS intubated patients led to an increase in PaO2/FiO2 and a decrease in Aa-gradient if we consider all the sessions together, the first one or the 4 subsequent sessions independently. When considering all sessions, CRS increased and VR and VD/VT HB only slightly increased.
Similar content being viewed by others
Background
Coronavirus Disease 19 (COVID-19) pandemic is still causing thousands of deaths worldwide [1]. Between 5 and 34% of hospitalized patients develop severe disease and are admitted in the intensive care unit (ICU). Most of these patients fulfill the criteria for acute respiratory distress syndrome (ARDS), with a high mortality rate [2,3,4,5,6,7,8]. Prone positioning demonstrated physiological and survival benefits in moderate to severe ARDS non related to COVID-19 and is recommended by the current international guidelines as part of ARDS management [9,10,11,12]. The prone position improves oxygenation by promoting dorsal recruitment, allowing for a more homogeneous ventilation distribution, and improving ventilation/perfusion matching. It may also reduce lung stress and strain with a potential for reducing Ventilation Induced Lung Injury (VILI) [13]. It is still debated if COVID-19 related ARDS represents a distinct entity and whether common treatments used in ARDS are equally effective [14,15,16]. International guidelines [17, 18] and experts [19], however, recommend the use of prone position in patients with COVID-19 related moderate to severe ARDS and this technique is more widely used than in the past [20, 21]. Some reports suggest a benefit of proning in COVID-19 patients [21,22,23,24,25,26,27,28,29], but few data are available on the physiological effects of proning in COVID-19 ARDS, except for the effect on the PaO2/FiO2 ratio. Factors associated with success and failure have also not been extensively described.
The main aim of this study was to assess the effects of proning in COVID-19 ARDS patients on oxygenation parameters (PaO2/FiO2 and alveolar-arterial gradient—Aa-gradient—) both for all the proning sessions considered together and for the first five proning sessions. As a secondary aim, we assessed the effects of proning (all sessions and first to fifth sessions) on other physiological and respiratory parameters such as respiratory mechanics, and dead space fraction estimates. Finally, as an ancillary aim, we looked for factors associated with treatment failure defined as ICU death or the need for veno-venous extracorporeal membrane oxygenation (VV-ECMO).
Methods
Retrospective study performed in the adult intensive care unit of the Lausanne University Hospital, Switzerland. The study protocol was accepted by the “Commission cantonale d’éthique de la recherche sur l’être humain” CER-VD (protocol number 2020-01453). All consecutive patients admitted during the first pandemic wave between the 06th of March and the 30th of April 2020 for PCR confirmed COVID-19 ARDS [30] who were invasively ventilated and proned at least once during their ICU stay were considered for inclusion. Patients proned only during ECMO treatment, patients already proned in a referring hospital and patients who refused utilization of their clinical data were excluded. To note, in Switzerland, for a retrospective analysis, the patients must accept the use of their recorded data for research purposes. Waiver of consent is possible, if accepted by the Ethics committee, for the deceased patients who did not refuse the use of their data before death, for the patients who did not adopt a position on the general consent procedure 6 weeks after having been contacted twice and for the patients who could not be contacted.
During the study period, all COVID-19 ARDS patients were treated following the local written clinical protocol that described intubation criteria, ventilation strategies including positive end-expiratory pressure (PEEP) setting (low to moderate PEEP strategy, clinical protocol available in the electronic supplementary material) and indications for proning. According to this protocol, all intubated patients with a PaO2/FiO2 < 150 mmHg and a FiO2 > 0.6 after curarisation were proned. When proning was decided, at least three sessions were performed, unless contraindicated or poorly tolerated. Data used in this study were retrieved from the patients’ medical file and the electronic medical records system. We collected data on demographics, established risk factors for severe COVID-19 infection, severity scores (SAPS II, SOFA) and blood gas analysis at ICU admission. On the day of intubation, we collected SOFA score, first blood gas analysis after intubation and concomitant end-tidal CO2 (EtCO2), ventilatory settings, plateau pressure and compliance of the respiratory system (CRS). Time from admission to intubation, from intubation to first proning and from the first documented PaO2/FiO2 < 150 mmHg to the first proning were recorded.
For each proning session we collected its duration and related serious complications (tube or catheter displacement, tube obstruction, cardiorespiratory arrest). Blood gas analysis and concomitant EtCO2, ventilatory settings, plateau pressure (Pplat), driving pressure (∆P) defined as Pplat–PEEP, and CRS were recorded within two hours before placement in prone position (pre-PP) and within two hours before returning supine (end-PP). Heart rate (HR), mean arterial pressure (MAP) and dose of norepinephrin in µg/kg/min were also recorded at the time of the blood gas analyses (pre-PP and end-PP times). As outcome data we recorded the number of days under mechanical ventilation, the number of ventilator free days at day 28 after intubation and the ICU and hospital length of stay.
Based on the collected data, we calculated for pre-PP and for end-PP time points Aa-gradient, PaCO2–EtCO2 gradient, ventilatory ratio (VR) [31] and dead space fraction estimated using the unadjusted Harris-Benedict estimate of resting energy expenditure and the rearranged Weir equation for CO2 production (VD/VT HB) [32] (Equations used are provided in Table 1).
As primary study outcome, we analyzed the effects of proning on oxygenation parameters (PaO2/FiO2 and Aa-gradient) both for all the prone positioning sessions and for the first to the fifth sessions independently. As a secondary aim we analyzed the effects of proning on other physiological and respiratory variables (blood gas analysis, VR, VD/VT HB, Pplat, ΔP and CRS) also for all the sessions and for the first to the fifth sessions. Positive response in terms of oxygenation (patients considered as O2-responders) was arbitrarily defined, as in a previous study [24], as an increase of more than 20% in PaO2/FiO2. Significant CO2 clearance (patients considered as CO2-responders) was defined as a decrease in PaCO2 of 1 mmHg or more according to the study by Gattinoni et al. [33] that showed a correlation between decrease in PaCO2 and outcome in non-COVID ARDS patients who were proned. To identify variables associated with patients’ outcomes, we arbitrarily defined treatment failure as a composite outcome including ICU death and need of VV-ECMO support. Consequently, treatment success was considered as ICU survival without VV- ECMO.
Statistics
Comparison between values before and at the end of proning (pre-PP and for end-PP timepoints) were assessed by paired T test or Wilcoxon signed rank test, according to data distribution. Continuous data for responders and non-responders and for treatment success and failure were compared with unpaired t test or Mann Whitney U test according to their distribution. Proportions were assessed using Fischer exact test or Chi square test as appropriate. Because most data were not normally distributed (Shapiro Wilk test), data are presented as medians with first and third quartiles (Q1-Q3). Data were analyzed with GraphPad Prism version 9.1 (GraphPad Software, San Diego, CA).
Results
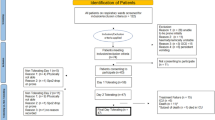
A total of 116 patients were admitted in our ICU due to COVID-19 pneumonia during the study period. Fifty-one were invasively ventilated and proned. Nine patients were excluded from the final analysis, 2 because they were proned during VV-ECMO treatment only, 6 because they did not accept the use of their data for retrospective analysis and 1 because he/she was already proned in another hospital before admission in our ICU. Thus, 42 patients were included in the final analysis (Fig. 1, flowchart). A total of 191 sessions were performed in these 42 patients and analyzed to assess the effect of proning on physiological parameters.
Baseline population and characteristics
The baseline characteristics and the baseline physiological and ventilatory parameters within 2 h after intubation (first available blood gas analysis after intubation, all patients paralyzed) are mentioned in Table 2 for the general patients population and for patients who experienced treatment success and failure. According to the Berlin classification [30], shortly after intubation among the global patients population, 10% were classified as severe ARDS, 80% as moderate and 10% as mild.
Among the 42 included patients, 12 (29%) experienced treatment failure, of whom 10 (24%) died in the ICU. Two (5%) eventually needed VV-ECMO support. These 2 patients were successfully weaned from VV-ECMO and mechanical ventilation and discharged from the hospital. The outcomes of the general population and of the patients who experienced treatment success and failure are mentioned in Table 2.
General data about intubation and proning
Median time from ICU admission to intubation was 4 (1–16) hours for the 36 patients who were not already intubated at ICU admission. Time from intubation to first proning was 46 (13–90) hours and time from the first PaO2/FiO2 < 150 mmHg to proning was 16 (5–36) hours. Patients sustained a median of 3 (2–6) proning sessions, with a median duration of 17 (16–19) hours. No serious complications attributed to prone positioning occurred during the 191 analyzed sessions.
No statistically significant differences between the success and failure groups were noted in intubation timing (p = 0.11) and proning timings (intubation to proning, p = 0.23 and first PaO2/FiO2 < 150 mmHg to proning, p = 0.48). The number of proning sessions (p = 0.94) or their duration (p = 0.39) were also not different between the 2 groups.
Effect of proning on physiological and respiratory data
Figure 2A illustrates the changes in PaO2/FiO2, FiO2, Aa-gradient, VR and VD/VT HB and CRS for all proning sessions considered together, between pre-PP and end-PP time points. The time between pre-PP blood gas analysis and start of proning was 66 (42–113) minutes. The time between end-PP blood gas analysis and end of proning was 72 (32–115) minutes. Figure 2B illustrates the changes on the same parameters for the first proning session.
Variations in PaO2/FiO2, FiO2, Aa gradient, CRS, VR and VD/VT HB for all sessions (A) and first session (B) before (pre PP) and at the end (end-PP) of the prone position session. PaO2: arterial partial pressure of oxygen, FiO2: fraction of inspired oxygen, Aa gradient: alveolo-arterial gradient, VR: ventilatory ratio, VD/VT HB: dead space fraction estimated using the unadjusted Harris-Benedict estimate of resting energy expenditure and the rearranged Weir equation for CO2 production, CRS: Compliance of the respiratory system
Additional physiological and respiratory variables, including hemodynamic data, before and at the end of the proning sessions are presented in Additional file 1 (Table S1) for all proning sessions together and for the first to the fifth sessions. Looking at the response in terms of oxygenation, 83% of all proning sessions led to an increase of more than 20% in the PaO2/FiO2 ratio (O2 responders). Only 44% of all proning sessions led to a significant reduction in CO2.
Table 3 illustrates the effects of the first to the third proning sessions on the changes in PaO2/FiO2, FiO2, Aa-gradient, VR, VD/VT HB, Pplat, ΔP and CRS for all the patients and for the patients who experienced treatment success or failure. The percentage of O2 and CO2 responders for the first to the third proning sessions for each patient group are also mentioned in Table 3. p values in Table 3 refer to the comparison between the treatment success and treatment failure groups. Additional file 1 (Table S2) mentions the same information for the fourth and the fifth sessions.
Factors associated with treatment failure
Patient in the treatment failure group were older (73 [61–78] vs 60 [56–69] years, p = 0.009), had a higher SOFA score at admission (6 (3–8) vs 3 (2–4), p = 0.012), less frequently had a BMI > 30 kg/m2 (8 vs 47%, p = 0.03), and were less likely to be smokers (0% vs 33%, p = 0.04) (Table 2). In addition, patients in the treatment failure group were less frequently O2-responders to the first proning session (p = 0.002), but not to the second (p = 0.66) and third (p = 0.64). The patients in the treatment failure group showed a smaller variation in Aa-gradient during the first session (− 105 [− 169–− 13] mmHg vs − 170 [− 248–− 124] mmHg, p = 0.01), but no differences in the variations in VR, VD/VT HB and CRS during the first session (P = 0.21, p = 0.19, p = 0.13, respectively), compared to the patients in the treatment success group. Variations of the same parameters during the second and third sessions are presented in Table 3 for the patients with treatment success and failure. Response in terms of CO2 clearance was not associated to outcome for any of the first three sessions (p = 0.51, p = 0.45 and p = 0.77, respectively).
Discussion
In this monocentric retrospective study performed in the Lausanne adult ICU during the first wave of the pandemic, we analyzed the physiological effects of prone positioning in a population of COVID-19 ARDS intubated patients treated with an early intubation, low to moderate PEEP and early proning strategy. At that time patients were managed in our ICU following a standardized protocol. They were systematically proned if they had a PaO2/FIO2 ratio < 150 mmHg despite curarization. Considering all proning sessions, we found a significative improvement in the PaO2/FiO2 ratio and reduction in Aa-gradient. We also found that 83% of the sessions lead to a more than 20% increase in the PaO2/FiO2 ratio. PaO2/FiO2 increment and Aa-gradient reduction was also found for each of the first five sessions individually. CRS increased with proning when all the sessions were considered together and we noticed a slight increase in VR and VD/VT HB. No serious adverse events were reported related to the proning sessions. Patients who experienced treatment failure were less frequently O2-responders to the first proning session, but not to the second and third sessions. They also had a smaller variation in the Aa-gradient following the first pronation. They were older, had a higher SOFA score at admission and were less frequently obese and smokers. Importantly, there were no differences in the time from intubation to the first proning, in the time from PaO2/FiO2 < 150 mmHg and the start of proning, in the number of proning sessions performed or in the sessions duration between the success and failure groups.
COVID 19 ARDS has some specificities compared to other forms of ARDS, such as severe hypoxemia being associated to slightly higher compliance in the early course of the disease [4, 34, 35]. In addition, according to Grieco et al. COVID-19 ARDS patients had higher VR, a dead space surrogate, than matched non COVID-19 patients [34]. This could be explained, even though still debated, to the presence of micro-thrombosis in the lung parenchyma [36], although technical issues such as dead space related to heat and moisture exchangers placed in the ventilator circuit might also be contributing factors [35]. In our cohort, we found a high VR at baseline shortly after intubation, in line with previous data in COVID patients [34, 37].
In the early phase of the pandemic, the value of the proning manoeuver in COVID-19 ARDS was questioned because of the above mentioned specificities [16], but the manoeuver has now been recognized as an adequate treatment option by experts [19].
Improvement in the PaO2/FiO2 ratio has been extensively reported during pronation in non-COVID-19 ARDS [9, 38] and the safety of this treatment strategy is well documented [38]. Increase in PaO2/FiO2 has been described in COVID-19 ARDS patients during proning [21,22,23,24, 28, 39] and our study confirms this finding. In addition, in our population treated with an early-intubation early-proning strategy, we found that a significant improvement in the PaO2/FiO2 ratio persists until the fifth proning session. This improvement is observed both with a reduction in FiO2 and a slight increase in PaO2. Several mechanisms may be implicated in this improvement in oxygenation. In ARDS from other causes, the main reason for the bettering of oxygenation is the improvement in ventilation-perfusion mismatch. This is a result of more homogeneous ventilation, with perfusion that is less altered by the prone position [13] and possibly less overdistension in the non-dependent lung regions. As a novel finding in our study, we observed the Aa-gradient to be practically halved at the end of the proning sessions. This observation was consistent throughout the five first sessions and definitely supports the major improvement of the ventilation to perfusion ratio during proning. This finding is of interest as this hypothesis is often mentioned as one of the main effects of prone positioning but very seldom reported in ARDS patients during proning.
Recruitment may in part account for the reduction in shunt fraction leading to better ventilation-perfusion matching. Indeed, in our cohort CRS increased when considering all sessions collectively. Other papers reported variable results regarding changes in CRS related to proning. Some showed improved compliance [27, 29], but others did not [21, 24]. The favorable effect of proning on CRS was also shown in a small group of COVID-19 patients studied by electrical impedance tomography [40]. The change in CRS is probably the result of both the change in thoracic compliance and in lung compliance due to the recruitment in the dorsal regions and compression in ventral regions [41] and this may differ in various patient cohorts. The favorable effects observed in our cohort might be due to proning in the early ARDS stage, in which lung may be more recruitable as suggested in the trial by Rossi et al. [42]. In this trial they found that during the first week of ventilation, patients with COVID-19 ARDS have more recruitable lung tissue than patients studied during the third week [42]. Interestingly, COVID-19 ARDS appears to be less recruitable than matched population with non-COVID-19 ARDS [43, 44]. It is worth noting that the change in CRS was not significant if we consider each session independently. This could be explained by a heterogeneity of response to recruitment between patients and in the same patient at different timepoints as reported by Beloncle et al. [45].
CRS might also fail to increase due to overdistention in non-dependent lung regions. This might be the case in our population as PEEP was not systematically adapted during proning and it was found to be only marginally decreased. In our cohort VR, a parameter which was correlated with measured VD/VT in COVID-19 ARDS patients [46, 47] as well as in non-COVID ARDS, was only slightly increased with an amplitude that in our opinion is not clinically relevant and this may suggest that overdistention is not a major concern. The absence in a clinically significant change of dead space estimated by VD/VT HB corroborates the absence of overdistention in our study.
Other studies investigated the changes in various physiological and respiratory parameters during proning in ARDS COVID-19 patients, but important differences between these studies and our must be underlined. Weiss and collaborators considered the first three proning sessions in 42 patients [24]. Their population could be compared to ours in term of CRS and PaO2/FiO2, but their ventilation strategy differed with a higher set PEEP (median of 16 cmH2O compared to 12 in our study) and lower tidal volumes (median of 6 compared to 6.7 ml/kg of predicted body weight in our study). In contrast to our study, VR increased significantly and CRS did not change during prone positioning in the Weiss’ study. The higher set PEEP strategy might have been responsible for increased overdistension and reduced perfusion in the overdistended area, as demonstrated in the physiological studies by Perier and Mauri [40, 48]. Our data reinforces the idea that a lower PEEP strategy might be beneficial in limiting overdistention, as suggested by some expert opinions [49] and recent data, at least in some COVID-19 ARDS patients [50]. Furthermore, differently from our population they observed a greater improvement in oxygenation for the first, second and third session in the treatment success group, whereas in our population, we found a major response (defined as an increase of at least 20% in the PaO2/FIO2 ratio) in terms of oxygenation only during the first proning session. Langer and collaborators studied 78 ARDS COVID-19 patients [21] before and after the first prone positioning. They found an improved PaO2/FiO2, but no difference in CRS and VR. Ziehr et al. also studied the response to the first proning session in 122 patients with COVID-19. They found similar results compared to ours for the first session, with an improved PaO2/FiO2 ratio, but no change in CRS or VD/VT [39]. In addition to this, we can confirm with our data that the same findings apply for at least each of the first five sessions. As these studies only considered the first proning session, they do not answer the question whether the effects of proning in COVID-19 ARDS patients are temporary or persistent. In summary, our study is one of the few to address the effects of proning on as many physiological variables and on as many sessions in COVID-19 ARDS patients ventilated with a low to moderate PEEP strategy.
Regarding the outcome prediction in our study, we found a correlation between treatment failure defined as ICU death or need for VV-ECMO and older age, lower BMI and higher SOFA score at admission. Patients in the failure group were less frequently responders to the first proning session in terms of oxygenation. Naturally, our results regarding the factors associated with treatment success and failure must be confirmed in larger cohorts. Interestingly, a better response in terms of oxygenation to the first prone position was recently associated to lower mortality and weaning from mechanical ventilation at 28 days in a prospective study [51], which is congruent with our results.
The main limitation of this study is its retrospective and monocentric design. However, we assessed all the patients admitted during the study period and we examined a high number of prone position sessions. As important parameters were automatically recorded in the patients’ medical files, we had few missing data. Secondly, we studied patients who were treated according to an early-intubation, moderate PEEP and early-proning strategy. Our results cannot be generalized to other treatment strategies, for example for higher PEEP. It is worth noting that the median tidal volume in our patient cohort was 6.7 [6.0–7.0] ml/kg of predicted body weight (PBW), which is in line with values reported in the literature for patients treated during the first wave of COVID-19 [20] and with guidelines [11]. Whether our results on physiologic parameters would have been the same with lower tidal volumes is unknown. Thirdly, there was no control group. However, as proning is recommended by experts as being part of the management of COVID-19 ARDS with moderate to severe hypoxemia, having such a group is currently not possible. Fourthly, studying the effects of proning on advanced hemodynamic parameters, shunt fraction and right heart function would have been of interest. However, this was not feasible based on the available data as venous blood gases, central venous pressure measurements, invasive hemodynamic monitoring and echocardiography could not be systematically performed due to the workload during the pandemics. In practice, they were only performed in a minority of patients who were hemodynamically unstable. Fifthly, we must acknowledge that the threshold of 20% of improvement in PaO2/FIO2 ratio chosen to define significant improvement on oxygenation is arbitrary and that different results regarding the proportion of O2 responders could have been found with different thresholds. The threshold we used was the same as the threshold used in the Weiss et al. study [24] but differs from the threshold used in the Langer et al. [21] and in the Vollenberg et al. [26] studies who respectively used a fixed threshold of 20 mmHg and a 15% improvement in PaO2/FIO2 ratio. The threshold of decrease in 1 mmHg or more in PaCO2 used to assess CO2 response was also arbitrary, even if previously associated with improved outcome in non-COVID ARDS patients who were proned [33]. Finally, regarding the evaluation of the factors associated with treatment failure or success, it is important to underline that the composite outcome used to define treatment failure (ICU death or need of VV-ECMO) is arbitrary.
Conclusion
In conclusion, our data showed the benefits of prone positioning in regards of improved oxygenation and reduction in alveolar-arterial gradient in COVID-19 ARDS patients with a PaO2/FiO2 ratio less than 150 mmHg treated with an early intubation, low to moderate PEEP and early pronation strategy. This was demonstrated for all proning sessions collectively as well as for the first and the subsequent sessions taken individually. When all the sessions were considered together, we also noticed an increase in CRS. No major complications related to proning were recorded. In addition, our data suggest that response to the first proning in terms of oxygenation and reduction of alveolar-arterial gradient might be linked to favorable outcome defined as survival without the need of VV-ECMO. Further studies are needed to confirm these interesting findings. From a clinical point of view, our study demonstrated similar physiological effects of proning in COVID-19 ARDS as compared to ARDS due to other causes and thus suggests that prone positioning in COVID-19 ARDS should be part of the standard of care.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- Aa-gradient:
-
Alveolo arterial gradient
- ARDS:
-
Acute respiratory distress syndrome
- COVID19:
-
Coronavirus disease 2019
- Crs :
-
Compliance of the respiratory system
- EtCO2 :
-
End tidal partial pressure of carbon dioxide
- FiO2 :
-
Fraction of inspired oxygen
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PaO2 :
-
Arterial partial pressure of oxygen
- PEEP:
-
Positive end-expiratory pressure
- PP:
-
Prone position
- Pplat:
-
Plateau pressure
- SAPS II:
-
Simplified Acute Physiology Score II
- SOFA:
-
Sequential Organ Failure Assessment
- VD/VT HB:
-
Dead space fraction estimated using the unadjusted Harris-Benedict estimate of resting energy expenditure and the rearranged Weir equation for CO2 production
- VILI:
-
Ventilation induced lung injury
- VR:
-
Ventilatory ratio
References
Johns Hopkins University. Coronavirus Resource Centre https://coronavirus.jhu.edu/map.html. Accessed 1 July 2022.
Lee HK, Kim EY, Kim HS, Park EJ, Lee HJ, Lee TY, et al. Effect of human mesenchymal stem cells on xenogeneic T and B cells isolated from lupus-prone MRL.Fas (lpr) Mice. Stem Cells Int. 2020;2020:5617192.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9.
Grasselli G, Tonetti T, Protti A, Langer T, Girardis M, Bellani G, et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med. 2020;8(12):1201–8.
Network C-IGobotR, the C-ICUI. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47(1):60–73.
Kurtz P, Bastos LSL, Dantas LF, Zampieri FG, Soares M, Hamacher S, et al. Evolving changes in mortality of 13,301 critically ill adult patients with COVID-19 over 8 months. Intensive Care Med. 2021;47(5):538–48.
Kim L, Garg S, O’Halloran A, Whitaker M, Pham H, Anderson EJ, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET). Clin Infect Dis. 2021;72(9):e206–14.
Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369: m1985.
Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–68.
Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69.
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–63.
Lee JM, Bae W, Lee YJ, Cho YJ. The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: updated study-level meta-analysis of 11 randomized controlled trials. Crit Care Med. 2014;42(5):1252–62.
Guerin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46(12):2385–96.
Fan E, Beitler JR, Brochard L, Calfee CS, Ferguson ND, Slutsky AS, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med. 2020;8(8):816–21.
Robba C, Battaglini D, Ball L, Patroniti N, Loconte M, Brunetti I, et al. Distinct phenotypes require distinct respiratory management strategies in severe COVID-19. Respir Physiol Neurobiol. 2020;279: 103455.
Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099–102.
Alhazzani W, Evans L, Alshamsi F, Moller MH, Ostermann M, Prescott HC, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: first update. Crit Care Med. 2021;49(3):e219–34.
Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020;48(6):e440–69.
Nasa P, Azoulay E, Khanna AK, Jain R, Gupta S, Javeri Y, et al. Expert consensus statements for the management of COVID-19-related acute respiratory failure using a Delphi method. Crit Care. 2021;25(1):106.
Grasselli G, Cattaneo E, Florio G, Ippolito M, Zanella A, Cortegiani A, et al. Mechanical ventilation parameters in critically ill COVID-19 patients: a scoping review. Crit Care. 2021;25(1):115.
Langer T, Brioni M, Guzzardella A, Carlesso E, Cabrini L, Castelli G, et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multi-centric study of more than 1000 patients. Crit Care. 2021;25(1):128.
Gleissman H, Forsgren A, Andersson E, Lindqvist E, Lipka Falck A, Cronhjort M, et al. Prone positioning in mechanically ventilated patients with severe acute respiratory distress syndrome and coronavirus disease 2019. Acta Anaesthesiol Scand. 2021;65(3):360–3.
Berrill M. Evaluation of oxygenation in 129 proning sessions in 34 mechanically ventilated COVID-19 patients. J Intensive Care Med. 2021;36(2):229–32.
Weiss TT, Cerda F, Scott JB, Kaur R, Sungurlu S, Mirza SH, et al. Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to COVID-19: a retrospective observational cohort study. Br J Anaesth. 2021;126(1):48–55.
Mittermaier M, Pickerodt P, Kurth F, de Jarcy LB, Uhrig A, Garcia C, et al. Evaluation of PEEP and prone positioning in early COVID-19 ARDS. EClinicalMedicine. 2020;28: 100579.
Vollenberg R, Matern P, Nowacki T, Fuhrmann V, Padberg JS, Ochs K, et al. Prone position in mechanically ventilated COVID-19 patients: a multicenter study. J Clin Med. 2021;10(5):1046.
Park J, Lee HY, Lee J, Lee SM. Effect of prone positioning on oxygenation and static respiratory system compliance in COVID-19 ARDS vs non-COVID ARDS. Respir Res. 2021;22(1):220.
Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, et al. Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: a cohort study and analysis of physiology. J Intensive Care Med. 2021;36(2):241–52.
Ziehr DR, Alladina J, Petri CR, Maley JH, Moskowitz A, Medoff BD, et al. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: a cohort study. Am J Respir Crit Care Med. 2020;201(12):1560–4.
Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
Sinha P, Fauvel NJ, Singh S, Soni N. Ventilatory ratio: a simple bedside measure of ventilation. Br J Anaesth. 2009;102(5):692–7.
Beitler JR, Thompson BT, Matthay MA, Talmor D, Liu KD, Zhuo H, et al. Estimating dead-space fraction for secondary analyses of acute respiratory distress syndrome clinical trials. Crit Care Med. 2015;43(5):1026–35.
Gattinoni L, Vagginelli F, Carlesso E, Taccone P, Conte V, Chiumello D, et al. Decrease in PaCO2 with prone position is predictive of improved outcome in acute respiratory distress syndrome. Crit Care Med. 2003;31(12):2727–33.
Grieco DL, Bongiovanni F, Chen L, Menga LS, Cutuli SL, Pintaudi G, et al. Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies. Crit Care. 2020;24(1):529.
Beloncle F, Studer A, Seegers V, Richard JC, Desprez C, Fage N, et al. Longitudinal changes in compliance, oxygenation and ventilatory ratio in COVID-19 versus non-COVID-19 pulmonary acute respiratory distress syndrome. Crit Care. 2021;25(1):248.
Santamarina MG, Boisier D, Contreras R, Baque M, Volpacchio M, Beddings I. COVID-19: a hypothesis regarding the ventilation-perfusion mismatch. Crit Care. 2020;24(1):395.
Torres A, Motos A, Riera J, Fernandez-Barat L, Ceccato A, Perez-Arnal R, et al. The evolution of the ventilatory ratio is a prognostic factor in mechanically ventilated COVID-19 ARDS patients. Crit Care. 2021;25(1):331.
Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplement4):S280–8.
Ziehr DR, Alladina J, Wolf ME, Brait KL, Malhotra A, La Vita C, et al. Respiratory physiology of prone positioning with and without inhaled nitric oxide across the coronavirus disease 2019 acute respiratory distress syndrome severity spectrum. Crit Care Explor. 2021;3(6): e0471.
Perier F, Tuffet S, Maraffi T, Alcala G, Victor M, Haudebourg AF, et al. Effect of positive end-expiratory pressure and proning on ventilation and perfusion in COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;202(12):1713–7.
Galiatsou E, Kostanti E, Svarna E, Kitsakos A, Koulouras V, Efremidis SC, et al. Prone position augments recruitment and prevents alveolar overinflation in acute lung injury. Am J Respir Crit Care Med. 2006;174(2):187–97.
Rossi S, Palumbo MM, Sverzellati N, Busana M, Malchiodi L, Bresciani P, et al. Mechanisms of oxygenation responses to proning and recruitment in COVID-19 pneumonia. Intensive Care Med. 2022;48(1):56–66.
Chiumello D, Busana M, Coppola S, Romitti F, Formenti P, Bonifazi M, et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: a matched cohort study. Intensive Care Med. 2020;46(12):2187–96.
Ball L, Robba C, Maiello L, Herrmann J, Gerard SE, Xin Y, et al. Computed tomography assessment of PEEP-induced alveolar recruitment in patients with severe COVID-19 pneumonia. Crit Care. 2021;25(1):81.
Beloncle FM, Pavlovsky B, Desprez C, Fage N, Olivier PY, Asfar P, et al. Recruitability and effect of PEEP in SARS-Cov-2-associated acute respiratory distress syndrome. Ann Intensive Care. 2020;10(1):55.
Diehl JL, Peron N, Chocron R, Debuc B, Guerot E, Hauw-Berlemont C, et al. Respiratory mechanics and gas exchanges in the early course of COVID-19 ARDS: a hypothesis-generating study. Ann Intensive Care. 2020;10(1):95.
Sinha P, Calfee CS, Beitler JR, Soni N, Ho K, Matthay MA, et al. Physiologic analysis and clinical performance of the ventilatory ratio in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2019;199(3):333–41.
Mauri T, Spinelli E, Scotti E, Colussi G, Basile MC, Crotti S, et al. Potential for lung recruitment and ventilation-perfusion mismatch in patients with the acute respiratory distress syndrome from coronavirus disease 2019. Crit Care Med. 2020;48(8):1129–34.
Hajjar LA, Costa I, Rizk SI, Biselli B, Gomes BR, Bittar CS, et al. Intensive care management of patients with COVID-19: a practical approach. Ann Intensive Care. 2021;11(1):36.
Bastia L, Rezoagli E, Guarnieri M, Engelberts D, Forlini C, Marrazzo F, et al. External chest-wall compression in prolonged COVID-19 ARDS with low-compliance: a physiological study. Ann Intensive Care. 2022;12(1):35.
Scaramuzzo G, Gamberini L, Tonetti T, Zani G, Ottaviani I, Mazzoli CA, et al. Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: a cohort study. Ann Intensive Care. 2021;11(1):63.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AB and LP contributed to the study design. AB MR LP performed data collection and analysis. AB wrote the first draft. All the authors contributed substantially to data interpretation and writing of the manuscript. AB MR and LP had full access to all the data in the study and take responsibility for the integrity and the accuracy of the data analysis They take responsibility for the content of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical Committee Name: Commission Cantonale d'Ethique de la Recherche sur l’Etre Humain (CER-VD). Retrospective use of clinical data (Protocol number: 2020-01453). Waiver of consent was obtained for the deceased patients who did not formerly refuse the use of their data for clinical research. The present protocol was registered on ClinicalTrials.gov (NCT05092737).
Consent for publication
Not applicable as data are coded.
Competing interests
The authors declare that they have no competing interests related to this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Physiological, ventilatory and hemodynamic data for all the sessions considered together (n=191) and for the first (n=42), the second (n=37), the third (n=31), the fourth (n=18) and the fifth (n=14) proning sessions). Table S2. Variations in physiological and ventilatory parameters during the fourth (n=18), the fifth (n=14) proning sessions. Comparisons between the success and failure group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boffi, A., Ravenel, M., Lupieri, E. et al. Physiological response to prone positioning in intubated adults with COVID-19 acute respiratory distress syndrome: a retrospective study. Respir Res 23, 320 (2022). https://doi.org/10.1186/s12931-022-02247-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02247-8